Abstract
Study design:
Prospective clinical study.
Background:
The aim of the study was to investigate cortical reorganisation after traumatic spinal cord injury (TSCI) using functional magnetic resonance imaging (fMRI).
Setting:
Tartu University Hospital, Tartu, Estonia.
Methods:
We studied six right-handed tetraplegic TSCI patients at 1, 3 and 12 months after the injury and 12 age- and gender-matched healthy controls. Individuals performed simple test–rest cycles of flexion/extension of the right-hand fingers and flexion/extension of the right ankle during fMRI. The volumes of activation (VOA), maximum t-values, centres of gravity (COG) and weighted laterality indexes were calculated.
Results:
There was no recovery of neurologic function in three patients and, according to the American Spinal Injury Association (ASIA) Impairment Scale the remaining three recovered. A positive correlation between the VOA in the primary motor cortex and the ASIA Impairment Scale (1 month: r=0.82, P=0.002; 3 Month: r=0.63, P=0.03; 12 Month: r=0.23, P=0.52) was found. The study also revealed a pattern of cortical activation that was increased among the patients who recovered (in Brodmann area 4 (BA 4), P=0.06; BA 1-2-3-5, P=0.08; BA 6, P=0.05). During the hand task there was an expansion of COG laterally, anteriorly and inferiorly among the patients who recovered. During the hand movement the cortical activation was less lateralised among the patients compared with the controls (P<0.05).
Conclusion:
Our study has found broadening of cortical activation and shift of COG during the first year after TSCI, depending on the recovery.
Similar content being viewed by others
Introduction
Depending on the type of nervous system lesion, completeness and recovery, different patterns of cortical reorganisation may occur.1 Earlier, body cortical representations were believed to be stable. Within the last 20 years, advances in neuroimaging and brain mapping have shown that the cortex may adapt to the environment.
Although spinal cord injury (SCI) does not affect the brain, changes in brain function of traumatic SCI (TSCI) patients have been identified by different studies. Several analysts have expressed doubts about the exact pattern of changes after TSCI because of varying and even conflicting results.1
A growing body of brain reorganisation studies has been performed on paraplegics. Only a few studies have investigated cortical reorganisation after cervical TSCI.2, 3, 4, 5
However, there is still little evidence on the temporal changes in reorganisation of the sensorimotor cortex.3, 4 Functional magnetic resonance imaging (fMRI) could be used as a surrogate marker of functional outcome after TSCI.6, 7
The aim of our study was to test the cortical activations in patients with cervical TSCI in acute and sub-acute phase after TSCI. We hypothesise that activation in the primary motor cortex and non-primary motor areas changes during the first year following injury, depending on the recovery.
Patients and methods
Six right-handed tetraplegic male patients (mean age 27.3±10.9 years, range 18–41 years) were studied repeatedly after TSCI by functional magnetic resonance imaging (fMRI) at 20.8±6.7, 111.3±21.9 and 376±26.3 days after the injury.
Twelve age- and gender-matched healthy controls (mean age 27.1±10.1 years, range 18–42 years) were studied at a single point of time and seven controls on two occasions (353.7±50.5 days between the studies). All subjects signed informed, written consent permission before the study, which was approved by the Research Ethics Committee of the University of Tartu, Estonia.
The baseline characteristics of the patients are shown in Table 1. Five of the TSCI patients were sustained at diving, one patient had fallen from a height (number 4).
Only patients with a neurological deficit lasting more than 1 week were included. The inclusion criteria were also tetraplegia due to cervical TSCI. TSCI patients had to be medically stable and be able to sign informed consent before the study. We excluded patients with traumatic brain injury, patients with a previous history of seizures and those who had contraindications to MRI.
The extent of injury was estimated according to the American Spinal Injury Association (ASIA) Impairment Scale.8 The patients were classified according to their motor level of injury (C5, C6 and C7). Patient number 1 was hospitalised with severe tetraplegia after TCSI. The first imaging was performed 19 days after trauma, when significant recovery had occurred. With three patients, the recovery of motor function occurred. Patient number 5 moved from the complete injury group to incomplete injury group, because over the course of the first year sensation in the sacral segments improved. However, he remained in the motor complete group of injury in this study.
fMRI study design
We used a study design similar to Tomberg et al.9 Each activation experiment consisted of a 40-s period of rest, followed by a 40-s period of movement, which was repeated three times. The individuals were trained to perform the movements at a frequency of 1 Hz.
During the fMRI study the individuals performed simple test–retest cycles of (1) flexion/extension of the right-hand fingers and (2) flexion/extension of the right ankle. Motor tasks were continuously visually monitored.
All patients were able to perform movement of the hand, but the movement observed was wrist movement of the patients with a higher level of injury. Ankle movement was not possible in half of the patients.
Image acquisition
Images were obtained on a 1.5-T clinical whole-body MR scanner (Magnetom Symphony; Siemens Medical Systems, Erlangen, Germany). Before functional scans, a high-resolution T1-weighted anatomical image was obtained with the gradient echo, fast low-angle shot sequence (repetition time (TR)=12 ms, echo time (TE)=5.68 ms, flip angle 15°, resolution 224 × 256, voxel size 1 × 1 × 1 mm3, 176 sagittal planes). Functional T2*-weighted images were obtained using the gradient echo planar imaging (EPI) sequence (TR=4 s, TE=50 ms, flip angle 90°, resolution 64 × 64, voxel size 3 × 3 × 3 mm3, slice gap 0.75 mm, 36 axial planes, interleaved scan).
Image processing
Image processing was performed using Statistical Parametric Mapping (SPM8, update rev. no. 4290; Wellcome Trust Centre for Neuroimaging, London, UK) software.
The first step of spatial pre-processing was the realignment of functional images, where movement effects were discounted, after which high-resolution anatomical images were co-registered with functional images, to maximize the mutual information. Pre-processing continued with segmentation of high-resolution anatomical images, where the Montreal Neurological Institute 452 white matter, grey matter and cerebrospinal fluid probability maps10 were used to yield a parametric description for normalisation. During normalisation, images were also bias-corrected. Image pre-processing ended with smoothing by 8 × 8 × 8 mm3 full-width at half maximum isotropic Gaussian kernel.
Statistical analysis
Modelling was done with boxcar functions convolved with canonical hemodynamic response function (HRF). Low-frequency noise was eliminated by using a 160-s high-pass filter. Estimation of model parameters was done by using SPM8, after which task versus rest activation was assessed by applying a t-test to the parameter estimates, resulting in statistical parametric t-maps for each subject. Multiple comparisons’ problems were corrected by masking images with the Brodmann area (BA) masks BA 1-2-3-5 (BA 1, 2, 3 and 5 were analysed as one area), BA 4 and BA 6 from MRIcro,11 by using SPM8 and by applying family-wise error correction with P<0.05, and by discounting all clusters smaller than three voxels.
From the resulting masked t-maps, maximum t-test results and Talairach coordinates of the maximum activation were recorded. The total volume of all activated cluster(s) in each region of interest (ROI) (defined by the masked areas) was calculated and Talairach coordinates of the geometric centres of gravity (COG) of the cluster with maximum t-test result in each ROI were found using MarsBaR release 0.43.12
Finally, weighted laterality index (wLI) was calculated by using the combined bootstrap/histogram analysis approach.13 Bootstrap algorithm helps to evaluate sampling distribution of a sample by repeatedly resampling, with replacement, the original sample, which would give approximately the ‘real’ distribution of the original sample.
Results
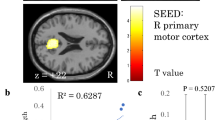
Figure 1 shows the brain activation during hand movements in TSCI patients and control subjects. Figure 2 shows the activated brain areas when the subjects moved or attempted to move their right ankle.
Activation patterns of control subjects
The mean movement rate of the control subjects was 0.58±0.17 Hz during hand movement and 0.46±0.13 Hz during ankle movement. There was no significant correlation between movement rate and the volume of BA 4 activation in the control group. In the control subjects studied twice (seven individuals), no significant change of volumes of activation (VOA) in BA 4 (hand, P=0.56; ankle, P=0.18), BA 1-2-3-5 (hand, P=0.45; ankle, P=0.42) or BA 6 area (hand, P=0.48; ankle, P=0.99) was found. The location of BA 4 activation was in the left anatomical hand region for all but one subject, who had no activation at the chosen threshold. The COG coordinates did not change significantly during 1 year (Table 2).
Activation patterns of TSCI patients
The mean hand movement rate was lower in the TSCI patients’ group compared with that in controls (0.36±0.19 Hz, P=0.02). A significant relationship was found between the movement rate and ASIA motor score (r=0.53, P=0.001). There were also significant correlations between the VOA in BA 4 and ASIA motor score. The correlation was the highest immediately after injury (r=0.82, P=0.002), veering towards no correlation by 3 months later (r=0.63, P=0.03) and 12 months later (r=0.23, P=0.52).
Among the patients who recovered, the VOA in BA 4, BA 6 and BA 1-2-3-5 was increased compared with those whose neurological state did not change during the year. This phenomenon was found in the hand as well as in the ankle movement (Figures 3 and 4).
(a) Volume of the right-hand movement-related BA 4 activation versus time post TSCI. (b) Volume of the right-hand movement-related BA 6 activation versus time post TSCI. (c) Volume of the right-hand movement-related BA1-2-3-5 activation versus time post TSCI. Abbreviations: VOA, volumes of activation; BA, Brodmann area; w, with; wo, without.
(a) Volume of the right-ankle movement-related BA 4 activation versus time post TSCI. (b) Volume of the right-ankle movement-related BA 6 activation versus time post TSCI. (c) Volume of the right-ankle movement-related BA1-2-3-5 activation versus time post TSCI. Abbreviations: VOA, volumes of activation; BA, Brodmann area; w, with; wo, without.
The overall VOA in the primary motor cortex of the patients who recovered was higher compared with other patients (hand, P=0.06; ankle, P=0.02). Because of the huge variability of VOA in BA 1-2-3-5 and BA 6, the difference did not reach a statistically significant level (BA 1-2-3-5: hand, P=0.08; ankle P=0.1; and BA 6: hand, P=0.05; ankle P=0.04).
At the first, second and third study sessions, a specific pattern of activation was found. Figures 3 and 4 demonstrate that the activation area was enlarged in the beginning of the study (first 3 months) and reached the level of controls and patients who did not recover by the end of the first year.
The overall location of COG in BA 1-2-3-5, BA 4 and BA 6 was similar among the patients who did not recover and the controls. There was no shift in COGs during the first year post TSCI. During the hand task, there was an expansion of COG laterally, anteriorly and inferiorly among the patients who recovered (BA 4: x −35.5 to −46.9, P=0.13; y −22.5 to −14.0, P=0.15, z 57.4 to 48.8, P=0.21; BA 1-2-3-5: x −38.2 to −47.2, P=0.14; y −28.9 to −27.1, P=0.14; z 54.5 to 47.8, P=0.23). Among the recovered TSCI patients during the ankle movement, the shift of COG was medial, anterior and superior in BA 4 (x: −6.3 to −1.8, P=0.02; y: −25.7 to −23.2, P=0.16; z 63.8 to 66.0, P=0.25).
Brain activation was more bilateral in TSCI patients than in controls (Table 3). In BA 4, the mean wLI was 0.72±0.19 during the right-hand movement among the patients compared with 0.90±0.11 among the controls (P<0.001). Similarly, in BA 6 and BA 1-2-3-5 the wLI was less lateralised during the hand movement among the patients (0.59±0.29 vs 0.74±0.16, P=0.005; 0.50±0.29 vs 0.73±0.14, P=0.02). During the movement of the leg, the wLI differences did not become statistically significant (BA 4, P=0.22; BA 1-2-3-5, P=0.95; BA 6, P=0.37).
Discussion
Our study provides a considerable insight into the changes of brain activation after TSCI. We have found that the brain activation patterns between the recovered and unrecovered patients are substantially different during the first 3 months after the injury. Activation is increased among the patients who recover. To our knowledge, our study is the first one to identify a shift in activation during the acute phase of cervical TSCI. We suggest that the results offer unique evidence for the usefulness of fMRI as a surrogate marker for outcome after TSCI.
One of the main goals of the study was to find the brain activation pattern changes in patients with cervical TSCI. Until now, only two studies have been performed to report the temporal evolution of cortical sensorimotor activity after TSCI.3, 4 In their first study, where TSCI patients with motor recovery were studied, a progressive enlargement in the primary motor cortex and decreased activation in associated cortical areas was detected.3 When they studied four tetraplegic individuals whose paralysis persisted, the activation was extensive in associated areas early post injury, but progressed towards no activation by the end of the first year.4 Our results differ slightly from these earlier findings. Soon after the injury, the activation was enlarged only among these TSCI patients who recovered and the enlargement was detected in every ROI. However, the activation decreased by the end of the first year and became similar among the patients and controls.
Despite the fact that two types of spatial shift have been observed, medial and posterior,1 we detected a shift of COG in BA 4 and BA 1-2-3-5 laterally, anteriorly and inferiorly during the right-hand movement. The earlier studies that have demonstrated these spatial shifts have tested patients in the chronic phase. For example, Mikulis et al.5 studied tetraplegic TSCI patients in the chronic phase and showed that when these patients moved their tongue, the primary motor cortex activation was shifted medially and posteriorly into the upper-limb representation region. Several investigators have proposed that similar shift takes place among paralysed patients when they move their hand.1, 14, 15, 16 It has been argued that the representation migrates superiorly and medially, as it borders on the adjacent disconnected upper- or lower-extremity cortex.1 The possible causes of the changes are destructed sensorimotor tracts, disruption of lateral inhibitory network in the cortex and modification of neuronal activity.5, 17
Methodically, the hand motor task we have used was more complex than in many other studies. The patients with TSCI could perform the hand task, but there was a significant reduction in force and speed of the movements. Patients with a complete injury performed movements only by the wrist. Hence, we speculated that by support of proximal arm muscles there would be a medial shift of activation as well as decreased VOA. Surprisingly, there was quite an opposite shift among the patients who recovered, and their VOA was larger compared with the control subjects.
Our results demonstrate the shift towards the intact face representation during hand movement, whereas the shift is opposite to the hand movement during the ankle movement. As a result, the COG moves towards the toes’ cortical representation. We are not aware whether there is an invasion of the affected part of the body cortical representation exactly into the face or toes’ zone, but contrary to other studies shifts to different directions are noticed during the first year. Our acute-phase findings appear to be well supported by a previous report that cortical representation of the body parts is continuously changing, depending on activity, the location of lesion in the nervous system or the new skills learned.18
Patients with TSCI and stroke share several aspects of brain reorganisation following injury.19 The more severe the hand motor deficit, the greater is the shift of primary motor cortex activation towards the contralateral hemisphere balance. According to wLI, cortical activation during hand movement was less lateralised among the patients than in controls in our study. The lower-limb cortical representation occupies a smaller and medial spatial extent in the primary cortex, which may be the main cause of non-significant wLI differences during the ankle movement among the patients and controls. As the sample was small, we did not find any statistically significant difference of laterality regarding the recovery.
Contrary to the earlier studies,6 we can conclude that the cortical functional reorganisation is larger among the patients who recover.
There were some limitations in the study as we did not image the spinal cord, so it is not possible to correlate the size of damaged area in association of cortical reorganisation.
The main limitation is the small number of patients in our study. The results would have been more conclusive when there were more patients with cervical TSCI. What we know about the cortical reorganisation is largely based on a small number of cases because of the strict inclusion and exclusion criteria.1 With longitudinal studies of this kind, it is complicated to recruit patients with similar neurological deficit and also to study the individuals repeatedly at certain time points. Patients must be medically stable during the imaging and could not have concomitant traumatic brain injury. In our study, we were able to study every patient regularly at the given time points, but there were also more activation in associated cortical sensorimotor areas of controls in our study compared with other studies.
In conclusion, our results show that during the first year post TSCI, compensatory changes in the brain function will take place. The increase of VOA is more extensive among the patients who recover.
Data archiving
There were no data to deposit.
References
Kokotilo KJ, Eng JJ, Curt A . Reorganization and preservation of motor control of the brain in spinal cord injury: a systematic review. J Neurotrauma 2009; 26: 2113–2126.
Curt A, Bruehlmeier M, Leenders KL, Roelcke U, Dietz V . Differential effect of spinal cord injury and functional impairment on human brain activation. J Neurotrauma 2002; 19: 43–51.
Jurkiewicz MT, Mikulis DJ, McIlroy WE, Fehlings MG, Verrier MC . Sensorimotor cortical plasticity during recovery following spinal cord injury: a longitudinal fMRI study. Neurorehabil Neural Repair 2007; 21: 527–538.
Jurkiewicz MT, Mikulis DJ, Fehlings MG, Verrier MC . Sensorimotor cortical activation in patients with cervical spinal cord injury with persisting paralysis. Neurorehabil Neural Repair 2010; 24: 136–140.
Mikulis DJ, Jurkiewicz MT, McIlroy WE, Staines WR, Rickards L, Kalsi-Ryan S et al. Adaptation in the motor cortex following cervical spinal cord injury. Neurology 2002; 58: 794–801.
Freund P, Weiskopf N, Ward NS, Hutton C, Gall A, Ciccarelli O et al. Disability, atrophy and cortical reorganization following spinal cord injury. Brain 2011; 134: 1610–1622.
Freund P, Curt A, Friston K, Thompson A . Tracking changes following spinal cord injury: insights from neuroimaging. Neuroscientist 2013; 19 (2): 116–128.
Maynard FM Jr, Bracken MB, Creasey G, Ditunno JF Jr, Donovan WH, Ducker TB et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Tomberg T, Braschinsky M, Rannikmäe K, Kepler J, Kepler K, Kõrv J et al. Functional MRI of the cortical sensorimotor system in patients with hereditary spastic paraplegia. Spinal Cord 2012; 50: 885–890.
Mazziotta J, Toga A . A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM). Philos Trans R Soc Lond B Biol Sci 2001; 356: 1293–1322.
Rorden C, Brett M . Stereotaxic display of brain lesions. Behav Neurol 2000; 12: 191–200.
Brett M, Anton J-L, Valabregue R, Poline J-B . Region of interest analysis using an SPM toolbox (abstract). Presented at the 8th International Conference on Functional Mapping of the Human Brain,, 2–6 June 2002, Sendai, Japan. Available on CD-ROM in NeuroImage. Vol. 16, No. 2.
Wilke M, Schmithorst V J . A combined bootstrap/histogram analysis approach for computing a lateralization index from neuroimaging data. Neuroimage 2006; 33: 522–530.
Freund P, Wheeler-Kingshott CA, Nagy Z, Gorgoraptis N, Weiskopf N, Friston K et al. Axonal integrity predicts cortical reorganisation following cervical injury. J Neurol Neurosurg Psychiatry 2012; 83: 629–637.
Curt A, Alkadhi H, Crelier GR, Boendermaker SH, Hepp-Reymond MC, Kollias SS . Changes of non-affected upper limb cortical representation in paraplegic patients as assessed by fMRI. Brain 2002; 125: 2567–2578.
Lotze M, Laubis-Herrmann U, Topka H, Erb M, Grodd W . Reorganization in the primary motor cortex after spinal cord injury—a functional magnetic resonance (fMRI) study. Restor Neurol Neurosci 1999; 14: 183–187.
Streletz LJ, Belevich JK, Jones SM, Bhushan A, Shah SH, Herbison GJ . Transcranial magnetic stimulation: cortical motor maps in acute spinal cord injury. Brain Topogr 1995; 7: 245–250.
Chen R, Cohen LG, Hallett M . Nervous system reorganization following injury. Neuroscience 2002; 111: 761–773.
Kokotilo KJ, Eng JJ, Boyd LA . Reorganization of brain function during force production after stroke: a systematic review of the literature. J Neurol Phys Ther 2009; 33: 45–54.
Acknowledgements
This study was supported by the Estonian Science Foundation research grant number 7868 and the targeted financing from the Estonian Ministry of Education and Research number SF0180064s07. We thank the nurses of the Radiology Clinic, Tartu University Hospital, for their kind help in performing the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sabre, L., Tomberg, T., Kõrv, J. et al. Brain activation in the acute phase of traumatic spinal cord injury. Spinal Cord 51, 623–629 (2013). https://doi.org/10.1038/sc.2013.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.41
Keywords
This article is cited by
-
Brain activation in the chronic phase of traumatic spinal cord injury
Spinal Cord (2016)