Abstract
Esophagogastric variceal bleeding (EVB) is one of the common digestive system emergencies with poor prognosis and high rate of rebleeding after treatment. To explore the effects of endoscopic therapy and drug therapy on the prognosis and rebleeding of patients with EVB, and then select better treatment methods to effectively improve the prognosis. From January 2013 to December 2022, 965 patients with EVB who were hospitalized in gastroenterology Department of the 940 Hospital of Joint Logistic Support Forces of PLA were retrospectively analyzed. Patients were divided into endoscopic treatment group (ET, n = 586) and drug treatment group (DT, n = 379). Propensity score matching (PSM) analysis was performed in both groups, and the general information, efficacy and length of hospital stay were recorded. The patients were followed up for 3 months after bleeding control to determine whether rebleeding occurred. There were 286 cases in each group after PSM. Compared with DT group, ET had higher treatment success rate (P < 0.001), lower rebleeding rate (P < 0.001), lower mortality rate within 3 months, and no significant difference in total hospital stay (P > 0.05). Compared with drug therapy, endoscopic treatment of EVB has short-term efficacy advantages, and can effectively reduce the incidence of rebleeding and mortality within 3 months.
Similar content being viewed by others
Introduction
Esophagogastric variceal bleeding (EVB) is one of the common digestive system emergencies with poor prognosis and a high rate of rebleeding after treatment1. Studies have shown that for untreated patients with EVB, the rate of rebleeding within 1–2 years is as high as 60%, and the 6-week fatality rate is as high as 20%2,3.Therefore, active and effective treatment is very important for reducing EVB rebleeding and mortality. Clinically, for patients highly suspected of EVB, early application of portal pressure reduction and antibacterial drugs is the primary treatment plan, while gastroscopy is still the main method for definite diagnosis of EVB4. So far, systematic reviews and meta-analyses have failed to reach consistent conclusions on the efficacy comparison of the above two treatments3,5. Therefore, how to optimize the above treatment methods, still need to carry out related clinical research.
Based on this, this study compared the effects of endoscopic therapy and drug therapy on the prognosis and rebleeding of patients with EVB, hoping to provide certain theoretical basis for clinicians to choose better treatment plans for patients with EVB.
Methods
Clinical information
A total of 965 patients with EVB admitted to the Gastroenterology Department of the 940 Hospital of Joint Logistic Support Forces of PLA from January 2013 to December 2022 were selected to collect their detailed clinical data. Baseline information included patient gender, age, smoking history, drinking history, underlying disease, Child–Pugh grade, primary disease, and treatment. Outcome, length of hospital stay, rate of early rebleeding, rate of delayed rebleeding, and mortality within 3 months after treatment were included. Patients were divided into endoscopic treatment group (ET) and drug treatment group (DT) according to the main treatment modalities.
Inclusion criteria: (i) 18–80 years; (ii) Meet the relevant diagnostic criteria for EVB: Under endoscopy, active varicose vein bleeding (oozing or spraying), thrombocephalic head, or varicose veins were present without any other lesions that could explain the bleeding.
Exclusion criteria: (i) those who do not meet the above diagnostic criteria; (ii) Patients with haemorrhagic diseases of the hematopoietic system or serious diseases of the heart, brain, kidney and other important organs; (iii) Patients with incomplete clinical data or no follow-up within 3 months after treatment; (iv) Patients receiving medication combined with endoscopic therapy.
This study was approved by the 940 Hospital of Joint Logistic Support Forces of PLA (approval number: 2023KYLL160) before its formal implementation. All participants in the study and/or their legal guardians were informed and consented to our study. The research programme complies with the ethical guidelines of the Declaration of Helsinki.
Treatment methods
ET group
Endoscopic treatment included endoscopic variceal ligation (EVL), endoscopic injection sclerotherapy (EIS) and endoscopic tissue adhesive injection.
EVL
Mainly used for GOV1 EVB patients, six or seven ring ligation device is commonly used, and the first ligation interval of 2 to 4 weeks can be repeated ligation or sclerosing agent injection and other sequential treatment until the varicose veins disappear or basically disappear.
EIS
Mainly in patients who are not suitable for EVL treatment, EIS or EVL can be repeated at an interval of 2 to 4 weeks after the first EIS until the varicose veins disappear or basically disappear. The commonly used hardener is lauryl alcohol (10 ml vs. 100 mg).
Endoscopic tissue adhesive injection
Mainly used for patients with GOV2 hemorrhage. The commonly used tissue adhesive is n-butyl cyocyanacrylate, and the sandwich Sandwich method is used for intravenous injection. Generally, one injection can completely block varicose veins.
DT group
The main drugs used for treatment are portal pressure lowering drugs, antibacterial drugs, proton pump inhibitors (PPIs) and other symptomatic treatment drugs.
Portal pressure lowering drug
Teripressin, the dose selected 2 ~ 12 mg/d; Somatostatin, 250 ~ 500 μg/h; Octreotide, dosage selected 25 ~ 50 μg/h. The above drugs were administered by continuous intravenous infusion, with a general course of 3 to 5 days.
Antimicrobials
All patients were given a broad spectrum of antimicrobials intravenously, and if there was evidence of infection, the grade of antimicrobials would be increased according to the corresponding laboratory results, and/or the course of treatment would be extended appropriately.
PPIs: Generally choose omeprazole, Rabeprazole and other drugs, usually 40 to 80 mg/d intravenous injection or 8 mg/h continuous intravenous infusion, the general course of 5 to 7 days.
Other drugs
According to the clinical manifestations of patients, hemostatic drugs such as intravenous hemocoagulase and vitamin K1 are selected. Apply for transfusion of blood and/or blood products if the patient has indications for transfusion. After active bleeding was controlled for 24 h, lactulose was administered orally or by enema, and anemia correction drugs were given if necessary.
Evaluation of curative effect and rebleeding
Evaluation of treatment failure6
One of the following manifestations: (i) Vomiting of fresh blood or more than 100 ml of fresh blood drawn by nasogastric tube ≥ 2 h after endoscopic therapy or drug therapy; (ii) Hemorrhagic shock occurs; (iii) Without transfusion, hemoglobin decreased by 30 g/L (hematocrit decreased by about 9%) during any 24 h period.
Signs of rebleeding6
Clinically significant active bleeding events after bleeding control (hematemesis, black stool, or blood in the stool; Systolic blood pressure decreased > 20 mmHg or heart rate increased > 20 beats/min; Hemoglobin decreased > 30 g/L in the absence of transfusion). (i) Early rebleeding: EVB appears within 120 h to 6 weeks after blood control; (ii) Delayed rebleeding: EVB occurs after 6 weeks of bleeding control; Non-EVB patients were not included.
Statistical analysis
The 1:1 PSM analysis was performed using SPSS25.0 software (SPSS Inc.), and the caliper value was set to 0.02. Matching factors included sex, age, smoking history, drinking history, underlying disease, and Child–Pugh rating. Continuous variables were expressed as mean ± SD (\(\overline{x }\) ± s), and two independent sample T-tests were used for comparison between groups. The categorical variables were expressed as frequency and percentage (%), and the Chi-square test or Fisher test was used for comparison between groups. P < 0.05 was considered statistically significant.
Results
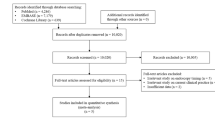
Propensity score matching
There were significant differences in smoking and drinking history before PSM between the two groups. PSM included gender, age, smoking history, drinking history, underlying diseases, Child–Pugh grade and other factors, and 286 cases in the ET group and 286 cases in the DT group were successfully matched 1:1, with no statistically significant differences in confounding variables (see Table 1).
Prognosis comparison
The clinical data of the two groups of patients after PSM are shown in Table 2. The short-term treatment success rate of ET was significantly better than that of DT (94.77% vs. 47.39, P< 0.001). Compared with the DT group, the rebleeding rate in ET was 26.83% vs. 44.60%, P < 0.001; Early bleeding rate: 1.4% vs. 14.69%, P < 0.001; The rate of delayed rebleeding was 21.68% vs. 31.82%, P = 0.006) and the rate of death within 3 months after treatment was lower (3.15% vs. 11.89%, P< 0.001). There was no significant difference in the mean length of stay between the two groups (11.45 ± 2.29 vs. 11.48 ± 2.30, P = 0.756), as shown in Table 2.
Discussion
At present, the treatment principles for EVB are mainly to correct hypovolemic shock while effectively controlling bleeding and preventing bleeding related complications7. Some studies have reported that TIPS ranked first in the prevention of EVB secondary prevention of rebleeding, and carvedilol has shown outstanding efficacy in improving survival, but EVL + NSBB does not seem to be ideal for preventing rebleeding and extending survival in patients with EVB8. As a common method for the treatment of esophageal and gastric variceal hemorrhage recommended by several relevant guidelines and consensus, both endoscopic therapy and drug therapy have certain curative effects9,10,11,12,13. However, for the comparison of the efficacy of endoscopic therapy or drug therapy alone, the current reports have not reached a consistent conclusion. The short-term treatment effect evaluation, whether rebleeding will occur after treatment and the probability of death after treatment can reflect the efficacy to some extent.
In this study, we used PSM to compare the effects of endoscopic therapy and drug therapy on prognosis and rebleeding in patients with EVB. We found that the success rate of short-term hemostasis in the ET group was significantly better than that in the DT group, indicating that ET have certain advantages in short-term efficacy, which can reduce the occurrence of hemorrhagic shock. Our present study shows that ET can effectively reduce the rate of rebleeding and mortality within 3 months after treatment, suggesting that ET are superior in improving overall prognosis and delaying patient survival. However, there was no significant difference in length of stay between the two groups (P = 0.756).
Previous research reports have confirmed the effectiveness of EVL in the treatment of esophageal varices, but there does not seem to be much reporting on the comparison of the efficacy of EVB with the three different endoscopic treatments mentioned in our research14. Therefore, we further analyzed the influence of different endoscopic treatment methods on the clinical prognosis of EVB patients. The results showed that EVL seemed to be superior to the other two methods in reducing rebleeding in patients with EVB, but there was no significant difference between them in short-term hemostatic effect, length of hospital stay, and whether death occurred (see Supplementary Table 1), which was similar to the results of previous studies15,16.
There are some limitations and shortcomings in this study: First, due to the single-center data source of the included study, the sample size and clinical data of the final included study are relatively limited for retrospective study, and the results may be biased; Second, although endoscopic treatment of EVB has short-term efficacy advantages and can effectively reduce the incidence of rebleeding and mortality within 3 months, due to the short follow-up time of the two groups of patients, further studies are needed to determine whether this difference will affect patients' long-term survival or other clinical indicators (As our long-term follow-up is still ongoing, data are not yet available).
Conclusions
In summary, successful hemostasis and reducing the occurrence of rebleeding are the key to effective treatment of EVB. According to our data, ET have a significant advantage over DT in successful hemostasis in the short term, and the probability of rebleeding events (whether early or delayed rebleeding) in ET seems to be much lower than that of DT. In addition, compared with the DT group, patients in the ET group had a lower mortality rate within 3 months after treatment. Therefore, for the patients with EVB, endoscopic treatment should be given in the case of excluding related contraindications to reduce the occurrence of rebleeding and improve the prognosis. However, more clinical studies with more data are needed to confirm which endoscopic therapy is more effective in alleviating or curing EVB.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due the raw data of this study contains the identity information of the subjects, which may involve their privacy, and the case browsing system of the hospital is not open to the public, but are available from the corresponding author on reasonable request.
References
Wu, K. et al. Analysis of the timing of endoscopic treatment for esophagogastric variceal bleeding in cirrhosis. Front. Med. (Lausanne) 9, 1036491. https://doi.org/10.3389/fmed.2022.1036491 (2022).
Magaz, M., Baiges, A. & Hernández-Gea, V. Precision medicine in variceal bleeding: Are we there yet?. J. Hepatol. 72(4), 774–784. https://doi.org/10.1016/j.jhep.2020.01.008 (2020).
Jiyao, S. et al. The progress in management of esophagogastric variceal bleeding in cirrhotic portal hypertension. Chin. J. Surg. 58(10), 808–812. https://doi.org/10.3760/cma.j.cn112139-20191111-00556 (2020).
Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Gastroendoscopy. Liver cirrhosis portal hypertension with esophageal gastric varices bleeding prevention guide. Chin. J. Liver Dis. 30(10), 1029–1043. https://doi.org/10.3760/cma.J.cn501113-20220824-00436 (2022).
Plaz Torres, M. C. et al. Secondary prevention of variceal bleeding in adults with previous oesophageal variceal bleeding due to decompensated liver cirrhosis: A network meta-analysis. Cochrane Database Syst. Rev. 3(3), CD013122. https://doi.org/10.1002/14651858.CD013122.pub2 (2021).
Chinese Society of Hepatology, Chinese Society of Gastroenterology, Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines on the management of esophagogastric variceal bleeding in cirrhotic portal hypertension. Chin. J. Intern. Med. 62(01), 7–22. https://doi.org/10.3760/cma.j.cn501113-20220824-00436 (2023).
Roberts, D. et al. Treatment for bleeding oesophageal varices in people with decompensated liver cirrhosis: A network meta-analysis. Cochrane Database Syst. Rev. 4(4), CD013155. https://doi.org/10.1002/14651858.CD013155.pub2 (2021).
Miao, Z. et al. Comparison of therapies for secondary prophylaxis of esophageal variceal bleeding in cirrhosis: A network meta-analysis of randomized controlled trials. Clin. Ther. 42(7), 1246-1275.e3. https://doi.org/10.1016/j.clinthera.2020.04.014 (2020).
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69(2):406–460. doi: https://doi.org/10.1016/j.jhep.2018.03.024. Epub 2018 Apr 10. Erratum in: J Hepatol. 2018;69(5):1207.
Biggins, S. W. et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 74(2), 1014–1048. https://doi.org/10.1002/hep.31884 (2021).
Aithal, G. P. et al. Guidelines on the management of ascites in cirrhosis. Gut 70(1), 9–29. https://doi.org/10.1136/gutjnl-2020-321790 (2021).
Tripathi, D. et al. Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut 64(11), 1680–704. https://doi.org/10.1136/gutjnl-2015-309262 (2015).
De Franchis, R. et al. Baveno VII Faculty. Baveno VII—Renewing consensus in portal hypertension. J. Hepatol. 76(4), 959–974. https://doi.org/10.1016/j.jhep.2021.12.022 (2022).
Zheng, J. et al. The endoscopic ultrasound probe findings in prediction of esophageal variceal recurrence after endoscopic variceal eradication therapies in cirrhotic patients: A cohort prospective study. BMC Gastroenterol. 19(1), 32. https://doi.org/10.1186/s12876-019-0943-y (2019).
Huang, Y. et al. Treatment strategies in emergency endoscopy for acute esophageal variceal bleeding (CHESS1905): A nationwide cohort study. Front. Med. (Lausanne) 9, 872881. https://doi.org/10.3389/fmed.2022.872881 (2022).
Dai, C. et al. Endoscopic variceal ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: A meta-analysis. World J. Gastroenterol. 21(8), 2534–2541. https://doi.org/10.3748/wjg.v21.i8.2534 (2015).
Funding
This research was supported by the "The Top talent" lifting project of the Chinese People's Liberation Army Joint Logistic Support Force.
Author information
Authors and Affiliations
Contributions
Jiu-cong Zhang and Xiao-feng Zheng designed the study. Jing-jing Jiang, Chun Gao and Jun-feng Mao wrote and revised the original manuscript. Guo-yuan Yang and Jun Huang made figures and tables, Xiao-hui Yu and Yong Tan collected the data and analyzed it. Jiu-Cong Zhang and Jing-jing Jiang revised the manuscript for important intellectual content. All authors contributed to and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, Jj., Gao, C., Mao, Jf. et al. Effect of endoscopic therapy and drug therapy on prognosis and rebleeding in patients with esophagogastric variceal bleeding. Sci Rep 14, 7364 (2024). https://doi.org/10.1038/s41598-024-57791-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57791-8
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.