Abstract
Since reports on the clinical significance of legumain in cancer have shown inconsistent results, we systematically evaluated clinical indicators of legumain in cancer. We searched the Cochrane Library, PubMed, Embase and EBSCO databases and the Wangfang and CNKI databases in China by using “legumain” and (“neoplasms” OR “cancer”) as search terms. We included case-controlled studies of legumain and cancer. The quality of the studies was evaluated by using Lichtenstein’s guidelines and valid data was extracted for analysis. In total, 10 articles were included in this study. Meta-analysis showed that legumain was overexpressed in cancer compared with in normal tissue and was higher in stage III–IV disease than in I–II disease. Moreover, legumain overexpression was correlated with poor prognosis and clinical stage. Furthermore, Cancer Genome Atlas data showed that among patients with rectal cancer, those with tumors overexpressing legumain had shorter overall survival than those in the low expression group (P < 0.05). Legumain appears to be involved in tumor development and deterioration; thus, it can potentially be developed into both a marker for monitoring and diagnosing tumors and a therapeutic target.
Similar content being viewed by others
Introduction
Legumain (LGMN) is a cysteine endopeptidase that belongs to peptidase family C131 and specifically hydrolyzes substrate asparaginyl bonds2 .Legumain was originally found in plants3 ; in mammals, LGMN was first identified in pigs as a 34-kDa glycoprotein2. The gene is widely conserved and is expressed in plants, parasites and mammals, including humans4. In mouse kidneys, LGMN is mainly distributed in the proximal tubule5. Legumain shows the highest expression in lysosomes, but is also expressed in the extracellular environment6. However, in colorectal cancer cell lines, 13–17% of total LGMN is found in the nucleus7. An increasing number of studies have examined legumain, particularly its expression in tumors.
Alginates can accelerate the autocatalytic activation of pro-LGMN at pH 4.0 and 5.08, with their activities increasing upon exposure to doxorubicin and reducing following knock-down of p539. Similarly, intracellular LGMN activity is decreased by internalization of cystatin E/M10. Aza-peptidyl inhibitors containing various non-natural amino acids and different electrophilic active sites can inactivate LGMN11. Legumain can promote cell proliferation independently of endopeptidase activity12. The LGMN promoter is sensitive to nuclear Ca2+, which has been shown to regulate LGMN expression through Elk-1, affecting cell proliferation12.
Little or no LGMN is expressed in normal tissues13, including normal tissues adjacent to tumor tissue4. However, in solid tumors, LGMN is overexpressed in tumors, the matrix and endothelial cells in the tumor microenvironment14. Briggs et al. reported that cystatin E/M can inhibit LGMN activity and the invasive potential of human melanoma cells15. Yoshio et al. reported that LGMN decreases the invasiveness and aggressiveness of prostate cancer16. Additionally, an LGMN DNA vaccine showed a potential protective effect against breast cancer in mice17. The results of studies on the clinical significance of LGMN expression in cancer are contradictory. To clarify the clinical and pathological significance of LGMN in cancer, we conducted a comprehensive meta-analysis of all eligible case-controlled studies. We also used The Cancer Genome Atlas (TCGA) (http://cancergenome.nih.gov/) database to confirm our results.
Results
Characteristics of eligible studies
We searched the Cochrane Library, PubMed, Embase and EBSCO databases and the Wangfang and CNKI databases in China. After reviewing titles and abstracts and analyzing the articles in detail, a total of 10 relevant articles were included in this meta-analysis,6,13,18,19,20,21,22,23,24,25 seven of which were in English13,18,19,21,22,23 and three of which were in Chinese (Table 1)20,24,25. One of the articles compared LGMN expression in ovarian cancer with that in both normal tissues and benign tumors23. Although the definitions of LGMN overexpression (LGMNHigh) varied among the articles, most characterized LGMN expression in ≥25% of neoplastic cells as LGMN overexpression.
Meta-analyses
Cancer tissues vs normal tissues
Five articles compared LGMNHigh in cancer tissue and in normal tissue13,19,20,22,23, including a total of 670 cancer cases (LGMNHigh: 51.9%) and 366 normal tissue samples (LGMNHigh: 13.4%). Since the studies were significantly heterogeneous (P < 0.10, I2 = 87%), we used a random-effect model for pooled analysis, which revealed significant differences between tumor tissues and normal tissues (RR = 3.32, 95% CI: 1.38–7.96, P < 0.05; Fig. 1). We analyzed each of the five articles individually. All five studies reported that LGMNHigh rates in cancer tissue were higher than in normal tissue. However, the sample sources were different and the research methods were not completely consistent, likely leading to heterogeneity (P < 0.10, I2 = 87%). Overall, in our meta-analysis, the LGMNHigh rate in cancer tissue was higher than that in normal tissue.
Good differentiation vs moderate and poor differentiation
Six studies compared LGMN overexpression in well-differentiated (36.9%; 141 cases) and moderate–poorly differentiated (34.8%; 1012 cases) cancers6,18,20,21,22,23. Since the studies were significantly heterogeneous (P < 0.10, I2 = 73%), we used the random-effect model for pooled analysis. The results showed no significant difference between the two groups (RR = 1.02, 95% CI: 0.65–1.61; P > 0.05; Fig. 2). All six articles were included in this research; only two reported a significant difference in LGMNHigh rates between the well-differentiated group and moderate–poorly differentiated groups. One study reported that LGMNHigh rates in the well-differentiated group was lower than in the moderate–poorly differentiated group20. However, the other study showed different results6. The remaining four articles reported no significant difference in LGMNHigh rates between the two groups. Therefore, combined with our meta-analysis, the LGMNHigh rate in the well-differentiated group was similar to that in the moderate–poorly differentiated group.
N0 vs N+
Four articles compared LGMNHigh rates in patients without (N0; 20.0%; 494 cases) and with (N+; 33.8%; 423 cases) lymph node metastases6,13,18,21. Since the studies were significantly heterogeneous (P < 0.10, I2 = 85%), we used the random-effect model for pooled analysis. The results revealed no significant differences between the two groups (RR = 0.66, 95% CI: 0.36–1.20; P > 0.05; Fig. 3). Thus, this analysis showed that the LGMNHigh percentage in the N0 group was similar to that in the N+ group.
Necrosis <10% vs necrosis >10%
Two articles compared the LGMNHigh rates in cancers with <10% necrotic tissue (34.5%; 168 cases) and with >10% necrotic tissue (80.7%; 192 cases)20,22. Since the studies were significantly heterogeneous (P < 0.10, I2 = 97%), we used the random-effect model for pooled analysis, but found no significant difference between the two groups (RR = 0.40, 95% CI: 0.09–1.76; P > 0.05). One study found a significant difference in LGMNHigh rates between the two groups20, but the other study did not22. According to the results of our meta-analysis, the LGMNHigh percentage in the cancer with <10% necrotic tissue group is likely no higher than that in the >10% necrotic tissue group.
Male vs female
Five articles compared LGMNHigh percentages in cancers in male patients (40.0%; 490 cases) and female patients (32.6%; 313 cases)6,13,20,21,25. Since the studies were not significantly heterogeneous (P > 0.10, I2 = 34%), we used the fixed-effect model for pooled analysis and found no significant difference between the two groups (RR = 1.10; 95% CI: 0.91–1.31; P > 0.05). This meta-analysis showed that among patients with cancer, the LGMNHigh rate in men was not higher than in women.
Stage I−II vs stage III −IV disease
Four articles compared LGMNHigh rates in stage I−II disease (28.1%, 334 cases) and stage III −IV disease (47.2%; 309 cases)6,20,21,23. Since the studies were not significantly heterogeneous (P = 0.77, I2 = 0%), we used the fixed-effect model for pooled analysis and found a significant difference between the two groups (RR = 0.67, 95% CI: 0.56–0.82, P < 0.05; Fig. 4), with a higher LGMNHigh rate in the stage III −IV group than in the stage I−II group.
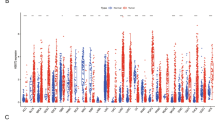
Survival rate
Three articles compared the 5-year survival rates between patients with LGMNHigh expression (51.7%; 298 cases) and those with LGMNLow expression (79.9%; 154 cases)13,19,24. Since the studies were not significantly heterogeneous (P > 0.10, I2 = 0.0%), we used the fixed-effect model for pooled analysis and found a significant difference between the two groups (RR = 0.66; 95% CI: 0.57–0.76; P < 0.05). We collected 61 cases of patients with rectal cancer from the TCGA database. We analyzed the follow-up data and tumor mRNA data (HiSeq RNASeqV2). Kaplan–Meier survival analysis revealed that the LGMNHigh group had significantly shorter survival compared to the LGMNLow group (P < 0.05; Fig. 5).
Sensitivity analysis
Even after eliminating one study for a low-quality grade, LGMN expression was significantly different between cancer tissues and normal tissues. Compared with the random-effect model, fixed-effect model analysis showed P < 0.05 in the N0 vs N+ groups and necrosis <10% vs necrosis >10% groups, indicating unstable results. However, we found no significant differences in the P values in other groups, indicating that the results were stable.
Test of publication bias
In funnel plots of cancer tissue vs normal tissue (Fig. 6), Egger’s test showed P < 0.05 and Begg’s test showed P > 0.05. We considered Begg’s test to be more appropriate because the data was heterogeneous. The plots for well vs moderate–poor differentiation (Fig. 7) and male vs female showed an even and symmetrical distribution (Egger’s and Begg’s tests: P > 0.05 for both), indicating no publication bias.
Discussion
This is the first meta-analysis to examine the association between LGMN and clinicopathological factors of cancer. We included ten studies in this analysis; three studies were in Chinese20,24,25 and two were doctoral theses24,25. One study included patient specimens from a biotechnology company20. Specimens used in the other nine studies were from surgical patients. Patient specimens had been pathology confirmed. We found differences in the sample sources and the research methods were not completely consistent. This may have led to heterogeneity (P ≤ 0.1, I2 ≥ 50%). The scores for two papers were low6,20, mainly because of poor case selection and bias.
Our analysis showed that the LGMNHigh percentages in cancer tissues and normal tissues were significantly different, with values of 51.9% and 13.4% respectively, indicating that LGMN was overexpressed in tumors. Sensitivity analysis confirmed that the results were stable and reliable. The rank correlation test for funnel plot asymmetry showed P > 0.05, indicating no publication bias (Fig. 6). Legumain has been found to be overexpressed in tumor and tumor-associated cells10, mouse kidney tumors26, gastric cancer19,20, ovarian cancer23 and colorectal cancer6,22. Legumain was also found to be overexpressed in adult zebrafish at lesion sites after injury27, suggesting that it was a stress protein. Overexpression of LGMN has also been suggested to affect liver carcinogenesis12. Additional studies are required to determine how legumain promotes tumor cell proliferation.
Our meta-analysis demonstrated that LGMN overexpression was not related to tumor differentiation or to lymph node metastasis. Six studies compared LGMN overexpression in well-differentiated and moderate–poorly differentiated cancers. One study20 reported LGMNHigh rates in well-differentiated tumors were lower than those in moderate–poorly differentiated tumors. However, one study showed different results6. The remaining four studies reported that LGMN overexpression was not related to tumor differentiation. Rong’s25 doctoral thesis also demonstrated that the overexpression of LGMN was not associated with tumor differentiation. Additionally, sensitivity analysis showed that this result was stable. Our analysis also showed that LGMN was not associated with tumor differentiation. Four studies compared LGMNHigh percentages in patients without (N0) and with (N+) lymph node metastases. The results showed no significant difference between the two groups (P > 0.05). However, sensitivity analysis showed significant differences in P values, indicating that this result was not stable.
We found that the LGMNHigh percentages were not significantly different in tumors with <10% necrotic tissue compared to in tumors with >10% necrotic tissue. The LGMNHigh percentages also did not differ based on patient sex, suggesting that LGMN overexpression was not affected by hormones.
Our study also indicated that LGMNHigh percentages were associated with clinical stage, further supporting a possible function for LGMN as a stress protein. Sensitivity analysis confirmed that this conclusion was stable. Other studies have demonstrated an association between LGMN and tumor invasion and metastasis. Li and colleagues reported that LGMN overexpression in tumor tissue was associated with large tumor size (P < 0.01)21, while Guo et al. showed that LGMN overexpression was associated with hepatic metastasis (P = 0.014)19. Cells overexpressing LGMN were found to be more migratory and invasive in vitro4, indicating that LGMN expression affects metastasis and invasion. Legumain can promote cell proliferation12, which may be related to its effect on tumor proliferation. Knock-down of LGMN decreased cell proliferation, but did not appear to promote cell apoptosis. Knock-down of LGMN in a mouse tumor model significantly reduced tumor growth and metastasis28, further supporting LGMN as a potential therapeutic target. Legumain can activate zymogene progelatinase A, which mediates extracellular matrix degradation29, this interaction may affect tumor invasion and metastasis4 .TBX2 is an oncogenic transcription factor that can drive breast cancer proliferation by maintaining LGMN activity30. The mechanism by which LGMN affects cell proliferation requires further study. Patients overexpressing LGMN showed lower 5-year survival rates than did patients with low LGMN expression, which agrees with results of reports correlating LGMN overexpression with poor prognosis in cancer6,13,19,20,22,23,24. TCGA data showed that among patients with rectal cancer, the LGMNHigh group had significantly shorter survival than the LGMNLow group (P < 0.05), further supporting the associations between high legumain expression, tumor progression and poor prognosis.
Our results showed that LGMN was overexpressed in tumor tissues, affected cancer development and deterioration and was associated with poor prognosis in cancer patients. We speculated that LGMN was a stress protein. Our meta-analysis showed that LGMN overexpression percentages were no higher in the N+ group than in the N0 group; however, sensitivity analysis indicated that this conclusion was unstable. Considering that LGMN was involved in tumor development and deterioration, we doubted that LGMN was also associated with lymph node metastasis, as it was an indicator of increased malignancy. We also hypothesized that LGMN was not related to tumor differentiation, tumor tissue necrosis, or patient sex. Our analysis data support these hypotheses. These factors share a common characteristic in that they do not effect tumor progression, suggesting that LGMN’s function in cancer was limited to tumor progression, unless other mechanisms were involved. Additionally, LGMN was not related to patient age, tumor location, or body mass index, as these factors were found to be unrelated to tumor progression.
Legumain is widely conserved, expressed in both plants and animals and has unique distribution characteristics4,6,7,16. Although low expression of LGMN is observed in normal tissue13, it is overexpressed in tumor, matrix and endothelial cells in the tumor microenvironment14. Legumain overexpression in rectal cancer offers both an opportunity and a challenge as a therapeutic target6. Knock-down of LGMN was shown to control tumors28, further supporting that LGMN can be used as a therapeutic target for cancer diagnosis and therapy31. Chen et al. developed an MRI contrast agent and a near-infrared fluorescence probe to monitor LGMN activity in tumors32. Numerous studies have been conducted to develop an LGMN vaccine for tumor treatment17,33,34 . As the target of a multi-peptide vaccine in a breast cancer model, legumain effectively inhibited the tumor load35. We previously developed a drug carrier for tumor treatment based on the attachment of endoprotease to LGMN36. The TBX2–CST6–LGMN signaling pathway may be a target for the development of novel therapies against breast cancer30. U.S. President Barack Obama unveiled a new medical research initiative known as the Precision Medicine Initiative on Jan 30, 201537. Targeting of LGMN should be involved in this initiative.
Conclusion
Our findings indicated that LGMN was overexpressed in cancer and was associated with tumor progression, deterioration and poor prognosis in cancer. Overexpression of LGMN was not associated with tumor differentiation, tumor tissue necrosis, or patient sex. LGMN may be used as a diagnostic marker or therapeutic target.
Methods
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines38.
Study identification and eligibility criteria
We systematically searched the Cochrane Library, PubMed, Embase and EBSCO databases and the Wangfang and CNKI databases in China by using the following search terms: “legumain” and (“neoplasms” [MeSH Terms] or “cancer”). We included studies published up to July 2015 with no language limitations. A study was eligible in the meta-analysis if it: (1) investigated the association between LGMN and cancer; (2) cancer cells were acquired from humans; (3) LGMN was tested by using immunohistochemical methods; (4) provided sufficient data on the relationship between LGMN expression and clinicopathological variables. We excluded studies that (1) had no control groups; (2) used animal models; (3) were case reports, letters, comments, or review articles; (4) did not allow us to extract needed data; (5) did not conduct immunohistochemical method detection of LGMN; (6) included patients who had received chemotherapy or radiotherapy before the study; or (7) included duplicated data. We also downloaded follow-up data and tumor mRNA data (HiSeq RNASeqV2) for patients with rectal cancer from the TCGA database on April 10th, 2015. After eliminating records with incomplete data, we sorted the remaining 61 cases into three groups based on LGMN expression: 21 studies with the highest expression (LGMNHigh), 20 with the lowest expression (LGMNLow) and 20 with moderate expression (moderate expression group) (Supplemental file 1).
Data extraction
For each study, two authors independently extracted the first author, publication year, country, numbers of cases and controls, cancer types, LGMN expression and clinical indicators. Disagreements were resolved by discussion between the two investigators.
Quality score assessment
The quality of the studies was evaluated by the Lichtenstein’s guidelines for case-control studies39. We evaluated quality based on the following aspects to determine whether: (1) the study design was used the scientific method; (2) inclusion criteria and basic structure characteristics of the studies were clear; (3) processing factors and methods were correct; (4) statistical methods were correct; (5) the existence of bias in the research was discussed. Satisfaction of any one of the above 5 aspects earned 1 point. When a study earned three points or more, the quality was considered reliable. Study quality was evaluated by two independent researchers (Zhao Shuangtao and Ye Zhen). Disagreements between the two researchers were resolved through discussion.
Statistical analysis
We used RevMan 5.2 software, provided by the Cochrane Collaboration, to perform the meta-analysis and to merge RR values. Heterogeneity was tested by chi-square analysis. If P ≤ 0.10 for the chi-square test indicated heterogeneity across studies, a fixed-effects model was used for homogeneous data (P > 0.1, I2 < 50%) and a random effects model for significantly different data (P ≤ 0.1, I2 ≥ 50%). Publication bias was evaluated by using a funnel plot if a sufficient number of studies (n > 4) was included. We used the Egger’s and Begg’s tests to evaluate publication bias by using R version 3.1.2 (http://www.r-project.org/). Stability of the data was tested by sensitivity analysis. We eliminated a low-quality document after sensitivity analysis. We also compared the use of the fixed-effect model and random-effect model for sensitivity analysis. We created a Kaplan–Meier survival curve by using the log-rank test for TCGA data to compare the LGMNHigh group with the LGMNLow group. SPSS 22.0 (SPSS, Inc., Chicago, IL, USA) was used for this statistical analysis. P < 0.05 was considered significant.
Additional Information
How to cite this article: Zhen, Y. et al. Clinicopathologic significance of legumain overexpression in cancer: a systematic review and meta-analysis. Sci. Rep. 5, 16599; doi: 10.1038/srep16599 (2015).
References
Barrett, A. & Rawlings, N. Families and clans of cysteine peptidases. Perspectives in Drug Discovery and Design 6, 1–11 (1996).
Chen, J. M. et al. Cloning, isolation and characterization of mammalian legumain, an asparaginyl endopeptidase. Journal of Biological Chemistry 272, 8090–8098 (1997).
Kembhavi, A. A., Buttle, D. J., Knight, C. G. & Barrett, A. J. The two cysteine endopeptidases of legume seeds: purification and characterization by use of specific fluorometric assays. Archives of biochemistry and biophysics 303, 208–213 (1993).
Liu, C., Sun, C., Huang, H., Janda, K. & Edgington, T. Overexpression of legumain in tumors is significant for invasion/metastasis and a candidate enzymatic target for prodrug therapy. Cancer research 63, 2957–2964 (2003).
Yamane, T. et al. Legumain from bovine kidney: its purification, molecular cloning, immunohistochemical localization and degradation of annexin II and vitamin D-binding protein. Biochimica et Biophysica Acta (BBA) - Protein Structure and Molecular Enzymology 1596, 108–120 (2002).
Haugen, M. H. et al. High expression of the cysteine proteinase legumain in colorectal cancer—Implications for therapeutic targeting. European Journal of Cancer 51, 9–17 (2015).
Bogyo, M. et al. Nuclear legumain activity in colorectal cancer. Plos One 8, e52980 (2013).
Berven, L. et al. Alginates induce legumain activity in RAW 264.7 cells and accelerate autoactivation of prolegumain. Bioactive Carbohydrates and Dietary Fibre 2, 30–44 (2013).
Yamane, T. et al. Transcriptional regulation of the legumain gene by p53 in HCT116 cells. Biochemical and Biophysical Research Communications 438, 613–618 (2013).
Smith, R. et al. Intra- and extracellular regulation of activity and processing of legumain by cystatin E/M. Biochimie 94, 2590–2599 (2012).
Lee, J. & Bogyo, M. Synthesis and evaluation of aza-peptidyl inhibitors of the lysosomal asparaginyl endopeptidase, legumain. Bioorganic & Medicinal Chemistry Letters 22, 1340–1343 (2012).
Andrade, V. et al. Nucleoplasmic calcium regulates cell proliferation through legumain. J Hepatol 55, 626–635 (2011).
Wu, M. et al. Legumain protein as a potential predictive biomarker for asian patients with breast carcinoma. Asian Pacific Journal of Cancer Prevention: APJCP 15, 10773–10777 (2014).
Wu, W. et al. Targeting cell-impermeable prodrug activation to tumor microenvironment eradicates multiple drug-resistant neoplasms. Cancer Res. 66, 970–980 (2006).
Briggs, J. J. et al. Cystatin E/M suppresses legumain activity and invasion of human melanoma. BMC Cancer. 10, 17 (2010).
Ohno, Y. et al. Association of legumain expression pattern with prostate cancer invasiveness and aggressiveness. World J Urol 31, 359–364 (2013).
Liu, Z. et al. Alginic acid-coated chitosan nanoparticles loaded with legumain DNA vaccine: effect against breast cancer in mice. Plos One 8, e60190 (2013).
Gawenda, J., Traub, F., Luck, H. J., Kreipe, H. & von Wasielewski, R. Legumain expression as a prognostic factor in breast cancer patients. Breast Cancer Res Tr 102, 1–6 (2007).
Guo, P. et al. Expression of legumain correlates with prognosis and metastasis in gastric carcinoma. Plos One 8, e73090 (2013).
Huaidong, F. Q. L. Q. X. R. S. H. L. Y. H. Prognostic significance of legumain overexpression in gastric cancer patients. J Third Mil Med Univ 36, 232–235 (2014).
Li, N. et al. Effects of legumain as a potential prognostic factor on gastric cancers. Medical oncology (Northwood, London, England) 30, 621 (2013).
Murthy, R. V., Arbman, G., Gao, J., Roodman, G. D. & Sun, X. F. Legumain expression in relation to clinicopathologic and biological variables in colorectal cancer. Clin Cancer Res 11, 2293–2299 (2005).
Wang, L. N. et al. Legumain: A biomarker for diagnosis and prognosis of human ovarian cancer. J Cell Biochem 113, 2679–2686 (2012).
Yuanwei, L. The relationship between legumain expression of human orbital rhabdomyosareoma and tumor invasion. doctorate thesis, Tianjin Medical University, (2010).
Weining, R. Analysis the expression of Legumain in retinoblastoma and its relationwith clinicopathological features and prognosis. doctorate thesis, Tianjin Medical University (2010).
Yamane, T. et al. Knockdown of legumain inhibits cleavage of annexin A2 in the mouse kidney. Biochemical and Biophysical Research Communications 430, 482–487 (2013).
Ma, L. P., Shen, Y. Q., Khatri, H. P. & Schachner, M. The asparaginyl endopeptidase legumain is essential for functional recovery after spinal cord injury in adult Zebrafish. Plos One 9, 12 (2014).
Luo, Y. et al. Targeting tumor-associated macrophages as a novel strategy against breast cancer. J Clin Invest. 116, 2132–2141 (2006).
Chen, J.-M., Fortunato, M., Stevens, R. A. & Barrett, A. J. Activation of progelatinase A by mammalian legumain, a recently discovered cysteine proteinase. Biological Chemistry 382, 777–784 (2001).
D’Costa, Z. C. et al. TBX2 represses CST6 resulting in uncontrolled legumain activity to sustain breast cancer proliferation: a novel cancer-selective target pathway with therapeutic opportunities. Oncotarget 5, 1609–1620 (2014).
Haugen, M. H. et al. Legumain in colorectal cancer: Unorthodox localization and trafficking. Cancer Research 74, 1093–1093 (2014).
Chen, Y.-J. et al. Peptide-based MRI contrast agent and near-infrared fluorescent probe for intratumoral legumain detection. Biomaterials 35, 304–315 (2014).
Lewēn, S. et al. A Legumain-based minigene vaccine targets the tumor stroma and suppresses breast cancer growth and angiogenesis. Cancer Immunology, Immunotherapy 57, 507–515 (2008).
Smahel, M., Duskova M Fau-Polakova, I., Polakova I Fau-Musil, J. & Musil, J. Enhancement of DNA vaccine potency against legumain. J Immunother. 37, 1537–4513 (Electronic) (2014).
Karyampudi, L. et al. Accumulation of memory precursor CD8 T cells in regressing tumors following combination therapy with vaccine and anti-PD-1 antibody. Cancer Research 74, 2974–2985 (2014).
Liu, Z. et al. Legumain protease-activated TAT-liposome cargo for targeting tumours and their microenvironment. Nat. Commun. 5, 11 (2014).
Bogu, Y. Obama unveils details on precision medicine initiative. Xinhua(2015). Available at: http://news.xinhuanet.com/english/world/2015-01/31/c_127442236.htm. (Accessed: 20th July 2015).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6, 1–6 (2009).
Michael, J. & Lichtenstein, C. D. M. a. P. C. E. Guidelines for Reading Case-Control Studies. J Chronic Dis. 40, 893–903 (1987).
Acknowledgements
This work was supported by the National Basic Research Program of China 973 Program (No. 2013CB967201 and the National Natural Science Foundation of China (No. 81273331).
Author information
Authors and Affiliations
Contributions
Y.Z. and X.R. conceived and designed the study. S.W., G.C., W.R., L.X., N.H. and L.D. collected literature and extracted the data. Z.S. and Y.Z. evaluated quality of the studies. Y.Z., T.X. and J.S. performed statistical analysis. Y.Z. and L.Na completed the article writing.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhen, Y., Chunlei, G., Wenzhi, S. et al. Clinicopathologic significance of legumain overexpression in cancer: a systematic review and meta-analysis. Sci Rep 5, 16599 (2015). https://doi.org/10.1038/srep16599
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep16599
This article is cited by
-
Clonorchis sinensis legumain promotes migration and invasion of cholangiocarcinoma cells via regulating tumor-related molecules
Parasites & Vectors (2023)
-
Cleavage of tropomodulin-3 by asparagine endopeptidase promotes cancer malignancy by actin remodeling and SND1/RhoA signaling
Journal of Experimental & Clinical Cancer Research (2022)
-
Proteasome regulation by reversible tyrosine phosphorylation at the membrane
Oncogene (2021)
-
Legumain is an independent predictor for invasive recurrence in breast ductal carcinoma in situ
Modern Pathology (2019)
-
Expression of both poly r(C) binding protein 1 (PCBP1) and miRNA-3978 is suppressed in peritoneal gastric cancer metastasis
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.