Abstract
Study design:
The study is conducted on the basis of comparative-repeated measures.
Objectives:
The objective of this study is to assess the reliability of non-invasive cardiac output (CO) measurements in individuals with tetraplegia (TP) at rest and during exercise using Innocor, and to test the hypothesis that CO measurements are less reliable in TP than in able-bodied (AB) individuals.
Setting:
Ambulatory volunteers, Switzerland.
Methods:
Nine male motor-complete TP (C5–C7) and nine pair-matched AB performed repeated CO measurements at rest and during submaximal arm-crank and wheelchair exercises in four different test sessions. Within- and between-day reliabilities were compared between TP and AB.
Results:
Mean differences between measurements at rest (TP vs AB, within-day: 0.1±0.5 vs 0.2±0.6 l min−1, between-day: −0.7±0.6 vs −0.1±0.8 l min−1), during arm-crank (TP vs AB, within-day: 0.1±0.9 vs 0.5±0.7 l min−1, between-day: −0.3±1.1 vs 0.0±1.1 l min−1) and wheelchair exercises (TP vs AB, within-day: 0.3±1.2 vs –0.1±0.8 l min−1, between-day: 0.1±1.1 vs 0.5±0.9 l min−1) were not significantly different between TP and AB (all P>0.05). Coefficients of variation in TP (within-day, rest: 6.8%, arm-crank: 9.6% and wheelchair: 10.8%; between-day, rest: 11.9%, arm-crank: 11.2% and wheelchair: 10.3%) and in AB (within-day, rest: 7.7%, arm crank: 6.8% and wheelchair: 6.0%; between-day, rest: 9.2%, arm crank: 8.5% and wheelchair: 8.0%) indicated acceptable reliability.
Conclusion:
In contrast to our hypothesis, we found non-invasive CO measurements using Innocor to be as reliable in TP as they are in AB. Consequently, Innocor can be recommended for repeated assessments of CO in TP within routine diagnostics or for evaluation of training progress.
Sponsorship:
The study was supported by the Swiss National Science Foundation (Grant no. 32–116777).
Similar content being viewed by others
Introduction
Cardiovascular disease is a major cause of death also in individuals with tetraplegia (TP), partly due to reduced cardiorespiratory fitness.1, 2 Physical training improves cardiorespiratory fitness and the associated risk factors.3 To determine the most efficient cardiovascular training mode, to verify training effects and to evaluate cardiovascular limitations, it is important to assess cardiac function. Although in able-bodied individuals (AB), heart rate is often used as an estimator of cardiac function during exercise, this variable is not sufficient as the only measurement in TP. Owing to the disturbed sympathetic nervous system, cardiovascular adaptations to exercise differ from those in AB,4 for example, heart rate reserve is reduced and vasomotor regulation is impaired. Thus, the measurement of cardiac output (CO) allows better characterization of cardiac function and the efficiency of cardiovascular training modalities. The primary stimulus to elicit cardiovascular training adaptations is adequate volume loading of the heart. Volume loading is, in part, reflected by the stroke volume, which can be derived from concomitant assessment of CO and heart rate. Gold standard methods, such as direct Fick, dye-dilution or thermodilution to assess CO are invasive, and therefore not appropriate for regular monitoring.5 Alternatively, non-invasive techniques such as carbon dioxide or inert gas rebreathing can be used to measure cardiac function. Innocor (Innovision, Odense, Denmark), a system using inert gas rebreathing, proved to be a reliable non-invasive tool to measure CO at rest6, 7, 8 and during exercise in AB,8 and showed consistency with gold standard methods.9, 10, 11 In addition, the Innocor device can estimate pulmonary shunts and evaluate the degree of gas mixing. Therefore, CO might be more precisely assessed by this method than by carbon dioxide rebreathing.6
Despite being a simple and comfortable measurement procedure, a critical requirement to obtain valid measurements has been reported as being the ability to rebreathe 40% of the predicted vital capacity during four consecutive breaths within 20 s to assure complete alveolar mixing of the test gases.12 As TP is associated with a number of pulmonary-related impairments, including compromised lung function, resulting partly from the low active respiratory muscle mass,13 feasibility of CO measurement with Innocor needs to be evaluated in TP.
Although feasibility and reliability of CO measurements have been previously determined during submaximal arm exercise in individuals with spinal cord injury by carbon dioxide rebreathing, and acceptable reliability was obtained,14 specific analyses for TP were not reported and between-day reliability was not assessed. Evaluating between-day reliability is important when considering repeated CO measurements in the course of a progressing disease or training. Between-day reliability may be affected by differences in sleep duration/quality, diet composition or by the disturbed vasomotor regulation in TP.4 Thus, evaluating a homogeneous group of TP is essential, as potential sources of measurement error might specifically relate to TP.
Therefore, the aim of the present study was to determine the reliability of CO measurement by Innocor at rest and during exercise in TP and to compare these results with AB. To test this, TP and AB performed CO measurements on different days at rest, during arm-crank and wheelchair exercises. We hypothesized that the reliability of CO measurements at rest and during exercise would be lower in TP compared with AB because of changes in autonomic function and its consequences on vasomotor regulation and cardiac control.
Materials and methods
Subjects
Nine male TP (age 43±12 years, height 178±7 cm and weight 69±12 kg) with traumatic spinal cord injury American Spinal Injury Association Impairment Scale A or B (two C5, three C6 and four C7, time since injury 18±11 years) and nine pair-matched AB (age 42±12 years, height 177±7 cm and weight 73±10 kg; all P>0.05 vs TP) participated in the study. Vital capacity was significantly lower in TP (4.1±0.4 l, 85±11% predicted) compared with AB (5.7±1.4 l, 120±30% predicted). After detailed information about the study protocol and testing procedures, subjects gave their written informed consent. The protocol was approved by the Ethics Committee of the canton of Lucerne (Switzerland). The study was performed according to the Declaration of Helsinki. Subjects were required to refrain from strenuous physical activity for 48 h before the day of testing. Drinking caffeinated or alcoholic beverages on test days was forbidden and no food intake was allowed within the last 2 h before testing.
Study protocol
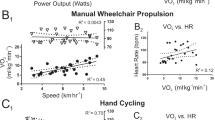
The experiments were conducted in four test sessions as depicted in Figure 1.
Session A
Lung function was assessed according to standard procedures15 using a body plethysmograph (MasterLab, Jaeger, Wuerzburg, Germany). After that, the pressure of the wheelchair tires was adjusted to 6.5 bar. Then a facemask (Hans Rudolph, Shawnee, KS, USA) and a forehead pulse oximeter sensor (8000R, Nonin Medical, Plymouth, MN, USA) were fitted to the subjects and connected to the Innocor system. Thereafter, three-practice CO measurement maneuvers, without test gas, were followed by two resting CO measurements (A1, A2, each preceded by 5 min of quiet breathing). Afterwards, subjects were randomized and assigned to start with the arm-crank test followed by the wheelchair test or viceversa. Both tests included 5 min of resting measurements followed by 8 min of exercise at constant loads of 15 W. The CO measurements (for details, see below) were started after 3:40 (A4) and 7:40 min (A8) of exercise. Ventilation and gas exchange were recorded breath by breath using the Innocor device. The tests were separated by 20 min.
Arm-crank exercise tests were conducted with an electromagnetically braked, synchronous arm-crank ergometer (Ergoline, Hoechberg, Germany). The center of the crank-shaft was set at the same height as the shoulder joint of the subjects. The elbow was slightly bent when the arm was outstretched, and the hands were fixed with bandages. The work rate was 15.0±0.0 W and the push rate was 61±2 r.p.m.
Wheelchair tests were conducted on a treadmill (Treadmill Giant, Bonte Zwolle, Netherlands) with a moving rail to prevent potential falls from the treadmill. Before each wheelchair test, a drag test was performed to determine the treadmill's velocity for the following wheelchair test. A detailed description of the drag test can be found elsewhere.16 The work rate during the test was 15.2±0.3 W and the push rate was 50±6 r.p.m. Mean velocities were 2.7±0.3 and 3.0±0.5 km h−1 for TP and AB, respectively. The slope was set at 1.5% with two exceptions (one TP: 1%, one TP: 2%).
Session B
Session B was identical to session A.
Sessions C and D
Resting measurements were performed similar to sessions A and B. Thereafter, exercise tests were performed that do not belong to the scope of the present study. However, resting values of these two sessions were included to investigate potential systematic errors due to learning effects over repeated sessions.
CO measurement using Innocor
Before taking the CO measurement, a rebreathing bag was filled with a specific gas mixture, consisting of 28% oxygen, 0.5% nitrous oxide and 0.1% sulphur hexafluoride in nitrogen. The filling volume was set at 40% of the subject's predicted vital capacity. If this was not achieved by the TP, then the filling volume was set at 44% of the effective vital capacity for TP. CO measurements were performed at a breathing frequency of 18–22 breaths per minute over a maximum of 20 s. Heart rate was derived from the pulse oximeter. Stroke volume was derived from CO and heart rate. CO measurements were carried out by one operator.
Data analysis
Within- and between-day reliabilities were evaluated by calculating the bias (difference between two measurements) ± 95% limits of agreement (LOA: ±1.96 × s.d. of the bias), coefficients of variation (CVs), and intra-/interclass correlation coefficients (ICCs), as suggested by Atkinson and Nevill.17
First, we performed repeated measures analysis of variance with Bonferroni–Holm correction for between- and within-pairs bias for resting values and Student's paired t-tests for exercise data. As no significant differences were found and bias ± LOA for the separate sessions were similar, thus, within-day pairs for resting values (A1/A2, B1/B2, C1/C2 and D1/D2) were pooled.18 Similarly, within-day pairs of exercise values (A4/A8 and B4/B8) were pooled. The same was carried out for between-day pairs of resting (A1/B1, A2/B2, C1/D1 and C2/D2) and exercise values (A4/B4 and A8/B8). We then recalculated the bias±LOA for the pooled data. CVs (100 × (s.d.)/mean) were calculated for each session separately and then averaged. ICCs were calculated using a one-way random effects model, expressed as single-measures reliability.
Absolute physiological values were evaluated by using paired and unpaired Student's t-tests to test for significant differences within or between different conditions and between TP and AB. For this purpose, oxygen consumption was averaged over the second to fourth minute at rest, and over 30 s before the start of the CO measurement during exercise. Then oxygen consumption and hemodynamic parameters of resting measurements in sessions A–D were averaged, and exercise values for sessions A and B were averaged for arm-crank and wheelchair exercises, separately.
Analyses were performed using SPSS 17.0 (SPSS, Chicago, IL, USA) and Prism 5.0 (GraphPad, San Diego, CA, USA) and statistical significance was accepted for P<0.05.
We certify that all the applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during the course of this research.
Results
From a total of 144 CO measurements in each group, nine CO measurements had to be excluded (TP: n=4; AB: n=5) because of incomplete gas mixing or technical problems.
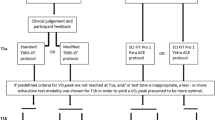
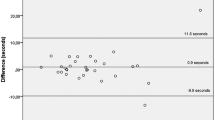
Bias ± 95% limits of agreement
Within-day CO bias at rest (Figure 2) and during exercise (Figure 3) was not significantly different between TP and AB (all P>0.05). Between-day LOAs were wider compared with within-day LOAs for all measures and conditions (Table 1).
Bland–Altman plot of within-day cardiac output comparisons at rest. Results of duplicate cardiac output measurements at rest (measurements: n=72 in individuals with tetraplegia, n=70 in able-bodied individuals). The differences of two measurements are plotted against their mean value. CO, cardiac output.
Bias of within-day cardiac output comparisons during exercise. Mean difference (bias) between cardiac output measurements ending at 4 min and 8 min of exercise (measurements: AC n=34, WC n=30 in individuals with tetraplegia; AC n=34, WC n=30 in able-bodied individuals). CO, cardiac output; WC, wheelchair exercise; AC, arm-crank exercise.
Coefficients of variation
Coefficients of variation are shown in Table 2. Within-day CO CVs in TP were generally smaller in resting compared with exercise measurements (rest 6.8%, arm crank 9.6% and wheelchair 10.8%). The highest CVs were found for stroke volume during exercise in TP. The smallest CVs were found for heart rate in both groups for all conditions.
Intra- and interclass correlation coefficients
ICCs are shown in Table 3. Overall ICCs were slightly lower in TP compared with AB.
Hemodynamic parameters and oxygen consumption
The values of cardiac output, heart rate and oxygen consumption were significantly greater during exercise compared with at rest in both groups (Table 4) and were greater for AB compared with TP. Stroke volume increased during exercise in AB but not in TP.
Discussion
Non-invasive CO measurement assessed with Innocor demonstrated acceptable reliability at rest and during exercise. Our hypothesis that the reliability of CO measurements in TP compared with AB would be lower was rejected. Thus, differences in cardiovascular control between TP and AB did not substantially affect the reliability of these measurements.
Although TP showed lower ICCs compared with AB, ICCs should be interpreted with caution, as they have the major limitation of depending heavily on the range of values, and they are specific for the individuals in this sample only. The consideration of the CVs might therefore be more relevant as they cover 68% of the variability that is actually present in repeated measurements for an average individual. CVs of CO at rest (TP: 6.8%; AB: 7.7%) in our study demonstrated good reliability compared with gold standard methods in which within-day CVs are generally 5–10%.5
Furthermore, CVs of resting assessments in TP and AB compare well with those of Fontana et al.8 who found within-day CVs of 8.6% and between-day CVs of 10.0% in resting AB, using the Innocor system. During submaximal leg exercise in AB, Fontana et al.8 found CVs ranging from 4.3 to 6.4%, whereas CVs during arm exercise in the present study appeared slightly higher (TP: 9.6–11.2%; AB: 6.0–8.5%). Arm movements represent a possible source of error during rebreathing. In particular, TP rely also on arm and upper chest muscles to support respiration.19 However, the importance of these considerations seems negligible, as CVs were still in an acceptable range compared with other invasive or non-invasive methods for CO determination.5
We observed that the major contribution to CO variability originated from stroke volume variability shown by higher CVs in stroke volume compared with heart rate, in which CVs were constantly low in both groups. In addition, TP had slightly higher stroke volume CVs than AB, possibly because of larger breathing irregularities with arm exercise compared with AB, leading to transient changes in intrathoracic or intra-abdominal pressure swings,20 or abnormal vasomotor regulation, both factors that could influence venous return and therefore stroke volume.
Interestingly, absolute physiological responses to exercise were different between TP and AB, despite using the same exercise protocol. For example, stroke volume did not increase in TP in contrast to AB. This lack of increase with exercise likely results from a lack of increase in venous return related to an inefficient vasoconstrictor response in non-working muscles. Apparently, the reliability of CO measurements is independent of the magnitude of the values in this setting, shown by comparable measures of reliability in TP and AB.
Clinical relevance
We conclude that the Innocor device is suitable for routine CO assessment, as familiarization and measurement procedures were not time consuming, systematic errors due to learning effects were not observed and the quality of the obtained measurement could be easily verified by adhering to strict criteria. To evaluate cardiac function in TP, heart rate as a single measure is not sufficient because of cardiovascular restrictions related to the changed function of the autonomic nervous system. Therefore, CO measurements are necessary to obtain important information (for example, stroke volume) of the cardiovascular response to exercise and/or training to ultimately enhance cardiovascular health in TP. Regarding the reliability of the CO measurements, a certain amount of random error due to biological or mechanical variations cannot be avoided, thus, is the Innocor device precise enough to be of practical use to assess CO in TP? From the present data, LOAs predict that 95% of future CO measurements will deviate between −0.9 to 1.1 l min−1 in TP and −1.0 to 1.5 l min−1 in AB from a previous measurement. These values are similar compared with the values found by Peyton et al.7 in AB (−0.88 to 0.88 l min−1) using Innocor. In view of the present results, we support those authors recommendation to perform two or more measurements (depending on the degree of precison needed) and to use the average of these measurements when assessing CO. Importantly, Atkinson and Nevill17 pointed out that it is the task of the scientist, physician or coach to judge whether LOAs are narrow enough for the test to be of practical use. To decide, it might be helpful to calculate the sample size required to detect between-day CO changes of 1.5–2.0 times the CV18 for future CO measurements. On the basis of current findings, a training study able to detect CO changes of 15% during exercise, calculated based on 80% power and a two-sided test with P<0.05 for significance, would need to include thirteen TP.
Technological considerations
First, the sample size in our study was small, but the inclusion criteria restricted the available number of active and otherwise healthy volunteers with TP. To partly overcome this issue, we increased the number of sessions to improve the statistical power and we included a matched group of AB for comparison.
Second, our findings account for submaximal exercise. It might be easier to perform the rebreathing maneuvers at submaximal exercise compared with maximal exercise, in which, for example, the coordination could be more challenging, particularly for TP. Also, at maximal arm exercise, measurement errors due to arm movements, or breathing irregularities might be more pronounced.
Third, our study design does not address the validity of CO measurements with Innocor in TP. As determination of the validity would require cardiac catheterization to compare CO measurements of Innocor with CO measurements from the Fick method, we reasoned that the invasiveness of the measurement would reduce the pool of available volunteers wanting to participate in our study. In addition, the risks and possible complications associated with heart catheterization and a sudden occurrence of autonomic dysreflexia would not warrant its use in healthy TP.
Conclusions
In summary, Innocor provides reliable CO measurements for TP at rest and during exercise. These results add to the existing literature related to inert gas rebreathing by providing within- and between-day reliability analyses of CO and stroke volume during exercise. Innocor provides a non-invasive alternative for routine evaluation of cardiac function as well as for monitoring progression of disease or improvement of cardiac function during rehabilitation or training in TP.
References
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
Myers J, Lee M, Kiratli J . Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil 2007; 86: 142–152.
Blomqvist CG, Saltin B . Cardiovascular adaptations to physical training. Annu Rev Physiol 1983; 45: 169–189.
Krassioukov A . Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol 2009; 169: 157–164.
Warburton DE, Haykowsky MJ, Quinney HA, Humen DP, Teo KK . Reliability and validity of measures of cardiac output during incremental to maximal aerobic exercise. Part I: conventional techniques. Sports Med 1999; 27: 23–41.
Jakovljevic DG, Nunan D, Donovan G, Hodges LD, Sandercock GR, Brodie DA . Comparison of cardiac output determined by different rebreathing methods at rest and at peak exercise. Eur J Appl Physiol 2008; 102: 593–599.
Peyton PJ, Bailey M, Thompson BR . Reproducibility of cardiac output measurement by the nitrous oxide rebreathing technique. J Clin Monit Comput 2009; 23: 233–236.
Fontana P, Boutellier U, Toigo M . Reliability of measurements with Innocor during exercise. Int J Sports Med 2009; 30: 747–753.
Agostoni P, Cattadori G, Apostolo A, Contini M, Palermo P, Marenzi G et al. Noninvasive measurement of cardiac output during exercise by inert gas rebreathing technique: a new tool for heart failure evaluation. J Am Coll Cardiol 2005; 46: 1779–1781.
Gabrielsen A, Videbaek R, Schou M, Damgaard M, Kastrup J, Norsk P . Non-invasive measurement of cardiac output in heart failure patients using a new foreign gas rebreathing technique. Clin Sci (Lond) 2002; 102: 247–252.
Peyton PJ, Thompson B . Agreement of an inert gas rebreathing device with thermodilution and the direct oxygen Fick method in measurement of pulmonary blood flow. J Clin Monit Comput 2004; 18: 373–378.
Kallay MC, Hyde RW, Smith RJ, Rothbard RL, Schreiner BF . Cardiac output by rebreathing in patients with cardiopulmonary diseases. J Appl Physiol 1987; 63: 201–210.
Brown R, DiMarco AF, Hoit JD, Garshick E . Respiratory dysfunction and management in spinal cord injury. Respir Care 2006; 51: 853–868 discussion 869–870.
Myers J, Brown H, Smith S, Perkash I, Kiratli BJ . Reproducibility of noninvasive cardiac output during arm exercise in spinal cord injury. J Rehabil Res Dev 2007; 44: 547–552.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338.
de Groot S, Zuidgeest M, van der Woude LH . Standardization of measuring power output during wheelchair propulsion on a treadmill Pitfalls in a multi-center study. Med Eng Phys 2006; 28: 604–612.
Atkinson G, Nevill AM . Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med 1998; 26: 217–238.
Hopkins WG . Measures of reliability in sports medicine and science. Sports Med 2000; 30: 1–15.
Lucke KT . Pulmonary management following acute SCI. J Neurosci Nurs 1998; 30: 91–104.
Willeput R, Rondeux C, De Troyer A . Breathing affects venous return from legs in humans. J Appl Physiol 1984; 57: 971–976.
Acknowledgements
The study was supported by the Swiss National Science Foundation (Grant no. 32–116777). We thank all volunteers for participating in this study, Dr R Briggs for English editing, and Nonin (Nonin Medical) for providing pulse oximeter sensors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest. The Swiss National Science Foundation was not involved in the study design, collection, analysis and interpretation of data, writing of the report or the decision to submit the paper for publication.
Rights and permissions
About this article
Cite this article
Hostettler, S., Brechbühl, J., Leuthold, L. et al. Reliability of non-invasive cardiac output measurement in individuals with tetraplegia. Spinal Cord 49, 665–671 (2011). https://doi.org/10.1038/sc.2010.173
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.173
Keywords
This article is cited by
-
Hemodynamic and cardiorespiratory responses to various arm cycling regimens in men with spinal cord injury
Spinal Cord Series and Cases (2019)