Abstract
The COVID-19 pandemic has seen a rise in anxiety and depression among adolescents. This study aimed to investigate the longitudinal associations between sleep and mental health among a large sample of Australian adolescents and examine whether healthy sleep patterns were protective of mental health in the context of the COVID-19 pandemic. We used three waves of longitudinal control group data from the Health4Life cluster-randomized trial (N = 2781, baseline Mage = 12.6, SD = 0.51; 47% boys and 1.4% ‘prefer not to say’). Latent class growth analyses across the 2 years period identified four trajectories of depressive symptoms: low-stable (64.3%), average-increasing (19.2%), high-decreasing (7.1%), moderate-increasing (9.4%), and three anxiety symptom trajectories: low-stable (74.8%), average-increasing (11.6%), high-decreasing (13.6%). We compared the trajectories on sociodemographic and sleep characteristics. Adolescents in low-risk trajectories were more likely to be boys and to report shorter sleep latency and wake after sleep onset, longer sleep duration, less sleepiness, and earlier chronotype. Where mental health improved or worsened, sleep patterns changed in the same direction. The subgroups analyses uncovered two important findings: (1) the majority of adolescents in the sample maintained good mental health and sleep habits (low-stable trajectories), (2) adolescents with worsening mental health also reported worsening sleep patterns and vice versa in the improving mental health trajectories. These distinct patterns of sleep and mental health would not be seen using mean-centred statistical approaches.
Similar content being viewed by others
Introduction
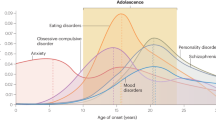
Mental disorders are the leading cause of disability among young people aged up to 24 years worldwide, accounting for one quarter of all years lived with disability1. In Australia, mental disorders make up three of the five leading causes of burden of disease among those aged 12–24 years2 and cost the economy approximately $200–220 billion yearly3. The COVID-19 pandemic has caused disruptions to all facets of adolescent development and exacerbated mental health issues such as depression, anxiety and self harm4,5,6,7. Examining modifiable factors that were protective of mental health throughout this global crisis can offer insights on targets for prevention and early intervention, especially since improving the mental health of young people is a critical public health priority8.
There is growing evidence that sleep is a key modifiable factor associated with mental health9,10,11,12,13,14. Human sleep is primarily under biological control, governed by the well-supported two-process model of sleep15,16. The first process is sleep homeostatis, whereby pressure to sleep builds across the waking day and evening and dissipates during sleep. As adolescents develop, their ability to build sleep pressure in the evening declines, resulting in increased alertness in the evening. This inevitably results in a delay in the onset of sleep (i.e., a longer sleep onset latency)16. The second process—the circadian rhythm—is a cycle of sleep and wake across the 24 h day, and is of particular relevance during adolescence. From about age 10 to 20 years, the timing of the circadian rhythm delays, resulting in a later onset of sleep in the evening, and a later rise time (when allowed to sleep-in)16. However, 5 out of 7 days of the week, adolescents are prevented from sleeping at their natural circadian times as they need to wake relatively early to prepare for, travel to, and attend school17. This inevitably results in a restriction of sleep across the school week (i.e., shortened total sleep time) and weekend catch-up, which leads to irregular sleep and pepetuates weekday sleep debt17.
Multiple studies have shown that poor sleep during paediatric development can increase the odds of developing anxiety and depression, with two mechanisms implicated9. First, the restriction of sleep (less total sleep time) has been shown to dampen positive mood and hinder one’s next-day emotion regulation9. Second, an extended sleep onset latency is proposed to create an ideal environment for repetitive negative thinking (i.e., worry and rumination), which has been linked to both depression and anxiety in young people. An extended sleep onset latency is common among later chronotypes, which may be a predisposing factor for the development of depression and anxiety symptoms18. Conversely, a healthy sleep profile (particularly short sleep onset latency—between 5 and 30 min19, sufficient total sleep time—between 8 and 10 h20, and less daytime sleepiness) is associated with increased mental resilience (i.e., lower symptoms of anxiety and depression)21,22. Therefore, sleep is an important risk-/protective factor for the development of mental ill-health.
During the COVID-19 pandemic, mental resilience was tested on a global scale, and many adolescents experienced heightened psychopathology4,5,6,7. Sleep was also impacted, potentially relating to heightened stress and restrictions on movement and closure of schools; however, evidence as to whether healthy sleep improved or worsened has been mixed23,24,25. Surprisingly, one longitudinal study found that the prevalence of depressive symptoms, anxiety symptoms and sleep problems was higher before, compared to during and after, the pandemic26. While studies focusing on average changes are informative, they might miss for whom changes occur. Did all adolescents experience worse sleep and mental health? Were adolescents with healthy sleep patterns more resilient? For example, later chronotype26,27, shorter sleep duration27 and insomnia symptoms28 were associated with higher risk for adolescents’ mental ill-health during the pandemic. Identifying subgroups of adolescents at lower risk for mental ill-health during the pandemic, and thoroughly examining protective sleep characteristics, can inform key targets for prevention and early interventions in this population. Previous studies, however, have examined changes across their entire samples, and have examined only a few interindividual differences in sleep patterns.
To address this gap, we utilised data from pre-pandemic (2019), and during the pandemic (in the latter half of 2020 and 2021) among a large sample of early- to mid-Australian adolescents29. Using a person-centred analysis, we examined whether adolescents who experienced lower and stable levels of anxiety and depression before and during the pandemic had healthier sleep patterns (i.e., shorter sleep onset latency and night-time awakenings, sufficient total sleep time, low levels of sleepiness, an earlier chronotype, and shorter catch-up sleep on weekends) compared to adolescents experiencing poor and worsening mental health symptoms.
Results
Descriptive statistics
The analytical sample of the current study consisted of 2781 students (baseline Mage = 12.6, SD = 0.5; 47% boys and 1.4% ‘prefer not to say’). The largest group was from New South Wales (49.8%), followed by Western Australia (28.1%), and Queensland (22.2%). The average perceived socioeconomic status in the sample was 9.43 (range 0–13; SD = 1.85). The majority of adolescents were born in Australia (86.2%) or another English-speaking country (6.9%). In line with this, the majority reported speaking English at home (93.1%). Means and standard deviations of depressive and anxiety symptoms and sleep variables (sleepiness, weekday sleep duration, sleep onset latency [SOL], wake after sleep onset [WASO], and chronotype) are presented in Table 1.
Changes in depressive and anxiety symptoms over time
Two separate latent growth curve models were estimated to examine whether and how adolescents’ depressive and anxiety symptoms changed over time, from early to mid-adolescence and throughout the pandemic. Both yielded a good model fit (see Table 2). The mean of the slope was positive and statistically significant for both depression and anxiety symptoms, which indicates that on average, participants reported increasing symptoms over time. The variances of the slope and the intercept were both statistically significant, which indicates that adolescents differed both in the level of depressive and anxiety symptoms at T1 and in how they changed from T1 to T3 (see Table 2). Therefore, we went on to explore subgroups of adolescents following different trajectories of depressive and anxiety symptoms.
Depressive symptoms subgroup trajectories
We used latent class growth analysis (LCGA) to identify subgroups of adolescents who followed different trajectories of depressive symptoms over time and found four different trajectories (see “Supplementary material”). The first class (high-decreasing) included 7.1% of the sample. Adolescents in this class reported high levels of depressive symptoms at T1 and average symptoms at T3, relative to the sample average scores. The second class (average-increasing) included 19.2% of the sample and started at average levels of depression before the pandemic and increased to moderate symptoms over time. The third class (low-stable) represented 64.3% of the sample, who were adolescents reporting low symptoms of depression at T1 and their symptoms remained stable over time. The final trajectory class (moderate-increasing) represented 9.4% of the sample. Adolescents in this class reported higher-than-average levels of depressive symptoms at T1 and showed a significant increase in their symptoms over time. The four trajectories and the estimated mean changes are shown in Fig. 1. The four trajectories significantly differed in their symptoms levels at T1 [F(3,2777) = 1379.0, p < 0.001], at T2[F(3,2276) = 537.63, p < 0.001], and T3 [F(3,2091) = 2894.02, p < 0.001]. Depressive symptoms means and SDs for each trajectory at each time point are presented in Table 3.
Anxiety symptoms trajectories
Analysis for anxiety symptoms yielded three different trajectories (see Supplementary material). The first class (high-decreasing) included 13.6% of the sample. Adolescents in this trajectory showed a statistically significant decline in anxiety symptoms, but still well above the average for the whole sample. The second trajectory (average-increasing) included 11.6% of the sample and went from average to high symptoms from T1 to T3. The third trajectory (low-stable) included 74.8% of the sample and showed a slight but significant increase in anxiety symptoms over time, although still in the low range. The three trajectories and the estimated mean changes are shown in Fig. 2. The three trajectories significantly differed in their symptoms levels at T1 [F(2,2641) = 2154.50, p < 0.001], at T2[F(2,2182) = 979.60, p < 0.001], and T3 [F(2,2031) = 1281.02, p < 0.001]. Anxiety symptoms means and SDs for each trajectory at each time point are presented in Table 3.
Sleep and sociodemographic characteristics among adolescents by trajectories of depressive symptoms
Sex distribution was significantly different among adolescents with different trajectories of depressive symptoms, χ2(6) = 151.25, p < 0.001. In the high-decreasing group, girls were the majority (58%) together with the largest proportion of adolescents answering “prefer not to say” for their sex at birth (4%). Girls were overrepresented in the low-increasing trajectory (67.7% vs. 30.6% boys) and in the average-increasing trajectory (67.8% vs. 30.7% boys). Boys represented the majority in the low-stable trajectory (75.7% vs. 54.5% girls). Some differences in cultural and linguistic diversity emerged, χ2 = 12.0, p = 0.007, with the high-decreasing trajectory having the highest proportion of adolescents with an immigrant background (18.9%), followed by the low-stable group (10.5%) and the average-increasing and moderate-increasing (8.3% and 8.4% respectively). Relative socioeconomic position did not differ among the trajectories χ2 = 3.3, p = 0.348.
Table 3 shows the comparisons for sleep characteristics for each of the depressive symptom trajectories. Adolescents in the low-stable trajectory of depressive symptoms reported significantly better sleep patterns at all time points, including the shortest SOL and WASO, the longest sleep duration, the lowest sleepiness, and the earliest chronotype. Adolescents in the high-decreasing trajectory of depressive symptoms showed the worst sleep patterns compared to the other groups at T1, but by T3 there were no significant differences from the low-stable group in WASO, sleep duration, and chronotype. Sleepiness and SOL were still high but no longer the highest compared to adolescents in the two increasing-symptoms trajectories. In fact, adolescents in the two increasing trajectories were better off at T1, but reported significantly longer SOL and WASO, shorter sleep duration, excessive daytime sleepiness (> 17)30 and later chronotype by T3. Interestingly, SOL was problematic in all trajectories, as it was close to or above the clinical guidelines of 30 min required for sleep-onset insomnia19.
Sleep and sociodemographic characteristics among adolescents by trajectories of anxiety symptoms
Sex distribution was significantly different among adolescents in different trajectories of anxiety symptoms, χ2(4) = 181.26, p < 0.001. In the high-decreasing trajectory, girls were the largest group (73.5%) together with the largest proportion of adolescents answering “prefer not to say” for their sex at birth (2.4%). Girls were also overrepresented in the average-increasing trajectory (72.3% vs. 26.5% boys) whereas boys were slightly overrepresented in the low-stable trajectory (54.4% vs. 44.4% girls). Adolescents differed in cultural and linguistic diversity, χ2 = 9.11, p = 0.011, with the average-increasing trajectory having the lowest proportion of adolescents with an immigrant background (8.4%), compared to the low-stable (10.2%) and the high-decreasing group (13%). Relative socioeconomic position did not differ among the trajectories χ2 = 1.75, p = 0.416.
Table 4 shows the comparisons for sleep characteristics for each of the anxiety symptom trajectories. Adolescents in the low-stable trajectory of anxiety symptoms reported significantly better sleep patterns at all time points compared to the other groups, including the shortest SOL and WASO, the longest sleep duration, the lowest sleepiness, and the earliest chronotype. Adolescents in the high-decreasing trajectory of anxiety symptoms showed the worst sleep patterns compared to the other groups at T1, but by T3 there was no significant difference in WASO compared to the low-stable group and their sleep duration was no longer the shortest. Yet, sleepiness was still above recommended levels (> 17) and chronotype significantly later than the low-stable trajectory. Adolescents in the average-increasing trajectories started with similar SOL, WASO, and chronotype as the low-stable trajectory, but already reported a significantly shorter sleep duration and more sleepiness. By the end of the study, they were worse off in all sleep parameters. As in the depressive symptom trajectories, SOL was problematic in all groups (i.e., ≥ 30 min).
Discussion
The aim of this study was to explore whether healthy sleep patterns were protective of adolescent mental health throughout the COVID-19 pandemic.
In the present study, both depression and anxiety symptoms generally increased over time. While this trend is similar to pre-pandemic studies for depression, it is in the opposite direction for anxiety, whose symptoms have previously shown to decline from childhood throughout adolescence31. A recent meta-analysis of mental health changes throughout the pandemic shows a clear increase in depressive symptoms in children and adolescents, and a slight increase in anxiety symptoms, with girls generally showing worse mental health6. Similar to previous trajectory-studies examining depressive and anxiety symptoms32,33, in the present study, not all adolescents displayed increasing symptoms: the majority of adolescents reported stable-low symptoms of both anxiety and depression, and a small portion of adolescents showed improving mental health. Identifying modifiable protective factors reported by adolescents in these low and declining symptom trajectories is crucial for promoting mental health in this population. In this study, we examined sleep as a potential protective factor and found that adolescents in low-risk trajectories of anxiety and depression consistently reported the healthiest sleep patterns. These healthy sleep characteristics included: (1) longer weekly sleep duration, (2) earlier chronotype, (3) lower sleepiness, (4) shorter sleep latency and time awake during the night. Weekend catch-up was significantly shorter for the low-stable trajectory of depression but was not significantly different between the trajectories of anxiety. When looking at the divergent trajectories of increasing vs decreasing symptoms of anxiety and depression, some interesting differences emerged.
Among adolescents whose depressive symptoms improved over time, sleep duration no longer differed from the low-risk trajectory by the end of the study. Similarly, for adolescents whose anxiety symptoms improved over time, their sleep duration was no longer the shortest compared to increasing-symptom trajectories. This is not surprising, as studies examining the link between sleep duration and mental health have found a dose-response association that supports the positive association between the recommended 8–10 h of sleep for adolescents and emotional health34,35. Chronotype followed similar trends as sleep duration, as a later chronotype leads to later bedtimes during schooldays, shortening the sleep opportunity when wake-times are fixed36. In contrast, an early chronotype seems to be protective for adolescents’ mental health, in line with previous studies during the pandemic26,27. An interesting finding was that the chronotype of adolescents in the high-decreasing trajectory of depression was significantly later than the other trajectories at T1, but did not differ from adolescents in the low-risk trajectory by the end of the study. Conversely, chronotype became significantly later for adolescents in the two increasing trajectories of depressive symptoms. This suggests that the natural delay in sleep timing slowed for teenagers whose depressive symptoms improved, while it delayed further for adolescents with increasing symptoms. This finding is worth exploring further, as an earlier chronotype has been found to be protective for depression for several reasons, not only because it is linked to earlier bedtimes and longer sleep duration, but also because it better aligns with the environment (e.g., bright light exposure) and with social obligations (e.g., morning school times)18. One hypothesis may be that for some adolescents, the more unstructured nature of online classes could have prompted more irregular sleep routines, making room for a delay in bed- and wake-times (and a later sleep midpoint/chronotype). However, some adolescents were able to increase their sleep duration and maintain (rather than delay) their timing. In this study, we did not directly assess lockdown status, but a previous study found a general increase in sleep duration in this population, independent of lockdown measures25. This might also explain the relatively small difference in weekend catchup between trajectories. Future studies should further explore what may explain these variations in chronotype, including individual characteristics and contextual factors (e.g., self-control, parental rules about sleep).
In addition to sleep quantity, perceived sleep quality is an important aspect closely linked to mental wellbeing22. Experts agree that measures of sleep continuity are good indicators of sleep quality19. In particular, time taken to fall asleep as well as time awake at night are hypothesised as important mechanisms for both anxiety and depression, as they create an opportunity for worry at a time when more adaptive emotion regulation strategies might not be activated12. Although SOL was markedly long among all adolescents (> 30 min), it was consistently shorter in the low-risk trajectories of both anxiety and depression, and no longer the longest among decreasing-symptom trajectories. Time awake at night followed similar trends. Finally, we also examined daytime complaints in relation to depression and anxiety symptoms. In the present study, teenagers who belonged to improving mental health symptom trajectories no longer reported the highest sleepiness by the end of the study, compared to worsening mental health symptom trajectories. Feelings of tiredness have been previously found to be both cross-sectionally and longitudinally linked to anxiety and depression in adolescents22. All in all, these results show significantly better sleep quality and quantity and less daytime sleepiness among adolescents with better mental health across the pandemic years. Furthermore, the divergent trajectories of anxiety and depressive symptoms clearly show that sleep patterns followed closely.
Sleep and mental health are closely intertwined. The aim of this study was not to discern directionality, rather we aimed to use a person-oriented perspective to inform who is at risk for developing problems, and poor sleep characteristics were a common determinant among risk-trajectories for both anxiety and depressive symptoms. Some differences in sleep patterns existed from the start of the study—for example, adolescents in the average-increasing trajectory of depression already reported overall worse sleep health compared to the low-stable trajectory. For the average-increasing trajectory of anxiety, sleep duration and sleepiness were distinct from the low-risk adolescents. These differences in sleep patterns could help explain why the pandemic sparked an increase in mental health problems in these adolescents and can potentially aid in the identification of individuals in need of early interventions. In fact, a recent study found that stressful events were followed by an increase in sleep problems and later increases in anxiety symptoms within a few months among adolescents37. Nonetheless, it might still be difficult to identify these emerging risk-groups (average-increasing trajectories), as their sleep was significantly different from the low-stable trajectories but it was not yet problematic (e.g., sleep duration close to the recommended 8 h/night20; see Tables 4, 5). This supports the importance of promoting sleep health in the adolescent population in a universal manner, as some of the adolescents at-risk might easily be missed. Given that the link between sleep and mental health is ultimately bi-directional and can create a vicious cycle of poor emotional regulation and poor sleep quality and quantity38, breaking this cycle by targeting sleep is warranted and has shown promising benefits for mental health9. For example, sleep has shown significant improvements (sleep onset latency in particular) alongside symptoms of depression following bright light therapy, cognitive behavioural therapy for insomnia (CBT-I), school-based sleep interventions9, and later school-start times39. Two recent meta-analyses found evidence that improving sleep can lead to an improvement in both anxiety and depressive symptoms40,41. In addition, addressing sleep problems first can be advantageous because it is less stigmatized and easier to talk about compared to mental health40.
The present study has a number of strengths and limitations that need to be taken into account when interpreting the results. Mental health symptoms and sleep patterns were self-reported, which can be subject to error and common method bias. However, externally developed measures that have been validated in adolescents were used. Although objective sleep measures are encouraged in future studies, self-reported sleep has proven valid compared to actigraphy42,43. This is also a more feasible method when including a large sample of adolescents followed over time. The large and diverse sample, spanning three Australian states is a strength of the study, together with the longitudinal design, which enabled to capture changes throughout the pandemic. Despite the three waves of longitudinal data, the results of this study cannot discern whether sleep patterns or mental health precede one another. More frequent longitudinal sampling could have provided a clearer picture44. However, using sophisticated person-oriented analyses allowed to highlight that not all adolescents were impacted the same way during the COVID-19 pandemic. In fact, the majority of the sample coped well during this stressful time (low-stable trajectories) and these low-risk classes also reported the healthiest sleep patterns. In addition, although WASO and SOL decreased over time in the whole sample, when looking at subgroups the decrease occurred only among adolescents whose symptoms improved. These important results might have been missed if only average changes were examined.
To conclude, sleep and mental health go hand-in-hand for adolescents. During a stressful time such as the COVID-19 pandemic, good sleep health was distinctive of adolescents who maintained low and stable symptoms of anxiety and depression. Given the bidirectional nature of the link between sleep and mental health, promoting healthy sleep habits in adolescents is a promising modifiable factor to improve and maintain mental health. Adolescent mental health is a public health priority8, and this study provides empirical evidence that sleep health should be one central target for prevention and intervention.
Method
Design and participants
This study utilises data from the “Health4Life” cluster randomised controlled trial, which aimed to evaluate the efficacy of an eHealth intervention targeting six modifiable risk factors among Australian adolescents (sleep, physical activity, diet, screen time, alcohol use and tobacco smoking). Baseline data were collected in 2019 (approximately July-November) using online self-report surveys among Year 7 students at 71 secondary schools across New South Wales (NSW), Queensland (QLD) and Western Australia (WA), with follow up surveys conducted in 2020 (approximately July-December) and 2021 (approximately July-December). To avoid contamination effects from the intervention, this study focuses on control group data. Only students with data on depressive and anxiety symptoms at baseline were included (Depressive symptom trajectories: NT1 = 2781, NT2 = 2280, NT3 = 2095; Anxiety symptom trajectories: NT1 = 2781, NT2 = 2267, NT3 = 2088). Participants provided written consent and parents provided passive, active written or active verbal consent, depending on the approved procedures for the school/region. The Health4Life trial was performed in accordance with relevant guidelines and regulations, it was registered with the Australian and New Zealand Clinical Trials registry (ACTRN12619000431123) and has ethical approval from ten relevant committees (University of Sydney HREC2018/882, NSW Department of Education SERAP 2019006, University of Queensland 2019000037, Curtin University HRE2019-0083 and several Catholic Diocese committees). The study protocol provides further details on recruitment and consent procedures29.
Measures
Sociodemographic characteristics
Sociodemographic factors included sex assigned at birth, age, cultural and linguistic diversity (CALD), and relative socioeconomic position. CALD was defined as per recommendations from a recent Australian review45 to include participants who were born in a non-English speaking country and/or primarily speak a language other than English at home. Relative family affluence was identified using the Family Affluence Scale III (FASIII), which has demonstrated good test–retest reliability (r = 0.90) and strong correlation with parental report46. The FASIII generates a summed score across indicators of familial wealth (e.g., number of computers, number of bathrooms in home, etc.) as a proxy for familial socioeconomic status that children and adolescents might be better at reporting compared to parent or caregivers’ income and education.
Sleep patterns
Average sleep duration per night was measured using the validated Modified Sleep Habits Survey42,43. Students reported the time they usually: (1) went to bed (time—12 h format), (2) attempted sleep (time—12 h format), (3) took to fall asleep (duration—h, min), (4) were awake during the night (duration—h, min), and 5() woke up in the morning (time—12 h format) over the past week (separately for week nights and weekend nights). In the present study, we derived several sleep parameters, including sleep onset latency (SOL; i.e., time taken to fall asleep), wake after sleep onset (WASO; i.e., time awake during the night), total sleep time (TST; i.e., time between falling asleep and wake up in the morning, minus WASO) during schooldays, and chronotype. We calculated chronotype as the midpoint of sleep on free days (i.e., sleep onset time on weekends plus sleep duration on weekends, divided by 2). According to Roenneberg et al.47 a correction needs to be made as many adolescents restrict their sleep on schooldays and attempt to catch up on weekends. Therefore, if the sleep duration on weekends is longer than on schooldays, sleep midpoint is calculated as sleep onset time (weekends) plus sleep duration (average schoolday-weekend) divided by 2. The midpoint of sleep is a good behavioural marker for circadian phase47. Finally, to examine irregular sleep patterns during weekdays and weekends, we calculated “weekend sleep-in” by subtracting wake-up time on weekends—wake-up time on weekdays48.
Sleepiness
The Pediatric Daytime Sleepiness Scale was used to assess daytime sleepiness30. It has been validated in adolescents and includes eight items such as ‘How often do you fall asleep or feel drowsy in class?’ and ‘How often do you have trouble getting out of bed in the morning?’ with five response options from ‘Never’ (0) to ‘Very often/ always’ (4), with scores ranging from 0 to 32. The cutoff for excessive sleepiness is 14 for boys and 17 for girls30. The Cronbach’s alpha was acceptable (α = 0.72).
Anxiety
Past 7-day anxiety symptoms were assessed with the PROMIS Anxiety Paediatric (PROMIS-AP) scale, which has been validated among adolescents49. The 13-item scale asks participants to report frequency of symptoms including difficulty relaxing, and feelings of nervousness, worry, and fear, amongst others on a scale from ‘never’ (1) to ‘almost always’ (5), the total ranging from 13–6549. The Cronbach’s alpha was 0.94.
Depression
Past 7-day depressive symptoms were measured using the modified Patient Health Questionnaire for Adolescents scale (PHQ-A)50. The 9-item scale asks participants to report how often they experienced symptoms such as “feeling down, depressed, irritable or hopeless”, sleep issues, tiredness, and changes in appetite, weight or behaviours on a scale from ‘not at all’ (0) to ‘nearly every day’ (3)50. The 9th item (measuring thoughts of death and self-harm) was removed on request of the ethics board. In addition, 2 items were excluded from analyses because of their overlap with sleep, our variable of interest. Depression symptoms were analysed using a sum of the remaining six items, ranging from 0–18 (Cronbach’s alpha = 0.84).
Data analysis
We followed a two-step procedure to identify different mental health trajectories51. In Step 1, we estimated a latent curve growth model to examine how, on average, adolescents’ mental health symptoms changed over a 2 years period, and to examine whether there was a significant between-person variation in intercept (initial level) and slope (change over time) of depression and anxiety. In Step 2, we used latent class growth analysis (LCGA) to identify adolescents with different mental health trajectories. To determine the number of trajectories that best fit the data we looked for the lowest Bayesian Information Criterion (BIC), highest entropy (i.e., classification accuracy), non-significant Lo–Mendell–Rubin test (LMR; i.e., model fit improvement from n − 1 to n classes), and the proportion of adolescents in each group trajectory (> 5%)52. When these indicators were contrasting, we chose the most parsimonious solution (i.e., fewer classes)52. We analyzed trajectories for depressive symptoms and anxiety separately. To validate the distinctiveness of the classes, we compared depression and anxiety symptom trajectories on symptom levels at each time point using ANOVAs. After establishing the different trajectories, we compared adolescents in each trajectory on sex distribution and sleep parameters across three time points using the BCH method in Mplus53. This method uses a weighted multiple group analysis, where the groups correspond to the latent classes, and therefore the classes established in the LCGA model are not affected in this second step (i.e., when analysing differences in sleep patterns)53. Data were analysed in SPSS (v. 26) and Mplus54. We handled missing data in Mplus using full information maximum likelihood (FIML). Depressive symptoms model: 4 missing data patterns, covariance coverage ranged between 0.67 and 1.00. Anxiety model: 4 missing data patterns, covariance coverage ranged between 0.67 and 1.00. The covariance coverage was well above the recommended 0.10 to reliably use FIML. Moreover, FIML is a superior method compared to mean imputation, listwise deletion or pairwise deletion, as it provides more reliable standard errors55.
Data availability
The data underlying this article cannot be shared publicly due to the agreement made with the individuals that participated in the study. The data will be shared on reasonable request to the corresponding author.
References
Erskine, H. E. et al. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol. Med. 45(7), 1551–1563 (2015).
Australian Institute of Health and Welfare. Health of Young People. https://www.aihw.gov.au/reports/children-youth/health-of-young-people (2020).
Australian Government Productivity Commission. Mental Health. https://www.pc.gov.au/inquiries/completed/mental-health/report (2020).
Viner, R. et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: A systematic review. JAMA Pediatr. 176(4), 400–409 (2022).
Samji, H. et al. Mental health impacts of the COVID-19 pandemic on children and youth – A systematic review. Child Adolesc. Ment. Health 27(2), 173–189 (2022).
Madigan, S. et al. Changes in depression and anxiety among children and adolescents from before to during the COVID-19 pandemic: A systematic review and meta-analysis. JAMA Pediatr. 177(6), 567–581 (2023).
Bower, M. et al. A hidden pandemic? An umbrella review of global evidence on mental health in the time of COVID-19. Front. Psychiatry 14, 1664–2640. https://doi.org/10.3389/fpsyt.2023.1107560 (2023).
World Health Organization (WHO). WHO-UNICEF Helping Adolescents Thrive Initiative. https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/who-unicef-helping-adolescents-thrive-programme (2023).
Gradisar, M. et al. Sleep’s role in the development and resolution of adolescent depression. Nat. Rev. Psychol. 1, 512–523 (2022).
Jamieson, D., Broadhouse, K. M., Lagopoulos, J. & Hermens, D. F. Investigating the links between adolescent sleep deprivation, fronto-limbic connectivity and the onset of mental disorders: A review of the literature. Sleep Med. 66, 61–67 (2020).
Jamieson, D., Shan, Z., Lagopoulos, J. & Hermens, D. F. The role of adolescent sleep quality in the development of anxiety disorders: A neurobiologically-informed model. Sleep Med. Rev. 59, 101450. https://doi.org/10.1016/j.smrv.2021.101450 (2021).
Lovato, N. L. & Gradisar, M. A. Meta-analysis and model of the relationship between sleep depression in adolescents: Recommendations for future research and clinical practice. Sleep Med. Rev. 18, 521–529 (2014).
Marino, C. et al. Association between disturbed sleep and depression in children and youths: A systematic review and meta-analysis of cohort studies. JAMA Netw. Open 4(3), e212373. https://doi.org/10.1001/jamanetworkopen.2021.2373 (2021).
Short, M. A., Gradisar, M., Lack, L. C. & Wright, H. R. The impact of sleep on adolescent depressed mood, alertness and academic performance. J. Adolesc. 36(6), 1025–1033 (2013).
Leger, D., Beck, F., Richard, J. B. & Godeau, E. Total sleep time severely drops during adolescence. PLoS One 7(10), e45204. https://doi.org/10.1371/journal.pone.0045204 (2012).
Hagenauer, M. H. & Lee, T. M. Adolescent sleep patterns in humans and laboratory animals. Horm. Behav. 64(2), 270–279 (2013).
Crowley, S., Wolfson, A., Tarokh, L. & Carskadon, M. An update on adolescent sleep: new evidence informing the perfect storm model. J. Adolesc. 67, 55–65 (2018).
Bauducco, S., Richardson, C. & Gradisar, M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 34, 77–83 (2020).
Ohayon, M. et al. National sleep foundation’s sleep quality recommendations: First report. Sleep Health 3(1), 6–19 (2017).
Hirshkowitz, M. et al. National sleep foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 1(1), 40–43 (2015).
Yip, T. The effects of ethnic/racial discrimination and sleep quality on depressive symptoms and self-esteem trajectories among diverse adolescents. J. Youth Adolesc. 44, 419–430 (2015).
Orchard, F., Gregory, A. M., Gradisar, M. & Reynolds, S. Self-reported sleep patterns and quality amongst adolescents: Cross-sectional and prospective associations with aniety and depression. J. Child. Psychol. Psychiat. 61, 1126–1137 (2020).
Stone, J. E. et al. In-person vs home schooling during the COVID-19 pandemic: Differences in sleep, circadian timing, and mood in early adolescence. J. Pineal Res. 71(2), e12757. https://doi.org/10.1111/jpi.12757 (2021).
Olive, L. S. et al. Child and parent physical activity, sleep, and screen time during COVID-19 and associations with mental health: Implications for future psycho-cardiological disease?. Front. Psychiatry 12, 774858. https://doi.org/10.3389/fpsyt.2021.774858 (2021).
Gardner, L. A. et al. Lifestyle risk behaviours among adolescents: A two-year longitudinal study of the impact of the COVID-19 pandemic. BMJ Open 12(6), e060309. https://doi.org/10.1136/bmjopen-2021-060309 (2022).
Li, Y. et al. How does the COVID-19 affect mental health and sleep among Chinese adolescents: A longitudinal follow-up study. Sleep Med. 85, 246–258 (2021).
Zhao, J., Xu, J., He, Y. & Xiang, M. Children and adolescents’ sleep patterns and their associations with mental health during the COVID-19 pandemic in Shanghai, China. J. Affect. Disorders 301, 337–344 (2022).
Bacaro, V. et al. The impact of COVID-19 on Italian adolescents’ sleep and its association with psychological factors. J. Sleep Res. 31(6), e13689 (2022).
Teesson, M. et al. Study protocol of the Health4Life initiative: A cluster randomised controlled trial of an eHealth school-based program targeting multiple lifestyle risk behaviours among young Australians. BMJ Open 10(7), e035662. https://doi.org/10.1136/bmjopen-2019-035662 (2020).
Drake, C. et al. The pediatric daytime sleepiness scale (PDSS): Sleep habits and school outcomes in middle-school children. Sleep 26(4), 455–458 (2003).
McLaughlin, K. A. & King, K. Developmental trajectories of anxiety and depression in early adolescence. J. Abnorm. Child Psychol. 43, 311–323 (2015).
Wang, D. et al. Longitudinal trajectories of depression and anxiety among adolescents during COVID-19 lockdown in China. J. Affect. Disord. 299, 628–635 (2022).
van Loon, A. W. et al. Trajectories of adolescent perceived stress and symptoms of depression and anxiety during the COVID-19 pandemic. Sci. Rep. 12(1), 15957. https://doi.org/10.1038/s41598-022-20344-y (2022).
Smout, S., Gardner, L. A., Newton, N. & Champion, K. E. Dose-response associations between modifiable lifestyle behaviours and anxiety, depression and psychological distress symptoms in early adolescence. Aust. N. Z. J. Public Health 47(1), 100010. https://doi.org/10.1016/j.anzjph.2022.100010 (2023).
Short, M.A., Booth, S.A., Omar, O., Ostlundh, L., Arora, T. (2020) The relationship between sleep duration and mood in adolescents: A systematic review and meta-analysis. Sleep medicine reviews. 52, 101311; https://doi.org/10.1016/j.smrv.2020.101311.
Meltzer, L.J., et al. COVID-19 instructional approaches (in-person, online, hybrid), school start times, and sleep in over 5,000 U.S. adolescents. Sleep. 44(12), zsab180; https://doi.org/10.1093/sleep/zsab180 (2021).
Vidal Bustamante, C. M. et al. Within-person fluctuations in stressful life events, sleep, and anxiety and depression symptoms during adolescence: a multiwave prospective study. J. Child. Psychol. Psychiat. 61(10), 1116–1125 (2020).
Palmer, C. A. & Alfano, C. A. Sleep and emotion regulation: an organizing, integrative review. Sleep Med. Rev. 31, 6–16 (2017).
Mousavi, Z. & Troxel, W. M. Later school start times as a public health intervention to promote sleep health in adolescents. Curr. Sleep Med. Rep. 9, 152–160 (2023).
Gee, B. et al. The effect of non-pharmacological sleep interventions on depression symptoms: A meta-analysis of randomised controlled trials. Sleep Med. Rev. 43, 118–128 (2019).
Staines, A. C., Broomfield, N., Pass, L., Orchard, F. & Bridges, J. Do non-pharmacological sleep interventions affect anxiety symptoms? A meta-analysis. J. Sleep Res. 31(1), e13451 (2022).
Wolfson, A. R. et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2, 213–216 (2003).
Short, M. A., Gradisar, M., Lack, L. C., Wright, H. R. & Chatburn, A. Estimating adolescent sleep patterns: Parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nat. Sci. Sleep 5, 23–26 (2013).
Rynders, C. A. et al. A naturalistic actigraphic assessment of changes in adolescent sleep, light exposure, and activity before and during COVID-19. J. Biol. Rhythms 37(6), 690–699 (2022).
Pham, T. T. L. et al. Definitions of culturally and linguistically diverse (CALD): A literature review of epidemiological research in Australia. Int. J. Environ. Res. Public Health 18(2), 737 (2021).
Torsheim, T. et al. Psychometric validation of the revised family affluence scale: A latent variable approach. Child Indic. Res. 9(3), 771–784 (2016).
Roenneberg, T., Pilz, L. K., Zerbini, G. & Winnebeck, E. C. Chronotype and social jetlag: A (self-) critical review. Biology 8(3), 54. https://doi.org/10.3390/biology8030054 (2019).
Gradisar, M. et al. A randomized controlled trial of cognitive-behavior therapy plus bright light therapy for adolescent delayed sleep phase disorder. Sleep 34(12), 1671–1680 (2011).
Irwin, D. et al. An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual. Life Res. 19(4), 595–607 (2010).
Johnson, J. G., Harris, E. S., Spitzer, R. L. & Williams, J. B. W. The patient health questionnaire for adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J. Adolesc. Health 30(3), 196–204 (2002).
Jung, T. & Wickrama, K. A. An introduction to latent class growth analysis and growth mixture modeling. Social and personality psychology compass. 2(1), 302–317 (2008).
Weller, B. E., Bowen, N. K. & Faubert, S. J. Latent class analysis: A guide to best practice. J. Black Psychol. 46(4), 287–311 (2020).
Asparouhov, T. & Muthén, B. Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes 21(2), 1–22 (2014).
Muthén, L.K., Muthén, B.O. Mplus User’s Guide. (Muthén & Muthén, 1998–2017).
Little, R. J. & Rubin, D. B. Statistical Analysis with Missing Data 2nd edn. (Wiley, 2002).
Acknowledgements
The Health4Life study was led by researchers at the Matilda Centre at the University of Sydney, Curtin University, the University of Queensland, the University of Newcastle, Northwestern University, and UNSW Sydney: Teesson, M., Newton, N.C, Kay-Lambkin, F.J., Champion, K.E., Chapman, C., Thornton, L.K., Slade, T., Mills, K.L., Sunderland, M., Bauer, J.D., Parmenter, B.J., Spring, B., Lubans, D.R., Allsop, S.J., Hides, L., McBride, N.T., Barrett, E.L., Stapinski, L.A., Mewton, L., Birrell, L.E., & Quinn, C & Gardner, L.A.
Funding
Open access funding provided by Örebro University. The Health4Life study was funded by the Paul Ramsay Foundation and the Australian National Health and Medical Research Council via Fellowships (KC, APP1120641; MT, APP1078407; and NN, APP1166377) and via a Centre of Research Excellence in the Prevention and Early Intervention in Mental Illness and Substance Use (PREMISE; APP11349009). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to acknowledge all the research staff who have worked across the study, as well as the schools, students and teachers who participated in this research. The research team also acknowledges the assistance of the New South Wales Department of Education (SERAP 2019006), the Catholic Education Diocese of Bathurst, the Catholic Schools Office Diocese of Maitland-Newcastle, Edmund Rice Education Australia, the Brisbane Catholic Education Committee (373), and Catholic Education Western Australia (RP2019/07) for access to their schools to conduct this research.
Author information
Authors and Affiliations
Contributions
L.A.G., K.E.C., M.G., and S.B. conceived the idea behind the study. S.B. analysed the data. K.E.C., L.A.G., N.C.N. and M.T. acquired the fundings and coordinated data collection. All authors contributed to the interpretation of the results, writing, and reviewing the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Gradisar reports that he is the CEO of WINK Sleep Pty Ltd which provides professional training for the treatment of sleep disorders, and is employed by Sleep Cycle AB, a listed company whose app tracks sleep.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bauducco, S., Gardner, L.A., Smout, S. et al. Adolescents’ trajectories of depression and anxiety symptoms prior to and during the COVID-19 pandemic and their association with healthy sleep patterns. Sci Rep 14, 10764 (2024). https://doi.org/10.1038/s41598-024-60974-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60974-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.