Abstract
Introduction
Chronic neuropathic pain (NeP) often develops following traumatic spinal cord injury (SCI). This case report explores variability in clinical and neurophysiological aspects of pain evaluation in early post-trauma stages.
Case presentation
A 34-year old female presenting with acute incomplete sensorimotor tetraplegia C4 AIS D was examined by neurological examination and pain assessment at three time points after acute trauma T1 (8 weeks), T2 (11 weeks), and T3 (24 weeks). Quantitative sensory testing (QST) and laser-evoked potentials (LEPs) were measured above (control area), at (area of NeP), and below (foot) the neurological level of injury (NLI). Musculo-skeletal and neuropathic pain were clinically present already during T1 but showed variations in localization and occurrence over time. Neuropathic pain classification varied between time points due to shifting of NLI. Above-level QST revealed minor, less pronounced abnormalities similar to at-level site. At-level QST (site of NeP) showed loss for thermal and mechanical detection thresholds but also gain of function for mechanical pain thresholds with a tendency of amelioration over time. QST below-level did not reveal remarkable changes over time. LEPs above- and below-level were within normal limits. At-level LEPs abolished after T1.
Discussion
In early stages post injury (up to 6 month) variations in pain presentation for both, musculo-skeletal and neuropathic pain as well as QST and LEP could be demonstrated. These findings suggest ongoing adaption mechanisms in sensory pathways, which require further exploration and may be relevant for prognostic and preventive strategies against the development of chronic neuropathic and nociceptive pain.
Similar content being viewed by others
Introduction
Pain is the most encountered problem in functioning among individuals with spinal cord injury (SCI) [1]. The estimated prevalence of pain following traumatic SCI is 74% [2], the point prevalence of neuropathic pain (NeP) is 53% [3]. Besides, pain is a difficult problem to manage and also directly contributes to disability by reducing the person’s capacity to participate in rehabilitation and return to work [4]. Onset of neuropathic SCI pain (SCIP) is observed within the first 12 month following SCI and tend to become persistent, whereas musculoskeletal pain either resolves in cases of early onset [5] or more often has a late onset. Chronic pain is defined as persistent or recurrent pain lasting longer than 3 months [6]. The diagnosis of different pain types, including NeP, is clinically according the International Spinal Cord Injury Pain Classification (ISCIP) which distinguishes between nociceptive, neuropathic and unknown pain [7]. In unclear pain presentation neurophysiology as pain-related evoked potentials and quantitative sensory testing (QST) may help to support the diagnosis of NeP [8, 9].
Pain-related evoked potentials like laser evoked potentials (LEPs) and contact heat evoked potentials (CHEPs) as well as QST have been shown to be abnormal in chronic NeP in individuals with SCI [8, 10, 11]. In addition, QST has also been applied in early stages of SCI (within 2 weeks up to 6 month) to monitor early changes of sensory profiles showing abnormalities in thermal thresholds and signs of hypersensitivity [12]. QST according to the German network on neuropathic pain (DFNS) is a comprehensive tool to examine a wide range of sensory modalities including thermal and mechanical detection and pain thresholds [13].
Within the Swiss Spinal Cord Injury Cohort Study (SwiSCI), approved by local ethical committee (EKNZ 2017-00634) we report a case where pain assessment and neurophysiology as LEPs and QST were applied during first rehabilitation after SCI to explore early clinical, pain-related and neurophysiological aspects of pain development and chronification.
Case presentation
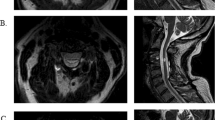
After an acute trauma due to a traffic accident, a 34-year old female presented with an incomplete sensorimotor tetraplegia, C4, American Spinal Injury Association (ASIA) Impairment Scale (AIS) grade D. We monitored her by neurological examination, pain assessment and neurophysiological examinations during 3 different time points: 8 weeks (T1), 11 weeks (T2) and 24 weeks (T3) after injury. The neurological level of injury C4 at T1 shifted on left side to C3 at T2, further on to C1 at T3. Overall, there was a clinical improvement from T1 to T3 (sensory level on the right side improved by 3 points, motor levels on both sides improved by 17 points in total according to the International standards for neurological classification of spinal cord injury, ISNCSCI) [14].
The SwiSCI inception cohort, of which the presented case was part of, has five measurement and sampling time points by design to ensure the longitudinal follow up of the functioning after SCI. Due to early discharge from hospital data is only available from the first three time points. The assessments included the ISNCSCI, the ISCIP-classification [7], the International Spinal Cord Injury Pain Basic Data Set (SCIPBDS), version 2.0 [15], the Spinal Cord Injury Pain Instrument (SCIPI) [16] and pain drawings. Neurophysiological examinations as LEPs and QST were performed at 3 different locations on her left body site: [1] Within 2 dermatomes above the neurological level of injury (NLI) as an unaffected control area, named above-level area. The range of 2 dermatomes was chosen for technical reasons to improve suspected accessibility for the neurophysiological tests [2]. Within 3 dermatomes below NLI, named at-level area. This area is suspected to correlate with the area of neuropathic At-level SCIP and associated sensory findings [3]. At the dorsum of the foot, named below-level area. QST was performed according to the standardized protocol of the German network for NeP [13]. This protocol includes the acquisition of cold detection threshold (CDT), warm detection threshold (WDT), thermal sensory limen (TSL), cold pain threshold (CPT), heat pain threshold (HPT), pressure pain threshold (PPT), mechanical pain threshold (MPT), mechanical pain sensitivity (MPS), wind-up ratio (WUR), mechanical detection threshold (MDT), vibration detection threshold (VDT), dynamic mechanical allodynia (DMA) and paradoxical heat sensations (PHS). Thermal stimuli were applied using TSA-II, Medoc, Ramat Yishai, Israel (temperature range: 0–50 °C, baseline temperature 32 °C). For TSL thermal difference limen using alternating cool and warm stimuli, for PHS the number of reported paradoxical heat sensations were recorded. For mechanical detection threshold (MDT) modified von Frey hairs (Opti-hair2-Set; Marstock Nervtest, Schriesheim, Germany), for mechanical pain threshold (MPT) calibrated pinpricks (MRC Systems, Heidelberg, Germany), for vibration detection threshold (VDT) Rydel-Seiffer tuning fork (64 Hz) and for pressure pain threshold (PPT) pressure algometer (FDN200 foot; FDN100 face, neck, arm; Wagner Instruments, Greenwich, CT, USA) were used. For determination of mechanical pain sensitivity (MPS) and dynamic mechanical allodynia (DMA) pinprick stimuli (as above) and slight tactile stimuli (cotton wisp, 3 mN; Q-tip, 100 mN; soft brush, 200–400 mN; Somedic, Hörby, Sweden) were given in a standardized randomized order. Wind up ratio (WUR) was assessed as a ratio between a single pinprick stimulus and a series of 10 repetitive applications of the same stimulus intensity in a frequency of 1/s. To determine MPS, DMA and WUR the patient was asked to rate the stimuli on a numeric rating scale (NRS), 0 = no pain, pricking, stinging or burning sensation, 100 = maximal pain imaginable. LEPs measurements were performed using a Thulium-YAG laser (StarMedTec GmbH, Starnberg, Germany). For LEPs recording, a randomized application by the machine of different laser intensities alternating between 1.6 and 1.8-fold of the pain threshold and randomized inter-stimulus interval lasting between 7 and 15 s were given. All evoked potentials were recorded from Cz versus linked earlobes (band pass 1–30 Hz, sampling rate 500 Hz, impedance < 5 kΩ). Ground electrode was attached to the right hand. The Electro-Oculo-Gram (EOG) of the right eye was recorded from two linked surface electrodes.
Findings
The evaluation of the SCIPBDS 2.0 revealed that during her 3 visits the patient showed variable pain distributions with regard to the occurrence of nociceptive pain on right shoulder (abolished intermittent) and a conversion from nociceptive pain on both upper arms to NeP at T2. The localization of NeP was also variable between T1 and T2 with reduction of the extent of whole hand to thumb only, which went along with a change in classification from Below-level SCIP (Be-L SCIP) to At-level SCIP (At-L SCIP). In addition, due to a change of the NLI over time, the classification At-L SCIP on T2 for both locations (upper arms and left hand) changed again to Be-L SCIP at T3 (Fig. 1). The pain interference for daily activities improved from T1 to T2 and T3 from NRS 4 to 2/10 (0 stands for no interference at all, 10 for very high interference). Mood and sleep were not affected by the pain at T1, but sleep was mildly affected by pain at T2 and T3 (NRS 3 and 2/10 resp.). Pain interference on mood was obvious on T3 showing NRS 3/10. Medical treatment at T1 included anti-epileptics, opioids and analgesics. At visit T2 opioids had been stopped while at T3 she was not on pain medication. SCIPI questionnaires at T1 were concordant with musculo-skeletal pain (right shoulder 0/6 items, upper arms 0/6 items), but for NeP failed to be discriminative (3/6 items). SCIPI questionnaire were concordant according musculo-skeletal pain (right shoulder at T3 1/6 items) and NeP upper arms (T2 4/6, T3 5/6 items) and for thumb 4/6 items at T2 and T3.
QST at the above-level site showed, despite clinically not affected by pain or neurological deficits, at T1 some loss for thermal and mechanical detection thresholds but gain of function for pressure pain (Fig. 2A) which partly persisted at T2 but improved to a lesser extent at T3. QST at the at-level area (site of NeP) showed basically the same time course with more pronounced values, but normalization for mechanical loss at T3 (Fig. 2B). QST at the below-level area showed loss of function for mechanical detection thresholds, but less pronounced at T3 (Fig. 2C). Latencies and amplitudes of LEPs at the above-level site were within normal limits at all 3 time points, amplitudes showed a stepwise increase with time. At the at-level site, LEPs abolished after T1. LEPs at the below-level site were within normal limits but amplitudes improved at T3 (Fig. 3).
A Above-level testing area, (B) at-level testing area, (C) below-level testing area. Parameters are shown in z-score values, except for PHS and DMA (inset). Values below zero indicate a loss of function and values above zero indicate a gain of function. The gray area indicates values in normal range (−1.96 to 1.96). CDT cold detection threshold, WDT warm detection threshold, TSL thermal sensory limen, CPT cold pain threshold, HPT heat pain threshold, PPT pressure pain threshold, MPT mechanical pain threshold, MPS mechanical pain sensitivity, WUR wind-up ratio, MDT mechanical detection threshold, VDT vibration detection threshold, PHS paradoxical heat sensations, DMA dynamic mechanical allodynia; T1, 8 weeks; T2, 11 weeks; T3, 24 weeks, NRS numeric rating scale.
Stimulation level is indicated on the left side of each image and is further specified in the table indicating the stimulated dermatome. Note, due to change of the neurological level of injury at time point T3, above level stimulation was done in the face. Registration started 500 ms before laser stimulation. Arrow indicates time of stimulation. EOG: electro-oculogram was recorded to detect artifacts. n.d.: not detected.
Discussion
The aim of this case report is to report pain-related and neurophysiological aspects of pain development during the early phase of SCI (between 8 and 24 weeks after trauma), a time period where processes of pain chronification take place. We observed variations in pain manifestations during the first 6 months following SCI for both pain types, nociceptive and neuropathic pain. In addition, due to variations of pain distribution and shifting of NLI, appropriate classification of NeP varied between At-L and Be-L SCIP. QST abnormalities were most pronounced within the neuropathic pain site, while LEPs abolished early at the neuropathic pain site. Findings may suggest ongoing adaption mechanisms in sensory pathways during the early post-injury stages, which may need further exploration to predict and prevent development of neuropathic and nociceptive pain.
It was found that both nociceptive and neuropathic pain types were present already 8 weeks after trauma. At week 24 nociceptive pain was diminishing but NeP was partly extending. This is in line with the literature as nociceptive pain is the most common type of pain early after injury whereas the prevalence of NeP increases over time [5]. Long term follow-up of 5 years after injury has shown a strong correlation for persisting NeP but poor correlation for nociceptive pain [17]. Time point T2 (11 weeks after trauma) in our report seemed to be interesting, since a transition of initial nociceptive appearing arm pain to a neuropathic At-L SCIP was noted. While the ISCIP-classification [7] contains the term “unknown pain” for pain types which cannot be classified properly, possibly such pain types may be potential candidates for such transition. We assume that mechanisms of central sensitization, which are involved in the transition from acute to chronic pain [18] and changes in the pain matrix [19] might be involved. A further interesting finding at T2 was, that due to a reduction of the extent of NeP from left whole hand (dermatomes C6, C7 and C8) at week 8 to thumb only (dermatome C6), there was a change from Be-L SCIP to At-L SCIP. But finally at T3 (week 24), the same thumb pain, due to a shift of the NLI from C3 to C1, had to be classified as Be-L SCIP. This change of NLI remains unclear since the study does not include MRI. But spreading of hypersensitivity to above-level areas up to several dermatomes in patients with Be-L SCIP pain has been described [20]. Neuronal, generalized and unspecific sensitization patterns of the central nervous system have been discussed [20]. In SCI with central neuropathic pain, significantly higher thermal and tactile detection thresholds have been found above the lesion level [21] in comparison to an SCI pain free group. Therefore, we propose that sensory changes above the NLI in patients with neuropathic SCIP may interfere with the exact determination of NLI and therefore with the appropriate NeP classification as At-L or Be-L SCIP.
The transition—as discussed above—from nociceptive to neuropathic pain has been supported by changes in SCIPI questionnaires accordingly. But SCIPI questionnaire at week 8 at the neuropathic pain site of left hand failed to be discriminative for NeP while on week 11 and 24 it was indicative for NeP. SCIPI questionnaire is validated to distinguish between nociceptive and neuropathic pain in SCI [16]. Failure in discrimination may be explained by sensitivity and specificity characteristics of this questionnaire.
QST results of our patient show a loss of thermal and mechanical detection thresholds at the at-level area (site of NeP) but a gain of function for mechanical pain thresholds with the tendency of mild amelioration over time. Sensory hypersensitivity in dermatomes corresponding to the lesion level was found more frequently in SCI patients with central pain than in those without pain [22]. Report of SCIP within one year after injury is related to an increase of Be-L SCIP, while report of At-L SCIP within the first 6 month is initially increasing, but later partly decreasing. Early sensory hypersensitivity, particularly cold-evoked dysesthesia at one month was found as a predictor for the development of Be-L SCIP at 12 months [15]. In addition, SCI patients who developed Be-L SCIP showed higher thermal thresholds than those who did not and displayed high rates of abnormal sensations (allodynia and hyperpathia), which gradually increased with time until central pain has been developed [12]. In chronic SCIP loss of thermal and mechanical detection and pain thresholds as well as gain of thermal and mechanical pain thresholds have been reported [8] but were also found in SCI without NeP [11]. In addition, QST in our patient at the above-level site showed, despite being clinically not affected by pain or neurological deficits, on T1 minor loss for thermal and mechanical detection thresholds but gain of function for mechanical pain threshold partly improving over time. QST changes above the NLI have been reported patients with SCIP [11, 20, 21]. Similar phenomena of QST changes in non-affected areas contralateral to NeP sites are also known from other NeP-syndromes [23, 24] or extraterritorial spread of symptoms [25], suggested to be related to chronic maladaptive cortical plasticity [23] or to pain-induced sensory changes through central mechanisms [24, 25]. QST at the below-level area in our patient was done in a not painful area. QST abnormalities have been reported in chronic pain free SCI individuals [11] basically showing impaired sensation due to SCI. The improvement in the below-level area at 24 weeks in our patient may reflect the clinical improvements from T1 to T3.
In our case abnormal respectively absent LEPs were found at the site of NeP only from week 8, suggesting ongoing changes within the spinothalamic tract [26]. Absent LEPs in chronic SCIP have been shown [8] but same findings were also found in SCI without pain [11]. Preserved LEPs at the below-level site may be related to incomplete SCI AIS D.
We conclude that early stages post injury (up to 6 month) may play an important role in the development of both, nociceptive and neuropathic pain. Findings may suggest ongoing adaption mechanisms during early stages post injury within sensory pathways, which may need further exploration to predict and prevent development of neuropathic and nociceptive pain as well as pain chronification.
References
Rubinelli S, Glässel A, Brach M. From the person’s perspective: perceived problems in functioning among individuals with spinal cord injury in Switzerland. J Rehabil Med. 2016;48:235–43.
Müller R, Brinkhof MW, Arnet U, Hinrichs T, Landmann G, Jordan X, et al. Prevalence and associated factors of pain in the Swiss spinal cord injury population. Spinal Cord. 2017;55:346–54.
Burke D, Fullen BM, Stokes D, Lennon O. Neuropathic pain prevalence following spinal cord injury: a systematic review and meta-analysis. Eur J Pain. 2017;21:29–44.
Siddall PJ. Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord. 2009;47:352–9.
Finnerup NB, Jensen MP, Norrbrink C, Trok K, Johannesen IL, Jensen TS, et al. A prospective study of pain and psychological functioning following traumatic spinal cord injury. Spinal Cord. 2016;54:816–21.
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain. 2015;156:1003–7.
Bryce TN, Biering-Sørensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International spinal cord injury pain classification: part I. Background and description. March 6-7, 2009. Spinal Cord. 2012;50:413–7.
Landmann G, Berger MF, Stockinger L, Opsommer E. Usefulness of laser-evoked potentials and quantitative sensory testing in the diagnosis of neuropathic spinal cord injury pain: a multiple case study. Spinal Cord. 2017;55:575–82.
Lefaucheur JP. Clinical neurophysiology of pain. Handb Clin Neurol. 2019;161:121–48.
Wydenkeller S, Maurizio S, Dietz V, Halder P. Neuropathic pain in spinal cord injury: significance of clinical and electrophysiological measures. Eur J Neurosci. 2009;30:91–9.
Opsommer E, Korogod N, Stockinger L, Landmann G. Multimodal sensory evaluation of neuropathic spinal cord injury pain: an experimental study. Spinal Cord. 2021. Jan 14. Online ahead of print.
Zeilig G, Enosh S, Rubin-Asher D, Lehr B, Defrin R. The nature and course of sensory changes following spinal cord injury: predictive properties and implications on the mechanism of central pain. Brain. 2012;135:418–30.
Rolke R, Baron R, Maier C, Tölle TR, Treede RD, Beyer A, et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain. 2006;123:231–43.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Widerström-Noga E, Biering-Sørensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord. 2014;52:282–6.
Franz S, Schuld C, Wilder-Smith EP, Heutehaus L, Lang S, Gantz S, et al. Spinal Cord Injury Pain Instrument and painDETECT questionnaire: convergent construct validity in individuals with Spinal Cord Injury. Eur J Pain. 2017;21:1642–56.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
Arendt-Nielsen L, Morlion B, Perrot S, Dahan A, Dickenson A, Kress HG, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain. 2018;22:216–41.
Garcia-Larrea L, Peyron R. Pain matrices and neuropathic pain matrices: a review. Pain. 2013;154:S29–43.
Vogel C, Rukwied R, Stockinger L, Schley M, Schmelz M, Schleinzer W, et al. Functional characterization of at-level hypersensitivity in patients with spinal cord injury. J Pain. 2017;18:66–78.
Finnerup NB, Johannesen IL, Bach FW, Jensen TS. Sensory function above lesion level in spinal cord injury patients with and without pain. Somatosens Mot Res. 2003;20:71–6.
Finnerup NB, Sørensen L, Biering-Sørensen F, Johannesen IL, Jensen TS. Segmental hypersensitivity and spinothalamic function in spinal cord injury pain. Exp Neurol. 2007;207:139–49.
Krause T, Asseyer S, Geisler F, Fiebach JB, Oeltjenbruns J, Kopf A, et al. Chronic sensory stroke with and without central pain is associated with bilaterally distributed sensory abnormalities as detected by quantitative sensory testing. Pain. 2016;157:194–202.
Younis S, Maarbjerg S, Reimer M, Wolfram F, Olesen J, Baron R, et al. Quantitative sensory testing in classical trigeminal neuralgia-a blinded study in patients with and without concomitant persistent pain. Pain. 2016;157:1407–14.
Matesanz L, Hausheer AC, Baskozos G, Bennett DL, Schmid AB. Somatosensory and psychological phenotypes associated with neuropathic pain in entrapment neuropathy. Pain. 2021;162:1211–20.
Treede RD, Lorenz J, Baumgärtner U. Clinical usefulness of laser-evoked potentials. Neurophysiol Clin. 2003;33:303–14.
Acknowledgements
This study has been supported and financed in the framework of the Swiss Spinal Cord Injury Cohort Study (SwiSCI, www.swisci.ch), supported by the Swiss Paraplegic Foundation which the authors thank for. The members of the SwiSCI Steering Committee are: Xavier Jordan, Bertrand Léger (Clinique Romande de Réadaptation, Sion); Michael Baumberger, Hans Peter Gmünder (Swiss Paraplegic Center, Nottwil); Armin Curt, Martin Schubert (University Clinic Balgrist, Zürich); Margret Hund-Georgiadis, Kerstin Hug (REHAB Basel, Basel); Hans Georg Koch, (Swiss Paraplegic Association, Nottwil); Hardy Landolt (representative of persons with SCI, Glarus); Nadja Münzel (ParaHelp, Nottwil); Mirjam Brach, Gerold Stucki (Swiss Paraplegic Research, Nottwil); Martin Brinkhof (SwiSCI Study Center at Swiss Paraplegic Research, Nottwil).
Funding
SwiSCI is hosted and funded by Swiss Paraplegic Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ernst, M., Ljutow, A., Stockinger, L. et al. Variability in clinical and neurophysiological evaluation of pain development following acute spinal cord injury: a case report. Spinal Cord Ser Cases 7, 72 (2021). https://doi.org/10.1038/s41394-021-00435-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00435-0