Abstract
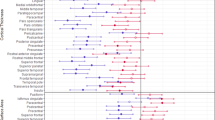
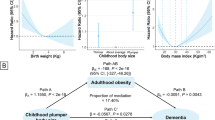
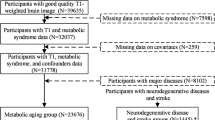
There is increasing attention on the associations between body weight and several neurological and psychiatric disorders. Using a total of 438,483 participants from the UK Biobank, we aimed to understand the effects of body mass index (BMI), BMI change and BMI-metabolic health status on the incidence of common neurological and psychiatric disorders. Associations of body weight with six disorders (stroke, dementia, Parkinson’s disease, anxiety, depression and sleep disorders) were analysed by Cox regression models. We performed linear regression models and mediation analysis to explore the underlying mechanisms. Overweight or obesity group had a higher risk of stroke, anxiety, depression and sleep disorders. Metabolically healthy obesity demonstrated a higher risk of depression and sleep disorders. The differing effects of metabolically healthy versus unhealthy obesity on brain structure, dietary intake and inflammatory markers provided clues to the underlying associations. Hence, weight management should be recommended for individuals with obesity irrespective of their metabolic health status.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from UKB project site, subject to registration and application process. Further details can be found at https://www.ukbiobank.ac.uk. The GWAS data of neurological and psychiatric disorders were retrieved from the exogenous population which is publicly available (stroke: https://doi.org/10.1038/s41588-018-0058-3; AD: https://doi.org/10.1038/s41588-019-0358-2; PD: https://doi.org/10.1016/s1474-4422(19)30320-5; major depression: https://doi.org/10.1038/s41588-018-0090-3; anxiety disorders: https://doi.org/10.1038/ng.3888; insomnia: obstructive sleep apnoea: https://doi.org/10.1183/13993003.03091-2020).
Code availability
Packages including ‘survival’ (version 3.5-3), ‘TwoSampleMR’ (version 0.5.6) and ‘mediation’ (version 4.5.0) in R version 4.1.2 were used to perform Cox proportional hazard regression model, MR study and mediation analysis, respectively. The codes of these analyses were available at https://github.com/RongzeWang06/BW. Freesurfer v6.0 and FSL 6.0 were used to process the imaging data, and MATLAB 2018b was used to perform corresponding linear association analysis.
References
Prince, M. et al. No health without mental health. Lancet 370, 859–877 (2007).
Zhang, Y. R. et al. Modifiable risk factors for incident dementia and cognitive impairment: an umbrella review of evidence. J. Affect. Disord. 314, 160–167 (2022).
Ascherio, A. & Schwarzschild, M. A. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 15, 1257–1272 (2016).
Muanido, A. et al. Prevalence and associated factors of common mental disorders in primary care settings in Sofala Province, Mozambique. BJPsych Open 9, e12 (2023).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781 (2014).
Muscogiuri, G. et al. Obesity and sleep disturbance: the chicken or the egg. Crit. Rev. Food Sci. Nutr. 59, 2158–2165 (2019).
Gariepy, G., Nitka, D. & Schmitz, N. The association between obesity and anxiety disorders in the population: a systematic review and meta-analysis. Int. J. Obes. 34, 407–419 (2010).
Zhuang, Q. S., Meng, L., Wang, Z., Shen, L. & Ji, H. F. Associations between obesity and Alzheimer’s disease: multiple bioinformatic analyses. J. Alzheimer’s Dis. 80, 271–281 (2021).
Astell-Burt, T., Navakatikyan, M. A. & Feng, X. Behavioural change, weight loss and risk of dementia: a longitudinal study. Prev. Med. 145, 106386 (2021).
Singh, G., Jackson, C. A., Dobson, A. & Mishra, G. D. Bidirectional association between weight change and depression in mid-aged women: a population-based longitudinal study. Int. J. Obes. 38, 591–596 (2014).
Kisanuki, K. et al. Weight change during middle age and risk of stroke and coronary heart disease: The Japan Public Health Center-based Prospective Study. Atherosclerosis 322, 67–73 (2021).
Després, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 444, 881–887 (2006).
Stefan, N., Häring, H. U., Hu, F. B. & Schulze, M. B. Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet. Diabetes Endocrinol. 1, 152–162 (2013).
Gao, M. et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: a cohort study. PLoS Med. 17, e1003351 (2020).
Ma, L. Z. et al. Metabolically healthy obesity reduces the risk of Alzheimer’s disease in elders: a longitudinal study. Aging 11, 10939–10951 (2019).
Jokela, M., Hamer, M., Singh-Manoux, A., Batty, G. D. & Kivimäki, M. Association of metabolically healthy obesity with depressive symptoms: pooled analysis of eight studies. Mol. Psychiatry 19, 910–914 (2014).
Briguglio, M. et al. Healthy Eating, Physical Activity, and Sleep Hygiene (HEPAS) as the winning triad for sustaining physical and mental health in patients at risk for or with neuropsychiatric disorders: considerations for clinical practice. Neuropsychiatr. Dis. Treat. 16, 55–70 (2020).
Psaltopoulou, T. et al. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann. Neurol. 74, 580–591 (2013).
Martins, L. B., Monteze, N. M., Calarge, C., Ferreira, A. V. M. & Teixeira, A. L. Pathways linking obesity to neuropsychiatric disorders. Nutrition 66, 16–21 (2019).
Castanon, N., Lasselin, J. & Capuron, L. Neuropsychiatric comorbidity in obesity: role of inflammatory processes. Front. Endocrinol. 5, 74 (2014).
Navarro, E., Funtikova, A. N., Fíto, M. & Schröder, H. Can metabolically healthy obesity be explained by diet, genetics, and inflammation? Mol. Nutr. Food Res. 59, 75–93 (2015).
Wang, X. et al. The relationship between body mass index and stroke: a systemic review and meta-analysis. J. Neurol. 269, 6279–6289 (2022).
Deng, Y. T. et al. Association of life course adiposity with risk of incident dementia: a prospective cohort study of 322,336 participants. Mol. Psychiatry 27, 3385–3395 (2022).
de Wit, L. M., van Straten, A., van Herten, M., Penninx, B. W. & Cuijpers, P. Depression and body mass index, a u-shaped association. BMC Public Health 9, 14 (2009).
Carneiro-Barrera, A., Díaz-Román, A., Guillén-Riquelme, A. & Buela-Casal, G. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: systematic review and meta-analysis. Obes. Rev. 20, 750–762 (2019).
Wang, C. et al. Weight loss and the risk of dementia: a meta-analysis of cohort studies. Curr. Alzheimer Res. 18, 125–135 (2021).
Marcus, Y. et al. Metabolically healthy obesity is a misnomer: components of the metabolic syndrome linearly increase with BMI as a function of age and gender. Biology https://doi.org/10.3390/biology12050719 (2023).
Lassale, C. et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case–cohort analysis. Eur. Heart J. 39, 397–406 (2018).
Mongraw-Chaffin, M. et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J. Am. Coll. Cardiol. 71, 1857–1865 (2018).
Amiri, S. & Behnezhad, S. Obesity and anxiety symptoms: a systematic review and meta-analysis. Neuropsychiatrie 33, 72–89 (2019).
Hammen, C. Risk factors for depression: an autobiographical review. Annu. Rev. Clin. Psychol. 14, 1–28 (2018).
Mehra, R. & Redline, S. Sleep apnea: a proinflammatory disorder that coaggregates with obesity. J. Allergy Clin. Immunol. 121, 1096–1102 (2008).
Suemoto, C. K., Gilsanz, P., Mayeda, E. R. & Glymour, M. M. Body mass index and cognitive function: the potential for reverse causation. Int. J. Obes. 39, 1383–1389 (2015).
Kivimäki, M. et al. Body mass index and risk of dementia: analysis of individual-level data from 1.3 million individuals. Alzheimer’s Dement. 14, 601–609 (2018).
Iacobini, C., Pugliese, G., Blasetti Fantauzzi, C., Federici, M. & Menini, S. Metabolically healthy versus metabolically unhealthy obesity. Metabolism 92, 51–60 (2019).
Wadden, T. A., Tronieri, J. S. & Butryn, M. L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 75, 235–251 (2020).
Salas-Salvadó, J. et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: one-year results of the PREDIMED randomized trial. Arch. Intern. Med. 168, 2449–2458 (2008).
Bañuls, C. et al. Oxidative and endoplasmic reticulum stress is impaired in leukocytes from metabolically unhealthy vs healthy obese individuals. Int. J. Obes. 41, 1556–1563 (2017).
Ghaben, A. L. & Scherer, P. E. Adipogenesis and metabolic health. Nat. Rev. Mol. Cell Biol. 20, 242–258 (2019).
Blüher, M. Metabolically healthy obesity. Endocr. Rev. https://doi.org/10.1210/endrev/bnaa004 (2020).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. In World Health Organization Technical Report Series 894, i–xii, 1–253 (WHO, 2000).
UK Biobank Biomarker Project. biobank https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/serum_biochemistry.pdf (2019).
Zhou, Z. et al. Are people with metabolically healthy obesity really healthy? A prospective cohort study of 381,363 UK Biobank participants. Diabetologia 64, 1963–1972 (2021).
Brain imaging documentation. biobank https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/brain_mri.pdf (2022).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31, 968–980 (2006).
Fischl, B. et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33, 341–355 (2002).
Category 100080. biobank https://biobank.ndph.ox.ac.uk/showcase/label.cgi?id=100080.
UK Biobank Haematology Data Companion Document. biobank http://biobank.ndph.ox.ac.uk/showcase/showcase/docs/haematology.pdf (2017).
Harrell, F. E. Regression Modeling Strategies (Springer, 2001).
Polemiti, E. et al. BMI and BMI change following incident type 2 diabetes and risk of microvascular and macrovascular complications: the EPIC-Potsdam study. Diabetologia 64, 814–825 (2021).
Zhu, Z. et al. Shared genetic and experimental links between obesity-related traits and asthma subtypes in UK Biobank. J. Allergy Clin. Immunol. 145, 537–549 (2020).
Malik, R. et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat. Genet. 50, 524–537 (2018).
Kunkle, B. W. et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 51, 414–430 (2019).
Nalls, M. A. et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 18, 1091–1102 (2019).
Wray, N. R. et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat. Genet. 50, 668–681 (2018).
Otowa, T. et al. Meta-analysis of genome-wide association studies of anxiety disorders. Mol. Psychiatry 21, 1391–1399 (2016).
Hammerschlag, A. R. et al. Genome-wide association analysis of insomnia complaints identifies risk genes and genetic overlap with psychiatric and metabolic traits. Nat. Genet. 49, 1584–1592 (2017).
Strausz, S. et al. Genetic analysis of obstructive sleep apnoea discovers a strong association with cardiometabolic health. Eur. Resp. J. https://doi.org/10.1183/13993003.03091-2020 (2021).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife https://doi.org/10.7554/eLife.34408 (2018).
Tingley, D., Yamamoto, T., Hirose, K., Imai, K. & Keele, L. mediation: R package for causal mediation analysis. J. Stat. Softw. 59, 1–38 (2014).
Acknowledgements
The authors gratefully thank all the participants and professionals contributing to the UKB. This study was funded by the STI2030-Major Projects (2022ZD0211600), National Natural Science Foundation of China (82071201, 82071997), Shanghai Municipal Science and Technology Major Project (2018SHZDZX01), Research Start-up Fund of Huashan Hospital (2022QD002), Excellence 2025 Talent Cultivation Program at Fudan University (3030277001), Shanghai Talent Development Funding for The Project (2019074), Shanghai Rising-Star Program (21QA1408700), 111 Project (B18015) and ZHANGJIANG LAB, Tianqiao and Chrissy Chen Institute and the State Key Laboratory of Neurobiology and Frontiers Center for Brain Science of Ministry of Education, and Shanghai Center for Brain Science and Brain-Inspired Technology, Fudan University. The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization, J.-T.Y.; methodology, R.-Z.W., Y.H. and Y.-T.D.; investigation, R.-Z.W., Y.H., Y.-T.D., H.-F.W. and Y.Z.; writing—original draft, R.-Z.W. and Y.H.; writing—review and editing, R.-Z.W. and Y.H.; funding acquisition, J.-T.Y.; resources, J.-F.F., W.C. and J.-T.Y.; supervision, W.C. and J.-T.Y.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Raaj Biswas, Richard Musil and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Methods, Tables 1–33 and Figs. 1–3.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, RZ., He, Y., Deng, YT. et al. Body weight in neurological and psychiatric disorders: a large prospective cohort study. Nat. Mental Health 2, 41–51 (2024). https://doi.org/10.1038/s44220-023-00158-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00158-1