Abstract
Phospholipase C epsilon 1 (PLCE1) plays an important role in cell growth, differentiation and oncogenesis. An increasing number of individual studies have investigated the association between PLCE1 rs2274223 polymorphism and cancer risk, but the conclusions are inconclusive. To obtain a comprehensive conclusion, we performed a meta-analysis of 22 studies with 13188 cases and 14666 controls. The pooled results indicated that PLCE1 rs2274223 A > G polymorphism was associated with an increased risk of overall cancer (G vs. A: OR = 1.15, 95% CI = 1.06–1.25; GG vs. AA: OR = 1.30, 95% CI = 1.10–1.55; GA vs. AA: OR = 1.18, 95% CI = 1.08–1.30; GG/GA vs. AA: OR = 1.20, 95% CI = 1.08–1.32; GG vs. GA/AA: OR = 1.22, 95% CI = 1.04–1.42). The stratification analysis showed the polymorphism was significantly associated with an increased risk of esophageal squamous cell carcinoma (ESCC) other than gastric cancer (GC), especially among the subgroups of Asian, high quality score, sample size > 1000 and the studies consistent with Hardy-Weinberg equilibrium (HWE). This meta-analysis demonstrated that PLCE1 rs2274223 A > G polymorphism may be associated with increased susceptibility to cancer, especially for ESCC. However, due to the substantial heterogeneities across the studies, the conclusion might be not conclusive that need more studies to confirm.
Similar content being viewed by others
Introduction
Cancer is a worldwide problem and its incidence is increasing year by year, which severely endangers the human health and lives. In 2008, the world has more than 12 million new cases of cancer and by 2030, this figure will be over 25 million1,2. Until now, the pathogenesis of cancer has not been clarified. A majority of studies suggest it may contribute to the cooperation of environmental factors, genetic susceptibility and acquired susceptibility. And, what is noteworthy is that part of the cancer susceptibility comes from human genome diversity3.
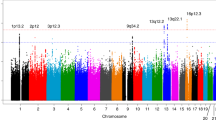
As genome-wide association studies (GWASs) strategy is putting forward, gene mutations or susceptibility loci have been identified for many diseases. To date, more than 50 GWASs focused on cancer have been published, comprising at least 15 different kinds of malignant tumors4. In 2010, Abnet et al firstly performed a GWAS of gastric cancer (GC) and esophageal squamous cell carcinoma (ESCC) in Chinese populations and identified variants located in the PLCE1 gene at chromosome 10q23 had a genome-wide significantly correlation with gastric cardia cancer (GCA) and ESCC5. At the same period, Wang et al also found two susceptibility genes, PLCE1 and C20orf54, were associated with risk of ESCC and GCA for Chinese subjects in another large-scale GWAS6. Later, Wu et al further confirmed seven single nucleotide polymorphisms (SNPs) at five regions significantly associated with ESCC, among which is PLCE1 rs2274223 that has also been found in the former two GWASs7.
Rs2274223, located in the 26th exon of the PLCE1 gene, is a non-synonymous SNP that can cause the amino acid change from histidine to arginine6. Since three related GWASs were completed, SNP rs2274223 in PLCE1 became one of the most studied polymorphic loci. A growing number of studies have been conducted to verify its association with kinds of cancer risk. However, the findings were inconsistent. The discrepancies among these studies might attribute to the relatively small sample size in each research and ethnic variation. Therefore, we performed a meta-analysis of all eligible case-control studies to systematically estimate the effects of PLCE1 rs2274223 A > G polymorphism on the susceptibility to cancer.
Results
Characteristics of eligible publications
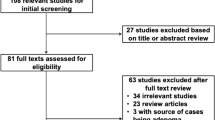
A total of 17 eligible articles were identified in the final meta-analysis, which contained 22 studies and involved 13188 cases and 14666 controls. The study selection process was shown in Figure 18,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24.
Among the 22 studies, six studies reported on GC with 6813 cases and 5666 controls and nine studies reported on ESCC with 3348 cases and 5309 controls. In the rest of the studies, there were two studies on esophageal adenocarcinoma (EAC), two studies on colorectal cancer, one study on head and neck cancer (HNC), one study on squamous cell carcinoma of head and neck (SCCHN) and one study on gallbladder cancer (GBC). All studies follow the Hardy-Weinberg equilibrium (HWE) except three studies which derived from Palmer's article15. In addition, there were eight studies for Caucasian population, 12 studies for Chinese population, one study for African population and one study for mixed population. The main characteristics of those studies are listed in Table 1.
Results of meta-analysis
The associations of PLCE1 rs2274223 polymorphism with the risk of different types of cancer were shown in Table 2, Figure 2. Overall, statistically significant associations were observed among all of the genetic models (G vs. A: OR = 1.15, 95% CI = 1.06–1.25; GG vs. AA: OR = 1.30, 95% CI = 1.10–1.55; GA vs. AA: OR = 1.18, 95% CI = 1.08–1.30; GG/GA vs. AA: OR = 1.20, 95% CI = 1.08–1.32; GG vs. GA/AA: OR = 1.22, 95% CI = 1.04–1.42). Further analysis showed the polymorphism was significantly associated with an increased risk of ESCC other than GC in all genetic models, among which the most obvious is for homozygous model (GG vs. AA: OR = 1.55, 95% CI = 1.17–2.06) and weakest for heterozygous model (GA vs. AA: OR = 1.27, 95% CI = 1.09–1.47).
In GC, stratification analysis by genotyping methods showed that rs2274223 was significantly associated with the risk of GC using TaqMan (G vs. A: OR = 1.20, 95% CI = 1.04–1.39; GA vs. AA: OR = 1.27, 95% CI = 1.12–1.44; GG/GA vs. AA: OR = 1.28, 95% CI = 1.10–1.49). No significant association was detected in the subgroup analysis by ethnicity, source of control, sample size and HWE in controls (Table 3).
In ESCC, significantly increased ESCC risk was only discovered for Asian subgroup (G vs. A: OR = 1.44, 95% CI = 1.25–1.66; GG vs. AA: OR = 2.04, 95% CI = 1.47–2.85; GA vs. AA: OR = 1.39, 95% CI = 1.24–1.56; GG/GA vs. AA: OR = 1.49, 95% CI = 1.29–1.72; GG vs. GA/AA: OR = 1.76, 95% CI = 1.31–2.36), but not for Caucasians and other ethnicities. In the stratified analysis by source of control, significant association was only found for hospital-based controls (G vs. A: OR = 1.29, 95% CI = 1.19–1.41; GG vs. AA: OR = 1.61, 95% CI = 1.29–2.03; GA vs. AA: OR = 1.33, 95% CI = 1.18–1.49; GG/GA vs. AA: OR = 1.37, 95% CI = 1.23–1.53; GG vs. GA/AA: OR = 1.42, 95% CI = 1.13–1.77). When stratified by sample size, we observed a significantly increased risk of ESCC in large sample size whose number was more than 1000 (G vs. A: OR = 1.20, 95% CI = 1.09–1.32; GG vs. AA: OR = 1.34, 95% CI = 1.10–1.64; GA vs. AA: OR = 1.26, 95% CI = 1.12–1.41; GG/GA vs. AA: OR = 1.28, 95% CI = 1.14–1.43). We also performed stratification analysis by quality score, significant association was only identified in high score (G vs. A: OR = 1.22, 95% CI = 1.05–1.41; GG vs. AA: OR = 1.46, 95% CI = 1.10–1.93; GA vs. AA: OR = 1.25, 95% CI = 1.06–1.47; GG/GA vs. AA: OR = 1.27, 95% CI = 1.06–1.52; GG vs. GA/AA: OR = 1.32, 95% CI = 1.05–1.65). Furthermore, in the stratified analysis by HWE in controls, we found a significant increased association between PLCE1 rs2274223 polymorphism and ESCC risk in the studies consistent with HWE (G vs. A: OR = 1.29, 95% CI = 1.13–1.47; GG vs. AA: OR = 1.62, 95% CI = 1.21–2.15; GA vs. AA: OR = 1.32, 95% CI = 1.19–1.46; GG/GA vs. AA: OR = 1.37, 95% CI = 1.20–1.56; GG vs. GA/AA: OR = 1.42, 95% CI = 1.10–1.83) (Table 3).
Heterogeneity and sensitivity analysis
We observed substantial heterogeneities among all investigations (GG vs. AA: P = 0.000; GA vs. AA: P = 0.000; GG/GA vs. AA: P = 0.000; GG vs. GA/AA: and G vs. A: P = 0.001) (Table 2). The meta-regression analysis yielded no significant difference between subgroup analysis (Supplemental Table 1). We further conducted sensitivity analyses to estimate the influence of each individual data on the combined ORs and no significant differences were observed in all genetic models (Supplemental Figure 1).
Publication bias
We performed Begg's funnel plot and Egger's test to assess the publication bias. The shape of the Begg's funnel plot showed basically symmetric distribution. The results of Egger's test were as follows: G vs. A: t = −0.20, P = 0.846; GG vs. AA: t = −0.55, P = 0.586; GA vs. AA: t = 0.22, P = 0.831; GG/GA vs. AA: t = −0.02, P = 0.983 and GG vs. GA/AA: t = −0.56, P = 0.580, which further provided no evidence of publication bias (Figure 3).
Discussion
In the meta-analysis, we comprehensively evaluate the association between PLCE1 rs2274223 polymorphism and cancer risk through 22 studies with 13188 cases and 14666 controls. We observed the genetic variation significantly increased the risk of overall cancer, especially for ESCC. We also found the associations existed in the subgroups of Asian ethnicity, sample size > 1000, high quality score and the studies consistent with HWE in ESCC.
The PLCE1 gene is located on chromosome 10q23, encoding PLCE1 protein which is a member of phosphoinositide-specific phospholipase C (PLC). PLCE1 protein, like other PLC families, is composed of the PLC catalytic domain, PH domain, EF domain and C2 domain. In addition, PLCE1 protein also has unique regions, two RA domains at its C terminus and a CDC25-like domain at its N terminus. Especially, the former directly interact with several Ras family GTPases, such as oncogenic KRas and HRas. Therefore, PLCE1, as a multifunctional signaling protein, plays an important role in cell growth, differentiation and oncogenesis25,26,27. Simultaneously, an increasing amount of studies start to investigate the association of PLCE1 rs2274223 polymorphism on the susceptibility of different cancer.
To our knowledge, PLCE1 mutation is closely associated with many diseases, such as nephrotic syndrome28 and cardiac hypertrophy29. Although the PLCE1 rs2274223 polymorphism is associated with a high risk of cancers, the exact mechanism is still unknown. Some studies suggest that PLCE1 protein plays a crucial role in the process of information transmission between the cell membrane and the nucleus. And it probably through augmenting angiogenesis and inflammation, two distinct mechanisms, acts on intestinal tumorigenesis30,31. Furthermore, the research of gene-gene, gene-environmental interactions may provide some important information. However, the Song's study32 indicated that smoking, drinking and Body Mass Index (BMI) did not significantly change the effect of rs2274223 polymorphism in Chinese population.
Two previously meta-analyses33,34 have investigated the association between PLCE1 rs2274223 and different kinds of cancer. Both of them demonstrated that the polymorphism increased the risk of cancer in the pooling analysis, which was the same with ours. In the stratification analysis, the former publication33 showed that PLCE1 rs2274223 polymorphism contributed to the high risk of esophageal and gastric cancer in Asians. However, in the present study, we observed an increased association in Asian ethnicity only for ESCC other than GC. The discrepancy may result from three reasons as the follows: First of all, we classified esophageal cancer into ESCC and EAC for the reason that genetic variation may have different effect on different pathological type of cancer. Because of a limited number of published studies for EAC, we failed to perform further stratification analysis. Therefore, the association between the PLCE1 rs2274223 polymorphism and EAC risk was ambiguous. Secondly, the positive result about GC might be attributed to small sample size, when we increased the number more than half, we failed to find the significant association. Moreover, the former study mistakenly put the northern Indian population into Asians which may make the result bias. The latter study34 identified PLCE1 rs2274223 polymorphism was associated with the risk of upper aerodigestive tract cancer (ESCC, EC, HNC and SCCHN) but not with gastric and colorectal cancer. However, we did not combine the HNC, SCCHN, EAC and colorectal cancer, because it might be more appropriate to show the results without meta-analysis when the number of studies was less than three.
Compared with the previous publications, our meta-analysis has advantages. Above all, this is by far an analysis with the largest sample size which provided a power of above of 80% investigating the association. What is more, among all the included studies, 95.45% (21/22) were considered as high quality. Furthermore, sensitivity analysis revealed no significant influence of a single study on the summary ORs or the 95% CI. Additionally, no obvious evidence of publication bias existed, which indicated that the result may be unbiased. Some studies have discovered some sequence variants in the region of chromosome, such as 5p15.33 and 8q24, are associated with risk of different cancer types35,36,37,38,39, so we speculated that rs2274223 may be the specific site associated with different cancer types. However, in the further subgroup analyses, we found rs2274223 significantly associated with an increased risk of ESCC rather than GC which suggested it has no non-specific effect on different types of cancer. So, it appropriate or not to calculate the association of genetic variation with the risk of cancer by pooling the data from different type of cancer remains open to question although researchers have always done this way. Additionally, further functional studies should be carried out to explore the mechanism underlying the variant-related associations with cancer risk.
There was substantial between-study heterogeneity in the meta-analysis. So, although the statistical evidence proved the findings to be reliable, we did not deem lightly of the issue. We used random-effects model to incorporate heterogeneity among studies. However, random-effects model is not a substitute for a thorough investigation of heterogeneity. In addition, we performed the analysis with strict criteria for study inclusion, carried out meta-regression but found no source of heterogeneities. However, further stratification analysis demonstrated that cancer type, source of control and sample size may be the main source of heterogeneities. Besides, there is other heterogeneity that cannot be explained.
Some other limitations should be acknowledged. Firstly, although we had enrolled 22 studies, the sample size for certain cancer types and ethnicities remained relatively small that we could not perform further subgroup analyses. Secondly, we failed to conduct the adjusted estimates for unavailable original data, such as age, sex, smoking and drinking status et al which could make the result masked. Thirdly, some studies are hospital-based design which would not represent the people who live in a certain region. Lastly, even though there is no statistical evidence of publication bias, we may miss some unpublished investigations showing no significant effect or publications written in other languages. Additionally, the power of the funnel plot to test the asymmetry is relatively low when studies were less than 30 or smaller studies were lower methodological quality. What is more, most of the data are retrospective in the meta-analysis. Therefore, reporting publication bias from prospective studies is needed.
In conclusion, the meta-analysis suggests that PLCE1 rs2274223 polymorphism may be associated with increased susceptibility to cancer, especially for ESCC. However, due to the limitations of the meta-analysis, the conclusion might be not conclusive which need more studies with larger sample size and appropriate design to confirm.
Methods
Publication searching
We identified publications from PubMed and The New England Journal of Medicine (OVID platform) using the following search items: “PLCE1” or “Phospholipase C epsilon 1” “SNP” or “polymorphism” or "variant" and “cancer” or "carcinoma" or "neoplasm" or "malignance". We also identified related publications written in Chinese from China National Knowledge Infrastructure (CNKI) and WanFang database using the combinations terms of “PLCE1” or “Phospholipase C epsilon 1” “SNP” or “polymorphism” or "variant" and “cancer” or "carcinoma" in Chinese. The languages were limited to English and Chinese. We further screened the whole references with the date up to April 2014 and confirmed potential relevant studies according to the title and abstract.
Selection criteria
All studies included in the meta-analysis are accorded with the following inclusion criteria: (a). Full text available; (b). Study focus on the association of PLCE1 rs2274223 polymorphism and cancer susceptibility; (c). Case-control studies; (d). Genotype data available. In addition, exclusion criteria were as follows: (a). Overlapped articles or repeated studies; (b). Review articles, dissertations and conference reports.
Data extraction
Two researchers independently extracted data from each eligible study with the following items: the first author, year of publication, the type of cancer, country, ethnicity, source of controls, genotyping technology, number of cases and controls, the quantity of each genotype in cases and controls, Minor Allele Frequency (MAF) and value of HWE. In order to ensure the accuracy of the data, when encountering inconsistent, we discussed together to reach a consensus.
Quality assessment
According to the quality assessment criteria (Supplemental Table 2), we assessed the quality of each study. Quality scores of studies ranged from 0 (lowest) to 15 (highest). Studies which scores less than 9 were categorized into low quality, while those scores equal to or greater than 9 were regarded as high quality40.
Data analysis
STATA software (version 11.0; Stata Corporation, College Station, TX) was used to perform all analyses. We used allelic (G vs. A), homozygote (GG vs. AA), heterozygote (GA vs. AA), dominant (GG/GA vs. AA) and recessive (GG vs. GA/AA) as the models. The genetic association between the PLCE1 rs2274223 polymorphism and the risk of cancer was evaluated by the pooled odds ratios (OR) and 95% confidence interval (CI). If the P value of the Z test was less than 0.05, we considered the pooled OR statistically significant. Heterogeneity was analyzed using the Chi-squared-based Q-test. When there existed significant heterogeneity (P < 0.10), the random-effects model was used41. Otherwise, the fixed effects model was used42. Stratification and meta-regression analyses were conducted to explore the potential source of heterogeneity across studies. We also performed stratified analyses by cancer type (ESCC and GC), ethnicity (Asian and Caucasian), control source (hospital-based and population-based), quality score of studies (low and high), sample size (>1000 and ≤1000), Genotyping methods (TaqMan and others) and HWE. Sensitivity analyses were performed to measure the stability of the results when one study was removed and the influence of the independent study on the pooled OR at the same time. Publication bias among the literatures was evaluated by Begg's funnel plot and Egger's test (P < 0.05 was considered significant)43,44.
References
Vineis, P. & Wild, C. P. Global cancer patterns: causes and prevention. The Lancet 383, 549–557 (2014).
Are, C. et al. A review of global cancer burden: trends, challenges, strategies and a role for surgeons. J Surg Oncol 107, 221–226 (2013).
Wang, L. & Chen, S. J. Environment, Genome and Cancer. Yi Chuan 23, 269–275 (2001).
Stadler, Z. K. et al. Genome-wide association studies of cancer. J Clin Oncol 28, 4255–4267 (2010).
Abnet, C. C. et al. A shared susceptibility locus in PLCE1 at 10q23 for gastric adenocarcinoma and esophageal squamous cell carcinoma. Nat Genet 42, 764–767 (2010).
Wang, L. D. et al. Genome-wide association study of esophageal squamous cell carcinoma in Chinese subjects identifies susceptibility loci at PLCE1 and C20orf54. Nat Genet 42, 759–763 (2010).
Wu, C. et al. Genome-wide association study identifies three new susceptibility loci for esophageal squamous-cell carcinoma in Chinese populations. Nat Genet 43, 679–684 (2011).
Ma, H., Wang, L. E., Liu, Z., Sturgis, E. M. & Wei, Q. Association between novel PLCE1 variants identified in published esophageal cancer genome-wide association studies and risk of squamous cell carcinoma of the head and neck. BMC cancer 11, 258–258 (2011).
Zhang, H. et al. Genetic variants at 1q22 and 10q23 reproducibly associated with gastric cancer susceptibility in a Chinese population. Carcinogenesis 32, 848–852 (2011).
Bye, H. et al. Distinct genetic association at the PLCE1 locus with oesophageal squamous cell carcinoma in the South African population. Carcinogenesis 33, 2155–2161 (2012).
Gu, H. et al. Replication study of PLCE1 and C20orf54 polymorphism and risk of esophageal cancer in a Chinese population. Mol Biol Rep 39, 9105–9111 (2012).
Hu, H. et al. Putatively functional PLCE1 variants and susceptibility to esophageal squamous cell carcinoma (ESCC): a case-control study in eastern Chinese populations. Ann Surg Oncol 19, 2403–2410 (2012).
Li, F. X. et al. Association of 10q23 with colorectal cancer in a Chinese population. Mol Biol Rep 39, 9557–9562 (2012).
Yang, X.-X. et al. Association of Genetic Polymorphisms at 1q22 but not 10q23 with Gastric Cancer in a Southern Chinese Population. Asian Pac J Cancer Prev 13, 2519–2522 (2012).
Palmer, A. J. et al. Genetic variation in C20orf54, PLCE1 and MUC1 and the risk of upper gastrointestinal cancers in Caucasian populations. Eur J Cancer Prev 21, 541–544 (2012).
Wang, M. et al. Potentially functional variants of PLCE1 identified by GWASs contribute to gastric adenocarcinoma susceptibility in an eastern Chinese population. PloS one 7, e31932–e31932 (2012).
Zhou, R. M. et al. PLC-epsilon1 gene polymorphisms significantly enhance the risk of esophageal squamous cell carcinoma in individuals with a family history of upper gastrointestinal cancers. Arch Med Res 43, 578–584 (2012).
Dura, P. et al. GWAS-uncovered SNPs in PLCE1 and RFT2 genes are not implicated in Dutch esophageal adenocarcinoma and squamous cell carcinoma etiology. Eur J Cancer 22, 417–419 (2013).
Duan, F. et al. Novel functional variants locus in PLCE1 and susceptibility to esophageal squamous cell carcinoma: based on published genome-wide association studies in a central Chinese population. Cancer Epidemiol 37, 647–652 (2013).
Yuan, Z. et al. Genetic variants at 10q23 are associated with risk of head and neck cancer in a Chinese population. Oral Oncol 49, 332–335 (2013).
Sharma, K. L. et al. Association of potentially functional genetic variants of PLCE1 with gallbladder cancer susceptibility in north Indian population. J Gastrointest Cancer 44, 436–443 (2013).
Chen, Y. Z. et al. Relationship between rs2274223 and rs3765524 polymorphisms of PLCE1 and risk of esophageal squamous cell carcinoma in a Kazakh Chinese population. Zhonghua Bing Li Xue Za Zhi 42, 795–800 (2013).
Wang, Q., Chen, P., Chen, D., Liu, F. & Pan, W. Association between phospholipase C epsilon gene (PLCE1) polymorphism and colorectal cancer risk in a Chinese population. J Int Med Res 42, 270–281 (2014).
Song, H. R. et al. Common genetic variants at 1q22 and 10q23 and gastric cancer susceptibility in a Korean population. Tumour Biol 35, 3133–3137 (2014).
Wing, M. R., Bourdon, D. M. & Harden, T. K. PLC-epsilon: a shared effector protein in Ras-, Rho- and G alpha beta gamma-mediated signaling. Mol Interv 3, 273–280 (2003).
Bunney, T. D. et al. Structural and mechanistic insights into ras association domains of phospholipase C epsilon. Mol Cell 21, 495–507 (2006).
Bunney, T. D. & Katan, M. Phospholipase C epsilon: linking second messengers and small GTPases. Trends Cell Biol 16, 640–648 (2006).
Jefferson, J. A. & Shankland, S. J. Familial nephrotic syndrome: PLCE1 enters the fray. Nephrol Dial Transplant 22, 1849–1852 (2007).
Wang, H. et al. Phospholipase C epsilon modulates beta-adrenergic receptor-dependent cardiac contraction and inhibits cardiac hypertrophy. Circ Res 97, 1305–1313 (2005).
Harden, T. K. & Sondek, J. Regulation of phospholipase C isozymes by ras superfamily GTPases. Annu Rev Pharmacol Toxicol 46, 355–379 (2006).
Li, M., Edamatsu, H., Kitazawa, R., Kitazawa, S. & Kataoka, T. Phospholipase Cepsilon promotes intestinal tumorigenesis of Apc(Min/+) mice through augmentation of inflammation and angiogenesis. Carcinogenesis 30, 1424–1432 (2009).
Song, X. et al. Correlation of PLCE1 gene polymorphism in the smokers/non-smokers, drinking/non-drinking and BMI subgroups with esophageal squamous cell carcinoma. Journal of Henan Medical University 31, 186–202 (2012).
Umar, M., Upadhyay, R. & Mittal, B. PLCE1 rs2274223 A > G polymorphism and cancer risk: a meta-analysis. Tumour Biol 34, 3537–3544 (2013).
Zhang, Y. et al. Meta-analysis of phospholipase C epsilon 1 polymorphism and cancer risk. Cancer Biomark 13, 483–489 (2013).
Gudmundsson, J. et al. Genome-wide association study identifies a second prostate cancer susceptibility variant at 8q24. Nat Genet 39, 631–637 (2007).
Yeager, M. et al. Genome-wide association study of prostate cancer identifies a second risk locus at 8q24. Nat Genet 39, 645–649 (2007).
Haiman, C. A. et al. Multiple regions within 8q24 independently affect risk for prostate cancer. Nat Genet. 39, 638–644 (2007).
Tomlinson, I. et al. A genome-wide association scan of tag SNPs identifies a susceptibility variant for colorectal cancer at 8q24.21. Nat Genet 39, 984–988 (2007).
Kiemeney, L. A. et al. Sequence variant on 8q24 confers susceptibility to urinary bladder cancer. Nat Genet. 40, 1307–1312 (2008).
Thakkinstian, A. et al. Systematic review and meta-analysis of the association between complement component 3 and age-related macular degeneration: a HuGE review and meta-analysis. Am J Epidemiol 173, 1365–79 (2011).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–88 (1986).
Mantel, N. & Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22, 719–48 (1959).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. .Biometrics 50, 1088–101 (1994).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–34 (1997).
Author information
Authors and Affiliations
Contributions
L.Z.L. and J.H. conceived and designed this study; Y.W.W., M.L.Z. and W.J.X. searched databases and collected the data; W.J.X. and M.L.Z. performed the statistical analysis, interpretation of data and wrote the manuscript. All authors reviewed the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xue, W., Zhu, M., Wang, Y. et al. Association between PLCE1 rs2274223 A > G polymorphism and cancer risk: proof from a meta-analysis. Sci Rep 5, 7986 (2015). https://doi.org/10.1038/srep07986
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07986
This article is cited by
-
An Association and Meta-Analysis of Esophageal Squamous Cell Carcinoma Risk Associated with PLCE1 rs2274223, C20orf54 rs13042395 and RUNX1 rs2014300 Polymorphisms
Pathology & Oncology Research (2020)
-
Genetic association between NFKB1 −94 ins/del ATTG Promoter Polymorphism and cancer risk: a meta-analysis of 42 case-control studies
Scientific Reports (2016)
-
Genetic Variations in Phospholipase C-epsilon 1 (PLCE1) and Susceptibility to Colorectal Cancer Risk
Biochemical Genetics (2016)
-
Evaluation of GWAS-identified SNPs at 6p22 with neuroblastoma susceptibility in a Chinese population
Tumor Biology (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.