Abstract
Study design
Descriptive study.
Objectives
To examine grouped and intra-individual relationships between 1) exercise intensity and heart rate (EI-HR); 2) EI and oxygen uptake (EI-VO2); 3) VO2 and HR (VO2-HR); and 4) perceived exertion and VO2 (PE-VO2) in persons with tetraplegia (C4/5–C8) during different modes of exercise.
Setting
Community in Winnipeg, Canada.
Methods
Participants exercised at 3 graded intensities during arm ergometry (ERG), wheeling indoors on cement (MWC), or hand-cycling outdoors (HC). EI (Watts, km/hr) and VO2, HR and PE were recorded.
Results
22 persons completed ERG, 14/22 also completed MWC and 5/22 completed ERG, MWC and HC. Regression analysis of grouped data showed a significant relationship between EI-VO2 but not for EI-HR or HR-VO2. Intra-individual analyses showed a strong correlation (r or ρ > 0.7) for VO2-HR for 16/22 during ERG. In the participants completing multiple exercise modes, a strong VO2-HR relationship was present in 12/14 in ERG, but in only 6/14 in MWC. The 5 persons exercising with all 3 modes had a strong HR-VO2 relationship in 5/5 for ERG, 2/5 in MWC and 1/5 in HC. A strong relationship for PE-VO2 was observed in a higher proportion of participants (versus HR-VO2) during MWC (9/14) and HC (2/4).
Conclusion
Within the same individual, the HR-VO2 relationship varies across modes, despite exercising over similar ranges of steady-state VO2. HR appears less able to predict VO2 compared to PE. Based on these new findings, systematic investigation of the HR-VO2 relationship across modes of exercise in tetraplegia is warranted.
Similar content being viewed by others
Introduction
Tetraplegia comprises 40–60% of the population with traumatic spinal cord injury [1, 2]. Obesity, cardiovascular disease, and type II diabetes occur at much higher rates after spinal cord injury (SCI), and those with tetraplegia are at even higher risk than those with paraplegia [3,4,5]. Since these diseases are caused mainly by inadequate activity of a sufficient intensity and are related to obesity, many studies have attempted to determine the ‘sufficient’ level of exercise needed to confer a health benefit to persons living with SCI.
Recently updated guidelines recommend 3–5 sessions per week of 20–30 min upper body aerobic exercise at ‘moderate to vigorous intensity’ to improve cardiorespiratory fitness in individuals with SCI [6, 7]. However, these and other authors acknowledge that the vast majority of exercise studies rely solely, or mainly, on participants with paraplegia and have concluded there is insufficient data to make tetraplegia-specific exercise recommendations [6, 8]. Exercise intervention studies that do include sufficient numbers of participants with tetraplegia show relatively small improvements in body composition and non-significant changes in vascular health [9]. It is unclear why participants with tetraplegia demonstrate such relatively small improvements when exercising at moderate to vigorous intensity. Moderate to vigorous aerobic exercise intensity is defined as 60–65% peak oxygen uptake (VO2) or 60–80% of peak heart rate (HR). However, impairment of sympathetic nervous system function severely limits exercise capacity and exercise response in persons with complete tetraplegia such that peak HR is less than 130 bpm and peak VO2 is less than 20 mg.kg−1.min−1, even in paralympic athletes [10,11,12]. Thus, exercise prescription at moderate to vigorous intensity based on HR or VO2 may not be appropriate or sufficient in this population to confer a health benefit. Another surrogate measure of exercise intensity (EI) validated in the general population is rating of perceived exertion (PE) [13]. In addition to HR, VO2, and PE, absolute measures of EI such as speed or power output (PO) should relate directly to VO2, but may not be useful for EI prescription as they do not account for the physiological capacity of each individual or other external factors (e.g., terrain, mechanical efficiency).
Positive and strongly predictive linear relationships between PE and HR and VO2 have been demonstrated and validated for the active and sedentary general population [14, 15], and for those with SCI below T6 [16, 17]. However, results on whether HR can be used to reliably predict VO2 in tetraplegia are mixed, and some authors suggest that a linear VO2-HR relationship is more likely in those with lower-level tetraplegia [18,19,20,21]. Whether PE can be used to predict PO or VO2 in those with tetraplegia is unclear, with some reporting strong reliability for predicting peak oxygen uptake during manual wheeling, while others show it may only be useful at relatively low levels of intensity or in trained athletes [22,23,24,25,26]. Authors of a recent systematic review concluded that there was insufficient research evidence of suitable quality to provide a strong recommendation for using PE to assess aerobic exercise intensity in the SCI population as a group [27]. Comparison of HR versus PE suggests PE may be a more reliable indicator of absolute work effort during wheeling in trained wheelchair athletes with para- or tetraplegia [28]. For these reasons, we tested participants with a range of tetraplegia level injury (C4/5–C8) across three different modes of steady-state exercise and compared the reliability of HR and PE to assess objective measures of exercise intensity (EI). Thus our objectives were to determine if either 1) HR or 2) PE can reliably predict oxygen uptake (VO2) or absolute measures of EI during different modes of steady-state exercise in the same study participants.
Participants and methods
Participant recruitment
Adults with tetraplegia (n = 25) of at least one-year duration were recruited by word of mouth, from the Manitoba Wheelchair Sport Rugby Team, the Manitoba Division of the Canadian Paraplegic Association and flyers posted at the SCI outpatient clinic at the Health Sciences Centre in Winnipeg. Participant characteristics were previously published and consistent with historically reported features of persons with tetraplegia, in terms of range(s) of injury level (C4/5–C8), gender (80% male) and injury completeness [~25% incomplete and ambulatory [29]]. Measurements took place over 2–4 visits at generally the same time of day. Participants were advised not to engage in strenuous exercise the day preceding testing.
Exercise modes and equipment
Steady-state exercises were performed based on participant capabilities and using personal wheelchairs and hand-cycles (1 add-on; 3 touring, non-recumbent). Arm crank ergometry was performed on a calibrated SCIFit height adjustable arm ergometer, or a table-mounted calibrated Colorado arm crank ergometer. Manual wheeling was performed on a large level indoor cement track, and hand-cycling outdoors on a 400 m track or on the University Campus streets. A bicycle odometer transmitter was placed on each participant’s wheel for real-time monitoring of speed to maintain a steady pace during each trial. The actual wheel rotations were documented using a G-Link accelerometer mounted on a rear-wheel axis. Measurement of each person’s wheel circumference allowed conversion of rotations to distance and speed. Accelerometer data were downloaded and files converted for subsequent analysis of rates using custom-developed in-house Spinal Cord Research Centre software and Microsoft Excel (2010, 2011Mac). Participants were monitored for symptoms of autonomic dysreflexia, and the exercise protocol was stopped until the symptoms subsided. Data collected during the episode were not analyzed and testing resumed in the 3 participants once symptoms subsided.
Oxygen uptake measurement during sub-maximal multi-stage exercise
Oxygen uptake and carbon dioxide production were measured using the Jaeger Oxycon Mobile (Carefusion Respiratory Care, Yorba Linda, CA) exercise testing system. Gas analysers were calibrated and the system thermostated and compensated for barometric pressure and environmental humidity variations before each test, according to the manufacturer’s recommendations (Jaeger Oxycon User Manual). Heart rate was monitored continuously with a Polar chest strap or Jaeger ear clip-based sensor, based on user preference and occasionally when movement artifact interfered with chest strap signals. Each person rested with the equipment for at least three minutes before testing. Activities were undertaken for a minimum of 3 min (after attaining a particular speed or power output). Speeds and power outputs were self-selected to represent the range of intensities normally undertaken with each activity based on a pre-test in which participants were tested to identify the highest level of activity they could maintain for a minimum three-minute period, as previously described [29]. The target was 3 sub-maximal stages, at a low, medium, and high intensity of exercise for each mode. For example, if a participant had a peak steady-state PO of 30 W during ERG, they would perform exercise at 20, 25 and 30 W for their three stages. Post-hoc analysis revealed that most persons ‘low’ EI for one mode of exercise was, on average, within 16% of the ‘low’ EI for any other mode of exercise performed. In addition, some were only able to engage in one or two levels of output, based on their injury and fitness level. Data is included only for those who completed at least two stages (n = 22).
VO2, HR, and EI were recorded every 5 s and data averaged over 30 s epochs for each steady-state trial. The coefficient of variation was calculated for each steady-state trial. Data points with co-efficient of variation ≤10% were included. PE was recorded at the end of each steady-state trial (at the end of each intensity trial) and participants monitored their absolute intensity to maintain the same output for the duration of the trial. Accelerometers mounted on the ERG, MWC and HC were analyzed later and confirmed a CV < 5% was maintained during each trial for each participant. For individual analyses, only participants with at least 8 data points were included (n = 22 persons, 126 trials, 69 during ERG, 40 during MWC and 17 during HC). In grouped analysis, all trials were pooled.
Ratings of perceived exertion
The 0–10 category ratio (CR) score of PE [13] was selected because it has been used in this population previously [30] and it is more useful for participants with tetraplegia due to lost sympathetic input and related inability to increase HR beyond ~130 bpm. We presented each participant with a laminated 8 × 10 paper copy of the 10-point visual scale and explained the scale with consistent examples. Because they were masked, we explained that they should respond by nodding their head when the investigator’s finger pointed to the correct number on the 10-point scale. Each participant was asked to rank his or her PE at the end of each set of steady-state exercise, for each intensity. We re-affirmed their selection by stating the number back to them and asking them to nod if correct.
Statistical analysis
For our initial analysis we used grouped data and linear regression analysis to examine the strength of relationships between the controlled variable (PO or speed) and VO2 and HR as described previously in this population [19, 31]. Subsequently, we performed individual analyses of correlation (Pearson or Spearman) to examine the strength of the relationship between and HR and VO2 and between RPE and VO2 for each individual during different modes of exercise[18, 20]. All statistical analyses were performed using GraphPad Prism statistical software (version 7 or 8; GraphPad Software, La Jolla, California, USA). The D’Agostino and Pearson omnibus test determined whether data were normally distributed. Based on the results from normality testing, results are reported as either r-values for parametric Pearson correlations or as ρ-values for non-parametric Spearman correlations with r or rho ≥ 0.7, or R2 ≥ 0.49 considered as strong [32]. The co-efficient of determination (r-squared, R2) is reported for linear regression analyses; residuals were normally distributed unless otherwise noted. Correlations with fewer than eight pairs are not reported, due to their N being too small for normality testing.
Results
Overall, 22 participants performed ERG, 14 performed ERG + MWC and 5 performed ERG + MWC + HC. Regression analysis of grouped data showed a strong and significant relationship for PO to predict VO2 (Fig. 1A1–C1, bottom, all R2 ≥ 0.38) whereas R2 values describing the relationship between HR and PO or HR and VO2 were negative (HC) or showed a very poor and non-significant relationship during each of ERG (R2 = 0.049 for PO vs VO2; R2 = 0.059 for VO2 vs HR), MWC (R2 = 0.0043 for speed vs VO2; R2 = 0.12 for VO2 vs HR) and HC [(R2 < 0 for speed vs VO2; R2 = 0.19 for VO2 vs HR); Fig. 1: A1–C1 top versus (vs.) A2–C2]. Thus, as a group VO2, but not HR, was related to absolute measures of EI (PO or speed) during different modes of exercise.
A clear correlation between PO and VO2 was present during arm ergometry (A1, bottom, p < 0.0001), wheeling (B1 bottom, p = 0.0002), and hand cycling (C1 bottom, p = 0.03), black circles, whereas less than 19% of the variation in either PO or VO2 was shared with heart rate variation during arm ergometry (A1 top, A2) wheeling (B1 top, B2), or hand-cycling (C2), open triangles, all p > 0.05. Although 70% of variation in speed related to variation in heart rate during hand cycling, the relationship was negative (C1 top). Dotted lines show the 95% confidence interval. The residuals of regression analysis for oxygen uptake (VO2) vs. heart rate during arm ergometry (A2), hand cycling (C2), and for speed vs. heart rate (B1) failed normality testing.
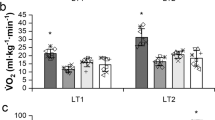
To overcome the limitations of grouped regression analysis of these relationships, we then assessed the individual correlation values between HR and VO2 for each study participant for each mode of exercise they completed (69 trials of ERG, 40 trials of MWC and 17 trials HC). Comparison of intra-individual correlation data in Fig. 2 showed a strong correlation [r or ρ ≥ 0.7 [32]] for HR vs. VO2 in 16/22 persons during ERG (2A), 6/14 during MWC (2B) and 1/5 during HC (2C). Thus the proportion of persons with a strong HR vs. VO2 correlation coefficient was greater during ERG (73%) vs. MWC (43%) vs. HC (20%). Individual correlation values can be found in Table 1 for ERG, Table 2 for MWC and Table 3 for HC.
Additionally, within the same group of participants, strong correlations between either VO2 and HR or between VO2 and PE was observed more often in ERG vs. MWC and in MWC vs. HC. Graphic summaries of each Pearson or Spearman correlation co-efficient for each of VO2 vs. HR, BORG ratings of perceived exertion (PE) and EI for each of A. arm ergometry (ERG, n = 22); B manual wheelchair propulsion (MWC, n = 14) and C hand cycling (HC, n = 5). Line indicates strong correlation values ≥0.70.
Correlation coefficients between PE and VO2 [≥0.7 (r or ρ)] were observed in 15/21 during ERG; 9/14 during MWC; and 2/4 during HC (Fig. 2A–C, second column ‘vs. PE’). Thus, the proportion of persons with a strong PE vs. VO2 correlation coefficient was greater during ERG (71%) vs. MWC (64%) vs. HC (50%). Further, the reliability for either PE or HR to predict oxygen uptake were similar during ERG (compare ‘vs. HR’ (17/22) to ‘vs. PE’ (15/21) in Fig. 2A) while PE showed greater reliability than HR during MWC (compare ‘vs. HR’ (6/14) to ‘vs. PE’ (9/14) in Fig. 2B). Numbers are too small to comment regarding HC.
Figure 2 also summarizes the correlation coefficients for the absolute EI (watts or km/hr) vs. VO2 for each trial. As expected, individual correlation values for PO/EI vs. VO2 are highest during indoor ERG (17/22) compared to MWC (12/14) or during HC outdoors under different wind conditions (2/5, Fig. 2).
All three modes of exercise were performed in a sub-set of 5 participants, which allowed us to make more direct comparisons of the correlations between HR vs. VO2, between PE and VO2 and between EI and VO2. Figure 3 demonstrates that a strong relationship between HR and VO2 occurred in 5/5 during ERG, 2/5 during MWC and 1/5 during HC. For PE, a strong relationship was observed in 4/5 during ERG, 5/5 during MWC and 2/4 during HC (Fig. 3A2–C2, solid lines). Examining the range of VO2 values for each participant in Fig. 3 demonstrates that the variability for HR to predict VO2 occurred despite exercising over similar ranges of absolute oxygen uptake. For example, participant 23C5/6M (solid triangles) had a VO2 range of ~350–1200 ml/min during ERG (Fig. 3A1) vs. ~400–1200 ml/min during MWC (Fig. 3B1) yet had a Pearson r = 0.94 during ERG and a negative correlation of r = −0.55 during MWC. This variability also occurred over similar ranges of PE (compare PE of 4–9 during ERG (Fig. 3A2) to 1–9 during MWC (Fig. 3B2). Similar ranges in oxygen uptake and PE were observed for the other 4 participants completing all 3 modes of exercise (Fig. 3).
HR showed a strong correlation with VO2 most consistently during arm ergometry (in 5/5, A2) whereas only 2/5 showed a strong correlation during MWC (B2) and 1/5 during HC (C2). Strong correlations between PE and VO2 were present in 4/5 during arm ergometry (A1), 5/5 during MWC (B1) and in 2/4 during HC (C1).
Discussion
We investigated the relationships between VO2, HR, PE, and EI during ERG, MWC and HC in 22 persons living with tetraplegia. As expected, absolute measures of EI were correlated most strongly with VO2. We observed that overall, PE showed greater ability to predict VO2 across different modes of exercise when compared to HR. Further, we showed that the ability of PE and HR to predict VO2 varied within each person across different modes of exercise. This finding was unexpected, and most evident for HR, such that the ability for HR to predict VO2 was greatest in persons during ERG (73%) versus MWC (43%) and versus HC (20%), and suggests that other factors, in addition to absent sympathetic innervation of the heart, contribute to the relationship between HR and oxygen uptake during different forms of exercise.
Several autonomic functions are impaired after tetraplegia that limit exercise performance. With injury above the T1 spinal level, sympathetic neural function is impaired and heat-mediated sweat responses for cooling are typically absent [reviewed in [11]]. Increases in heart rate and cardiac output with increasing physical workload are blunted [33]. Thus increases in heart rate are mediated by removing basal parasympathetic drive, which allows for a small increase in HR with activity that typically peaks at ~130 bpm. Sympathetic descending neural control of the adrenal glands and other systems supporting energy substrate mobilization and use by active tissues is also impaired, such that even after prolonged exercise, athletes with motor complete tetraplegia do not show increases in circulating catecholamines [34] or any change in lipid metabolism [35]. Some have suggested the lack of linear relation between HR and VO2 is due to lower limb venous pooling since supine arm cranking showed a better HR/VO2 relation than arm cranking while seated [36]. However, given that exercising supine may also have allowed some back and arm muscles to contribute more to cranking rather than providing trunk support, it is possible that the stronger relationship between HR and VO2 may have been due in part to exercising at a lower level of peak aerobic capacity while supine. Similar to other studies in participants with tetraplegia our findings were mixed, such that some, but not all, demonstrated a linear relationship between HR and VO2 during arm exercise [18, 20, 22]. Some studies suggested that those with higher-level injury (C5-C6 vs. C7-C8) were less likely to demonstrate a linear relationship [20], whereas others have suggested a linear relationship was only observed while exercising at very low intensity levels [22]. Valent et al., reported that a large VO2 range did not always correspond to a linear HR-VO2 relationship, but participants with a small VO2 range and low physical capacity always had a poor HR-VO2 relationship [20]. We did find that 4/6 participants with low ability for HR to predict VO2 during ERG were participants with higher-level injuries (see Table 1). However, since we compared ability for HR to predict VO2 during different modes of exercise, we also showed the HR-VO2 relationship varied within individuals during different modes of exercise, despite similar levels of oxygen uptake and perceived exertion. It is possible that these relationships may vary day to day, but this remains to be investigated.
It is unclear why the strength of the HR-VO2 relationship varies within individuals with tetraplegia and is greatest during ERG compared to MWC or HC. It is possible that the frequency of the exercise may contribute to the stronger relationship during ERG. In particular, only 6 of the 14 able to perform MWC had r or p ≥ 0.70, whereas 13/14 showed r or p > 0.70 during ERG. These differences occurred despite performing ERG and MWC over similar ranges of VO2 and PE. Further, in the 5 persons capable of performing all 3 exercise modes, the strength of the HR-VO2 relationship decreased from 5/5 during ERG to 2/5 during MWC to 1/5 during HC. Thus even within the same individuals, the strength of the HR-VO2 relationship was decreased during MWC or HC exercise compared to ERG exercise. It is possible that the strength of relationship between oxygen uptake and heart rate deteriorates in situations where a greater muscular influence is required and performed at lower frequencies, as in HC and MWC compared to ERG. During ERG, cycling frequencies were typically >60 rpm per arm, but were performed asynchronously correlating to a total of >120 arm rotations per minute (rpm). HC was performed with synchronous arm cranking, between 30 and 70 rpm. MWC typically involved synchronous pushes at ~0.5 Hz (~30 rpm). Animal research demonstrates that the strength of the hindlimb muscle afferent-evoked pressor-reflex that mediates increases in HR and blood pressure varies depending upon the muscle activated [37]. Given that pressor responses can also be elicited from forelimb muscle afferents [38], it is possible that differences exist in the degree to which pressor-reflexes are elicited in humans during different rates and modes of exercise as well. In the absence of the normal descending activation of HR for persons injured above T1, these local spinal reflex responses may play a relatively greater role in facilitating HR responses during exercise. Thus it would be of interest in future studies to systematically assess whether frequency-based afferent feedback contributes to the ability of HR to increase with increasing intensity of effort in persons with impaired sympathetic innervation of the heart. Other factors such as environmental temperature may also influence this relationship [11].
Because of the limited ability to increase HR, and for HR to correlate with absolute measures of EI after tetraplegia as demonstrated here and elsewhere, surrogate measures of EI, such as PE have been recommended [18]. Recent review of the literature indicated that although further studies were required, PE was cautiously suggested as an adequate measure of EI in persons with SCI, and shows some stability over time with repeated testing when used by trained athletes or at low steady-state levels in non-athletes [23, 24, 26, 27]. Overall we observed that PE was similar to, or more reliable than, HR for correlating with VO2 across modes of exercise. The proportion of persons with PE reliability >0.7 was similar during ERG (71% >0.7 for PE vs. 73% for HR) whereas PE was more reliable (vs. HR) during MWC (64% for PE vs 43% for HR) and during HC (50% for PE vs. 20% for HR). It is quite possible that expertise with the exercise (e.g., MWC) and the ability to physically sense and monitor the absolute intensity of the exercise contributed to the stronger reliability of PE to predict VO2 compared to HR during MWC or HC. Our finding that PE can be more reliable than HR to predict VO2 is consistent with the inability for PE to predict HR reported in other studies [24]. In addition to limited sympathetic innervation of the heart, other sympathetically regulated systems impaired with high-level SCI may contribute to the intra-individual variability in PE reliability with different forms of exercise [e.g., temperature regulation, fat lipolysis, and mobilization: [11]]. Thus, in addition to absolute intensity (or oxygen uptake) other factors, such as the environmental conditions under which the different modes of exercise are performed, or the frequency of muscle activation may contribute to temperature changes or rates of energy substrate mobilization which would influence each person’s rating of PE. In the future, it would be of interest to systematically examine relationships between sympathetically regulated metabolic and homeostatic functions, such as temperature regulation or energy substrate bioavailability, to investigate factors contributing to PE during different forms of exercise in persons with tetraplegia. This would identify strategies that reduce PE for a given absolute intensity of exercise, with the ultimate goal to increase the upper limit of exercise intensity and duration that can be performed. Given that persons with tetraplegia show lower than expected oxygen uptake levels (41–46% VO2peak) when asked to exercise at ‘moderate to vigorous intensity’ (3–6 on the Borg 10-point scale) in a study assessing user preferences regarding four different exercise modes [39], identifying strategies to increase exercise performance in this population would increase the potential health benefit of exercise. As our results were unanticipated, we did not perform peak testing and have each participant exercise at a given percent of his/her VO2peak, which is a limitation of our current study. In the future, it would be of interest to examine the relationship between HR and VO2 for a given % peak VO2 across different modes of exercise, employing repeated-measures correlation to increase the statistical power of the observations.
Conclusion
We demonstrated that 1) although absolute EI was correlated with VO2 during different modes of exercise, 2) HR was inconsistent; and 3) PE correlated with VO2 more often than HR during different modes of exercise. An unexpected finding of the present study was that the correlation between HR and VO2 varied across exercise modes, within the same individual. Given the lack of stable markers of relative exercise intensity (either HR or PE), exercise prescription for those with tetraplegia may be better based on absolute measures of intensity such as power output or speed [e.g., [29, 40]]. However, if using absolute intensity it is important to work at an intensity level that attains the highest weekly volume of activity-based energy expenditure safely possible without increasing risk for over-use injuries.
Data availability
Original excel data files generated and analyzed during the current study are not publicly available due to personal information protection but are available upon reasonable request.
References
Noonan VK, Fingas M, Farry A, Baxter D, Singh A, Fehlings MG, et al. Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology. 2012;38:219–26.
Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6.
Duckworth WC, Solomon SS, Jallepalli P, Heckemeyer C, Finnern J, Powers A. Glucose intolerance due to insulin resistance in patients with spinal cord injuries. Diabetes. 1980;29:906–10.
Groah SL, Weitzenkamp D, Sett P, Soni B, Savic G. The relationship between neurological level of injury and symptomatic cardiovascular disease risk in the aging spinal injured. Spinal Cord. 2001;39:310–7.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr., Waters RL, et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95:2398–407.
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21.
van der Scheer JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Bochkezanian V, Raymond J, de Oliveira CQ, Davis GM. Can combined aerobic and muscle strength training improve aerobic fitness, muscle strength, function and quality of life in people with spinal cord injury? A systematic review. Spinal Cord. 2015;53:418–31.
Totosy de Zepetnek JO, Pelletier CA, Hicks AL, MacDonald MJ. Following the physical activity guidelines for adults with spinal cord injury for 16 weeks does not improve vascular health: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96:1566–75.
Haisma JA, van der Woude LH, Stam HJ, Bergen MP, Sluis TA, Bussmann JB. Physical capacity in wheelchair-dependent persons with a spinal cord injury: a critical review of the literature. Spinal Cord. 2006;44:642–52.
Cowley KC. A new conceptual framework for the integrated neural control of locomotor and sympathetic function: implications for exercise after spinal cord injury. Appl Physiol Nutr Metab. 2018;43:1140–50.
Bhambhani Y. Physiology of wheelchair racing in athletes with spinal cord injury. Sports Med. 2002;32:23–51.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81.
Faulkner J, Eston R. Overall and peripheral ratings of perceived exertion during a graded exercise test to volitional exhaustion in individuals of high and low fitness. Eur J Appl Physiol. 2007;101:613–20.
Kavanagh T, Shephard RJ. Maximum exercise tests on “postcoronary” patients. J Appl Physiol. 1976;40:611–8.
Al-Rahamneh HQ, Eston RG. The validity of predicting peak oxygen uptake from a perceptually guided graded exercise test during arm exercise in paraplegic individuals. Spinal Cord. 2011;49:430–4.
Hjeltnes N. Oxygen uptake and cardiac output in graded arm exercise in paraplegics with low level spinal lesions. Scand J Rehabil Med. 1977;9:107–13.
McLean KP, Jones PP, Skinner JS. Exercise prescription for sitting and supine exercise in subjects with quadriplegia. Med Sci Sports Exerc. 1995;27:15–21.
Coutts KD, Rhodes EC, McKenzie DC. Submaximal exercise responses of tetraplegics and paraplegics. J Appl Physiol. 1985;59:237–41.
Valent LJ, Dallmeijer AJ, Houdijk H, Slootman J, Janssen TW, Hollander AP, et al. The individual relationship between heart rate and oxygen uptake in people with a tetraplegia during exercise. Spinal Cord. 2007;45:104–11.
Leicht CA, Bishop NC, Goosey-Tolfrey VL. Submaximal exercise responses in tetraplegic, paraplegic and non spinal cord injured elite wheelchair athletes. Scand J Med Sci Sports. 2012;22:729–36.
Lewis JE, Nash MS, Hamm LF, Martins SC, Groah SL. The relationship between perceived exertion and physiologic indicators of stress during graded arm exercise in persons with spinal cord injuries. Arch Phys Med Rehabil. 2007;88:1205–11.
Bhambhani YN, Eriksson P, Steadward RD. Reliability of peak physiological responses during wheelchair ergometry in persons with spinal cord injury. Arch Phys Med Rehabil. 1991;72:559–62.
Stewart MW, Melton-Rogers SL, Morrison S, Figoni SF. The measurement properties of fitness measures and health status for persons with spinal cord injuries. Arch Phys Med Rehabil. 2000;81:394–400.
Paulson TA, Bishop NC, Eston RG, Goosey-Tolfrey VL. Differentiated perceived exertion and self-regulated wheelchair exercise. Arch Phys Med Rehabil. 2013;94:2269–76.
Paulson TA, Bishop NC, Leicht CA, Goosey-Tolfrey VL. Perceived exertion as a tool to self-regulate exercise in individuals with tetraplegia. Eur J Appl Physiol. 2013;113:201–9.
van der Scheer JW, Hutchinson MJ, Paulson T, Martin Ginis KA, Goosey-Tolfrey VL. Reliability and validity of subjective measures of aerobic intensity in adults with spinal cord injury: a systematic review. PM R. 2018;10:194–207.
Goosey-Tolfrey VL, Paulson TA, Tolfrey K, Eston RG. Prediction of peak oxygen uptake from differentiated ratings of perceived exertion during wheelchair propulsion in trained wheelchair sportspersons. Eur J Appl Physiol. 2014;114:1251–8.
Shea JR, Shay BL, Leiter J, Cowley KC. Energy expenditure as a function of activity level after spinal cord injury: the need for tetraplegia-specific energy balance guidelines. Front Physiol. 2018;9:1286.
van der Scheer JW, de Groot S, Tepper M, Faber W, group A, Veeger DH, et al. Low-intensity wheelchair training in inactive people with long-term spinal cord injury: A randomized controlled trial on fitness, wheelchair skill performance and physical activity levels. J Rehabil Med. 2016;48:33–42.
Schmid A, Schmidt-Trucksass A, Huonker M, Konig D, Eisenbarth I, Sauerwein H, et al. Catecholamines response of high performance wheelchair athletes at rest and during exercise with autonomic dysreflexia. Int J Sports Med. 2001;22:2–7.
Evans JD. Straightforward statistics for the behavioral sciences. Pacific Grove, CA: Brooks/Cole Publishing; 1996.
Hostettler S, Leuthold L, Brechbuhl J, Mueller G, Illi SK, Spengler CM. Maximal cardiac output during arm exercise in the sitting position after cervical spinal cord injury. J Rehabil Med. 2012;44:131–6.
Ogawa T, Nakamura T, Banno M, Sasaki Y, Umemoto Y, Kouda K, et al. Elevation of interleukin-6 and attenuation of tumor necrosis factor-alpha during wheelchair half marathon in athletes with cervical spinal cord injuries. Spinal Cord. 2014;52:601–5.
Campbell IG, Williams C, Lakomy HK. Physiological and metabolic responses of wheelchair athletes in different racing classes to prolonged exercise. J Sports Sci. 2004;22:449–56.
Figoni SF. Exercise responses and quadriplegia. Med Sci Sports Exerc. 1993;25:433–41.
Mitchell JH, Kaufman MP, Iwamoto GA. The exercise pressor reflex: its cardiovascular effects, afferent mechanisms, and central pathways. Annu Rev Physiol. 1983;45:229–42.
Potts JT, Spyer KM, Paton JF. Somatosympathetic reflex in a working heart-brainstem preparation of the rat. Brain Res Bull. 2000;53:59–67.
Pelletier CA, Ditor DS, Latimer-Cheung AE, Warburton DE, Hicks AL. Exercise equipment preferences among adults with spinal cord injury. Spinal Cord. 2014;52:874–9.
Holmlund T, Ekblom-Bak E, Franzen E, Hultling C, Wahman K. Intensity of physical activity as a percentage of peak oxygen uptake, heart rate and Borg RPE in motor-complete para- and tetraplegia. PLoS One. 2019;14:e0222542.
Acknowledgements
We thank the study participants who generously gave their time to this research.
Funding
The authors acknowledge support from the Natural Sciences and Engineering Research Council of Canada (NSERC) (funding reference no. RGPIN-2015-04810), the Manitoba Spinal Cord Injury Research Committee (Canadian Paraplegic Association (Manitoba) Inc., Rick Hansen Institute, and Government of Manitoba), and a Will-to-Win Professorship.
Author information
Authors and Affiliations
Contributions
KCC identified the research question and KCC and BLS designed the study protocols. All contributed to collecting data from study participants, JRS was responsible for most of the data analysis and writing the first draft of the paper. All three contributed to editing, and KCC wrote the final draft submitted.
Corresponding author
Ethics declarations
Ethics approval
Study procedures used were reviewed and approved by the University of Manitoba Ethics Review Board, and all study participants provided written informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shea, J.R., Shay, B.L. & Cowley, K.C. The ability of heart rate or perceived exertion to predict oxygen uptake varies across exercise modes in persons with tetraplegia. Spinal Cord 59, 1247–1255 (2021). https://doi.org/10.1038/s41393-021-00670-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00670-0
This article is cited by
-
Intensity of overground robotic exoskeleton training in two persons with motor-complete tetraplegia: a case series
Spinal Cord Series and Cases (2023)
-
Sympathetic function as key player in VO2 max and brachial artery diameter
European Journal of Applied Physiology (2023)