Abstract
To investigate the associations between corneal curvature (CC) and other anterior segment biometrics in young myopic adults. In this retrospective multi-center study, 7893 young myopic adults were included. CC and other anterior segment biometrics were measured by Scheimpflug imaging (Pentacam). CC was defined as SimK at central 3 mm area, and other anterior segment biometrics included white-to-white corneal diameter (WTW), central corneal thickness (CCT), corneal volume (CV) at 3 mm, 5 mm, and 7 mm area, anterior corneal astigmatism (ACA), posterior corneal astigmatism (PCA), anterior corneal eccentricity (ACE) and asphericity (ACAP), posterior corneal eccentricity (PCE) and asphericity (PCAP), anterior chamber depth (ACD), and anterior chamber volume (ACV). Univariate regression analyses were used to assess the associations between CC and other anterior segment biometrics, and multivariate regression analyses were further performed to adjusted for age, gender and spherical equivalent. CC was higher in patients of female gender and higher myopia (all P < 0.05). Eyes in higher CC quartiles had lower WTW, thinner CCT, lower CV at 3 mm and 5 mm, lower ACD, and lower ACV (all P < 0.001), but had larger ACA, larger PCA, less PCE and less PCAP (all P < 0.001), compared to eyes in lower CC quartiles. The trends of CV at 7 mm, ACE and ACAP were inconsistent in different CC quartiles. After adjusting for age, gender and spherical equivalent with multivariate linear regression, CC was positively correlated to CV at 7 mm (βs = 0.069), ACA (βs = 0.194), PCA (βs = 0.187), ACE (βs = 0.072), PCAP (βs = 0.087), and ACD (βs = 0.027) (all P < 0.05), but was negatively correlated to WTW (βs = − 0.432), CCT (βs = − 0.087), CV-3 mm (βs = − 0.066), ACAP (βs = − 0.043), PCE (βs = − 0.062), and ACV (βs = − 0.188) (all P < 0.05). CC was associated with most of the other anterior segment biometrics in young myopic adults. These associations are important for better understanding of the interactions between different anterior segment structures in young myopic patients, and are also useful for the exploration of the pathogenesis of myopia.
Similar content being viewed by others
Introduction
Myopia is a common ocular health issue with an estimated global prevalence of 28.3%, especially affecting children and young adults in east and south-east Asian countries1,2. During the development of myopia, ocular biometrics are believed to play crucial roles3,4. Although the key mechanism of myopia mainly involves elongation of the eyeball and vitreous cavity5, changes of anterior segment structures are also suggested to play roles in myopia6,7. Moreover, different ocular biometrics are often inter-correlated in myopia, suggesting interplay of different ocular structures in myopia development8,9.
The cornea is the foremost refractive tissue of the eye. It provides about two third of the refractive power of the eye. Corneal refractive power can be measured as corneal curvature (CC) which is commonly shown as simulated keratometry (SimK). In general and aged populations, it was shown that corneal refractive power was correlated to axial length (AL)10,11 and some of the anterior segment biometrics, such as central corneal thickness (CCT) and anterior chamber depth (ACD)10.
In patients with myopia, CC was also correlated to AL12,13. However, the correlations of CC and other anterior segment biometrics in myopia were rarely reported14. In the present study with data from multiple centers, we have found correlations between CC and other anterior segment biometrics in young myopic adults. The findings may reveal the relationships of CC and other anterior segment biometrics in myopia.
Methods
Participants
The participants were described in previous studies8,15,16, which were approved by the Institutional Review Board (IRB) of Guangzhou Aier Eye Hospital (GZ), Shenyang Aier Eye Hospital (SY), Wuhan Aier Eye Hospital (WH), Chengdu Aier Eye Hospital (CD) and Hankou Aier Eye Hospital (HK). The study were conducted according to the tenets of the Declaration of Helsinki, without the needs for informed consent, because no participants could be identified from the data8,15,16. We included right eye data of young myopic adults aged 18–40 and with a spherical equivalent (SE) ≤ -0.50 diopter (D) and good quality Pentacam scans. Patients were excluded if they had coexisting corneal diseases, such as keratoconus (a significantly asymmetrical bowtie on the curvature map, a posterior elevation value of ≥ + 15 at the thinnest point with red spot on Belin/Ambrosio Enhanced Ectasia Display)8,17 and forme fruste keratoconus (such as the follow eye of patients with unilateral keratoconus)8,18, previous ocular surgery or trauma, severe dry eye, uveitis, glaucoma, wearing soft contact lenses within 2 weeks or rigid gas-permeable lenses within 1 month before examination8,15,16.
Examinations
All patients underwent a set of ocular examinations, including best-corrected visual acuity (BCVA), intraocular pressure (IOP), manifest and cycloplegic refraction, slit-lamp examination of the anterior segment, corneal topography, and Pentacam measurements8,15,16. Myopia was divided into three groups according to the SE: low myopia (− 3.00 D < SE ≤ − 0.50 D), moderate myopia (− 6.00 D < SE ≤ − 3.00 D) and high myopia (SE ≤ − 6.00 D).
Pentacam (Oculus GmbH, Wetzlar, Germany) was used to obtain CC (SimK at central 3 mm area) and other anterior segment biometrics, including white-to-white corneal diameter (WTW), CCT, corneal volume (CV) at 3 mm, 5 mm, and 7 mm area, anterior corneal astigmatism (ACA), posterior corneal astigmatism (PCA), anterior corneal eccentricity (ACE) and asphericity (ACAP), posterior corneal eccentricity (PCE) and asphericity (PCAP), anterior chamber depth (ACD), and anterior chamber volume (ACV). All of the CC and anterior segment parameters were recorded before mydriasis.
Statistical analysis
Normal distributions of the data were tested by Kolmogorov–Smirnov (KS) test. Basic characteristics of different CC quartiles, CC in different age and myopia groups, and other anterior segment biometrics in different CC quartiles were compared by Kruskal–Wallis test. Multivariate linear regression with the standardized regression coefficients (βs) were used to test the correlations of CC and other ocular biometrics adjusted for age, gender and SE. P < 0.05 was considered to be statistically significant.
Ethics statement
This study was conformed to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Guangzhou Aier Eye Hospital (GZ), Shenyang Aier Eye Hospital (SY), Wuhan Aier Eye Hospital (WH), Chengdu Aier Eye Hospital (CD) and Hankou Aier Eye Hospital (HK). This study was only a review of medical records from which patients could not be identified, so the IRBs decided to waive the requirement to get informed consent.
Results
Basic characteristics
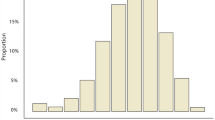
CC of the participants was normally distributed (Fig. 1). Age, sex, spherical error, astigmatism, and SE in different CC quartiles were significantly different (Table 1). Older age and more females were observed in higher CC quartiles (P < 0.001). More spherical error, astigmatism, and SE were also present in higher CC quartiles (P < 0.001).
CC in different sex, age and myopia groups
CC was significantly different in different age, sex and myopia groups (Tables 2 and 3). CC was higher in females than in males in every age group and myopia group (P < 0.001). In every age group and sex group, CC was higher in eyes with high myopia, compared to those with mild or moderate myopia (P < 0.05).
Other anterior segment biometrics in different CC quartiles
Other anterior segment biometrics were statistically different in eyes of different CC quartiles (Table 4 and Fig. 2). Eyes in higher CC quartile had smaller WTW, thinner CCT, smaller CV-3 mm and CV-5 mm, higher ACA and PCA, lower PCE, higher PCAP, smaller ACD and ACV (P < 0.001). Although there were significant differences in CV-7 mm and ACE in different CC quartiles (P < 0.05), the trends were inconsistent.
Multiple comparisons of Other anterior segment biometrics in different CC quartiles. Multiple comparisons were conducted using the Dunn-Bonferroni test. Using letters (e.g. a, ab, b) to represent different levels of significance among groups. The meaning of these letters is as follows: If two groups share the same letter (e.g. a and a), there is no significant difference between them. If two groups have different letters (e.g. a and b), there is a significant difference between them. If two groups share the same letter, but there are other groups with different letters (e.g. ab and a), it means that groups with the same letter do not have significant differences between them, however, there are significant differences between them and groups with different letters. CC corneal curvature, SD standard deviation, WTW white-to-white corneal diameter, CCT central corneal thickness, CV corneal volume, ACA anterior corneal astigmatism, PCA posterior corneal astigmatism, ACE anterior corneal eccentricity, ACAP anterior corneal asphericity, PCE posterior corneal eccentricity, PCAP posterior corneal asphericity, ACD anterior chamber depth, ACV anterior chamber volume.
Correlations of CC and other anterior segment biometrics
In univariate linear regression analyses, CC was significantly correlated to all of the other anterior segment biometrics (all P < 0.001). In multivariate linear regression analyses adjusting for age, gender and SE, CC was positively correlated to CV-7 mm (βs = 0.069), ACA (βs = 0.194), PCA (βs = 0.187), ACE (βs = 0.072), PCAP (βs = 0.087), and ACD (βs = 0.027) (all P < 0.05), but was negatively correlated to WTW (βs = − 0.432), CCT (βs = − 0.087), CV-3 mm (βs = − 0.066), ACAP (βs = − 0.043), PCE (βs = − 0.062), and ACV (βs = − 0.188) (all P < 0.05) (Table 5).
Discussion
Using data from multiple centers, we revealed the correlations of CC and other anterior segment biometrics in young myopic adults. The findings are useful for better understanding of the interactions of anterior segment structures in myopia.
CC was higher in females than in males in the present study. This is consistent with many other previous studies6,10,13. In a population-based study, both the horizontal and vertical corneal refractive power was higher in women than in men10. In a study with healthy young university students (mean SE − 4.1 ± 2.7 D), although there was no sex difference in refractive errors, female participants had higher CC than male participants6. In highly myopic patients with the mean age of 31.2 ± 16.5 years, females were also shown to have higher CC than males13. In the present study, CC was higher in female participants than in male participants across all myopia groups, suggesting sex difference in corneal characteristics of myopia patients. One of the reasons for higher CC in females may be due to shorter axial length (AL) in women than men, and more corneal refractive power is needed to converge the light in female eyes6,19. Another reason is that higher CC in females is required for better emmetropization to prevent further myopic shift due to AL elongation20.
The correlations of CC and other anterior segment biometrics were also demonstrated in the present study. CC was negatively correlated to WTW after adjusting for age, sex and SE. This was consistent with previous studies conducted in 4–18 years old children21 and cataract patients22. A possible explanation of the negative correlation of CC and WTW is that CC is lower in taller subjects21,23, who have been shown to have larger WTW24. Another mechanism is that CC is decreased with AL elongation10,13, but the WTW is increased with longer AL25. We also demonstrated a negative correlation of CC and CCT, and similar results were also reported in previous studies with young subjects12,26. However, the correlation of CC and CCT may be positive in the elderly27,28. CC was also negatively correlated to CV-3 mm in the present study, but CC was not correlated to CV-5 mm, and was positively correlated to CV-7 mm, suggesting that the correlation of CC and CV may differ according to the area of interest.
CC was shown to be positively correlated to ACA and PCA. Only few studies have reported the correlation of CC and astigmatism. In the Shandong Children Eye Study, lower corneal refractive power was correlated to smaller cylindrical refractive error21. In another study with university students, lower corneal astigmatism was also observed in participants with lower corneal refractive power29. However, none of the previous studies has evaluated the correlation of CC and PCA. Our study showed that CC was correlated not only to ACA, but also to PCA, suggesting changes of corneal refractive power may affect both the anterior and posterior corneal toricity in myopia, and such changes are more prominent in some meridians.
CC was correlated to anterior and posterior corneal eccentricity and asphericity, including ACE, ACAP, PCE, and PCAP. Similar correlations were observed in a study with subjects from 6 to 83 years old and another study with the elderly30,31. According to these findings, when the cornea is steeper, it is also more prolate and eccentrical on the anterior surface but less prolate and eccentrical on posterior surface. It would be meaningful to investigate whether a steeper cornea is associated with more postoperative corneal eccentricity and asphericity, which are important parameters of visual quality after refractive surgery.
For biometrics of the anterior chamber, CC was positively correlated to ACD but negatively correlated to ACV. Since in the present study the CC reflected the steepness of the central 3 mm cornea, and the ACD showed the depth of the central anterior chamber, it was expected that a steeper central cornea was associated with a deeper central anterior chamber. Similar findings were also reported in a general population10. However, negative correlation of CC and ACD may be present in subjects of older age (40–80 years)32. Higher CC is also correlated to smaller WTW10,21,29, and smaller WTW is correlated to smaller ACV33. This may explain the negative correlation of CC and ACV in myopic patients. It is noteworthy that in patients with shallow anterior chambers, the correlation of CC and ACV may not exist34.
It is well known that CC is correlated to many other ocular biometrics in normal subjects. We revealed that CC is also correlated to other anterior segment biometrics in myopic adults. The correlations help us better understand the interactions of different anterior segment structures in the development of myopia. In myopic eyes, when the CC is steeper, WTW is smaller, CCT is thinner, corneal toricity, anterior corneal eccentricity and asphericity are higher, ACD is deeper, and ACV is smaller. The changes of these anterior segment structures may affect the development of myopia, or may be the consequences of AL elongation. Further studies are required to clarify the roles of these biometrics in myopia.
In conclusions, CC was correlated to most of the other anterior segment biometrics in young myopic adults, suggesting the interactions of different anterior segment structures in myopia. The sequential order of the changes of these structures in the development of myopia need to be further investigated.
Data availability
Data are available from the corresponding author upon reasonable request.
References
Baird, P. N. et al. Myopia. Nat. Rev. Dis. Primers 6(1), 99 (2020).
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016).
Tao, Z. et al. A longitudinal study of the effect of ocular biometrics measures on myopia onset. Graefes Arch. Clin. Exp. Ophthalmol. 259(4), 999–1008 (2021).
Zhao, E. et al. Ocular biometrics and uncorrected visual acuity for detecting myopia in Chinese school students. Sci. Rep. 12(1), 18644 (2022).
Lee, S. S. et al. Incidence and progression of myopia in early adulthood. JAMA Ophthalmol. 140(2), 162–169 (2022).
Kato, K., Kondo, M., Takeuchi, M. & Hirano, K. Refractive error and biometrics of anterior segment of eyes of healthy young university students in Japan. Sci. Rep. 9(1), 15337 (2019).
Richter, G. M. et al. Ocular determinants of refractive error and its age- and sex-related variations in the Chinese American Eye Study. JAMA Ophthalmol. 135(7), 724–732 (2017).
Tang, C. et al. A multicenter study of the distribution pattern of posterior-to-anterior corneal curvature radii ratio in Chinese myopic patients. Front. Med. (Lausanne) 8, 724674 (2021).
Li, M., Luo, Z., Yan, X. & Chen, Z. The anterior segment biometrics in high myopia eyes. Ophthalmic Res. 66, 75–85 (2022).
Jonas, J. B., Nangia, V., Sinha, A. & Gupta, R. Corneal refractive power and its associations with ocular and general parameters: The Central India Eye and Medical Study. Ophthalmology 118(9), 1805–1811 (2011).
Han, S. U. et al. Analysis of keratometric measurements in accordance with axial length in an aged population. Sci. Rep. 12(1), 4087 (2022).
Wang, Q., Liu, W., Wu, Y., Ma, Y. & Zhao, G. Central corneal thickness and its relationship to ocular parameters in young adult myopic eyes. Clin. Exp. Optom. 100(3), 250–254 (2017).
Jin, G. et al. Corneal biometric features and their association with axial length in high myopia. Am. J. Ophthalmol. 238, 45–51 (2022).
Wang, Y. et al. Corneal and lenticular biometry in Chinese children with myopia. Clin. Exp. Optom. 106, 1–9 (2022).
Tang, C. et al. The distribution pattern of ocular residual astigmatism in Chinese myopic patients. Front. Med. 9, 763833 (2022).
Xu, G. et al. Distribution of white-to-white corneal diameter and anterior chamber depth in Chinese myopic patients. Front. Med. 8, 732719 (2021).
Mas Tur, V., MacGregor, C., Jayaswal, R., O’Brart, D. & Maycock, N. A review of keratoconus: Diagnosis, pathophysiology, and genetics. Surv. Ophthalmol. 62(6), 770–783 (2017).
Henriquez, M. A., Hadid, M. & Izquierdo, L. Jr. A systematic review of subclinical keratoconus and forme fruste keratoconus. J. Refract. Surg. 36(4), 270–279 (2020).
Zocher, M. T. et al. Biometry and visual function of a healthy cohort in Leipzig, Germany. BMC Ophthalmol. 16, 79 (2016).
Park, S. H., Park, K. H., Kim, J. M. & Choi, C. Y. Relation between axial length and ocular parameters. Ophthalmologica 224(3), 188–193 (2010).
Zhang, Y. Y. et al. Corneal curvature radius and associated factors in Chinese children: The Shandong Children Eye Study. PLoS One 10(2), e0117481 (2015).
Wei, L. et al. Evaluation of the white-to-white distance in 39,986 Chinese cataractous eyes. Investig. Ophthalmol. Vis. Sci. 62(1), 7 (2021).
Logan, N. S., Shah, P., Rudnicka, A. R., Gilmartin, B. & Owen, C. G. Childhood ethnic differences in ametropia and ocular biometry: The Aston Eye Study. Ophthalmic Physiol. Opt. 31(5), 550–558 (2011).
Hashemi, H. et al. White-to-white corneal diameter in the Tehran Eye Study. Cornea 29(1), 9–12 (2010).
Jiang, W. J. et al. Corneal diameter and associated parameters in Chinese children: The Shandong Children Eye Study. Clin. Exp. Ophthalmol. 45(2), 112–119 (2017).
Pan, C. W. et al. Central corneal thickness and its association with birth parameters in chinese adolescents. Ophthalmic Epidemiol. 26(5), 360–366 (2019).
Wang, D. et al. Central corneal thickness and related factors in an elderly American Chinese population. Clin. Exp. Ophthalmol. 39(5), 412–420 (2011).
Hashemi, H. et al. Central corneal thickness and its determinants in a geriatric population: A population-based study. Eye (Lond.) 37(3), 427–433 (2023).
Nieto-Bona, A., Lorente-Velázquez, A. & Mòntes-Micó, R. Relationship between anterior corneal asphericity and refractive variables. Graefes Arch. Clin. Exp. Ophthalmol. 247(6), 815–820 (2009).
Zhang, Z. et al. Corneal asphericity and its related factors in 1052 Chinese subjects. Optom. Vis. Sci. 88(10), 1232–1239 (2011).
Hashemi, H. et al. Corneal asphericity and related factors in the geriatric population: A population-based study. Ophthalmic Physiol. Opt. 41(4), 691–701 (2021).
Chen, M. J. et al. Relationship between central corneal thickness, refractive error, corneal curvature, anterior chamber depth and axial length. J. Chin. Med. Assoc. 72(3), 133–137 (2009).
Hashemi, H. et al. Anterior chamber angle and anterior chamber volume in a 40- to 64-year-old population. Eye Contact Lens. 42(4), 244–249 (2016).
Yang, F. & Bao, Y. Correlations of corneal curvature with corneal spherical aberration and anterior chamber parameters in eyes with shallow anterior chambers. Ophthalmol. Ther. 12(1), 239–249 (2023).
Funding
This study was funded by the NSFC Incubation Project of Guangdong Provincial People's Hospital (KY0120220807), the Science Research Foundation of Aier Eye Hospital Group (AF2009D4), by the Scientific Research Foundation of Health Commission of Hubei Province, China (WJ2021M035), the Medical Scientific Research Foundation of Health Commission of Wuhan City, China (WX21D11), the 8th Batch of Young and Middle-aged Medical Backbone Talents of Wuhan City, China, and the Research Fund Project of Clinical Research Institute of Aier Eye Hospital Group (AR2009D5, AR2209D2, AR2210D3).
Author information
Authors and Affiliations
Contributions
L.J. and Y.H. designed the study and wrote the manuscript. L.J., Z.D. and W.S. organized and analyzed the data and commented on the manuscript. S.Z., L.X., X.F., J.Z., Q.Z. and X.L. provided the data and commented on the manuscript. Q.Z., Z.W. and Y.H. supervised the study and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, L., Du, Z., Sun, W. et al. Associations between corneal curvature and other anterior segment biometrics in young myopic adults. Sci Rep 14, 8305 (2024). https://doi.org/10.1038/s41598-024-59037-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59037-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.