Abstract
Hypnotizability, one’s ability to experience cognitive, emotional, behavioral and physical changes in response to suggestions in the context of hypnosis, is a stable neurobehavioral trait associated with improved treatment outcomes from hypnosis-based therapy. Increasing hypnotizability in people who are low-to-medium hypnotizable individuals could improve both the efficacy and effectiveness of therapeutic hypnosis as a clinical intervention. Hypnotizability is associated with dorsolateral prefrontal cortex (DLPFC) functions and connectivity with the salience network, yet there is conflicting evidence as to whether unilateral inhibition of the DLPFC changes hypnotizability. We hypothesized that using personalized neuroimaging-guided targeting to non-invasively stimulate the left DLPFC with transcranial magnetic stimulation (TMS) would temporarily increase hypnotizability. In a preregistered, double-blinded, randomized controlled trial, we recruited a sample of 80 patients with fibromyalgia syndrome, a functional pain disorder for which hypnosis has been a demonstrated beneficial non-pharmacological treatment option. All participants were TMS-naive. Participants were randomly assigned to active or sham continuous theta-burst stimulation over a personalized neuroimaging-derived left-DLPFC target, a technique termed SHIFT (Stanford Hypnosis Integrated with Functional Connectivity-targeted Transcranial Stimulation). We tested our hypothesis using the hypnotic induction profile scores, a standardized measure of hypnotizability. Pre-to-post SHIFT change in the hypnotic induction profile scores was significantly greater in the active versus sham group after 92 s of stimulation (P = 0.046). Only the active SHIFT group showed a significant increase in hypnotizability following stimulation (active: P < 0.001; sham: P = 0.607). As such, modulation of trait hypnotizability is possible in humans using non-invasive neuromodulation. Our findings support a relationship between the inhibition of the left DLPFC and an increase in hypnotizability. Dose–response optimization of spaced SHIFT should be explored to understand the optimal dose–response relationship. ClinicalTrials.gov registration: NCT02969707.
Similar content being viewed by others
Main
Hypnosis, the first Western conception of psychotherapy1, can facilitate treating and managing a host of psychiatric and neurological symptoms2. However, not all people respond equally to hypnosis. Hypnotizability, an individual’s capacity to respond to suggestions given in hypnosis, is a stable neurobehavioral trait comprised of cognitive, neural and behavioral components3,4. Hypnotizability has been demonstrated to moderate the effects of hypnosis-based interventions5, particularly in the reduction of both clinical6 and experimental7 pain. Approximately two-thirds of the general adult population is estimated to be at least somewhat hypnotizable, and 15% are highly hypnotizable8, able to manage clinical pain6 and even undergo surgery without chemical anesthesia using hypnotic analgesia9,10. Hypnotizability has been shown to be a stable trait in individuals throughout adulthood, with 0.7 test–retest correlations over a 25 year interval (from a mean age of 19.5 to 45 years)11. By comparison, test–retest correlations of personality traits and IQ (intelligence quotient) at corresponding ages range between 0.51 and 0.62 (ref. 12). Attempts to modulate trait hypnotizability have been tried for decades. Previous studies have attempted to modify hypnotic responsiveness using psychoactive drugs and other pharmaceutical substances, but with little effect13. Further efforts to enhance hypnotizability using behavioral training approaches14 yielded inconsistent results15 and have generally failed to elicit increases in responsiveness in large numbers of individuals16, with inconsistent results across different laboratories. Lynn and colleagues argued that inherent neurocognitive differences between ‘naturally’ high-hypnotizable and low-hypnotizable individuals had been thought to explain the limits of modifying hypnotizability behaviorally17.
High hypnotizability is associated with altered activations of the prefrontal and anterior cingulate cortices, although other brain regions are involved in hypnosis based on task demands18. Responsiveness to suggestions in hypnosis is a top-down process that is driven primarily by the executive control and salience networks18. Consistent with this, previous work from our group3 found high hypnotizability to be associated with increased functional connectivity between the left dorsolateral prefrontal cortex (L-DLPFC) and the dorsal anterior cingulate cortex (dACC), whereas low hypnotizability was associated with low L-DLPFC–dACC connectivity. Whereas previous neuroimaging findings centered on the role of the anterior cingulate cortex in responding to suggestions in hypnosis via its involvement in attentional processes, a recent systematic review emphasized the complex integration of high-order cognitive processes in hypnotizability (primarily managed by frontal brain structures) beyond the attentional component and specific task demands18 (for example, as seen in hypnotic analgesia). During hypnosis, the dACC shows reduced activation, while the L-DLPFC increases its functional connectivity with the insula (a central node of the salience network) and reduces its connectivity with the posterior cingulate cortex (a key node in the default mode network)19. Notably, the involvement of frontal functions in hypnotizability is potentially moderated by individual differences20, emphasizing the benefit for future research to take a ‘precision medicine’ approach and individualize relevant interventions.
Transcranial magnetic stimulation (TMS) non-invasively modulates neuronal activity and functional connectivity21,22,23 using a high-intensity magnetic field to induce a brief, focal electric field in the cortex that can either activate or inhibit neurons depending on the pattern of the stimulation approach. Repetitive TMS (rTMS) produces periods of lasting facilitation or inhibition that persist after stimulation24. Inhibitory rTMS applied to the DLPFC, beyond its inhibiting effects on the DLPFC itself, is associated with decreased DLPFC activity and increased functional connectivity with the dACC21,25. Spaced forms of a highly efficient form of rTMS, such as continuous theta-burst stimulation (cTBS), produce more durable changes in cortical excitability26,27. A modified form of cTBS (cTBSmod) is capable of consistently producing inhibition in the motor cortex compared with conventional cTBS, which produces these changes inconsistently28.
A previous study by Dienes and Hutton29 demonstrated that a short application (300 pulses) of inhibitory (1 Hz) rTMS when applied to the L-DLPFC increased both objective and subjective reports of hypnotic responsiveness in a small cohort of medium-hypnotizable individuals. A replication study by Coltheart et al.30 did not replicate this finding but found that inhibition of the right DLPFC resulted in a significant increase in objective (but not subjective) responses to hypnotic suggestions, interpreted as driven by interrupting networks involved in belief formation. A potential explanation for the contradicting findings may also lie in the modest stimulation parameters and the skull-based targeting approach used in both studies. In this study, we elected to utilize an optimized non-invasive neurostimulation technique, termed SHIFT (Stanford Hypnosis Integrated with Functional Connectivity-targeted Transcranial Stimulation), to modulate trait hypnotizability. On the basis of our previous finding that high hypnotizability is associated with increased L-DLPFC–dACC functional connectivity3, as well as L-DLPFC functions29, we hypothesized that the application of active spaced SHIFT over the individualized L-DLPFC target that shows the greatest resting-state functional connectivity with the dACC would significantly increase trait hypnotizability as measured by the hypnotic induction profile (HIP), as well as the subjective hypnotic experience using the hypnotic intensity scale (HIS), compared with sham stimulation. We conducted a double-blind, randomized, sham-controlled trial to determine whether SHIFT can be utilized to modulate hypnotizability.
Results
Eighty participants were included in the analyses (93.8% female, mean age 48.3 ± 12.4 years). See Table 1 for the reported demographic information by treatment group. In both groups, most participants guessed receiving active treatment, and the guesses were not associated with the actual treatment received (χ² = 2.257, P = 0.133) or with the pre-to-post change in HIP scores (U = 510.5, P = 0.152). The correlation between HIP scores during the screening appointment and the initial hypnotizability testing at the treatment visit was ρ = 0.73 (P < 0.001), in line with known HIP test–retest reliability30 (0.76). In addition, baseline HIP scores were not significantly different (U = 679, P = 0.242) between the active (mean ± s.d. = 4.9 ± 3.4, median = 6, range: 0–10) and sham (mean ± s.d. = 5.7 ± 3.3, median = 7, range: 0–10) groups. Similarly, baseline HIS scores were correlated with baseline HIP scores (ρ = 0.51, P < 0.001) and were not significantly different (U = 790, P = 0.921) between the active (mean ± s.d. = 3.45 ± 2.76, median = 3, range: 1–10) and sham (mean ± s.d. = 3.47 ± 2.55, median = 3, range: 1–8) groups.
Within-group Wilcoxon signed-ranks tests indicated that, although the active group had a statistically significant change in HIP scores from pre- to immediate post-SHIFT (Z = −3.305, P < 0.001; large effect size: r = 0.52), the sham group did not show a significant difference (Z = −0.514, P = 0.607; small effect size: r = 0.08). Based on the intention-to-treat comparison, ΔHIP scores were significantly greater in the active SHIFT group compared with the sham group (U = 601, P = 0.046; small effect size: r = 0.25; Fig. 1). Additionally, there were no significant differences in pre- to post-SHIFT in HIS ratings between the groups (U = 702.5, P = 0.412). See Figs. 2–4 for detailed information about recruitment, target selection and intervention.
Individual ΔHIP points are presented in blue if increased, red if decreased or gray if there was no change from baseline to post-SHIFT. Immediate ΔHIP scores showed a significant difference from baseline in the active SHIFT group but not in the sham group. Similarly, ΔHIP scores were significantly greater in the active SHIFT group than in the sham group. Four participants (two in each group) had ΔHIP scores of >3. The center lines represents the median; the boxes represent the 25th and 75th percentiles; the error bars represent outlier estimation based on 1.5 × interquartile range.
The timeline of study events included the participants undergoing a one-hour baseline MRI scanning session in which both structural and functional MRI sequences were completed. These magnetic resonance images were then used to individually target the TMS (SHIFT) treatment. Participants then received either active or sham SHIFT targeted to the L-DLPFC. Hypnotizability was assessed pre-SHIFT, immediately post-SHIFT and one hour post-SHIFT using the HIP.
Personalized L-DLPFC neurostimulation targets (blue) for all participants were used in comparison with the commonly used Beam F3 skull-based measurement coordinates (−35.5, 49.4, 32.4). Although shown here in Montreal Neurological Institute standard space for illustration purposes, individual targets were analyzed and identified in native subject space representing the greatest L-DLPFC–dACC functional connectivity.
Time effects
When tested again approximately one hour post-SHIFT, the pre- to post-SHIFT difference in HIP (ΔHIP) scores was smaller but still significant in the active group (Z = −2.336, P = 0.020, medium effect size: r = 0.37) and not significant in the sham group (Z = −1.898, P = 0.058, medium effect size: r = 0.30; one participant was missing one-hour post-SHIFT HIP scores). Although the one-hour post-SHIFT ΔHIP scores were greater in the active SHIFT group compared with the sham group, the difference between the groups at one hour post-SHIFT was not statistically significant (U = 764.5, P = 0.876; small effect size: r = 0.02).
Discussion
SHIFT, a novel neuromodulation approach, demonstrated immediate modulation of hypnotizability—a stable, clinically relevant neurobehavioral trait. Building on our group’s previous work on the neural bases of hypnotizability3,19,31, our results provide further support for a relationship between the L-DLPFC and hypnotizability, as its inhibition produced changes in a hypnotizability measure. As hypnotizability was previously associated with L-DLPFC–dACC functional connectivity3, we chose a neurostimulation approach that has been demonstrated to inhibit DLPFC activity and increase functional connectivity with the dACC21,25. To modulate the targeted network temporarily, we utilized SHIFT, as convergent data suggest that two spaced cTBS sessions increase the durability of the cTBS effect over a single cTBS session28. To address the need for personalized intervention, we targeted the region of the L-DLPFC with the highest functional connectivity to the dACC. These findings are also consistent with the predictions of some theories of hypnosis. For example, the dissociated control theory32 equated the response to hypnosis to frontal lobe damage, by which account inhibition of the DLPFC (although not laterally specified) could result in increased hypnotic response. In addition, updated predictions of the cold control theory of hypnosis29,33 argue that prefrontal inhibition will reduce metacognitive awareness of intentions, thereby increasing the likelihood of successful responsiveness to suggestions to be experienced as involuntary.
Our approach achieved medium-to-large effect sizes after 92 s of non-invasive neurostimulation, a notably shorter approach than the 20 min stimulation protocol used in previous studies29,30. Whereas the increase in hypnotizability scores was inconsistent across subjects (Fig. 1), the effects per unit of time are quite notable. Providing evidence of a perturbation technique that is capable of transiently modulating stable traits is quite encouraging, as our technique can be further engineered for the intended effect. Certainly, the large pre–post effect size (r = 0.52) achieved with our brief SHIFT protocol is in line with the effect sizes of conventional rTMS for major depressive disorder (MDD), where 10 Hz rTMS is applied over 1,200 min across six weeks34. Furthermore, the open-label effect of this approach is unknown and could be even larger, given the differences between the controlled and open-label data in depression34,35. When comparing the effects of SHIFT with the placebo stimulation, we found a small effect (despite there being no significant differences in treatment expectancy between the groups or association of expectancy with a change in hypnotizability), suggesting that open-label treatments may yield greater effects.
Whereas we did not observe significant pre–post changes in the subjective experience of hypnotic depth, this may be explained by the time effects we identified. When compared with the immediately post-SHIFT results, the change in hypnotizability was not significantly different between the groups after one hour. This finding suggests that SHIFT produces a transient effect. As such, future clinical applications should prioritize scheduling the bulk of post-SHIFT interventions as close as possible to the stimulation. Nevertheless, given that the HIS was administered at baseline and approximately one hour post-SHIFT, if the effects on subjective hypnotic experiences are also transient, we would not expect a substantial change at this time point.
Lastly, alongside our evidence for the feasibility of altering a stable neurobehavioral trait through neuromodulation, previous research has demonstrated the ability to modulate other neurobehavioral traits. In a small study, Spronk et al.36 observed a significant decrease in trait neuroticism and an increase in extraversion following 15–25 rTMS sessions applied to the L-DLPFC. The modulation of trait neuroticism was later replicated by Berlim and co-workers37. This is notable as, beyond time-dependent changes in trait neuroticism, treatment for depression largely fails to modulate it38. Together with our findings, SHIFT may be able to modulate clinically relevant neurobehavioral traits associated with psychopathology and responsiveness to treatment.
Limitations
The interpretation of the current results involves caveats that could be addressed in future trials. In addition, this trial did not assess any outcome measures involving the modification of disease symptoms as this was designed to be a mechanistic study; future studies should build on these findings to evaluate the use of the neuromodulation of a neurobehavioral trait to assess clinical outcome measures in a patient population directly. Although HIP assessors were blind to intervention, their blinding was not evaluated via a questionnaire, as was done with the participants. Moreover, future studies could benefit from assessing the attitudes of participants towards hypnosis to understand potential contextual factors further.
Even though we showed that this trait could be modulated with SHIFT in this population, lower baseline connectivity in our fibromyalgia syndrome (FMS) sample may render hypnotizability enhancement via this route rather challenging. Persons who are innately more highly hypnotizable show greater functional connectivity between the DLPFC and the dACC3, and conditions that influence connectivity, such as fibromyalgia, may influence the degree to which the trait may be modulated39. As such, depending on the underlying neuropathophysiology of the intended condition, alternative neurostimulation models may be warranted to enhance hypnotizability.
The results achieved in this study provide evidence that hypnotizability, a stable neurobehavioral trait, can be directionally and measurably modulated using non-invasive brain stimulation. Further studies are needed to build on these findings to assess the dose–response relationships of SHIFT as well as the added efficacy of functional connectivity magnetic resonance imaging (MRI) targeting. Furthermore, to better understand the individual elements driving mechanistic change in neurobehavioral traits, future neuromodulation trials are needed to further explore the parameter space within the current technique with the aim of optimizing the dosing as a method for modulating the neural circuitry underlying trait-based disorders as well as enhancing trait-based interventions.
Lastly, future studies should examine other targeted neurostimulation approaches to test different stimulation mechanisms. A more portable yet less personalized, more dispersed neurostimulation approach, transcranial direct current stimulation (tDCS)40,41,42, could also be used to generate an increase in hypnotizability43, albeit requiring 18 min of stimulation. In addition, neither TMS nor tDCS can stimulate deeper hypnotizability-related circuits, such as the dACC, directly. An emerging non-invasive brain stimulation approach that can be individually targeted based on neuroimaging data is transcranial focused ultrasound (or tFUS), which has been demonstrated to successfully target the anterior cingulate cortex in both animal44 and human45 studies and may offer a viable solution.
Methods
Participants
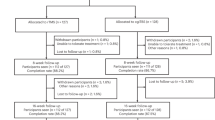
To test our hypotheses in a clinical population that is likely to benefit from a temporary increase in hypnotizability, we recruited individuals with FMS46, a central pain disorder of unclear etiology and mechanism that affects up to 8% of the general population47. Hypnosis-based treatments have shown success in pain management for patients with FMS48, and hypnotic pain reduction is sensitive to hypnotizability6. In FMS, functional connectivity is altered in the salience network and the default mode network, both of which are involved in hypnosis19. Hyperactivity in the endogenous opioid system in FMS renders opioid medications less effective in reducing pain49,50, making FMS a prime candidate for non-pharmacological interventions. As such, low to moderately hypnotizable male and female participants with FMS aged 18–69 years were recruited for this study starting in February 2017, with both recruitment and data collection reaching the targeted enrolment number in December 2019 (the trial was registered on ClinicalTrials.gov (NCT02969707)51; see Fig. 2 for the Consolidated Standards of Reporting Trials (CONSORT) recruitment diagram). The study was approved by the Stanford University Institutional Review Board; all participants provided informed consent and all enroled participants were financially compensated. Before enrolment, participants underwent phone and in-person screening procedures to determine their eligibility. Hypnotizability was assessed during the in-person screening by trained study personnel using the HIP (see below). Low to moderately hypnotizable individuals (with a HIP score of ≤8 out of 10) were eligible to participate in the study, and highly hypnotizable individuals (with a HIP score of >8 out of 10) were excluded after the screening appointment. All participants had a primary diagnosis of FMS, which a study clinician confirmed during the in-person screening. Diagnostic criteria were determined based on the American College of Rheumatology preliminary diagnostic criteria for FMS52, and participants provided results of a blood test completed within a year to confirm a normal complete blood count and inflammatory panel (including a complete blood count with differential, the erythrocyte sedimentation rate (ESR) and a metabolic panel; to exclude evidence from potential comorbid rheumatologic conditions). Participants who did not have a recent blood test completed this as part of the study screening visit. Exclusionary criteria included standard MRI contraindications (for example, ferromagnetic implants or claustrophobia), contraindications to TMS as measured by the TMS Adult Safety Screen, neurological disorders (for example, seizure disorder) and serious primary psychiatric disorders that, when present, could necessitate a psychiatric hospitalization. These comorbid psychiatric disorders included psychotic disorders, bipolar disorder, post-traumatic stress disorder with suicidal ideation and severe MDD with suicidal ideation (dysthymia, mild to moderate MDD and anxiety disorders were not exclusionary). Participants with FMS currently prescribed psychoactive medications underwent a voluntary washout period before neuroimaging and TMS (that is, a five-week washout for fluoxetine and a two-week washout for all other antidepressant medications; the washout periods were designed based on half-life values and were individually tailored to the participant by their prescribing physician). If participants were unable to see their prescribing physician, a study physician oversaw this medication washout. To assure blinding, only participants with no previous exposure to TMS were eligible for the study.
Neuroimaging for transcranial magnetic stimulation targeting
MRI data were collected using a research-dedicated 3.0T Discovery MR750 instrument (General Electric) with a 32-channel head coil (Nova Medical). Individualized neuroimaging for subsequent TMS targeting consisted of both structural and functional MRI sequences.
Personalized L-DLPFC targets were generated for each participant using resting-state functional MRI (fMRI) hierarchical clustering to determine the anatomical location within the L-DLPFC that exhibited the greatest functional connectivity to the dACC (Fig. 4). The dACC region of interest (ROI) was based on a previous coordinate-based meta-analysis aimed at determining the areas of the brain most functionally relevant to hypnotizability31. This general approach was previously reported in a clinical trial using the Stanford Accelerated Intelligent Neuromodulation Therapy for the treatment of depression53 and subsequently validated in a follow-up study54. Resting-state fMRI scans were acquired over ~8.5 min using a simultaneous multi-slice echo-planar imaging (EPI) sequence with the following parameters: time to echo (TE) = 30 ms, repetition time (TR) = 2,000 ms, flip angle = 77°, slice acceleration factor = 3, matrix = 128 × 128, 1.8 × 1.8 mm in-plane resolution, slice thickness = 1.8 mm, field of view (FOV) = 230 × 230 mm and 87 contiguous axial slices—see Supplementary Information for a detailed description of the target generation method.
Transcranial magnetic stimulation
Participants were randomized using a permuted-block design with varying block sizes to receive either sham or active cTBS, an efficient form of rTMS that is capable of producing inhibition of cortical excitability in the motor cortex26,28,55. Stimulation was delivered using a MagPro X100 system (MagVenture) with a Cool-B65 A/P coil. Specifically, we utilized a modified form of cTBS (termed SHIFT) applied in a spaced manner with two applications of ~46 s that were each comprised of 800 pulses, 200 pulses for ramping up slowly with 600 pulses at full intensity, delivered in a continuous train with each burst containing three pulses at 30 Hz repeated at 6 Hz (refs. 28,56).
Following the application of spaced SHIFT, participants were asked to refrain from discussing information pertaining to the subjective stimulation experience (for example, discomfort, facial movement or scalp sensation) with study personnel, including those conducting HIP assessments. Study personnel (not conducting behavioral assessments) administered a questionnaire to assess participant blinding after cessation of stimulation for the day, which included a binary question of whether they thought they received active or sham stimulation. See Fig. 3 for a neurostimulation summary.
Study objectives
This study addresses the hypnotizability-related outcomes of Secondary Objective B, testing the study’s behavioral hypotheses, which include a change in hypnotizability—the key behavioral variable in the project—to determine the effect of active, inhibitory rTMS (cTBS) over the L-DLPFC on enhancing the hypnotizability and the subjective experience of hypnosis (that is, hypnotic intensity). Secondary outcome measure 2 in the preregistered protocol is one of five secondary objectives, which are to determine the effect of active, inhibitory cTBS over the L-DLPFC on (1) the neural network that underlies hypnosis phenomena, (2) hypnotizability, (3) the neural network that underlies conflict regulation, (4) the neural network that underlies hypnotic modulation of the Stroop effect and (5) the neural network that underlies hypnotic analgesia.
Measures
Hypnotic induction profile
The HIP is a validated measure of hypnotizability2,57; it includes a standardized hypnotic induction followed by a set of specific suggestions. The HIP is scored by the administering clinician based on behavioral responsiveness and reports of the examinee’s subjective experience. HIP scores range from 0 (no responsiveness) to 10 (most responsive), with scores above 8 representing highly hypnotizable individuals. In the current study, the HIP was first administered immediately before L-DLPFC stimulation, immediately following the SHIFT stimulation and then again after the MRI, approximately one hour following SHIFT stimulation. To ensure assessor blinding, assessors waited and completed the HIP in a room that was separate from where the TMS machine and the stimulation took place. Furthermore, participants were requested not to share information about the stimulation with the assessors.
Hypnotic intensity scale
The HIS is a single self-report scale of 1–10 of the perceived ‘depth’ of the hypnotic experience during the fMRI hypnosis task19, ranging from ‘not hypnotized at all’ (1) to ‘deeply hypnotized’ (10). The HIS is rated in hindsight after participants completed their MRI scans. As such, whereas baseline HIS was administered immediately before the baseline HIP, the post-SHIFT HIP was administered at the end of the second MRI scan (approximately one hour post-SHIFT). The HIS is not a standardized scale and has been described by other names (for example, hypnotic depth scale or Long Stanford Scale)58. Here we used the scale as described by Deeley et al.58 and utilized in our previous work19.
Data analysis
Data were collected and organized using the REDCap methodology59, and analysis was performed in the SPSS v.26.0 environment60. According to our preregistered plan, analyses were completed within the intention-to-treat principle, and reported P values are nominal. To test the change in HIP scores following SHIFT, pre- to post-SHIFT changes in HIP scores (ΔHIP) were calculated by subtracting the immediate post-spaced SHIFT score from the pre-spaced SHIFT score. Neither the pre- or post-spaced SHIFT HIP variables nor the ΔHIP scores met the criteria for the assumption of normality (all Shapiro–Wilk P values < 0.001), rendering the first step in our preregistered plan of testing our hypotheses using analysis of variance (ANOVA) inappropriate. As such, we used non-parametric tests; within-group pre/post-SHIFT changes in HIP scores were tested using a two-tailed Wilcoxon signed-rank test. Two-tailed Mann–Whitney U-tests were used for group comparisons of ΔHIP scores between the active and sham groups. Effect sizes for the non-parametric tests were calculated using Cohen’s r statistic61,62. The study blind was tested using the chi-squared test.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Owing to the sensitivity of psychiatric patient data, the Stanford University Institutional Review Board requires individualized review before the sharing of data. We have produced anonymized data related to the present findings for sharing with all scientists, where the research plans and data-safeguarding plans comport with Stanford University guidelines. Data-sharing requests should be directed to the corresponding authors.
References
Ellenberger, H. F. The Discovery of the Unconscious: The History and Evolution of Dynamic Psychiatry (Basic Books, 1970).
Spiegel, H. & Spiegel, D. Trance and Treatment: Clinical Uses of Hypnosis (American Psychiatric Publishing, 2004).
Hoeft, F. et al. Functional brain basis of hypnotizability. Arch. Gen. Psychiatry 69, 1064–1072 (2012).
Faerman, A. & Spiegel, D. Shared cognitive mechanisms of hypnotizability with executive functioning and information salience. Sci. Rep. 11, 5704 (2021).
Lynn, S. J., Shindler, K. & Meyer, E. Hypnotic suggestibility, psychopathology, and treatment outcome. Sleep Hypn. 5, 17–25 (2003).
Milling, L. S., Valentine, K. E., LoStimolo, L. M., Nett, A. M. & McCarley, H. S. Hypnosis and the alleviation of clinical pain: a comprehensive meta-analysis. Int. J. Clin. Exp. Hypn. 69, 297–322 (2021).
Thompson, T. et al. The effectiveness of hypnosis for pain relief: a systematic review and meta-analysis of 85 controlled experimental trials. Neurosci. Biobehav. Rev. 99, 298–310 (2019).
Lynn, S. J., Meyer, E. & Shindler, K. in The Highly Hypnotizable Person: Theoretical, Experimental and Clinical Issues (eds Heap, M. et al.) 187–212 (Routledge, 2004).
Hammond, D. C. Hypnosis as sole anesthesia for major surgeries: historical & contemporary perspectives. Am. J. Clin. Hypn. 51, 101–121 (2008).
Tefikow, S. et al. Efficacy of hypnosis in adults undergoing surgery or medical procedures: a meta-analysis of randomized controlled trials. Clin. Psychol. Rev. 33, 623–636 (2013).
Piccione, C., Hilgard, E. R. & Zimbardo, P. G. On the degree of stability of measured hypnotizability over a 25-year period. J. Pers. Soc. Psychol. 56, 289–295 (1989).
Roberts, B. W. & DelVecchio, W. F. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychol. Bull. 126, 3–25 (2000).
Rajabi, M. et al. Improving hypnotizability in adults with Modafinil: what is the trick?! Aust. J. Clin. Exp. Hypn. 42, 11–18 (2017).
Gorassini, D. R. & Spanos, N. P. in Clinical Hypnosis and Self-regulation: Cognitive–Behavioral Perspectives (eds Kirsch, I. et al.) 141–177 (American Psychological Association, 1999); https://doi.org/10.1037/10282-006
Bates, B. L. & Brigham, T. A. Modifying hypnotizability with the Carleton Skills Training program: a partial replication and analysis of components. Int. J. Clin. Exp. Hypn. 38, 183–195 (1990).
Lynn, S. J. et al. Hypnosis, hypnotic phenomena, and hypnotic responsiveness: clinical and research foundations—a 40-year perspective. Int. J. Clin. Exp. Hypn. 67, 475–511 (2019).
Lynn, S. J., Laurence, J.-R. & Kirsch, I. Hypnosis, suggestion, and suggestibility: an integrative model. Am. J. Clin. Hypn. 57, 314–329 (2015).
Landry, M., Lifshitz, M. & Raz, A. Brain correlates of hypnosis: a systematic review and meta-analytic exploration. Neurosci. Biobehav. Rev. 81, 75–98 (2017).
Jiang, H., White, M. P., Greicius, M. D., Waelde, L. C. & Spiegel, D. Brain activity and functional connectivity associated with hypnosis. Cereb. Cortex 27, 4083–4093 (2017).
Parris, B. A. The role of frontal executive functions in hypnosis and hypnotic suggestibility. Psychol. Conscious. Theory Res. Pract. 4, 211–229 (2017).
Liston, C. et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol. Psychiatry 76, 517–526 (2014).
Fox, M. D., Halko, M. A., Eldaief, M. C. & Pascual-Leone, A. Measuring and manipulating brain connectivity with resting state functional connectivity magnetic resonance imaging (fcMRI) and transcranial magnetic stimulation (TMS). Neuroimage 62, 2232–2243 (2012).
Watanabe, T. et al. Bidirectional effects on interhemispheric resting-state functional connectivity induced by excitatory and inhibitory repetitive transcranial magnetic stimulation. Hum. Brain Mapp. 35, 1896–1905 (2014).
Bestmann, S. et al. Mapping causal interregional influences with concurrent TMS–fMRI. Exp. Brain Res. 191, 383 (2008).
Nyffeler, T. et al. Repetitive TMS over the human oculomotor cortex: comparison of 1-Hz and theta burst stimulation. Neurosci. Lett. 409, 57–60 (2006).
Huang, Y.-Z., Edwards, M. J., Rounis, E., Bhatia, K. P. & Rothwell, J. C. Theta burst stimulation of the human motor cortex. Neuron 45, 201–206 (2005).
Nyffeler, T., Cazzoli, D., Hess, C. W. & Müri, R. M. One session of repeated parietal theta burst stimulation trains induces long-lasting improvement of visual neglect. Stroke 40, 2791–2796 (2009).
Goldsworthy, M. R., Pitcher, J. B. & Ridding, M. C. A comparison of two different continuous theta burst stimulation paradigms applied to the human primary motor cortex. Clin. Neurophysiol. 123, 2256–2263 (2012).
Dienes, Z. & Hutton, S. Understanding hypnosis metacognitively: rTMS applied to left DLPFC increases hypnotic suggestibility. Cortex 49, 386–392 (2013).
Coltheart, M. et al. Belief, delusion, hypnosis, and the right dorsolateral prefrontal cortex: a transcranial magnetic stimulation study. Cortex 101, 234–248 (2018).
DeSouza, D. D. et al. Association between anterior cingulate neurochemical concentration and individual differences in hypnotizability. Cereb. Cortex 30, 3644–3654 (2020).
Jamieson, G. A. & Woody, E. in Hypnosis and Conscious States: The Cognitive Neuroscience Perspective (ed. Jamieson, G. A.) 111–129 (Oxford Univ. Press, 2007).
Dienes, Z. et al. Phenomenological control as cold control. Psychol. Conscious. Theory Res. Pract. 9, 101–116 (2022).
George, M. S. et al. Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trial. Arch. Gen. Psychiatry 67, 507–516 (2010).
Carpenter, L. L. et al. Transcranial magnetic stimulation (TMS) for major depression: a multisite, naturalistic, observational study of acute treatment outcomes in clinical practice. Depress. Anxiety 29, 587–596 (2012).
Spronk, D., Arns, M., Bootsma, A., van Ruth, R. & Fitzgerald, P. B. Long term effects of left frontal rTMS on EEG and ERPs in patients with depression. Clin. EEG Neurosci. 39, 118–124 (2008).
Berlim, M. T., McGirr, A., Beaulieu, M.-M., Van den Eynde, F. & Turecki, G. Are neuroticism and extraversion associated with the antidepressant effects of repetitive transcranial magnetic stimulation (rTMS)? An exploratory 4-week trial. Neurosci. Lett. 534, 306–310 (2013).
Renner, F., Penninx, B. W. J. H., Peeters, F., Cuijpers, P. & Huibers, M. J. H. Two-year stability and change of neuroticism and extraversion in treated and untreated persons with depression: findings from the Netherlands Study of Depression and Anxiety (NESDA). J. Affect. Disord. 150, 201–208 (2013).
Otti, A., Guendel, H., Wohlschläger, A., Zimmer, C. & Noll-Hussong, M. Frequency shifts in the anterior default mode network and the salience network in chronic pain disorder. BMC Psychiatry 13, 84 (2013).
Bestmann, S., De Berker, A. O. & Bonaiuto, J. Understanding the behavioural consequences of noninvasive brain stimulation. Trends Cogn. Sci. 19, 13–20 (2015).
Calzolari, S., Jalali, R. & Fernández-Espejo, D. Characterising stationary and dynamic effective connectivity changes in the motor network during and after tDCS. Neuroimage 269, 119915 (2023).
Parkin, B. L., Ekhtiari, H. & Walsh, V. F. Non-invasive human brain stimulation in cognitive neuroscience: a primer. Neuron 87, 932–945 (2015).
Perri, R. L. & Di Filippo, G. Alteration of hypnotic experience following transcranial electrical stimulation of the left prefrontal cortex. Int. J. Clin. Health Psychol. 23, 100346 (2023).
Folloni, D. et al. Manipulation of subcortical and deep cortical activity in the primate brain using transcranial focused ultrasound stimulation. Neuron 101, 1109–1116.e5 (2019).
Shin, D. H., Son, S. & Kim, E. Y. Low-energy transcranial navigation-guided focused ultrasound for neuropathic pain: an exploratory study. Brain Sci. 13, 1433 (2023).
Kong, J. et al. Altered resting state functional connectivity of the cognitive control network in fibromyalgia and the modulation effect of mind–body intervention. Brain Imaging Behav. 13, 482–492 (2019).
Clauw, D. J. Fibromyalgia: a clinical review. JAMA 311, 1547–1555 (2014).
Picard, P. et al. Hypnosis for management of fibromyalgia. Int. J. Clin. Exp. Hypn. 61, 111–123 (2013).
Arout, C. A., Edens, E., Petrakis, I. L. & Sofuoglu, M. Targeting opioid-induced hyperalgesia in clinical treatment: neurobiological considerations. CNS Drugs 29, 465–486 (2015).
Bellato, E. et al. Fibromyalgia syndrome: etiology, pathogenesis, diagnosis, and treatment. Pain Res. Treat. 2012, e426130 (2012).
Spiegel, D. Use of repetitive transcranial magnetic stimulation to augment hypnotic analgesia. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT02969707 (2021).
Wolfe, F. et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 62, 600–610 (2010).
Cole, E. J. et al. Stanford Accelerated Intelligent Neuromodulation Therapy for treatment-resistant depression. Am. J. Psychiatry 177, 716–726 (2020).
Cole, E. J. et al. Stanford Neuromodulation Therapy (SNT): a double-blind randomized controlled trial. Am. J. Psychiatry 179, 132–141 (2022).
Huang, Y.-Z. & Rothwell, J. C. The effect of short-duration bursts of high-frequency, low-intensity transcranial magnetic stimulation on the human motor cortex. Clin. Neurophysiol. 115, 1069–1075 (2004).
Wischnewski, M. & Schutter, D. J. L. G. Efficacy and time course of theta burst stimulation in healthy humans. Brain Stimul. 8, 685–692 (2015).
Spiegel, H., Aronson, M., Fleiss, J. L. & Haber, J. Psychometric analysis of the hypnotic induction profile. Int. J. Clin. Exp. Hypn. 24, 300–315 (1976).
Deeley, Q. et al. Modulating the default mode network using hypnosis. Int. J. Clin. Exp. Hypn. 60, 206–228 (2012).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
IBM SPSS Statistics for Windows v.26.0 (IBM Corp., 2019).
Fritz, C. O., Morris, P. E. & Richler, J. J. Effect size estimates: current use, calculations, and interpretation. J. Exp. Psychol. Gen. 141, 2–18 (2012).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences (Lawrence Erlbaum Associates, 1988).
Acknowledgements
This work was supported by the National Institutes of Health (NIH) Center for Complementary and Integrative Health (NCCIH) grant Innovation Award for Mechanistic Studies to Optimize Mind and Body Interventions (R33AT009305–03; D.S. and N.R.W.). This trial was preregistered on ClinicalTrials.gov (NCT02969707). We thank K. Sudheimer for his technical assistance.
Author information
Authors and Affiliations
Contributions
A.F., J.H.B., K.H.S., N.R.W. and D.S. contributed to project administration, writing, data curation and investigation. A.F. and B.J. contributed to formal analysis, validation and revision. J.H.B., K.H.S., D.D.D., E.K., N.R.W. and D.S. contributed to conceptualization and methodology. A.P., M.G., H.A., R.N. and A.D.G. contributed to data curation and investigation. All authors contributed to the writing of this paper.
Corresponding authors
Ethics declarations
Competing interests
N.R.W. is a named inventor on Stanford-owned intellectual property relating to accelerated TMS pulse pattern sequences and neuroimaging-based TMS targeting; he has served on scientific advisory boards for Otsuka, NeuraWell, Magnus Medical and Nooma as a paid advisor; he also has equity/stock options in Magnus Medical, NeuraWell and Nooma. There were no financial conflicts during the conduct of the trial or analysis of the data in this Article. D.S. is a co-founder of Reveri Health, Inc., an interactive hypnosis app (not utilized in the current study). A.F. is a consultant for Reveri Health, Inc. The other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Bence Palfi, Vilfredo De Pascalis and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Methods.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Faerman, A., Bishop, J.H., Stimpson, K.H. et al. Stanford Hypnosis Integrated with Functional Connectivity-targeted Transcranial Stimulation (SHIFT): a preregistered randomized controlled trial. Nat. Mental Health 2, 96–103 (2024). https://doi.org/10.1038/s44220-023-00184-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00184-z