Abstract
ABO blood group system, a well-known genetic risk factor, has clinically been demonstrated to be linked with thrombotic vascular diseases. However, the relationship between ABO blood group and coronary artery disease (CAD) is still controversial. We here performed an updated meta-analysis of the related studies and tried to elucidate the potential role of ABO blood group as a risk factor for CAD. All detectable case-control and cohort studies comparing the risk of CAD in different ABO blood groups were collected for this analysis through searching PubMed, Embase and the Cochrane Library. Ultimately, 17 studies covering 225,810 participants were included. The combined results showed that the risk of CAD was significantly higher in blood group A (OR = 1.14, 95% CI = 1.03 to 1.26, p = 0.01) and lower in blood group O (OR = 0.85, 95% CI = 0.78 to 0.94, p = 0.0008). Even when studies merely about myocardial infarction (MI) were removed, the risk of CAD was still significantly higher in blood group A (OR = 1.05, 95% CI = 1.00 to 1.10, p = 0.03) and lower in blood group O (OR = 0.89, 95% CI = 0.85 to 0.93, p < 0.00001). This updated systematic review and meta-analysis indicated that both blood group A and non-O were the risk factors of CAD.
Similar content being viewed by others
Introduction
In 1901, Karl Landsteiner, a Viennese MD and pathologist, discovered ABO blood group system which was the first human blood group1. From then on, studies on relation of ABO blood group system to various diseases have never been interrupted for a century, even in the popular era of gene detection, as ABO blood group is inherent in human’s body and easily to be tested.
It has been reported that ABO blood group system is associated with cognitive impairment2, preeclampsia3, bleeding, neoplastic diseases4 and even longevity5. Among all of those studies, the mechanism of relationship between ABO blood group and venous thrombosis is elucidated6 and its major determinants are von Willebrand factor (vWF) and coagulation factor VIII7 which result in thrombosis. This interesting finding makes a theoretical hypothesis that ABO blood group may also be related to risk of coronary artery disease (CAD) and myocardial infarction (MI). Unfortunately, results of previous relevant studies are currently not convincing due to inconsistent conclusions. And previous studies including original observations and meta-analysis8,9,10 mainly paid attention to the blood group non-O and O, ignoring the blood group A and other blood types. Moreover, in those studies, links of ABO blood group with MI was often focused on; however, the relation between risk of CAD and ABO blood group was carelessly overlooked. Therefore, this updated systematic review and meta-analysis aims to evaluate the relationship between CAD and each type of ABO blood group.
Results
Description of included studies
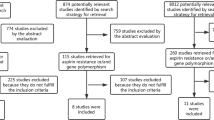
Two hundred and thirty-one studies (231 from Pubmed and 0 from the Cochrane Library) were identified from two databases. Among them, 10 records were removed on account of duplicates. By screening titles and abstracts, we excluded 147 records on account of animal experiments, traditional reviews, improper or lack of comparison, or other blood group classification systems rather than ABO blood type. By browsing full-text articles, we excluded 58 records because of improper or lack of comparison, other confounding factors, irrelevant to the outcomes of this study and unavailable outcomes. At last, a total of 16 articles11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26 which met inclusion criteria were included into this systematic review. A flow-chart of study selection was generated according to the PRISMA requirements (Fig. 1).
Study characteristics
One15 of these 16 articles contained 2 studies. All the 17 studies were published in English from 1961 to 2014. Eleven articles11,13,14,16,17,19,21,22,23,25,26 were case-control studies, 2 articles12,15 were prospective cohort studies and 3 articles18,20,24 were retrospective cohort studies. Finally, a total of 225,810 patients were included. All studies described race and characteristic of the two groups. Nine studies12,16,17,19,20,21,22,23,24 merely mentioned MI. Two studies12,17 only differentiated blood group non-O from blood group O. The remaining studies described all blood types. (Basic characteristics of included studies were presented in Table 1 and blood types distribution and outcome definitions of included studies were presented in Table 2 and Newcastle-Ottawa Scale (NOS) table was shown in Table 3).
Main, subgroup and sensitivity analysis
All the 17 studies were included in this meta-analysis. Because of unnegligible heterogeneity in them, we conducted a subgroup analysis according to the research types (case-control study, prospective or retrospective cohort study) and used random-effect model27. Risk of CAD was significantly increased in patients with blood group A compared with blood group non-A (odds ratio (OR) = 1.14, 95% confidence intervals (CI) = 1.03 to 1.26, p = 0.01). Subjects in blood group A had a statistical increase in CAD incidence in case-control studies (OR = 1.14, 95% CI = 1.04 to 1.26, p = 0.005) with moderate heterogeneity (I2 = 45%), while there was no statistical difference between blood group A and non-A in cohort studies (Fig. 2). Besides, risk of CAD had no statistical significant difference in patients with blood group B, AB compared with non-B, non-AB, respectively (Figs 3 and 4). Whereas, in contrast to the result of blood group A, blood group O was proved to be a protective factor in our analysis, presenting a decrease of CAD risk (OR = 0.85, 95% CI = 0.78 to 0.94, p = 0.0008). Our analysis found that there was statistical significant difference in CAD incidence in case-control studies (OR = 0.86, 95% CI = 0.75 to 0.99, p = 0.04) in spite of high heterogeneity (I2 = 78%), which is similar to prospective cohort studies (OR = 0.94, 95% CI = 0.89 to 0.98, p = 0.009) with no heterogeneity (I2 = 0). However, there was no statistical significant difference in CAD incidence in retrospective cohort studies (OR = 0.58, 95% CI = 0.35 to 0.97, p = 0.04) with high heterogeneity (I2 = 70%) (Fig. 5). In the sensitivity analysis, exclusion of any single study did not substantively alter the overall result in blood group A, B, AB and O. In order to exclude the effect of established positive relationship between ABO blood group and MI, we removed the studies12,16,17,19,20,21,22,23,24 which only paid attention to MI patients and found the similar relationship between ABO blood group and CAD as before, namely, A (OR = 1.05, 95% CI = 1.00 to 1.10, p = 0.03) and O (OR = 0.89, 95% CI = 0.85 to 0.93, p < 0.00001).
Furthermore, risk of MI was significantly higher in blood group A (OR = 1.24, 95% CI = 0.97 to 1.59, p = 0.08) compared with non-A group. Nevertheless, patients with blood group B or AB compared to non-B or non-AB, respectively, had no statistical differences in MI incidence (OR = 0.94, 95% CI = 0.74 to 1.18, p = 0.59; OR = 1.11, 95% CI = 0.91 to 1.35, P = 0.31). However, an overall effect was detected to be statistically different when comparing blood group O with non-O for the risk of MI (OR = 0.81, 95% CI = 0.69 to 0.94, p = 0.007).
Publication bias
We generated a funnel plot to assess publication bias. Exploration for the funnel plot of the blood group O in CAD suggested no asymmetry. No obvious evidence of publication bias was present in the comparison of blood group O (Fig. 6).
Discussion
Previous systematic reviews and meta-analysis paid more attention to the relationship between MI and ABO blood group, but the link of ABO blood group system to CAD was rarely evaluated. Besides, almost all available studies principally focused on blood type non-O and O. Hence, the relation between ABO blood group and risk of CAD is worthy to be assessed scientifically and strictly.
Our meta-analysis involved 16 articles (17 studies) covering 225,810 individuals. It was suggested that the risk of CAD in blood group A was mildly increased compared with that in blood group non-A (OR = 1.14). Meanwhile, we investigated the relationship of blood group B, AB compared with non-B, non-AB, respectively, but failed to confirm statistical difference. Moreover, our results indicated that the risk of CAD in blood group O was significantly lower than that in non-O groups (OR = 0.85), which is similar to previous studies8.
To our knowledge, this is the first meta-analysis involved the relationship between the risk of CAD and blood group A and non-A. Several clinical studies have provided direct evidence with different results. Whincup et al.28 found that the incidence of ischaemic CAD was higher in those with blood group A than that with blood group non-A (OR = 1.21, 95% CI = 1.01 to 1.46). A study from Wazirali et al.29 suggested that blood group A was associated with a substantially increased risk of CAD, which is independent of conventional cardiovascular risk factors. Whereas, another research did not support this association and indicated that the risk of CAD in blood group A was lower than that in other blood groups30. As we known, meta-analyses provide advance over traditional single studies. That is a reason why we performed a meta-analysis for further evaluating the relation of blood group A to the risk of CAD. In our study, we affirmed blood group A was a risk factor, which is more convincing and reliable. Similar evidence was more robust in the analysis for MI incidence (OR = 1.24).
Our study showed a significantly reduced risk of CAD in individuals with blood group O compared with that with blood group non-O (OR = 0.85, 95% CI = 0.78 to 0.94, p = 0.0008). Evidence was more obvious when we performed an analysis concerning the relationship between ABO blood group and MI (OR = 0.81, 95% CI = 0.69 to 0.94, p = 0.007). In fact, non-O blood group as an independent risk factor was already confirmed in other systematic reviews, too8,9,10. Wu et al.9 performed a meta-analysis with regard to the relation of ABO blood group to MI and angina in 2008. In their study, taking group O as index, group A and non-O were related to an increase in MI risk (OR = 1.29, 95% CI = 1.16 to 1.45, p < 0.00001, OR = 1.25, 95% CI = 1.14 to 1.36, p < 0.00001), while no similar effect was found in the risk of angina. Furthermore, a meta-analysis by Dentali et al.8 found that patients with blood group non-O presented a higher prevalence of MI than that with blood group O (OR = 1.28, 95% CI = 1.17 to 1.40, p < 0.001). Takagi et al.10 enrolled 10 studies with a total of 174,945 participants and demonstrated a 14% increase in CAD incidence in individuals with blood group non-O compared to that in blood group O (OR = 1.14, 95% CI = 1.04 to 1.25, p < 0.006). All in all, the quantitative results from these meta-analyses and our one provided plenty of evidence on the close relationship between risk of CAD and blood group non-O.
The underlying mechanism of the relationship between blood group O and CAD has been clarified. ABO antigen may affect plasma levels of vWF and coagulation factor VIII7 and blood group non-O has the lowest expression of O antigen and relatively higher levels of vWF and factor VIII31. That blood group O is a potentially important genetic risk factor for bleeding32, which also supports this mechanism theory. Another biologically plausible mechanism involves in glycotransferase-deficient enzyme which renders the ABO blood group to encode O phenotype, resulting in protection of subjects from MI risk33. The latest study reveals that serum lipid mediates the effect of ABO blood group on CAD. In fact, blood group A is one of the risk factors of CAD mainly due to higher serum total cholesterol (TC) concentration in subjects28. Our recent study also indicated that there is an association between blood group A and risk of CAD and around 10.5% of the effect of blood group A on CAD is mediated by TC levels34.
It was mentioned that there were several potential limitations in this study. Firstly, there was certain heterogeneity between various studies. Although we performed subgroup analyses, it was still different among the studies in blood testing methods and diagnostic criteria of CAD, race, life and eating habits, religious beliefs, socio-economic patterns and concern of the disease, which might result in the heterogeneity. Secondly, we did not find unpublished studies, which may bring about publication bias.
In conclusion, this updated meta-analysis suggests that blood group A and non-O are associated with an increased risk of CAD. However, considering the heterogeneity of included studies and limited number of studies, more rigorous studies with high quality are needed to give high level of evidence to confirm this association.
Methods
This meta-analysis was performed according to the MOOSE group guidelines of observational meta-analyses35.
Data sources and searches
Two reviewers (Zhuo Chen and Sheng-Hua Yang) searched Pubmed and the Cochrane Library from their inception to August 15, 2015 in order to identify all existing literature which assessed the association between ABO blood group and CAD. Mesh vocabulary and free text terms were used for each database with relevant key words such as blood grouping and cross-matching, ABO blood group system, blood group antigens, myocardial ischemia, myocardial infarction, acute coronary syndrome and angina pectoris. Language was limited to English. There was no limitation of country and publication date.
To ensure comprehensive acquisition of studies, the reference lists of the included articles were also manually screened to identify additional eligible studies. Manual searches were also performed on other databases, including Web of Science and Google Scholar. Furthermore, databases of ongoing trials were also searched: Clinical Trials.gov (http://clinicaltrials.gov/) and Current Controlled Trials (http://www.controlled-trials.com/).
Study selection
Studies were independently identified by two reviewers (Zhuo Chen and Sheng-Hua Yang) according to inclusion criteria. Disagreements were resolved through discussion and decided by a third reviewer. Both case-control and cohort studies were included if they met all the following criteria: 1) patients with CAD or even MI; 2) separate data for patients with or without CAD were provided; 3) diseases were objectively diagnosed in line with the diagnosis level at the time; 4) a clear extractable ABO blood group typing. Patients included were regardless of age and race.
Data extraction and quality assessment
The retrieved papers were subjected to a rigorous extraction by two authors (Zhuo Chen and Sheng-Hua Yang) independently according to a predesigned form. Disagreements were resolved by consensus or consulted from the third author (Hao Xu). We did not try to contact authors to obtain unpublished data. The methodological quality of studies was assessed using the NOS checklist for observational studies36. We rated cohort studies a maximum of 4 stars for selection, 2 stars for comparability and 3 stars for outcome assessment. The maximum score of case-control studies for selection, comparability and exposure assessment was 4, 2, 3, respectively, too. The highest score is 9 and more stars meant better quality.
Data analysis and synthesis
Revman 5.2 software (The Cochrane Collaboration, Oxford, UK) was used for data analyses. We presented dichotomous data as OR and its 95% CI. Data were assessed by both random and fixed effect models, but only the random effect analyses were reported if the heterogeneity was significant evaluated by the I2 statistic which assessed the appropriateness of pooling all studies27. A funnel plot was used to assess publication bias.
Additional Information
How to cite this article: Chen, Z. et al. ABO blood group system and the coronary artery disease: an updated systematic review and meta-analysis. Sci. Rep. 6, 23250; doi: 10.1038/srep23250 (2016).
References
Lesky, E. Viennese serological research about the year 1900: its contribution to the development of clinical medicine. Bull N Y Acad Med 49, 100–111 (1973).
Alexander, K. S. et al. ABO blood type, factor VIII and incident cognitive impairment in the REGARDS cohort. Neurology 83, 1271–1276 (2014).
Alpoim, P. N. et al. Preeclampsia and ABO blood groups: a systematic review and meta-analysis. Mol Biol Rep 40, 2253–2261 (2013).
Liumbruno, G. M. & Franchini, M. Hemostasis, cancer and ABO blood group: the most recent evidence of association. J Thromb Thrombolysis 38, 160–166 (2014).
Franchini, M. & Bonfanti, C. Evolutionary aspects of ABO blood group in humans. Clin Chim Acta 444, 66–71 (2015).
Dentali, F. et al. Non-O blood type is the commonest genetic risk factor for VTE: results from a meta-analysis of the literature. Semin Thromb Hemost 38, 535–548 (2012).
Jenkins, P. V. & O’Donnell, J. S. ABO blood group determines plasma von Willebrand factor levels: a biologic function after all? Transfusion 46, 1836–1844 (2006).
Dentali, F., Sironi, A. P., Ageno, W., Crestani, S. & Franchini, M. ABO blood group and vascular disease: an update. Semin Thromb Hemost 40, 49–59 (2014).
Wu, O., Bayoumi, N., Vickers, M. A. & Clark, P. ABO(H) blood groups and vascular disease: a systematic review and meta-analysis. J Thromb Haemost 6, 62–69 (2008).
Takagi, H. & Umemoto, T. Meta-analysis of non-O blood group as an independent risk factor for coronary artery disease. Am J Cardiol 116, 699–704 (2015).
Chen, Y. et al. Analysis of circulating cholesterol levels as a mediator of an association between ABO blood group and coronary heart disease. Circ Cardiovasc Genet 7, 43–48 (2014).
Sode, B. F., Allin, K. H., Dahl, M., Gyntelberg, F. & Nordestgaard, B. G. Risk of venous thromboembolism and myocardial infarction associated with factor V Leiden and prothrombin mutations and blood type. CMAJ 185, 229–237 (2013).
Biswas, S., Ghoshal, P. K., Halder, B. & Mandal, N. Distribution of ABO blood group and major cardiovascular risk factors with coronary heart disease. Biomed Res Int 2013, 782941 (2013).
Lee, H. F. et al. Association of blood group A with coronary artery disease in young adults in Taiwan. Intern Med 51, 1815–1820 (2012).
He, M. et al. ABO blood group and risk of coronary heart disease in two prospective cohort studies. Arterioscler Thromb Vasc Biol 32, 2314–2320 (2012).
Sari, I. et al. ABO blood group distribution and major cardiovascular risk factors in patients with acute myocardial infarction. Blood Coagul Fibrin 19, 231–234 (2008).
Tanis, B., Algra, A., van der Graaf, Y., Helmerhorst, F. & Rosendaal, F. Procoagulant factors and the risk of myocardial infarction in young women. Eur J Haematol 77, 67–73 (2006).
Amirzadegan, A. et al. Correlation between ABO blood groups, major risk factors and coronary artery disease. Int J Cardiol 110, 256–258 (2006).
Nydegger, U. E., Wuillemin, W. A., Julmy, F., Meyer, B. J. & Carrel, T. P. Association of ABO histo-blood group B allele with myocardial infarction. Eur J Immunogenet 30, 201–206 (2003).
Platt, D., Muhlberg, W., Kiehl, L. & Schmitt-Ruth, R. ABO blood group system, age, sex, risk factors and cardiac infarction. Arch Gerontol Geriatr 4, 241–249 (1985).
Saha, N., Toh, C. C. & Ghosh, M. B. Genetic association in myocardial infarction. Ethnicity; ABO, Rh, Le, Xg blood groups; G6PD deficiency; and abnormal haemoglobins. J Med Genet 10, 340–345 (1973).
Allan, T. M. & Dawson, A. A. ABO blood groups and ischaemic heart disease in men. Br Heart J 30, 377–382 (1968).
Gjorup, L. Blood groups and coronary occlusion. Acta Genet Stat Med 13, 178–183 (1963).
Pell, S. & D’Alonzo, C. A. A three-year study of myocardial infarction in a large employed population. JAMA 175, 463–470 (1961).
Franchini, M. et al. ABO blood group and risk of coronary artery disease. J Thromb Thrombolys 36, 286–287 (2013).
Gong, P. et al. High-sensitivity C-reactive protein mediates in part the impact of ABO blood group on coronary artery disease. Int J Cardiol 177, 641–643 (2014).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557 (2003).
Whincup, P. H., Cook, D. G., Phillips, A. N. & Shaper, A. G. ABO blood group and ischaemic heart disease in British men. BMJ 300, 1679–1682 (1990).
Wazirali, H., Ashfaque, R. A. & Herzig, J. W. Association of blood group A with increased risk of coronary heart disease in the pakistani population. Pak J Physiol 1, 1–2 (2005).
Yu, B. & Lin, G. A correlation research on Uyghur coronary heart disease patients and ABO blood genetic phenotype. J Xinjiang Med Univ 36, 808–810 (2013).
Gill, J. C., Endres-Brooks, J., Bauer, P. J., Marks, W. J. Jr. & Montgomery, R. R. The effect of ABO blood group on the diagnosis of von Willebrand disease. Blood 69, 1691–1695 (1987).
Dentali, F. et al. Relationship between ABO blood group and hemorrhage: a systematic literature review and meta-analysis. Semin Thromb Hemost 39, 72–82 (2013).
Reilly, M. P. et al. Identification of ADAMTS7 as a novel locus for coronary atherosclerosis and association of ABO with myocardial infarction in the presence of coronary atherosclerosis: two genome-wide association studies. Lancet 377, 383–392 (2011).
Gong, P. et al. [Total cholesterol mediates the effect of ABO blood group on coronary heart disease]. Zhonghua Xin Xue Guan Bing Za Zhi 43, 404–407 (2015).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283, 2008–2012 (2000).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25, 603–605 (2010).
Acknowledgements
This work was partially supported by the National Natural Science Foundation of China (81070171) awarded to Dr. Jian-Jun Li, MD, PhD.
Author information
Authors and Affiliations
Contributions
J.-J.L. and H.X. conceived and designed the review and provided methodological perspectives; Z.C. and S.-H.Y. developed the search strategy and did the literature search, study selection, data extraction, data analyses and interpretation.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chen, Z., Yang, SH., Xu, H. et al. ABO blood group system and the coronary artery disease: an updated systematic review and meta-analysis. Sci Rep 6, 23250 (2016). https://doi.org/10.1038/srep23250
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23250
This article is cited by
-
Blood group AB is associated with reduced blood loss but also elevated cardiovascular mortality in aortocoronary bypass surgery
Journal of Thrombosis and Thrombolysis (2024)
-
Host genetic regulation of human gut microbial structural variation
Nature (2024)
-
High-throughput genetic clustering of type 2 diabetes loci reveals heterogeneous mechanistic pathways of metabolic disease
Diabetologia (2023)
-
ABO and RhD blood group are not associated with mortality and morbidity in critically ill patients; a multicentre observational study of 29 512 patients
BMC Anesthesiology (2022)
-
Association between ABO blood groups and postoperative pain in children after adenotonsillectomy: a prospective cohort study
BMC Anesthesiology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.