Abstract
Evidence of associations between psychopathology and obesity in childhood remains inconsistent and most studies have been conducted in Western countries. This study investigated psychological and physiological correlates of obesity in a community sample of children in Taiwan. In total, 302 children (157 overweight/obese and 145 healthy-weight children) were selected from first- and fourth-grade schoolchildren in eight elementary schools in 2009. These children participated in a comprehensive health examination, including a physical examination, blood sample analysis and questionnaire administration. We found that regarding physiological characteristics, compared with the healthy-weight children, the overweight/obese children had significantly higher values for body fat estimated using the bioelectrical impedance method (p < 0.001), systolic blood pressure (p < 0.001) and diastolic blood pressure (p = 0.001); lower values for high-density lipoprotein (p < 0.001); and worse values for glutamic-pyruvic transaminase (p < 0.001), triglycerides (p < 0.001) and fasting blood glucose (p = 0.049). In logistic models adjusted for parental and child traits and physiological characteristics, children’s overweight/obesity was significantly associated with lower self-concept (odds ratio [OR] = 0.96, 95% confidence interval [CI] = 0.93–0.99) and less disruptive behavior (OR = 0.96, 95% CI = 0.92–0.99). Less disruptive behavior and the lack of a higher prevalence of anxiety and depression in childhood obesity appear to be a unique pattern in Taiwan that warrants further investigation.
Similar content being viewed by others
Introduction
Childhood obesity, similar to adulthood obesity, is a major global public health concern because of its wide geographic extent and high prevalence1,2. Obesity underlies a number of the most common illnesses seen in medical practice currently. Overweight and obese children are at a high risk of physiological abnormalities, including cardiovascular disease, metabolic syndrome3, nonalcoholic fatty liver disease, polycystic ovarian syndrome and breathing abnormalities during sleep4. In addition to physical diseases, studies have shown that obese children and young people are prone to develop psychosocial distress, including depression, anxiety and social withdrawal5,6,7 and tend to have a poor quality of life1,8 and behavioral problems9,10,11. However, evidence of associations between psychopathology and obesity in childhood remains inconsistent and psychological and physiological correlates of childhood obesity remain unclear11, with variations according to gender, age and contextual factors (such as familial eating, activity and nutritional patterns and parenting attitudes), as well as race and ethnicity12,13,14,15.
There is a need of further research on psychological problems in obese children, as these problems may be exacerbated over time. A study showed that childhood obesity can be a precursor of adult depression16. Because obese children are much more likely to become obese adolescents and adults unless they maintain healthier patterns of exercise and eating17, a deeper understanding and early effective intervention should be emphasized in younger children. However, most studies have focused on the psychosocial aspects of childhood obesity in older children or adolescents3,18.
Most research on psychological correlates of childhood obesity has been conducted in Western countries. Although a trend of a Westernized lifestyle has been noted in Asia during the past decades, impacts of cultural differences on psychological heterogeneity among obese young people should not be ignored. Consistent with studies in Western countries, recent studies in Asia have demonstrated that obese children exhibit body dissatisfaction and lower self-esteem; however, no relationship was observed between obesity and higher levels of depressive symptoms in children19. Furthermore, the risk of depressive symptoms has been associated with a subjective sense of negative body image and not with the degree of obesity14. A strong relationship between self-perception and behavior may not be observed in Taiwanese children because of the emphasis on the Confucian ideology of filial piety and obedience that pervades Taiwanese culture, in which children are expected to respect and obey their parents and elders instead of expressing their true selves20. This practice may affect the psychological impact of obesity on children. For example, under the pressure of authoritarian parenting, children may be discouraged to use assertive and externalizing behaviors as coping mechanisms20. Furthermore, little research has been conducted on childhood obesity regarding psychological and physiological correlates. In doing this further research, it would be useful to also include further consideration from both a physiological standpoint (e.g., blood pressure, plasma glucose and triglyceride levels, birthweight) and a psychosocial standpoint (e.g., parental smoking, gender)21,22.
Therefore, in this study, we investigated the differences in physiological and psychological dimensions among schoolchildren with healthy and overweight or obese weight statuses in metropolitan Taipei, Taiwan. We hypothesize that compared with healthy-weight children, Taiwanese obese children have poor physiological characteristics (e.g., higher values for systolic blood pressure (SBP), triglycerides (TGs), or fasting blood glucose) and greater psychosocial distress (e.g., lower self-concept and more anxiety or depression). Patterns of association among Taiwanese children may differ from those observed among Western children.
Methods
Participants
In early 2009, a baseline screening was conducted for approximately 3,500 first (aged 6–7 years) and fourth (aged 9–10 years) graders from eight urban elementary schools in metropolitan Taipei, Taiwan. These schools were selected on the basis of their willingness to participate in a health promotion program. Preliminary information on birth date, height, weight and blood pressure were collected. According to the World Health Organization criteria23, children were classified as having a healthy, overweight, or obese weight status depending on their body mass index (BMI) by gender and age.
During the baseline screening in the participating schools, all overweight and obese students were invited to take part in a more comprehensive health examination (a physical examination, blood sample analysis and questionnaire administration) at a hospital. Some healthy-weight students also volunteered for this examination, with a weight status ratio of approximately 1:1. Finally, a total of 302 children (156 overweight or obese children and 145 healthy-weight children) completed the health examination undertaken at Taipei Medical University Hospital.
Measurement of physiological characteristics
At the hospital, the children underwent a physical examination including the measurement of height, weight and blood pressure. Body height and weight were recorded without shoes to the nearest 0.5 cm and 0.1 kg using a combined wall-mounted stadiometer and metric balance scale (NAGATA K-100/P-100), respectively. BMI was calculated using the formula: body weight (kg) divided by height squared (m2). SBP and diastolic blood pressure (DBP) were measured in duplicate on the right arm by trained personnel using an automated sphygmomanometer (TERUMO ES-P2000) after the children had been seated quietly for 5 min prior to the assessments. Body fat was estimated using the bioelectrical impedance method (Omron Body Fat Analyzer HBF-306). Blood samples were also collected from these children after a 12-h overnight fast for measurements of lipid levels, lipoproteins, serum liver enzymes and fasting blood glucose.
Measurement of psychological characteristics
The Beck Youth Inventories, second edition (BYI-II)24, was used to assess the children’s reported thoughts, feelings and behaviors related to emotional and social dysfunction. Each inventory includes 20 questions that measure a child’s experiences in the five psychological domains of self-concept (assessing cognitions of competence, potency and positive self-worth), anxiety (assessing worries about school performance, the future, negative reactions of others and fears), depression (assessing negative thoughts about the self, life and the future and feelings of sadness and guilt), anger (assessing thoughts of being treated unfairly by others and feelings of anger and hatred) and disruptive behavior (assessing thoughts and behaviors associated with conduct disorder and oppositional defiant behavior). Responses were scored using a 4-point Likert scale, with 0 indicating “never” and 3 indicating “always.” Total scores were summed for each inventory. The higher the scores were, the stronger the presentation of a particular psychological domain. In addition, the raw scores were converted (standardized) into T scores (with a mean of 50 and standard deviation of 10) to enable comparing a child’s score with that of other children of the same age.
While high internal consistency was indicated as Cronbach’s α coefficients ranged from 0.86 to 0.96 for all age groups on all scales, good test-retest reliability was reported to range from 0.74 to 0.9325. Validity was supported by correlations with other instruments assessing similar characteristics25. Furthermore, both the reliability and validity were established for the Chinese version of the BYI-II26. All Cronbach’s α coefficients were clearly >0.9 for the five inventories. Specifically for first to fourth graders in their norm group, the Cronbach’s α coefficients ranged from 0.92 to 0.94 for the five inventories. Test-retest reliability ranged from 0.64 to 0.81. Criterion-related validity was also supported for all five inventories.
Finally, parents filled out a questionnaire investigating risk factors for overweight and obesity in children. Questions included the parental BMI status, educational level, smoking status and children’s birth history (i.e., maternal age when carrying the child, a low birthweight (birth weight < 2500 g), preterm birth and cesarean delivery).
This study is a part of an integrated project on child obesity, which was approved by the Ethics Committee of Taipei Medical University Hospital. The methods were conducted in accordance with the approved guidelines. Each child’s parents provided written consent before the children were included in the study. The children’s consent for participation was also obtained.
Data analysis
A Pearson’s χ2 test of significance was used to identify differences in the child, maternal and paternal traits on the basis of the children’s weight status (healthy weight vs. overweight or obese). Psychological and physiological characteristics were separately examined on the basis of the children’s weight status. Specifically, regarding physiological characteristics, age, body fat, SBP, DBP, total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL) and urea were normally distributed and were analyzed using independent-sample t tests. Other parameters, namely aspartate transaminase (AST), alanine aminotransferase (ALT), TGs and fasting blood glucose, were not normally distributed and were analyzed using a Mann–Whitney U-test. Finally, multivariable logistic regression analyses were performed to examine the associations between children’s weight status (response variable) and the parental and child characteristics. The selection of potential confounding variables entered into the regression models was based on the combined data of preliminary analysis and results of previous studies (e.g., parental BMI27, maternal smoking28 and preterm birth29). In model fitting, the child’s sociodemographics and parental traits were considered first and the child’s physiological and psychological characteristics were added separately. All parental and child characteristics were then considered in the final model. The backward stepwise model selection procedure, appropriate for selecting an interpretable model with the most valuable factors30, was used for variable selection. Interaction terms between gender and grade and other physiological and psychological characteristics that did not reach statistical significance were removed from the final analyses. SPSS version 15.0 (SPSS, Chicago, IL, USA) was used for the analysis. All tests of significance were two tailed, with the level of significance set to p < 0.05.
Results
Table 1 shows a comparison of the healthy-weight students with the overweight or obese students in relation to child, maternal and paternal traits. Ethnicity was not specifically assessed in our study, because the Taiwanese population is homogeneous and mainly dominated by the Han race (more than 90%). We found that compared with the healthy-weight children, the overweight or obese children were more likely to be male (p = 0.04). However, no significant differences were observed in the birth history, including maternal age when carrying the child, a low birthweight, preterm birth and cesarean delivery, among children with different weight statuses (all p > 0.05). The overweight or obese children were more likely to have mothers who were overweight or obese (p < 0.01) and smoked (p < 0.01) as well as fathers who were overweight or obese (p < 0.01).
Children’s psychological characteristics according to weight status
The overweight or obese children had significantly lower scores for self-concept and disruptive behaviors compared with the healthy-weight children (self-concept: 49.7 ± 7.3 vs. 51.5 ± 7.5; p = 0.03; disruptive behaviors: 45.9 ± 8.6 vs. 48.1 ± 8.4; p = 0.03) (Table 2). No significant difference was observed in the domains of anxiety, depression and anger between the healthy-weight and overweight or obese children.
Children’s physiological characteristics according to weight status
Compared with the healthy-weight children, the overweight or obese children had significantly higher values for body fat (p < 0.001), SBP (p < 0.001) and DBP (p = 0.001) and significantly lower values for HDL (p < 0.001) (Table 2). The overweight or obese children also had worse ALT (p < 0.001), TG (p < 0.001) and fasting blood glucose (p < 0.05) values.
The relationship between child weight status and psychological/physiological characteristics
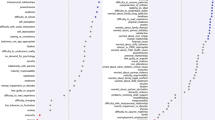
In logistic models including parental and child traits, children’s overweight/obese status was significantly associated with maternal overweight/obesity (odds ratio [OR] = 2.90) and paternal overweight/obesity (OR = 2.20) (Model I, Table 3). The relationship between children’s weight status and their physiological and psychological characteristics was investigated separately. After adjustment for parental and child traits, childhood overweight and obesity were associated with higher levels of body fat, SBP and urea (Model II) and with lower self-concept and less disruptive behavior (Model III). When physiological and psychological characteristics were considered simultaneously, childhood overweight and obesity remained associated with lower self-concept (OR = 0.96) and less disruptive behavior (OR = 0.96) in logistic models adjusted for parental and child traits (Model IV).
Discussion
According to a review of relevant literature, this is the first study to investigate multiple psychological aspects, including self-concept, anxiety, depression, anger and disruptive behavior and obesity-related physiological correlates in school-age children in Taiwan. The major finding was that compared with a healthy-weight status, an overweight or obese status was associated with lower self-concept and less disruptive behavior in children, even after adjustment for parental and child traits. We found no evidence showing that they had more abnormalities in the psychological domains of anxiety, depression and anger.
The construct of self-concept includes the subdomains of self-competence and self-worth and self-worth is likely correlated with self-esteem31. Similar to obese Western children, the obese Taiwanese children had lower self-concept, suggesting no racial differences in the association between low self-esteem and obesity. Previous studies have reported modest associations between obesity and global self-esteem in Chinese and other ethnic groups and body dissatisfaction seems to be associated with lower self-competence13,19,32,33. The inclusion of body image, self-competence, self-satisfaction and attitudes toward others in the scales of self-concept in our measurement26 might partially explain the effect of body dissatisfaction on self-concept. Although the direction of causality between body dissatisfaction and self-esteem remains obscure, obesity may increase the risk of body dissatisfaction, which in turn impairs self-esteem19,34. In addition, the stigma attached to being obese may damage the self-concept of obese children owing to prejudices of healthy-weight children1,10,15,35 and negative parental opinions36. The relationship between obesity and psychological problems was suggested to emerge after children begin regular schooling, when they are at a higher risk of being exposed to attitudes of children and adults outside their families6.
In our community sample in Taiwan, we found that childhood obesity was associated with less disruptive behavior. This seems to be a unique phenomenon that should be further investigated. Studies in Western countries have described an association between obesity and increased likelihood of externalizing behavior in children9,11; however, the magnitude of this association and the starting age of this connection still remain unclear9. In addition, evidence suggested that the impulsivity associated with disruptive behavior in childhood obesity could be related to dopamine dysfunction, poor inhibitory control and reward sensitivity11. However, previous studies have indicated that, in Chinese culture, children are more likely to have an increased capacity to use somatization or internalization as a means of coping37. Confucian ideology strongly pervades Taiwanese culture and its focus on obedience and respect strongly discourages the use of assertive and externalizing behaviors as coping mechanisms20. With the increasing trend of bullying in Taiwan38, obese children may encounter more discrimination owing to social stigmas; therefore, obese ethnic Chinese (i.e., Taiwanese) children may be prone to use somatization rather than present disruptive behaviors. By contrast, a recent study suggested that, in Taiwan, authoritarian parenting styles may affect parental child-feeding practices39. To distract children from their emotional or behavioral problems, Taiwanese parents may use food as a reward or may allow them to engage in sedentary pastimes such as watching television and playing videogames40. Such behavioral management strategies might result in childhood obesity. Therefore, cultural differences may account for the less disruptive behavior in our sample. To verify the association between childhood obesity and disruptive behavior, longitudinal follow-up or additional similar studies should be performed in Chinese and Taiwanese communities.
Previous studies reported an association of obesity with anxiety and depression5,6,7. In our study, although the sample size may be a reason for finding no association between childhood obesity and depression or anxiety, the finding may partially be explained by cultural factors. Western research has revealed that “weight stigma” can emerge in a subtle or overt form, leading to prejudice, discrimination, victimization and devalued social identity, which might mediate the relationship between depression and obesity15. Although stigmatization of childhood obesity appears to be a worldwide public health issue, Chinese culture has traditionally regarded plumpness, particularly in children, as relatively acceptable, healthy, or attractive19,41. In accordance with our findings, studies from Korea have indicated no relationship between obesity and high levels of depressive symptoms in children14,19, suggesting that Asian culture might at least protect children from depression. Regarding biological factors, it was proposed that depression and body fat regulation share genetic factors and have common monoamines and peptides (including serotonin, norepinephrine, dopamine, neuropeptide Y and corticotropin-releasing hormone)11. However, the exact mechanisms underlying the associations between childhood obesity and mood dysregulation remain to be clarified.
As expected and consistent with previous studies3, the overweight or obese children had more physiological abnormalities than did the healthy-weight children, such as abnormal lipids, impaired liver function and higher blood pressure and fasting blood glucose. Obesity is regarded as a chronic, low-grade systemic inflammatory state1. Inflammatory or immune markers might be used in predicting the severity of obesity-related illness42 if future studies of the pathogenesis or pathophysiology of obesity-related inflammation confirm the association between these biomarkers and childhood obesity.
Our study had several limitations. First, the study had a cross-sectional design. Longitudinal follow-up studies are required to clarify causal relationships between childhood obesity and psychological distress. Because our sample was a small subgroup of a much larger population, it is unclear whether the findings can be applied to the general population. Specifically, calculating the sample size in our study would yield statistical powers of 0.65 to 0.95, depending on various physiological and psychological characteristics used among children with healthy and overweight or obese weight statuses. Second, in our study, schools were selected on the basis of their willingness to participate in a health promotion program and they are located in Taipei City, which is one of the five major cities with high health care accessibility in Taiwan. These schools might consider students’ health issues a higher priority, possibly diminishing the differences between the healthy-weight and overweight or obese children. Ethnicity was not specifically assessed in our study, because the Taiwanese population is homogeneous and mainly dominated by the Han race. In addition, because the students were sampled in an urban area, our sample is a limited representation of the entire Taiwanese population.
Third, the rating scale used in this study was self-reported. Measurements of psychological characteristics may be incomplete because of problems with the completeness of reporting and may be subject to socially desirable effects and the participant’s interpretation. In addition, our findings on self-reported psychological characteristics, particularly by first graders, should be interpreted with caution, although researchers have suggested that first graders’ self-report of emotional disturbances, such as anxiety, might have clinical significance on the basis of their findings on the stability, caseness, prevalence and prognostic value of self-reported measures43,44; moreover, the reliability and validity were established for the Chinese version of the BYI-II26. A multi-informant approach may be considered in the future to provide a more accurate description of children’s problems in various contexts, with the simultaneous consideration of difficulties and discordance inherent in various reporters45. Finally, research on childhood obesity and comparison of data among countries may be problematic because of the lack of an internationally accepted measure of obesity3. Therefore, the results should be generalized to other populations with caution.
Conclusions
The key physiological finding of our study is that urban Taiwanese children in the first and fourth grades show signs of weight-related comorbidity even at this young age. Regarding psychological correlates, our findings indicate that childhood obesity is associated with lower self-concept. Less disruptive behavior and the lack of a higher prevalence of anxiety and depression in childhood obesity appear to be a unique pattern, which deserves further consideration. Although emotional and disruptive behaviors might not be a major issue in young overweight and obese children, careful attention should be paid to low self-esteem, consistently observed in our and Western studies, because of its adverse effects on mental health1,5,6,7,8,9,10,11. With increasing trends of obese children in both Western and Eastern countries, it is critical to recognize unfavorable values of certain physiological and psychological characteristics among overweight and obese students as young as 6–7 years and 9–10 years (first and fourth graders, respectively) to promote the physical and mental well-being of children in the current obesogenic environment.
Additional Information
How to cite this article: Chung, K.-H. et al. Psychological and physiological correlates of childhood obesity in Taiwan. Sci. Rep. 5, 17439; doi: 10.1038/srep17439 (2015).
References
Crothers, L. M., Kehle, T. J., Bray, M. A. & Theodore, L. A. Correlates and suspected causes of obesity in children. Psychol. Schools 46, 787–796, doi: 10.1002/pits.20417 (2009).
Kimm, S. Y. & Obarzanek, E. Childhood obesity: a new pandemic of the new millennium. Pediatrics 110, 1003–1007, doi: 10.1542/peds.110.5.1003 (2002).
Lee, W. W. An overview of pediatric obesity. Pediatr. Diabetes 8, Suppl 9, 76–87, doi: 10.1111/j.1399-5448.2007.00337.x (2007).
Daniels, S. R., Jacobson, M. S., McCrindle, B. W., Eckel, R. H. & Sanner, B. M. American Heart Association Childhood Obesity Research Summit Report. Circulation 119, e489–517, doi: 10.1161/CIRCULATIONAHA.109.192216 (2009).
Bell, L. M. et al. Increasing body mass index z-score is continuously associated with complications of overweight in children, even in the healthy weight range. J. Clin. Endocrinol. Metab. 92, 517–522, doi: 10.1210/jc.2006-1714 (2007).
Bradley, R. H. et al. The relationship between body mass index and behavior in children. J. Pediatr. 153, 629–634, doi: 10.1016/j.jpeds.2008.05.026 (2008).
Warschburger, P. The unhappy obese child. Int. J. Obes. (Lond) 29, Suppl 2, S127–129, doi: 10.1038/sj.ijo.0803097 (2005).
Schwimmer, J. B., Burwinkle, T. M. & Varni, J. W. Health-related quality of life of severely obese children and adolescents. JAMA 289, 1813–1819, doi: 10.1001/jama.289.14.1813 (2003).
Anderson, S. E., He, X., Schoppe-Sullivan, S. & Must, A. Externalizing behavior in early childhood and body mass index from age 2 to 12 years: longitudinal analyses of a prospective cohort study. BMC Pediatr 10, 49, doi: 10.1186/1471-2431-10-49 (2010).
Hebebrand, J. & Herpertz-Dahlmann, B. Psychological and psychiatric aspects of pediatric obesity. Child Adol Psych Cl 18, 49–65, doi: 10.1016/j.chc.2008.08.002 (2009).
Puder, J. J. & Munsch, S. Psychological correlates of childhood obesity. Int J Obes (Lond) 34, Suppl 2, S37–43, doi: 10.1038/ijo.2010.238 (2010).
Anderson, S. E. et al. Obesity and depressed mood associations differ by race/ethnicity in adolescent girls. Int. J. Pediatr. Obes. 6(1), 69–78, doi: 10.3109/17477161003728477 (2011).
Griffiths, L. J., Parsons, T. J. & Hill, A. J. Self-esteem and quality of life in obese children and adolescents: a systematic review. Int. J. Pediatr. Obes. 5, 282–304, doi: 10.3109/17477160903473697 (2010).
Kwak, Y. S. et al. Depressive symptoms in elementary school children in Jeju Island, Korea: prevalence and correlates. Eur Child Adolesc Psychiatry 17, 343–351, doi: 10.1007/s00787-008-0675-y (2008).
Puhl, R. M. & Latner, J. D. Stigma, Obesity and the Health of the Nation’s Children. Psychol Bull 133, 557 (2007).
Sanchez-Villegas, A. et al. Childhood and young adult overweight/obesity and incidence of depression in the SUN project. Obesity 18, 1443–1448, doi: 10.1038/oby.2009.375 (2010).
Guo, S. S., Wu, W., Chumlea, W. C. & Roche, A. F. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am. J. Clin. Nutr. 76, 653–658 (2002).
Walker, L. & Hill, A. J. Obesity: The role of child mental health services. Child and Adolesc. Ment. Heal. 14, 114–120, doi: 10.1111/j.1475-3588.2008.00522.x (2009).
Shin, N. Y. & Shin, M. S. Body Dissatisfaction, Self-Esteem and Depression in Obese Korean Children. J. Pediatr. 152, 502, doi: 10.1016/j.jpeds.2007.09.020 (2008).
Chen, J. L., Yeh, C. H. & Kennedy, C. Weight status, self-competence and coping strategies in Chinese children. J. Pediatr. Nurs. 22, 176–185, doi: 10.1016/j.pedn.2006.08.003 (2007).
Chu, N. F. Prevalence and trends of obesity among school children in Taiwan--the Taipei Children Heart Study. Int J Obes Relat Metab Disord 25, 170–176, doi: 10.1038/sj.ijo.0801486 (2001).
Chen, Y. C. et al. Environmental factors associated with overweight and obesity in taiwanese children. Paediatr Perinat Ep 26, 561–571, doi: 10.1111/ppe.12001 (2012).
Chen, W. & Chang, M. H. New growth charts for Taiwanese children and adolescents based on World Health Organization standards and health-related physical fitness. Pediatr Neonatol 51, 69–79, doi: 10.1016/S1875-9572(10)60014-9 (2010).
Beck, A. T. Cognitive therapy and the emotional disorders. Madison: International Universities Press, Inc. (1976).
Beck, J. S., Beck, A. T., Jolly, J. B. & Steer, R. A. Manual for the Beck Youth Inventories (2nd ed.). San Antonio, TX: Harcourt Assessment. (2005).
Cho, S. L., Hung, L. Y., Su, C. L. & Chen, H. C. A research of the Chinese Version Beck Youth Inventories. Psychol. Testing 56, 639–669 (2009).
Davis, M. M., McGonagle, K., Schoeni, R. F. & Stafford, F. Grandparental and parental obesity influences on childhood overweight: implications for primary care practice. J. Am. Board. Fam. Med. 21, 549–554, doi: 10.3122/jabfm.2008.06.070140 (2008).
Suzuki, K. et al. The association between maternal smoking during pregnancy and childhood obesity persists to the age of 9-10 years. J. Epidemiol. 19, 136–142, doi: 10.2188/jea.JE20081012 (2009).
Li, P. et al. Nutritional status and risk factors of overweight and obesity for children aged 9-15 years in Chengdu, Southwest China. BMC Public Health 12, 636, doi: 10.1186/1471-2458-12-636 (2012).
Hair J. F., Black W. C., Babin B. J. & Anderson R. E. Multivariate Data Analysis: A global perspective. Seventh Edition. Person Education, Inc., Upper Saddle River, New Jersey 07458 (2010).
Crocker, J. & Major, B. Social stigma and self-esteem: The self-protective properties of stigma. Psychol Rev. 96, 608–630, doi: 10.1037/0033-295x.96.4.608 (1989).
Sung, R. Y., Yu, C. W., So, R. C., Lam, P. K. & Hau, K. T. Self-perception of physical competences in preadolescent overweight Chinese children. Eur. J. Clin. Nutr. 59, 101–106, doi: 10.1038/sj.ejcn.1602044 (2005).
Young-Hyman, D., Schlundt, D. G., Herman-Wenderoth, L. & Bozylinski, K. Obesity, appearance and psychosocial adaptation in young African American children. J. Pediatr. Psychol. 28, 463, doi: 10.1093/jpepsy/jsg037 (2003).
Paxton, S. J., Neumark-Sztainer, D., Hannan, P. J. & Eisenberg, M. E. Body dissatisfaction prospectively predicts depressive mood and low self-esteem in adolescent girls and boys. J. Clin. Child. Adolesc. Psychol. 35, 539–549, doi: 10.1207/s15374424jccp3504_5 (2006).
Wardle, J. & Cooke, L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 19, 421–440, doi: 10.1016/j.beem.2005.04.006 (2005).
Vander Wal, J. S. & Thelen, M. H. Predictors of body image dissatisfaction in elementary-age school girls. Eat. Behav. 1, 105–122, doi: 10.1016/S1471-0153(00)00011-8 (2000).
Liu, X. et al. Prevalence and risk factors of behavioral and emotional problems among Chinese children aged 6 through 11 years. J. Am. Acad. Child. Adolesc. Psychiatry 38, 708–715, doi: 10.1097/00004583-199906000-00018 (1999).
Cheng, Y. Y., Chen, L. M., Ho, H. C. & Cheng, C. L. Definitions of school bullying in Taiwan: A comparison of multiple perspectives. School Psychol. Int. 32, 227–243, doi: 10.1177/0143034311404130 (2011).
Tung, H. J. & Yeh, M. C. Parenting style and child-feeding behaviour in predicting children’s weight status change in Taiwan. Public Health Nutr. 17, 970–978, doi: 10.1017/S1368980012005502 (2014).
Hsieh, P. L. & FitzGerald, M. Childhood obesity in Taiwan: review of the Taiwanese literature. Nurs. Health Sci. 7, 134–142, doi: 10.1111/j.1442-2018.2005.00218.x (2005).
Lee, S., Ho, T. P. & Hsu, L. K. Fat phobic and non-fat phobic anorexia nervosa: a comparative study of 70 Chinese patients in Hong Kong. Psychol. Med. 23, 999–1017, doi: 10.1017/S0033291700026465 (1993).
Michelson, P. H., Williams, L. W., Benjamin, D. K. & Barnato, A. E. Obesity, inflammation and asthma severity in childhood: Data from the National Health and Nutrition Examination Survey 2001-2004. Ann. of Allergy, Asthma Im. 103, 381–385, doi: 10.1016/s1081-1206(10)60356-0 (2009).
Ialongo, N., Edelsohn, G., Werthamer-Larsson, L., Crockett, L. & Kellam, S. The significance of self-reported anxious symptoms in first-grade children. J Abnorm. Child Psychol. 22, 441–455, doi: 10.1007/BF02168084 (1994).
Ialongo, N., Edelsohn, G., Werthamer-Larsson, L., Crockett, L. & Kellam, S. The significance of self-reported anxious symptoms in first grade children: prediction to anxious symptoms and adaptive functioning in fifth grade. J. Child Psychol. Psychiatry 36, 427–437, doi: 10.1111/j.1469-7610.1995.tb01300.x (1995).
Kraemer, H. C., Measelle, J. R., Ablow, J. C., Essex, M. J., Boyce, W. T. & Kupfer, D. J. A new approach to integrating data from multiple informants in psychiatric assessment and research: mixing and matching contexts and perspectives. Am J Psychiatry 160, 1566–1577, doi: 10.1176/appi.ajp.160.9.1566 (2003).
Acknowledgements
This project was funded by Taipei Medical University Hospital (98TMU-TMUH-01-5 and 99TMU-TMUH-02-4), Taiwan. Without this extremely generous and strong support, this project would not have been possible.
Author information
Authors and Affiliations
Contributions
K.C. managed the literature searches and study design, supervised the field work and wrote the draft. H.C. supervised the study and assisted in study design and result interpretations. Y.C. performed statistical analysis, interpreted statistical results and prepared the manuscript. All authors contributed to and reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chung, KH., Chiou, HY. & Chen, YH. Psychological and physiological correlates of childhood obesity in Taiwan. Sci Rep 5, 17439 (2015). https://doi.org/10.1038/srep17439
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep17439
This article is cited by
-
School-based intervention that integrates nutrition education and supportive healthy school food environment among Malaysian primary school children: a study protocol
BMC Public Health (2019)
-
Investigating the relationship between district-level socioeconomic status and individual obesity in Taiwanese adolescents: A large-scale cross-sectional analysis
Scientific Reports (2019)
-
The Methylation Capacity of Arsenic and Insulin Resistance are Associated with Psychological Characteristics in Children and Adolescents
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.