Abstract
Technical developments and improved access to neuroimaging techniques have brought us closer to understanding the neuropathological origins of schizophrenia. Using data-driven disease-progression modelling on cross-sectional magnetic resonance imaging (MRI) from 1,124 patients with schizophrenia, we characterize two distinct but stable ‘trajectories’ of brain atrophy, separately beginning in the Broca’s area (subtype1) and the hippocampus (subtype2). The two trajectories are replicated in cross-validation samples. Individuals within each subtype are further classified into two stages (‘pre-atrophy’ and ‘post-atrophy’). These subtypes show different atrophy patterns and symptom profiles. Longitudinal data from 523 patients with schizophrenia treated by antipsychotics only or adjunct transcranial magnetic stimulation (TMS) reveal that antipsychotics-only effects relate to phenotypic subtype (more effective in the subtype1) while adjunct transcranial-magnetic-stimulation effects relate to the stage (superior outcomes in the pre-atrophy stage). These findings suggest distinct pathophysiological processes underlying schizophrenia that potentially yield to stratification and prognostication—a key requirement for personalizing treatments in enduring illnesses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data of COBRE, NMorphCH, FBIRN and NUSDAST were obtained from the SchizConnect, a publicly available website (http://www.schizconnect.org/documentation#by_project). The NMorphCH dataset and NUSDAST dataset were download through a query interface at the SchizConnect (http://www.schizconnect.org/queries/new). The COBRE dataset was download from the Center for Biomedical Research Excellence in Brain Function and Mental Illness (COBRE) (https://coins.trendscenter.org/). The FBIRN dataset was download from https://www.nitrc.org/projects/fbirn/. The DS000115 dataset was download from OpenfMRI database (https://www.openfmri.org/). Data from the other datasets (cross-sectional datasets #1, #2, #3, #4, longitudinal AMP and TMS data) are not publicly available for download, but access requests can be made to the respective study investigators: cross-sectional data (datasets #1, #2, #3, #4)—corresponding author J. Feng; APM data—J. Wang (jijunwang27@163.com), X. Yu (yuxin@bjmu.edu.cn), W. Yue (dryue@bjmu.edu.cn) and C. Luo (chengluo@uestc.edu.cn); TMS data—J. Wang (jijunwang27@163.com), G. Ji (jigongjun@163.com), L. Cui (cui_fmmu@163.com) and C. Luo (chengluo@uestc.edu.cn). Requests for raw and analysed data can be made to the corresponding author J. Feng and will be promptly reviewed by the Fudan University Ethics Committee to verify whether the request is subject to any intellectual property or confidentiality obligations.
Code availability
Python of the SuStaIn algorithm is available on the UCL-POND GitHub (https://github.com/ucl-pond). The T1-weighted images were processed using the Computational Anatomy Toolbox (http://www.neuro.uni-jena.de/cat/) within SPM12 (https://www.fil.ion.ucl.ac.uk/spm/software/spm12/). The visualization of ROI-wise z score images was conducted using BrainNetViewer (https://www.nitrc.org/projects/bnv/). Statistical analyses, including correlation analysis, t test and ANOVA, were conducted using MATLAB (version: R2018b) and SPSS Statistics (version: 26.0). Other custom codes developed in the current study are available at GitHub (https://github.com/YuchaoJiang91/Disease-Progress-Model).
References
The Global Burden of Disease: 2004 Update (World Health Organization, 2008).
Fusar-Poli, P. et al. Heterogeneity of psychosis risk within individuals at clinical high risk: a meta-analytical stratification. JAMA Psychiatry 73, 113–120 (2016).
McCutcheon, R. A. et al. The efficacy and heterogeneity of antipsychotic response in schizophrenia: a meta-analysis. Mol. Psychiatry 26, 1310–1320 (2021).
Collado-Torres, L. et al. Regional heterogeneity in gene expression, regulation, and coherence in the frontal cortex and hippocampus across development and schizophrenia. Neuron 103, 203–216 (2019).
Brugger, S. P. & Howes, O. D. Heterogeneity and homogeneity of regional brain structure in schizophrenia: a meta-analysis. JAMA Psychiatry 74, 1104–1111 (2017).
Insel, T. R. & Cuthbert, B. N. Medicine. Brain disorders? Precisely. Science 348, 499–500 (2015).
Braff, D. L., Ryan, J., Rissling, A. J. & Carpenter, W. T. Lack of use in the literature from the last 20 years supports dropping traditional schizophrenia subtypes from DSM-5 and ICD-11. Schizophr. Bull. 39, 751–753 (2013).
van Erp, T. G. et al. Subcortical brain volume abnormalities in 2,028 individuals with schizophrenia and 2,540 healthy controls via the ENIGMA consortium. Mol. Psychiatry 21, 547–553 (2016).
van Erp, T. G. M. et al. Cortical brain abnormalities in 4,474 individuals with schizophrenia and 5,098 control subjects via the Enhancing Neuro Imaging Genetics Through Meta Analysis (ENIGMA) Consortium. Biol. Psychiatry 84, 644–654 (2018).
Palaniyappan, L. Progressive cortical reorganisation: a framework for investigating structural changes in schizophrenia. Neurosci. Biobehav. Rev. 79, 1–13 (2017).
Alnaes, D. et al. Brain heterogeneity in schizophrenia and its association with polygenic risk. JAMA Psychiatry 76, 739–748 (2019).
Jiang, Y. et al. Progressive reduction in gray matter in patients with schizophrenia assessed with MR imaging by using causal network analysis. Radiology 287, 633–642 (2018).
Wannan, C. M. J. et al. Evidence for network-based cortical thickness reductions in schizophrenia. Am. J. Psychiatry 176, 552–563 (2019).
Jiang, Y. et al. Antipsychotics effects on network-level reconfiguration of cortical morphometry in first-episode schizophrenia. Schizophr. Bull. 48, 231–240 (2022).
Kirschner, M. et al. Orbitofrontal-striatal structural alterations linked to negative symptoms at different stages of the schizophrenia spectrum. Schizophr. Bull. 47, 849–863 (2021).
Wong, T. Y. et al. An overlapping pattern of cerebral cortical thinning is associated with both positive symptoms and aggression in schizophrenia via the ENIGMA consortium. Psychol. Med. 50, 2034–2045 (2020).
Wen, J. et al. Multi-scale semi-supervised clustering of brain images: deriving disease subtypes. Med. Image Anal. 75, 102304 (2022).
Lalousis, P. A. et al. Heterogeneity and classification of recent onset psychosis and depression: a multimodal machine learning approach. Schizophr. Bull. 47, 1130–1140 (2021).
Chand, G. B. et al. Two distinct neuroanatomical subtypes of schizophrenia revealed using machine learning. Brain 143, 1027–1038 (2020).
Yang, Z. et al. A deep learning framework identifies dimensional representations of Alzheimer’s disease from brain structure. Nat. Commun. 12, 7065 (2021).
Varol, E., Sotiras, A., Davatzikos, C. & Alzheimer’s Disease Neuroimaging, I. HYDRA: revealing heterogeneity of imaging and genetic patterns through a multiple max-margin discriminative analysis framework. Neuroimage 145, 346–364 (2017).
Dong, A. et al. Heterogeneity of neuroanatomical patterns in prodromal Alzheimer’s disease: links to cognition, progression and biomarkers. Brain 140, 735–747 (2017).
Dwyer, D. B. et al. Brain subtyping enhances the neuroanatomical discrimination of schizophrenia. Schizophr. Bull. 44, 1060–1069 (2018).
Luo, C. et al. Subtypes of schizophrenia identified by multi-omic measures associated with dysregulated immune function. Mol. Psychiatry 26, 6926–6936 (2021).
Tronchin, G. et al. Progressive subcortical volume loss in treatment-resistant schizophrenia patients after commencing clozapine treatment. Neuropsychopharmacology 45, 1353–1361 (2020).
Young, A. L. et al. Uncovering the heterogeneity and temporal complexity of neurodegenerative diseases with Subtype and Stage iInference. Nat. Commun. 9, 4273 (2018).
Vogel, J. W. et al. Four distinct trajectories of tau deposition identified in Alzheimer’s disease. Nat. Med. 27, 871–881 (2021).
Fillman, S. G. et al. Elevated peripheral cytokines characterize a subgroup of people with schizophrenia displaying poor verbal fluency and reduced Broca’s area volume. Mol. Psychiatry 21, 1090–1098 (2016).
Li, T. et al. Brain-wide analysis of functional connectivity in first-episode and chronic stages of schizophrenia. Schizophr. Bull. 43, 436–448 (2017).
Du, J. et al. The genetic determinants of language network dysconnectivity in drug-naive early stage schizophrenia. NPJ Schizophr. 7, 18 (2021).
Crow, T. J. Is schizophrenia the price that Homo sapiens pays for language? Schizophr. Res. 28, 127–141 (1997).
Palaniyappan, L. & Liddle, P. F. Does the salience network play a cardinal role in psychosis? An emerging hypothesis of insular dysfunction. J. Psychiatry Neurosci. 37, 17–27 (2012).
Steen, R. G., Mull, C., McClure, R., Hamer, R. M. & Lieberman, J. A. Brain volume in first-episode schizophrenia: systematic review and meta-analysis of magnetic resonance imaging studies. Br. J. Psychiatry 188, 510–518 (2006).
Lieberman, J. A. et al. Hippocampal dysfunction in the pathophysiology of schizophrenia: a selective review and hypothesis for early detection and intervention. Mol. Psychiatry 23, 1764–1772 (2018).
Palaniyappan, L. Inefficient neural system stabilization: a theory of spontaneous resolutions and recurrent relapses in psychosis. J. Psychiatry Neurosci. 44, 367–383 (2019).
Andreasen, N. C., Liu, D., Ziebell, S., Vora, A. & Ho, B. C. Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: a prospective longitudinal MRI study. Am. J. Psychiatry 170, 609–615 (2013).
Austin, S. F. et al. Long-term trajectories of positive and negative symptoms in first episode psychosis: a 10year follow-up study in the OPUS cohort. Schizophr. Res. 168, 84–91 (2015).
Galderisi, S., Mucci, A., Buchanan, R. W. & Arango, C. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry 5, 664–677 (2018).
Addington, J. & Addington, D. Positive and negative symptoms of schizophrenia: their course and relationship over time. Schizophr. Res. 5, 51–59 (1991).
Hasan, A. et al. Structural brain changes are associated with response of negative symptoms to prefrontal repetitive transcranial magnetic stimulation in patients with schizophrenia. Mol. Psychiatry 22, 857–864 (2017).
Pomponio, R. et al. Harmonization of large MRI datasets for the analysis of brain imaging patterns throughout the lifespan. Neuroimage 208, 116450 (2020).
Erikainen, S. & Chan, S. Contested futures: envisioning ‘personalized,’ ‘stratified,’ and ‘precision’ medicine. New Genet. Soc. 38, 308–330 (2019).
Liu, Z. et al. Resolving heterogeneity in schizophrenia through a novel systems approach to brain structure: individualized structural covariance network analysis. Mol. Psychiatry 26, 7719–7731 (2021).
Wang, L. et al. SchizConnect: mediating neuroimaging databases on schizophrenia and related disorders for large-scale integration. Neuroimage 124, 1155–1167 (2016).
Fonteijn, H. M. et al. An event-based model for disease progression and its application in familial Alzheimer’s disease and Huntington’s disease. Neuroimage 60, 1880–1889 (2012).
Lawson, R. G. & Jurs, P. C. New index for clustering tendency and its application to chemical problems. J. Chem. Inf. Comput. Sci. 30, 36–41 (1990).
Pan, Y. et al. Morphological profiling of schizophrenia: cluster analysis of MRI-based cortical thickness data. Schizophr. Bull. 46, 623–632 (2020).
Sugihara, G. et al. Distinct patterns of cerebral cortical thinning in schizophrenia: a neuroimaging data-driven approach. Schizophr. Bull. 43, 900–906 (2017).
Groppe, D. M., Urbach, T. P. & Kutas, M. Mass univariate analysis of event-related brain potentials/fields I: a critical tutorial review. Psychophysiology 48, 1711–1725 (2011).
Acknowledgements
This work was supported by the grant from Science and Technology Innovation 2030-Brain Science and Brain-Inspired Intelligence Project (grant no. 2021ZD0200204 to J.Z.; no. 2022ZD0212800 to Y.T.). This work was supported by National Natural Science Foundation of China (no. 82202242 to Y.J.; no. 82071997 to W.C.; no. 81825009 to W.Y.; no. 82271949 to L.-B.C.; no. 82151314 to J.W.). This work was supported by grants from the National Key R&D Program of China (no. 2022ZD0208500 to D.Y.) and the CAMS Innovation Fund for Medical Sciences (no. 2019-I2M-5-039 to C.L.). This work was supported by the Shanghai Rising-Star Program (no. 21QA1408700 to W.C.) and the Shanghai Sailing Program (22YF1402800 to Y.J.) from Shanghai Science and Technology Committee. This work was supported by the projects from China Postdoctoral Science Foundation (no. BX2021078 and 2021M700852 to Y.J.). This work was supported by National Key R&D Program of China (no. 2019YFA0709502 to J.F.), the grant from Shanghai Municipal Science and Technology Major Project (no. 2018SHZDZX01 to J.F.), ZJ Lab, Shanghai Center for Brain Science and Brain-Inspired Technology, and the grant from the 111 Project (no. B18015 to J.F.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. L.P. acknowledges support from the Monique H. Bourgeois Chair (McGill University) and Tanna Schulich Chair of Neuroscience and Mental Health (Schulich School of Medicine & Dentistry, Western University) and a salary award from the Fonds de recherche du Quebec-Sante ́ (FRQS). We also thank the investigators who provided public access to MRI data from patients diagnosed with schizophrenia through the COBRE database funded by a Center of Biomedical Research Excellence grant 5P20RR021938/P20GM103472 from the NIH to V. Calhoun, the fBIRN data supported by grants to the Function BIRN (U24-RR021992) Testbed funded by the National Center for Research Resources at the National Institutes of Health, USA, the NMorphCH dataset funded by NIMH grant R01MH056584 and the SchizConnect funded by NIMH cooperative agreement 1U01 MH097435. This work is supported by the Zhangjiang International Brain Biobank (ZIB) Consortium.
Author information
Authors and Affiliations
Consortia
Contributions
J.F. led the project. Y.J., W.C. and J.F. were responsible for the study concept and the design of the study. J.W. and E.Z. provided crucial advice for the study. Y.J., E.Z., C.X., W.Z., J.L., D.C., C.S., X.W., B.Z., N.K., Y.-J.S. and J.K. analysed the data and created the figures. Y.J. wrote the manuscript. J.W., E.Z., L.P. and W.C. made substantial contributions to the manuscript and provided critical comments. J.W., E.Z., C. Luo, G.J., J.Y., Y.W., Y.Z., C.-C.H., S.-J.T., X.C., J.Z., H. Huang, H.He, M.D., Y.T., T.Z., C. Li, X.Y., T.S., W.Y., Z.L., L.-B.C., K.W., J.C., C.-P.L. and D.Y. contributed to the data acquisition.
Corresponding authors
Ethics declarations
Competing interests
L.P. reports personal fees from Janssen Canada, Otsuka Canada, SPMM Course Limited, UK, Canadian Psychiatric Association; book royalties from Oxford University Press; investigator-initiated educational grants from Janssen Canada, Sunovion and Otsuka Canada outside the submitted work. These interests played no role in the research reported here. Other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Johanna Seitz-Holland, Vince Calhoun, Jing Sui and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Integrated supplementary information
Extended Data Fig. 1 A flowchart of systematic characterization of heterogeneity in brain atrophy patterning.
(a) A total of cross-sectional MRI from 2170 individuals (1124 patients with schizophrenia) was used to characterize heterogeneity in brain atrophy patterning of schizophrenia. (b) Brain images were processed using voxel-based morphometry. GMV was extracted from ROIs based on the Automated Anatomical Labeling (AAL) atlas and adjusted by regressing out the effects of sex, age, the square of age, TIV and site effects. (c) Adjusted GMV values were normalized relative to control population using z scores. Higher z scores represent larger deviations from the normal (that is, more severe atrophy in patients with schizophrenia). (d) Brain pathophysiological model (that is, SuStaIn [31]) requires both spatial (brain regions) and temporal (z scores representing advancing atrophy severity) features as input (that is, an M × N z score matrix). Here, N represents the number of individuals with schizophrenia (N = 1124 in this study). M represents the number of ROIs (M = 17). (e) SuStaIn was used to identify diverse but distinct patterns of progression using cross-sectional neuroimaging data and to cluster individuals while accounting for disease progression. (f) Individuals with schizophrenia were classified according to the sequence of atrophy in different brain regions. For each subtype, brain-based staging was assessed from progressive spatial patterns with distinct origins. (g) Using a longitudinal sample, we examined whether subtype classification based on baseline brain features predict differential treatment response to antipsychotic medications and TMS.
Extended Data Fig. 2 Association between regional atrophy and clinical symptoms.
Spearman correlation analysis between PANSS (positive, negative and general psychopathology subscales) and GMV z scores were performed after adjusting for sex, age, the square of age, TIV and sites. Colored bar represents the r value after controlling the FWE corrected P < 0.05. L, left hemisphere; R, right hemisphere.
Supplementary information
Supplementary Information
Supplementary methods 1–10, tables 1–14 and figs. 1–10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, Y., Wang, J., Zhou, E. et al. Neuroimaging biomarkers define neurophysiological subtypes with distinct trajectories in schizophrenia. Nat. Mental Health 1, 186–199 (2023). https://doi.org/10.1038/s44220-023-00024-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00024-0
This article is cited by
-
Integrative omics analysis reveals epigenomic and transcriptomic signatures underlying brain structural deficits in major depressive disorder
Translational Psychiatry (2024)
-
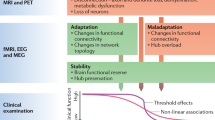
Data-driven modelling of neurodegenerative disease progression: thinking outside the black box
Nature Reviews Neuroscience (2024)
-
Longitudinal inference of multiscale markers in psychosis: from hippocampal centrality to functional outcome
Molecular Psychiatry (2024)
-
Identification of four biotypes in temporal lobe epilepsy via machine learning on brain images
Nature Communications (2024)
-
Cortical structural changes of morphometric similarity network in early-onset schizophrenia correlate with specific transcriptional expression patterns
BMC Medicine (2023)