Abstract
Introduction:
Transcranial motor evoked potential (TcMEP) monitoring is the gold standard for intra-operative neurological monitoring (IOM) of motor pathways during complex spine surgery because of its high sensitivity and specificity. However, although it is very low, the rate of false-negatives in TcMEP monitoring is not zero. Therefore, over-reliance on TcMEP monitoring can cause potentially preventable motor deficits.
Case presentation:
We report a case of motor deficits due to nerve root stretch after surgical correction of a congenital lumbar kyphoscoliosis in a 56-year-old woman. TcMEPs did not show any significant changes during surgery, whereas free-run electromyography (EMG) demonstrated a long-lasting train activity in the left quadriceps femoris muscle (QF) after correction at the osteotomy area. According to the normal findings on TcMEP monitoring, we did not release the correction. Postoperatively, a significant decrease (grade 2-) in the manual muscle test for the left QF and iliopsoas muscle and hypesthesia of the left anterior thigh was revealed. Fortunately, muscle strength was fully recovered without revision surgery at 6 months postoperatively; however, numbness in the left anterior thigh persisted at 2 years after surgery.
Discussion:
Our report suggests that the possibility of false-negative TcMEPs should be kept in mind, especially during surgery with a risk of nerve root injury. When abnormal findings in the free-run EMG, including long-lasting train activity, are observed, surgeons should consider performing appropriate responses, such as the release of the correction, even when no substantial changes are seen in the TcMEPs.
Similar content being viewed by others
Introduction
To enhance safety during complex spine surgery, such as that for spinal deformity, intra-operative neurologic monitoring (IOM) is typically performed, including transcranial motor evoked potential (TcMEP) monitoring, somatosensory evoked potential (SSEP) monitoring and free-run or triggered electromyography (EMG). Of these technologies, TcMEP monitoring is regarded as the gold standard for monitoring the intra-operative neurologic status of the motor pathway.1 However, because the rate of false-negatives in TcMEP monitoring is not zero, an over-reliance on TcMEP monitoring can cause potentially preventable motor deficits.
Herein, we present a case involving an adult patient who underwent deformity correction surgery for congenital lumbar kyphoscoliosis, during which IOM demonstrated false-negative TcMEPs accompanied by a true-positive free-run EMG.
Case presentation
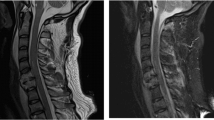
A 56-year-old woman with hemivertebrae of L4 and L5 presented with severe kyphoscoliosis (Figure 1). The pre-operative standing radiographs demonstrated an 83° thoracolumbar curve (T10-L4) and 56° lumbar kyphosis (L1-S1). No neurologic abnormalities were revealed in a pre-operative neurologic examination.
(a, b) Pre-operative standing radiographs (a, anteroposterior; b, lateral) show an 83° thoracolumbar curve (T10-L4) with a 10-cm truncal shift to the left and a 56° lumbar kyphosis (L1-S1) with an 11.5-cm positive sagittal alignment. (c) Pre-operative 3-dimensional CT reconstructions show severe thoracolumbar kyphoscoliosis due to hemivertebrae of the L3 and L4 vertebral bodies.
Surgical correction and fusion from T9 to the pelvis with posterior vertebral column resection (PVCR) was performed under general anesthesia and multimodal IOM (including SSEP, TcMEP and free-run EMG). PVCR is a surgical procedure designed to achieve the resection of the three-column of the spine, and is typically used in cases of severe, rigid spinal deformities.2 For IOM, the warning criteria included a >50% loss in amplitude or >10% increase in the latency from baseline for SSEPs, and a >70% loss in amplitude from baseline for TcMEPs.
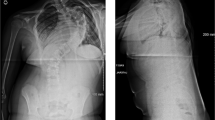
The surgery was performed through a posterior-only approach. After segmental spinal instrumentation using mainly pedicle screws, PVCRs of L3 and L4 were performed with a temporary rod on the right side. Then, two rods were placed on the left side at the levels of T9-L2 and L5-sacrum (Figure 2a). IOM did not demonstrate any significant changes during or after these procedures. The proximal rod was connected to the distal rod using domino-connectors, and the spinal column above the PVCR area was translated to the right (Figure 2b). Just after this procedure, the free-run EMG of the left quadriceps femoris muscle (QF) demonstrated train activity composed of 20–30 Hz spike waves that lasted ~30 min (Figure 3a). Therefore, we checked the condition of the dura and neural elements, and determined that the left L3 nerve root was stretched as the result of the translational shift of the proximal spinal column at the PVCR area; however, no mechanical contact with neural elements or neural injury was observed, and the left L4 nerve root was intact. Moreover, the TcMEP amplitude of the left QF was well maintained within the control levels (Figures 3b and c); thus, we did not release the correction at the PVCR area. An expandable cage was inserted into the PVCR area and closure of the PVCR area was performed using compression forces. At the end of the surgery, although the TcMEP amplitudes of the monitored muscles (including the upper extremities) tended to be decreased when compared with the control level (Figure 3b), the TcMEP amplitude of the left QF was at 65% of the control level (representing a 35% decrease; Figure 3c). During surgery, the amplitude and latency of the SSEPs remained within normal limits.
(a) Free-run EMG monitoring after spinal correction at the area of the PVCRs shows train activity composed of spike waves in the left QF. (b) TcMEPs did not show any significant changes during surgery. (c) TcMEPs of the left QF are shown during the following time points: (1) control, (2) after resection, (3) just after EMG train activity, (4) 30 min later and (5) at the end of surgery. APB, abductor pollicis brevis; FHB, flexor halluces brevis muscle; TA, tibialis anterior muscle.
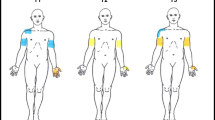
On wake-up from anesthesia, a neurologic examination revealed a significant decrease (grade 2-) in the manual muscle test for the left QF and iliopsoas muscle. At 1 day after surgery, weaknesses in the left QF and iliopsoas muscle persisted, and hypesthesia of the left anterior thigh was revealed; no other neurological deficits were revealed. She underwent a CT scan and MRI, which did not demonstrate any lesions capable of causing a compression of neural elements with neurological deficits. As muscle power and sensations in the left thigh gradually improved each day, we did not perform any revision surgeries, including release of the correction. Fortunately, muscle strength was fully recovered and she could walk independently at 6 months postoperatively; however, numbness in the left anterior thigh persisted at 2 years after surgery (Figure 4).
Discussion
Our patient was in one of the highest risk groups for neurological deficits including nerve root injury because she had congenital lumbar kyphoscoliosis and underwent 3-column osteotomies.3,4 Because of limitations associated with each individual IOM, multimodal IOM (including TcMEP, SSEP and fee-run EMG monitoring) has been widely used, especially in high-risk patients.
TcMEPs have high sensitivity (ranging from 75 to 100%) and high specificity (ranging from 84 to 100%), and are widely regarded as the gold standard for monitoring the motor pathway during surgery.1 However, controversy still exists regarding whether TcMEPs can entirely monitor spinal nerve root function. Several authors have shown that TcMEPs are highly sensitive to lumbar nerve root function,5–7 but others have emphasized that TcMEPs cannot detect an isolated nerve root insult due to the overlapping muscle innervation of adjacent root levels.8–10 In our patient, the cause of the motor deficit was thought to be the nerve root stretch of the left L3. Generally, QF is innervated by L2, L3 and L4 nerve roots.11 Therefore, the TcMEPs of the left QF in our patient may have been generated by the conduction of transcranial stimuli through L2 and L4, even after an L3 nerve root injury.
On the other hand, intra-operative free-run EMG is used to detect compromise in motor pathways, mainly in the motor nerve root, and provide real-time feedback, especially during spinal surgeries where peripheral nerves or roots are at a risk of injury.1 Indeed, Gunnarson et al.12 reported that 77.5% of 213 consecutive cases who underwent lumbosacral surgeries had at least one activation of free-run EMG, resulting in a low specificity for free-run EMG monitoring.5,12–14 This low specificity can cause free-run EMG to be less reliable in predicting postoperative motor deficits than TcMEPs, and can prevent surgeons from performing appropriate responses to abnormal EMGs with normal TcMEPs findings. There may be several reasons for the low specificity in free-run EMGs. First, free-run EMG provides real-time feedback. Therefore, it may lead one to alter the surgical procedures before the occurrence of a severe or irreversible neural injury, elevating the false-positive rate. Second, there are no definite warning criteria for free-run EMGs. Generally, activity patterns in free-run EMG are characterized as burst or train activity. Burst activity consists of nonrepetitive asynchronous potentials, while train activity consists of repetitive synchronous discharges that may last for several minutes. Although burst potentials are associated with any mechanical contact with the nerve root, the presence or degree of burst potentials are not likely to be associated with neural insult. On the other hand, sustained tonic activity in free-run EMG has been reported to be related to sustained traction and compression of nerve roots, and is more associated with neural injury.5,7,12,15,16 However, several authors have included not only train activity, but also burst activity, in the warning criteria for free-run EMGs, which might result in high sensitivity and low specificity in free-run EMG monitoring.12,14,17 Therefore, to establish definite warning criteria for free-run EMG monitoring, it is necessary to analyze true-positive cases in detail. In our patient, a true-positive finding with long-lasting train activity in the free-run EMG of the left QF occurred after correction with a translation technique at the PVCR area. Therefore, long-lasting train activity in free-run EMG may be one of the warning criteria for postoperative motor deficits.
In conclusion, the possibility of false-negative TcMEPs should be kept in mind, especially during surgery with a risk of nerve root injury. The present case was a rare case, but could represent cases with potentially preventable motor deficits after surgery, providing a warning for an over-reliance on TcMEP monitoring. When abnormal findings in the free-run EMG are observed (at least long-lasting train activity), surgeons should consider appropriate responses, such as the release of the correction, even when no substantial changes are seen in the TcMEPs.
Informed patient consent
The patient consented to the submission of this case report to the journal.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Lall RR, Lall RR, Hauptman JS, Munoz C, Cybulski GR, Koski T et al. Intraoperative neurophysiological monitoring in spine surgery: indications, efficacy, and role of the preoperative checklist. Neurosurg Focus 2012; 33: E10.
Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH . Posterior vertebral column resection for severe spinal deformities. Spine 2002; 27: 2374–2382.
Boachie-Adjei O, Yagi M, Nemani VM, Sacramento-Dominguez C, Akoto H, Cunningham ME et al. Incidence and risk factors for major surgical complications in patients with complex spinal deformity: a report from an SRS GOP site. Spine Deform 2015; 3: 57–64.
Burton DC, Carlson BB, Place HM, Fuller JE, Blanke K, Cho R et al. Results of the scoliosis research society morbidity and mortality database 2009–2012: a report from the Morbidity and Mortality Committee. Spine Deform 2016; 4: 338–343.
Bose B, Sestokas AK, Schwartz DM . Neurophysiological detection of iatrogenic C-5 nerve deficit during anterior cervical spinal surgery. J Neurosurg Spine 2007; 6: 381–385.
Lieberman JA, Lyon R, Feiner J, Hu SS, Berven SH . The efficacy of motor evoked potentials in fixed sagittal imbalance deformity correction surgery. Spine 2008; 33: E414–E424.
Lyon R, Lieberman JA, Feiner J, Burch S . Relative efficacy of transcranial motor evoked potentials, mechanically-elicited electromyography, and evoked EMG to assess nerve root function during sustained retraction in a porcine model. Spine 2009; 34: E558–E564.
Iwasaki H, Tamaki T, Yoshida M, Ando M, Yamada H, Tsutsui S et al. Efficacy and limitations of current methods of intraoperative spinal cord monitoring. J Orthop Sci 2003; 8: 635–642.
Macdonald DB, Al Zayed Z, Al Saddigi A . Four-limb muscle motor evoked potential and optimized somatosensory evoked potential monitoring with decussation assessment: results in 206 thoracolumbar spine surgeries. Eur Spine J 2007; 16: S171–S187.
Tsutsui S, Tamaki T, Yamada H, Iwasaki H, Takami M . Relationships between the changes in compound muscle action potentials and selective injuries to the spinal cord and spinal nerve roots. Clin Neurophysiol 2003; 114: 1431–1436.
Macdonald DB, Stigsby B, Al Homoud I, Abalkhail T, Mokeem A . Utility of motor evoked potentials for intraoperative nerve root monitoring. J Clin Neurophysiol 2012; 29: 118–125.
Gunnarsson T, Krassioukov AV, Sarjeant R, Fehlings MG . Real-time continuous intraoperative electromyographic and somatosensory evoked potential recordings in spinal surgery: correlation of clinical and electrophysiologic findings in a prospective, consecutive series of 213 cases. Spine 2004; 29: 677–684.
Jimenez JC, Sani S, Braverman B, Deutsch H, Ratliff JK . Palsies of the fifth cervical nerve root after cervical decompression: prevention using continuous intraoperative electromyography monitoring. J Neurosurg Spine 2005; 3: 92–97.
Quraishi NA, Lewis SJ, Kelleher MO, Sarjeant R, Rampersaud YR, Fehlings MG . Intraoperative multimodality monitoring in adult spinal deformity: analysis of a prospective series of one hundred two cases with independent evaluation. Spine 2009; 34: 1504–1512.
Devlin VJ, Schwartz DM . Intraoperative neurophysiologic monitoring during spinal surgery. J Am Acad Orthop Surg 2007; 15: 549–560.
Obi T, Mochizuki M, Isobe K, Mizoguchi K, Takatsu M, Nishimura Y . Mechanically elicited nerve root discharge: mechanical irritation and waveform. Acta Neurol Scand 1999; 100: 185–188.
Raynor BL, Padberg AM, Lenke LG, Bridwell KH, Riew KD, Buchowski JM et al. Failure of intraoperative monitoring to detect postoperative neurologic deficits: a 25-year experience in 12375 spinal surgeries. Spine 2016; 41: 1387–1393.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ohashi, M., Watanabe, K., Furutani, K. et al. False-negative transcranial motor evoked potentials (TcMEPs) during surgery for congenital lumbar kyphoscoliosis: a case report. Spinal Cord Ser Cases 3, 17053 (2017). https://doi.org/10.1038/scsandc.2017.53
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2017.53