Abstract
Post-traumatic orbital reconstruction remains a surgical challenge and requires careful preoperative planning, sound anatomical knowledge and good intraoperative judgment. Computer-assisted technology has the potential to reduce error and subjectivity in the management of these complex injuries. A systematic review of the literature was conducted to explore the emerging role of computer-assisted technologies in post-traumatic orbital reconstruction, in terms of functional and safety outcomes. We searched for articles comparing computer-assisted procedures with conventional surgery and studied outcomes on diplopia, enophthalmos, or procedure-related complications. Six observational studies with 273 orbits at a mean follow-up of 13 months were included. Three out of 4 studies reported significantly fewer patients with residual diplopia in the computer-assisted group, while only 1 of the 5 studies reported better improvement in enophthalmos in the assisted group. Types and incidence of complications were comparable. Study heterogeneities limiting statistical comparison by meta-analysis will be discussed. This review highlights the scarcity of data on computer-assisted technology in orbital reconstruction. The result suggests that computer-assisted technology may offer potential advantage in treating diplopia while its role remains to be confirmed in enophthalmos. Additional well-designed and powered randomized controlled trials are much needed.
Similar content being viewed by others
Introduction
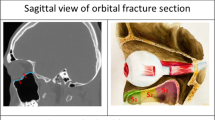
Orbital fractures occur in 40% of all craniomaxillofacial traumas1,2. Patients often present with diplopia or enophthalmos for surgical repair3. Enophthalmos, clinically defined as an inter-ocular difference of more than 2 mm in exophthalmometry, remains a surgical challenge in post-traumatic orbital reconstruction4,5,6,7. Orbital fracture repair includes reducing prolapsed tissues, removing unstable bones and replacing the bony defect with an implant without hindering extraocular motility8.
Computer-assisted technology using computerized tomography (CT) plays an emerging role in orbital reconstruction during preoperative planning, implant design, intraoperative navigation and postoperative auditing. In preoperative planning, a mirror image overlay (MIO) is created based on the uninjured, contralateral orbit and is superimposed onto the images of the injured side9. During computer-aided design and computer-aided modeling (CAD/CAM), the CT data is segmented and digitally transformed to create a three-dimensional model via stereolithography10,11. This is then used to manually mould or manufacture a “patient-specific” implant12,13. Using intra-operative navigation, surgeons obtain real-time coordinates of surgical instruments and implants with respect to the surrounding bony structures.
While there are recommendations and reviews on the indication and timing of surgery3, materials of reconstruction14, the role of endoscopic-assisted repair15, the role of computer-assisted technology in orbital reconstruction has not been defined. To address this, we conducted a systematic review on the use of computer-assisted technology augmented surgery versus conventional surgery in post-traumatic orbital reconstruction to evaluate its functional and safety outcomes.
Methods
Eligibility criteria for considering studies for this review
Studies were included if they:
-
1
Compared computer-assisted technology versus conventional surgery.
-
2
Used computer-assisted technology in the treatment of orbital reconstruction, including but not limited to preoperative planning, surgical navigation, or CAD/CAM implants.
-
3
Included detailed description of the computer-assisted techniques used.
-
4
Performed primary and/or secondary reconstruction of fractured orbital walls.
-
5
Examined at least one of the following outcomes: diplopia, enophthalmos, or procedure-related complications.
Studies were excluded if:
-
1
Computer-assisted technology were only used for diagnostic purposes.
-
2
Orbital reconstruction for non-traumatic (e.g. post tumor removal) cases.
-
3
Outcomes were reported in a qualitative manner.
-
4
Preoperative or postoperative outcome measurements were inadequate.
Search methods for identifying studies
We searched MEDLINE and EMBASE via the OVID platform, Cochrane Central Register of Controlled Trials (CENTRAL), ClinicalTrials.gov (www.clinicaltrials.gov) and World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) for any comparative studies. We used the Cochrane highly sensitive search strategy and combined with our search terms16. The detailed search strategy can be found in the Appendix 1 (supplementary material). We searched the references of the retrieved full-text articles to identify studies not found by our search strategy. We did not apply any language restriction. The final search was performed on February 17, 2015 for all the databases.
Study selection and Data Collection
Two reviewers (KHW and KKLC) independently assessed the titles and abstracts. In case of any unresolved discrepancies, a third reviewer (ALY) will arbitrate until a mutual conclusion was reached. We used a customized form to record the authors, year of publication, sample size, duration of follow up, fracture patterns, primary or secondary reconstruction, the modality of computer-assisted technologies used, surgical techniques, implants and outcome measures. We collected outcome data at the last follow-up. We used reduction in enophthalmos measured by exophthalmometer in millimeter (mm); if these data were not available, then the percentage of patients showing enophthalmos at the last follow-up were analyzed. Likewise, we extracted the percentage of patient complaining of diplopia at the last follow-up. Number and types of complications were recorded.
Risk of Bias Assessment
The quality of the studies was independently evaluated by 2 reviewers (KHW and KKLC) using the Cochrane Risk of Bias tools for RCTs17 and the Newcastle-Ottawa Scale for the observational studies18.
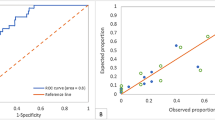
Statistical Analysis
We used the Review Manager (RevMan, version 5.3; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) for our meta-analysis. We analyzed the statistical heterogeneity of the included studies with the Cochrane Q-statistics chi-square test and I2 statistic. If there was any significant heterogeneity between studies (p < 0.1), a random-effect model was used for pooling the data; otherwise a fixed-effect model was used.
Results
We identified 239 titles and abstracts through our literature search and retrieved 12 articles for full text review. We included 6 studies in this systematic review according to our a priori criteria (Fig. 1)19,20,21,22,23,24. The PRISMA checklist and flow diagram can be found in Appendices 2 and 3 (supplementary material).
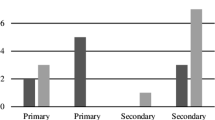
Study Characteristics
Table 1 shows the characteristics of the included trials. We did not identify any randomized controlled trials. Of the identified articles, 4 were prospective cohort studies20,21,22,23. 1 was a historical cohort trial19 and 1 was a retrospective cohort study24. Two studies described isolated orbital floor fracture22,24 while the rest had patients involving multiple or different orbital walls. Patients with secondary orbital reconstructions were examined in 2 studies21,22.
Table 2 summarizes the details of the 6 included studies. Computer-assisted intra-operative surgical navigation was studied in three studies using non-preformed implants of different materials19,20,21; two of which also applied the MIO technique during surgical planning19,20. Preformed CAD/CAM implants using glass-bioceramic or titanium mesh were evaluated in the other 3 studies22,23,24, which none of these studies used intra-operative navigation device.
Quality of Included Studies
Tables 3 and 4 summarize the risk of bias assessment of the included studies. Only 1 study used masked outcome assessor and addressed the confounding factors by matching the study and control group for age, sex, fracture pattern, preoperative ophthalmic features, etiology and severity of trauma, surgical approach and types of implant used20. The control groups were not comparable in two studies leading to potential bias on treatment effect22,24. Intervention bias was minimized in 2 studies by involving only one surgeon19,22. All studies had appropriate length of follow up and accounted for missing data.
Outcome Measures
Tables 5 and 6 summarize the outcomes of the three studies on intraoperative surgical navigation and the other three on individualized preformed CAD/CAM implants group, respectively. Four studies reported on postoperative diplopia19,20,21,24. Three of the 4 studies demonstrated statistically significant improvement of diplopia in the computer-assisted group over the control group (51 vs 60%19, 2 vs 10%20, 17 vs 88%24). Five studies measured changes of enophthalmos20,21,22,23,24. In the computer-assisted group, 3–27% of patients were still enophthalmic at the last follow-up, compared with 10–50% in the control group. A range of 1.5–3.25 mm improvement of enophthalmos was reported in the assisted group, compared to 1.8–3.88 mm in the control group. Four of these five studies concluded there was no difference in improving enophthalmos between the study group and the control group20,21,22,23. Only 1 study reported significantly lower percentage of patients with persistent enophthalmos using preformed CAD/CAM titanium mesh implants as compared to calvarial bone grafts24.
Procedure-related complications were documented in 3 studies19,20,21,22. In one study, extrusion or infection requiring implant removal, entropion, ectropion and epiphora were observed in the group using computer-assisted intra-operative surgical navigation, whereas implant removal, eyelid abscess, retrobulbar hematoma were encountered in the control19. In another study comparing preformed CAD/CAM glass-bioceramic implants implant with non-preformed titanium meshes, 1 case of reduced vision and 2 cases of suspected retrobulbar hematoma versus 2 cases of suspected retrobulbar hematoma were identified, respectively22. One study did not encounter any post-operative complications in either group21. The overall complication rates by individual studies were comparable between both groups.
Discussion
Computer assisted surgery (CAS) (ICD-9-CM Intervention code 00.3) represents surgical concepts and methods utilizing computer technology for preoperative planning and intraoperative guidance. It includes image-guided navigation (IGN) and image-guided surgery (IGS). Such guidance improves accuracy of surgical gestures and reduces surgeon’s action and effort25. This helps to decrease surgical errors and reduce operating time26. Computer-aided design and computer-aided modeling (CAD/CAM) and rapid prototyping (RP) technologies use image-derived data to fabricate custom-made medical guides and implants4. The accuracy of CAS is affected by the resolution of the imaging data set, the precision of the computer algorithm and the accuracy during data registration using superficial bony and surface landmarks27,28. Facial swelling after acute trauma may limit the accuracy of the registration process but can be overcome using a combination of referencing methods29. In patients with unilateral trauma, mirroring the uninjured orbit onto the affected side further improves accuracy9,26. However, MIO assumes perfect symmetry while variations do exist between normal orbits30.
Intra-operative navigation provides real-time feedback of anatomical location of the tracking device with respect to preoperative images25. Locations of and distances to extraocular muscles, infraorbital and optic nerves as well as orbital fissures can be assessed when dissecting through prolapsed orbital soft tissues to minimize iatrogenic injury31. Surgeons can also confirm the location of implant after placement32. Individually or industrially preformed CAD/CAM implants are designed to reproduce the intricate three-dimensional shape of the preinjured orbit for immediate loading. These implants reduce the time for intraoperative manipulation such as bending, trimming and repetitive fittings4 and minimize surgical trauma to periorbital soft tissues4,7.
Quality of Evidence
We did not identify any randomized controlled trials in computer-assisted technology for post-traumatic orbital reconstruction. Results of our systematic review were limited to cohort and case-control studies. Our review highlights the scarcity of relevant literatures. Clinical heterogeneities were present for the severities, location and number of fractures, primary versus secondary reconstruction, timing of surgery and surgical approaches including use of intraoperative navigation, implant types and materials. Methodological heterogeneities due to different type of study designs and operative approaches and clinical heterogeneities due to divergent patient groups limited us from performing meta-analysis.
Efficacy and Safety
Three studies reported the number of patients with clinically significant enophthalmos (difference >2 mm)20,21,24, while 2 studies provided exophthalmometry measurements22,23. We were unable to demonstrate any added benefit in correcting enophthalmos with the use of computer-assisted technologies. In the only study that showed such benefit24, the authors used pre-fabricated titanium implants in the assisted group versus calvarial bone grafts in control24. The main drawbacks of bone graft include difficulty in contouring and variability in resorption27, while titanium mesh are flexible yet rigid and stable over time33,34,35. The differences in implants used may confound the benefit of computer-assisted technologies in improving enophthalmos in this study.
Post-traumatic enophthalmos is not only related to orbital volume expansion but also loss of ligamental support, soft tissue atrophy and contracture36. However, current paradigm of post-traumatic orbital reconstruction focuses on restoring bony orbital volume and shape, which were found to correlate better with postoperative persistent enophthalmos than soft tissue atrophy in the long run37,38,39,31. Yet the latter may explain why anatomical reduction of the orbital fracture alone does not always guarantee long-term symmetry40. Soft tissue changes, if any, may be evaluated by systematically comparing magnetic resonance images (MRI) from both injured and uninjured orbits of surgically and conservatively managed patients41.
Post-traumatic diplopia can be caused by direct nerve or muscle injury causing paralytic strabismus or herniation/entrapment of muscle and/or surrounding connective tissue leading to restrictive strabismus. Our results showed that computer-assisted technology may provide additional improvements in diplopia compared to the conventional surgery. Fewer patients undergoing computer-assisted repair had residual diplopia except those in the study of Lauer et al.21. In that study, the authors used polydioxanone sheets (PDS) implants for 75% and 86% of cases in the assisted and control group respectively. Large orbital defects (>2.5 cm2) were present in 85% in the assisted group and 88% in the control group. However, previous study showed that PDS implant was suitable only for smaller defects (<2.5 cm2)42, thus potentially undermining the beneficial effect of intraoperative navigation21. We postulate that using computer-assisted technology allows more accurate anatomical restoration with better soft tissues repositioning and less implant impingement, leading to better postoperative motility and less diplopia.
Post-operative complications were similar in both groups with no statistical difference. These complications were inherent to the complexities and surgical approaches rather than the use of computer-assisted technologies.
Revisions surgeries are more challenging as scarring occurs over inadequately reduced soft tissues, remaining bone fragments as well as malpositioned implants. Extensive dissection and osteotomies are often necessary and spatial orientation and visualization become more difficult43. Secondary reconstruction is thus one of the strongest indications in using computer-assisted technologies. However, the two studies on secondary reconstruction did not show any additional benefit21,22.
Recommendations for future studies
Existing evidence is deemed insufficient to determine the emerging role of computer-assisted technologies. Future randomized trials will have to address important confounders including size and pattern (e.g. isolated floor versus combined medial wall and floor) of fracture, timing of repair (immediate versus delayed), types of implant and number of surgeons involved. It would also be relevant to study its impact among surgeons-in-training and in revision or complicated cases. Extended follow-up will allow evaluation of soft tissue atrophy, fibrosis and contracture on late-onset diplopia and enophthalmos. Finally, direct and indirect costs should be included in future studies.
Conclusion
To our knowledge, this is the first systematic review on computer-assisted technologies for post-traumatic orbital reconstruction. Results are limited by the paucity of high-quality studies available. Our data suggests advantage in its use for treating diplopia but not enophthalmos. As attractive and innovative as other new technologies, it is not a prerequisite for good outcomes, particularly in simple cases. Despite the potential to reduce error and subjectivity, it is still far from being routinely used due to the incurred time and cost. This review highlights the need of carefully-designed, randomized controlled trials in assessing the indications, safety and efficacy, as well as cost utility of computer-assisted technologies in post-traumatic orbital reconstruction.
Additional Information
How to cite this article: Wan, K. H. et al. The Role of Computer-Assisted Technology in Post-Traumatic Orbital Reconstruction: A PRISMA-driven Systematic Review. Sci. Rep. 5, 17914; doi: 10.1038/srep17914 (2015).
References
Jank S., et al. Clinical signs of orbital wall fractures as a function of anatomic location. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96, 149–153 (2003).
Manolidis S., Weeks B. H., Kirby M., Scarlett M. & Hollier L. Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions. The Journal of craniofacial surgery 13, 726–737; discussion 738 (2002).
Burnstine M. A. Clinical recommendations for repair of isolated orbital floor fractures: An evidence-based analysis. Ophthalmology 109, 1207–1210 (2002).
Metzger M. C. et al. Anatomical 3-dimensional pre-bent titanium implant for orbital floor fractures. Ophthalmology 113, 1863–1868 (2006).
Sargent L. A. & Fulks K. D. Reconstruction of internal orbital fractures with Vitallium mesh. Plast Reconstr Surg 88, 31–38 (1991).
Gellrich N. C. et al. Computer-assisted secondary reconstruction of unilateral posttraumatic orbital deformity. Plast Reconstr Surg 110, 1417–1429 (2002).
Metzger M. C., Schon R., Zizelmann C., Weyer N., Gutwald R. & Schmelzeisen R. Semiautomatic procedure for individual preforming of titanium meshes for orbital fractures. Plast Reconstr Surg 119, 969–976 (2007).
Folkestad L. & Granstrom G. A prospective study of orbital fracture sequelae after change of surgical routines. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 61, 1038–1044 (2003).
Zhang Y., He Y., Zhang Z. Y. & An J. G. Evaluation of the application of computer-aided shape-adapted fabricated titanium mesh for mirroring-reconstructing orbital walls in cases of late post-traumatic enophthalmos. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 68, 2070–2075 (2010).
Bell R. B. Computer planning and intraoperative navigation in cranio-maxillofacial surgery. Oral and maxillofacial surgery clinics of North America 22, 135–156 (2010).
Georgouli T., Pountos I., Chang B. Y. P. & Giannoudis P. V. Prevalence of ocular and orbital injuries in polytrauma patients. Eur J Trauma Emerg Surg 37, 135–140 (2011).
Andrews J. C., Mankovich N. J., Anzai Y. & Lufkin R. B. Stereolithographic model construction from CT for assessment and surgical planning in congenital aural atresia. The American journal of otology 15, 335–339 (1994).
Holck D. E., Boyd E. M., Jr., Ng J. & Mauffray R. O. Benefits of stereolithography in orbital reconstruction. Ophthalmology 106, 1214–1218 (1999).
Gart M. S. & Gosain A. K. Evidence-based medicine: Orbital floor fractures. Plast Reconstr Surg 134, 1345–1355 (2014).
Cheung K., Voineskos S. H., Avram R. & Sommer D. D. A systematic review of the endoscopic management of orbital floor fractures. JAMA Facial Plast Surg 15, 126–130 (2013).
Dreiling D. A. & Soto M. J. The pancreatic involvement in disseminated “collagen” disorders. Studies of pancreatic secretion in patients with scleroderma and Sjogren’s “disease”. Am J Gastroenterol 66, 546–553 (1976).
Chapter 8: Assessing risk of bias in included studies. In Cochrane Handbook of Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011] (ed^(eds Higgins JPT, Altman DG, Sterne JAC). The Cochrane Collaboration, 2011, available from www.cochrane-handbook.org 2011, (Accessed on April 21, 2014).
Wells G. A. et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. (ed^(eds). The Ottawa Health Research Institute, Retrieved from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed on March 14, 2015.
Bly R. A., Chang S. H., Cudejkova M., Liu J. J. & Moe K. S. Computer-guided orbital reconstruction to improve outcomes. JAMA Facial Plast Surg 15, 113–120 (2013).
Cai E. Z. et al. Computer-assisted navigational surgery improves outcomes in orbital reconstructive surgery. Journal of Craniofacial Surgery 23, 1567–1573 (2012).
Lauer G., Pradel W., Schneider M. & Eckelt U. Efficacy of computer-assisted surgery in secondary orbital reconstruction. Journal of Cranio-Maxillofacial Surgery 34, 299–305 (2006).
Nkenke E. et al. Secondary reconstruction of posttraumatic enophthalmos: Prefabricated Implants vs Titanium Mesh. Archives of Facial Plastic Surgery 13, 271–277 (2011).
Scolozzi P., Momjian A. & Heuberger J. Computer-aided volumetric comparison of reconstructed orbits for blow-out fractures with nonpreformed versus 3-dimensionally preformed titanium mesh plates: A preliminary study. Journal of Computer Assisted Tomography 34, 98–104 (2010).
Guo L., Tian W., Feng F., Long J., Li P. & Tang W. Reconstruction of orbital floor fractures: Comparison of individual prefabricated titanium implants and calvarial bone grafts. Ann Plast Surg 63, 624–631 (2009).
Ilankovan V. & Jackson I. T. Experience in the use of calvarial bone grafts in orbital reconstruction. The British journal of oral & maxillofacial surgery 30, 92–96 (1992).
Schmelzeisen R., Gellrich N. C., Schoen R., Gutwald R., Zizelmann C. & Schramm A. Navigation-aided reconstruction of medial orbital wall and floor contour in cranio-maxillofacial reconstruction. Injury 35, 955–962 (2004).
Marmulla R., Hassfeld S., Luth T. & Muhling J. Laser-scan-based navigation in cranio-maxillofacial surgery. J Craniomaxillofac Surg 31, 267–277 (2003).
Marmulla R., Luth T., Muhling J. & Hassfeld S. Automated laser registration in image-guided surgery: evaluation of the correlation between laser scan resolution and navigation accuracy. Int J Oral Maxillofac Surg 33, 642–648 (2004).
Luebbers H. T. et al. Comparison of different registration methods for surgical navigation in cranio-maxillofacial surgery. J Craniomaxillofac Surg 36, 109–116 (2008).
Forbes G., Gehring D. G., Gorman C. A., Brennan M. D. & Jackson I. T. Volume measurements of normal orbital structures by computed tomographic analysis. AJR American journal of roentgenology 145, 149–154 (1985).
Marin P. C., Love T., Carpenter R., Iliff N. T. & Manson P. N. Complications of orbital reconstruction: misplacement of bone grafts within the intramuscular cone. Plast Reconstr Surg 101, 1323–1327 (1998).
Lee H. J., Jilani M., Frohman L. & Baker S. CT of orbital trauma. Emergency radiology 10, 168–172 (2004).
Schlickewei W. & Schlickewei C. The Use of Bone Substitutes in the Treatment of Bone Defects–the Clinical View and History. Macromolecular Symposia 253, 10–23 (2007).
Ellis E., 3rd & Tan Y. Assessment of internal orbital reconstructions for pure blowout fractures: cranial bone grafts versus titanium mesh. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 61, 442–453 (2003).
Kelly C. P., Cohen A. J., Yavuzer R. & Jackson I. T. Cranial bone grafting for orbital reconstruction: is it still the best? The Journal of craniofacial surgery 16, 181–185 (2005).
Clauser L., Galie M., Pagliaro F. & Tieghi R. Posttraumatic enophthalmos: etiology, principles of reconstruction and correction. The Journal of craniofacial surgery 19, 351–359 (2008).
Bite U., Jackson I. T., Forbes G. S. & Gehring D. G. Orbital volume measurements in enophthalmos using three-dimensional CT imaging. Plast Reconstr Surg 75, 502–508 (1985).
Charteris D. G., Chan C. H., Whitehouse R. W. & Noble J. L. Orbital volume measurement in the management of pure blowout fractures of the orbital floor. The British journal of ophthalmology 77, 100–102 (1993).
Whitehouse R. W., Batterbury M., Jackson A. & Noble J. L. Prediction of enophthalmos by computed tomography after ‘blow out’ orbital fracture. The British journal of ophthalmology 78, 618–620 (1994).
Al-Sukhun J. & Lindqvist C. A Comparative Study of 2 Implants Used to Repair Inferior Orbital Wall Bony Defects: Autogenous Bone Graft Versus Bioresorbable Poly-L/DL-Lactide [P(L/DL)LA 70/30] Plate. Journal of Oral and Maxillofacial Surgery 64, 1038–1048 (2006).
Kolk A. et al. Secondary post-traumatic enophthalmos: high-resolution magnetic resonance imaging compared with multislice computed tomography in postoperative orbital volume measurement. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 65, 1926–1934 (2007).
Baumann A., Burggasser G., Gauss N. & Ewers R. Orbital floor reconstruction with an alloplastic resorbable polydioxanone sheet. Int J Oral Maxillofac Surg 31, 367–373 (2002).
Calnan J. The use of inert plastic material in reconstructive surgery. I. A biological test for tissue acceptance. II. Tissue reactions to commonly used materials. British journal of plastic surgery 16, 1–22 (1963).
Author information
Authors and Affiliations
Contributions
K.H.N. and K.K.L.C. contributed equally. K.K.L.C. conceived the study design. K.H.N. and K.K.L.C. acquainted the data. K.H.N. analyzed and interpreted the data. K.H.N. and K.K.L.C. drafted the manuscript. K.H.N., K.K.L.C. and A.L.Y. made the critical revision.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wan, K., Chong, K. & Young, A. The Role of Computer-Assisted Technology in Post-Traumatic Orbital Reconstruction: A PRISMA-driven Systematic Review. Sci Rep 5, 17914 (2015). https://doi.org/10.1038/srep17914
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep17914
This article is cited by
-
Orbital reconstruction: a systematic review and meta-analysis evaluating the role of patient-specific implants
Oral and Maxillofacial Surgery (2022)
-
Development of a core outcome set for amblyopia, strabismus and ocular motility disorders: a review to identify outcome measures
BMC Ophthalmology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.