Abstract
Over half of children with Attention-Deficit/Hyperactivity Disorder (ADHD) display interpersonal and social problems. Several lines of research suggest that suboptimal decision making, the ability to adjust choices to different risk-varying options, influences poorer choices made in social interactions. We thus measured decision making and its prediction of social problems longitudinally with the Cambridge Gambling Task in children with ADHD over four years. Children with ADHD had shown suboptimal decision making driven mainly by delay aversion at baseline and we expected this to be a stabile trait which would predict greater parent-reported social problems. From the baseline assessment (n = 70), 67% participated at the follow-up assessment, 21 from the ADHD group and 26 from the typically developing group. The mean age at the follow-up was 14.5 years old. The results confirmed our expectations that suboptimal decision making was a stabile trait in children and adolescents with ADHD. Although delay aversion did not differ from controls at follow-up it still proved to be the main longitudinal predictor for greater social problems. Our findings indicate that impulsivity in social interactions may be due to a motivational deficit in youth with ADHD.
Similar content being viewed by others
Introduction
Over half of the individuals with attention-deficit/hyperactivity disorder (ADHD) have difficulties in developing and maintaining social relationships1,2,3,4. These interpersonal problems seem to be the result of ill-considered and poorly timed social interventions and responses rather than a lack of knowledge about appropriate social conduct1,5,6. For instance, people with ADHD might choose to interject a comment into a conversation that has an inappropriate content, at an inappropriate moment or in an inappropriate way without thinking through the consequences of the actions7,8. In this sense interpersonal problems can be conceptualized, from one perspective, as expressions of suboptimal decision making causing poorer and impulsive choices to be made in social situations9. However, the question of whether the social and interpersonal problems of people with ADHD are underpinned by more general deficits in basic decision-making skills has not yet been addressed. Investigating the role of decision making in social problems in ADHD could lead to a complementary understanding compared to simply focusing on that inattentive, impulsive, and hyperactive people cannot focus, wait, or sit still enough to develop successful interactions. The core ADHD symptoms are in general found to predict social problems10, at the same time as, treatments that are effective in reducing ADHD symptoms, such as psychostimulant medication, only have small effects on enhancing social skills11,12,13,14. This suggests a dissociation between the core symptoms of ADHD and other neurocognitive processes linking the diagnosis to social impairment. It is thus a call for exploring if processes, such as social decision making, might improve the conceptualizations of the causes for social problems in ADHD and as such, contribute to finding relevant targets for social skill training15.
In the current paper, we examined this question by exploring the prospective predictive relationship between children’s performance on a widely used and well-validated task measuring risky and impulsive decision making (Cambridge Gambling Task; CGT)16,17 and parent-reported social and interpersonal problems later in development. This task measures the extent to which individuals can adjust their choices to more-or-less-risky options by integrating external information with internal value systems. The choices are made between response options with different outcome probabilities16,18. Suboptimal decision-making was measured with the CGT scores of: (1) Risk adjustment (the difficulty in adjusting decisions according to level of risk by learning from previous choices), (2) delay aversion (the choice of the less delayed option rather than the choice with the highest return), (3) reflection time (shorter reflection times reflect poorer inhibitory control19), and (4) risk proneness (over-attraction to the risky options). In phase one of the study, we included a cross-sectional baseline analysis of 36 drug-naïve children with ADHD and 34 typically developing peers aged between 8 and 12 years old. We observed that ADHD was associated with fewer optimal decisions (poorer risk adjustment), which was driven primarily by higher levels of delay aversion20. This finding was consistent with much broader literature highlighting delay aversion as a core motivational component of ADHD across settings21,22,23,24,25 and further, that poorer risk adjustment in ADHD seems to be due to other processes than being risk prone per se26. These different decision making parameters may predict greater social problems as part of an overall suboptimal decision making. For instance, impulsive choices made in social settings have been suggested to be caused predominantly by poorer inhibitory control27,28 or delay aversion29,30. However, several studies have shown a weak link between inhibitory control and social problems in ADHD31,32,33,34,35. As far as we know, no study has investigated the link between delay aversion and social problems despite the suggestions that it leads to impulsive and disruptive behavior in subjectively experienced stimulus-poor environments29,30. Furthermore, ADHD has been associated with increased risk prone behavior (see36). It is not clear to what extent this risky behavior in youth with ADHD is linked to a different social functioning in comparison with typically peers. One recent study indicated that peer influence compared to no such influence increased risk prone choices during the Balloon Analogue Risk Task across the groups of adolescents with ADHD and their typically developing peers alike37. This may suggest that risk proneness is similarly related to social influence in ADHD as in non-ADHD.
We followed up on the sample after 4 years to study the developmental outcomes associated with suboptimal decision making in ADHD. Based on the hypothesis that interpersonal problems in ADHD are driven by core deficits in decision making, we predicted that at follow-up individuals with ADHD displaying suboptimal decision making at baseline (T1) would (i) show more social and interpersonal difficulties and (ii) continue to display poor risk adjustment and delay aversion on the CGT and at the same time continue to not show difference from typically developing peers in reflection time (inhibitory control) or risk proneness. In addition to parent-reports of social problems from the Child Behavior Checklist (CBCL; Achenbach and Rescorla38), we also included parent-reports on two other subscales from CBCL of conduct problems and anxiety/depression problem symptoms due to these problems often being comorbid with ADHD and recognized in accompanying problems in social interactions. Children with ADHD often have social problems due to high frustration levels affecting their social functioning39. Conduct problems characteristically reflect higher levels of irritability, delinquency, and aggressiveness in the behavior towards peers and others40. Furthermore, problematic symptoms of anxiety and depression are associated with higher frustration levels and irritability41 as well as with social isolation42.
Results
Sample characteristics
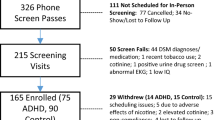
From the original sample (N = 70) at baseline performing the CGT (T1), 67% (N = 47) participated at the follow-up assessment (T2); 58% (n = 21) from the ADHD group and 77% (n = 26) from the typically developing group (see Supplemental Fig. 1). At T2, the age range was 11–17 years old with a mean age of 14.5 (SD = 1.31). The two groups did not differ significantly in age or gender distribution (see Table 1). The mean T1 and T2 interval was 4.5 years (SD = 0.7) with no significant difference in interval between the two groups. At T2, all the adolescents in the ADHD group still met the criteria for an ADHD diagnosis, and 48% of these had a comorbid disorder; six had anxiety; six had oppositional defiant disorder (ODD), two had tics, one had depression, and one obsessive–compulsive disorder. In the control group, two had an anxiety disorder. In the ADHD group, 76% (n = 16) used CNS stimulants to treat their ADHD. Of these, 88% conducted a washout period of at least 24 h before testing, whereas two participants had a washout period of at least 12 and 18 h, respectively. These are all acceptable washout periods due to the two that had a shorter period used methylphenidate, which has a half-life of two to three hours and the active ingredient eliminated after 10–15 h43,44. Children with ADHD who remained in the study at T2 showed no significant differences in scores on the CGT, Full-Scale IQ, or ADHD symptoms at T1 compared to their counterparts who dropped out (see Supplemental Table 1).
Did decision making deficits seen at baseline persist to follow up?
Cross-sectionally, the ADHD group showed poorer risk adjustment compared with the control group at both T1 and T2, higher delay aversion only at T1, and higher risk proneness only at T2 (see Table 1). No cross-sectional group differences appeared in relation to reflection times (inhibitory control). Longitudinally (alpha levels (α) were Bonferroni corrected for conducting four ANOVAs; p < 0.013), including both ADHD and the two time points as factors, there was a main effect (F(1,90) = 8.91, p = 0.004, ηp2 = 0.09) of group on decision making quality with the ADHD sample showing poorer risk adjustment at both baseline and follow-up (see Fig. 1 and Supplemental Table 2). There was no significant effect of time and no interaction between time and group. Furthermore, the risk adjustment scores at baseline and follow-up were significantly correlated in the whole sample (r = 0.36, p = 0.014) and in the ADHD group (r = 0.51, p = 0.018) but not in the control group alone (r = 0.20). However, stability was less clear for the other decision elements with the ADHD group showing more delay aversion than controls at baseline than follow-up (main effect of time points: F(1,90) = 18.16, p = 0.001, ηp2 = 0.20). Still, in the whole sample (r = 0.34, p = 0.02) and in the ADHD group (r = 0.45, p = 0.041), greater delay aversion at both time points correlated significantly, except in the control group (r = 0.29). No significant effect of ADHD appeared on risk proneness or in reflection times (inhibitory control) neither at baseline nor follow-up when the two time points were included as a factor in addition to ADHD. Risk proneness as measured at the two time points did not correlate, whereas reflection times correlated highly between the two timepoints in the whole sample and in both subgroups. See Supplemental Table 4 for all the intercorrelations of the CGT parameters cross-sectionally and longitudinally.
Did adolescents with ADHD show more social problems?
Parents reported that children with ADHD showed greater social problems and greater problems of conduct behavior and anxiety/depression at both time points compared with control children (see Table 1). At follow up all three problem areas of social problems, conduct behavior, and anxiety/depression correlated highly with each other (see Table 2).
Were social problems correlated with decision making on the CGT cross sectionally and longitudinally?
Table 2 shows the correlations between social problems at follow-up and CGT parameters at baseline and follow-up. Cross-sectional associations at follow-up were significant between the CGT parameters of poorer risk adjustment and longer reflection times (inhibitory control), and further, between poor risk adjustment and greater social problems, and greater anxiety/depression problems. Furthermore, the CGT parameters did not correlate with conduct problems nor did risk proneness correlate with social problems or problems of conduct behavior and anxiety/depression at follow-up. Longitudinally, significant correlations were seen for both the baseline CGT parameters of poorer risk adjustment and greater delay aversion with greater social problems at follow-up. Baseline reflection times (inhibitory control) and risk proneness did not correlate with social problems at follow-up. Further, only the baseline CGT parameter of greater delay aversion correlated with higher anxiety/depression problems at follow-up, and only longer reflection times (inhibitory control) at baseline correlated with greater conduct problems at follow up. To test for the specificity of the effect baseline CGT parameters had on social problems and problems of conduct behavior and anxiety/depression at follow up, we included the three baseline CGT parameters that correlated longitudinally with these problems as predictors (risk adjustment, delay aversion, and reflection times) in three multiple linear regression analyses with the three CBCL scores as outcome variables [alpha level (α) was Bonferroni corrected for conducting three regression analyses; p < 0.017]. The results showed that only greater delay aversion at baseline, and not poorer risk adjustment or reflection times (inhibitory control), predicted greater social problems at follow up (see Table 3 and Fig. 2). None of the CGT parameters specifically predicted level of conduct problems or anxiety/depression problems at follow-up.
Scatterplots of the longitudinal relationship between the baseline CGT parameters of risk adjustment, delay aversion, and reflection time (inhibitory control) and parent-reported social problems at follow-up. Delay aversion was the only predictor of these CGT parameters that predicted significantly greater social problems at follow-up.
Discussion
In the current study, children with ADHD were followed up longitudinally to study the development of suboptimal decision making over time and its prediction of social problems between childhood and adolescence. We originally found that the children with ADHD displayed suboptimal choices as measured with risk adjustment at baseline, driven primarily by delay aversion on the CGT compared with typically developing peers. At follow-up four years later, we expected that individuals with ADHD would still show poorer risk adjustment and greater delay aversion than their typically developing peers, and that baseline suboptimal decision making would predict greater parent-reports of social problems and conduct and anxiety/depression problems. As expected, the results showed that poorer risk adjustment was a stable trait over 4 years in children and adolescents with ADHD. Delay aversion, on the other hand, was no longer significantly different at follow-up in the ADHD group compared with the control group. Still, greater delay aversion along with poorer risk adjustment correlated from baseline to follow-up only in the ADHD group and not in the control group. The CGT parameters of poorer risk adjustment, greater delay aversion, and longer reflection times (inhibitory control) were correlated both cross-sectionally and longitudinally with greater interpersonal problems and conduct and anxiety/depression problems. However, when including these CGT parameters in the same statistical model, greater delay aversion at baseline (T1) was the only CGT parameter that four years later (T2) predicted greater social problems (see Fig. 3). Furthermore, none of these CGT parameters at baseline predicted conduct or anxiety/depression problems four years later. Risk proneness was not different in the ADHD group at T1 but showed a tendency to be higher in this group at T2. It did, however, not correlate with social problems or conduct or anxiety/depression problems. Reflection time (inhibitory control) was not different between the groups at either time point.
Hypothesized models illustrating (a) the expected prediction of baseline suboptimal decision making on longitudinal interpersonal problems, and the effect of delay aversion on interpersonal problems via poorer risk adjustment, and (b) the role of baseline delay aversion both as contributing to suboptimal decision making and directly predicting interpersonal problems four years later.
Parents and teachers consistently report that children with ADHD struggle with interpersonal interactions and relationships1,4,6,35, as is the case in the current study. These reports typically coincide with the perception reported by peers that children with ADHD are more often rejected and neglected by peers, having fewer friends and fewer and less diverse social activities13,31,45,46. Our results indicate that these problems are predicted by difficulties in adapting dynamically to changing contextual conditions. On the CGT this can be observed by difficulties in adapting choices to the changing patterns of outcome probabilities (poorer risk adjustment). In the current study, the motivational style of escaping delays was the main driver for these problems. Delay aversion has previously been suggested to cause social problems by leading to impulsive and disruptive behavior29,30. Importantly, our study appears, as far as we know, to be the first to experimentally investigate and link delay aversion with greater interpersonal problems. This is in line with the dominant causal hypothesis of ADHD in children in that they tend to choose immediate rewards more consistently when this choice gives escape from delay compared to when the same choice does not escape delay23. This drive for escape when children with ADHD perceive situations as tedious (stimulus-poor) is suggested to be associated with a negative affective state (high frustration), which is supported by fMRI studies of adolescents25,47 and adults48 with ADHD.
In line with findings from several previous studies31,32,33,34,35, the children with ADHD did not show suboptimal decision making or social problems due to poorer inhibitory control as reflected in shorter reflection times. Rather, it was a general finding that longer reflection times correlated with greater social problems, which probably are linked to challenges of processing information fast enough in social situations49. Important to note, though, is that a previous study has shown that the delay aversion score from the CGT can be challenging to distinguish from poor inhibitory control in ADHD22. In our original study20, we therefore tested for this and found that (a) the delay aversion score was linked to shorter test duration time—showing the CGT delay aversion score to be linked to escape of delay and not just an impulsive drive for immediate reward (see23,50), and (b) the prediction of delay aversion in explaining suboptimal decision making in ADHD was not explained by poorer inhibitory control (as measured with the Cambridge Stop Signal Test) or by level of intelligence and working memory capacity. Inhibitory control, intelligence and working memory capacity did not either covary in our original study with suboptimal decision making when testing the group differences between ADHD and control children20.
Our findings showed that delay aversion at baseline tended to specifically predict greater interpersonal problems in general and not conduct or anxiety/depression problems. Both conduct and anxiety/depression problem scores were significantly higher in the ADHD group and highly correlated with social problems. In relation to the CGT scores, greater delay aversion correlated with higher anxiety/depression problem symptoms, and longer reflection times with greater conduct problems. This supports delay aversion being described as expressing negative affectivity48—typically associated with higher levels of anxiety and/or depression51. Longer reflection times have also been found to be associated with lower motivation to do tasks as instructed52, which higher conduct problems can reflect via non-compliance with external expectations. However, including the CGT parameters that correlated with social problems and the problem scores of conduct behavior and anxiety/depression in the same regression models, showed that none of them specifically predicted higher conduct or anxiety/depression problems.
To our knowledge, this is the first study that has investigated the link between suboptimal decision making and interpersonal problems in ADHD. However, in adults with schizophrenia53 and in young healthy adults54, both studies using a different test method than CGT, found that suboptimal decision making was associated with poorer social skills and interpersonal relationships. In children with ADHD, one study investigated the ability of teacher-reported ADHD symptoms to predict parent-reports on the social problem subscale from the CBCL and performance on a decision making task using affective cues two years later55. The ADHD symptoms predicted both greater social problems and poorer decision making. However, the cross-sectional correlation coefficient between social problems and the affective cuing decision making task scores was low (r = 0.21). Future studies are encouraged to further test the prediction of suboptimal decision making on social problems in ADHD. The low sample size in the current study may rise issues of low statistical power when testing longitudinal associations despite the a priori power analysis showed the sample size to be sufficient for avoiding a type II error.
In the current study, the children with ADHD were drug naïve at baseline and the majority on medication at follow-up. This may have affected the longitudinal findings in that medication according to its objectives is supposed to have long-term effects on cognition and motivational style56. These effects may be present even though we asked the participants to refrain from taking the medicine before the testing. We found, however, that suboptimal decision making was a stable trait in the ADHD group suggesting that CNS medication did not have a long-term effect on improving the ability to choose optimal options in ambiguous and risky situations (on the gambling task)—besides the short-term effects shown previously on the CGT57. This is in line with a recent study on the effects of methylphenidate in adolescents with ADHD, in which no long-term effects were found on any of the outcome measures including on cognitive functioning14. It is possible that medication may have led to a higher tolerance for delay at the follow-up assessment, or it may be due to the children with ADHD being older and more mature in their decision making abilities. In relation to social competence and the effect of CNS medication, one systematic review found that children treated with medication and/or non-pharmacological interventions for their ADHD had better social functioning compared to untreated children with ADHD58. Other studies, however, have found that methylphenidate alone, or in combination with cognitive behavioral therapy, had only a limited effect on social behavior in children with ADHD11,12,13,14. In boys with ADHD, the positive effect of methylphenidate was specifically observed in higher compliance with expected behavior and a decrease in aggressive behavior tendencies12.
Conclusion
Interpersonal problems are recognized as one of the important impairments negatively affecting quality of life in children with ADHD58,59. Early predictors and mechanisms of interpersonal problems are thus essential to identify15. The current study showed that suboptimal decision making driven by delay aversion can be an important predictor to address in future studies of interpersonal competence in ADHD. A deeper understanding of this relationship may initiate specific programs of psychoeducation about living with ADHD for caregivers and the children. This relationship may also be important to address in training programs to improve quality of life for children with ADHD.
Methods
Participants
The current study was a follow-up of children 8 to 12 years old with ADHD and age-matched typically developing peers performing the CGT20. The children were originally included at baseline (T1) with a Full-Scale Intelligent Quotient (FSIQ) > 8060 and diagnostically evaluated with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS)61. The K-SADS was re-administered at the follow-up assessment (T2). The test administrators of the neuropsychological test battery including the CGT were blinded to group status both at T1 and T2. The parents reported on the children’s’ mental health and social functioning at both time points (described below). At T2, children were first interviewed with the K-SADS while parents filled out questionnaires, and subsequently the children performed a neuropsychological test battery and filled out questionnaires while the parents were interviewed with the K-SADS. The study protocol was approved by the Regional committee for medical research ethics of western Norway (study number: 2014/1304) and research was conducted according to relevant regulations and guidelines. Informed consent was given both orally and in written form from all the parents and the adolescents. Both the adolescents’ (at T2) and their parents (at T1 and T2) signed written consent in accordance with the Declaration of Helsinki. The participants received a reimbursement of $115.
Cambridge gambling task (CGT)
The CGT from the Cambridge Neuropsychological Test Automated Battery, CANTAB; www.camcog.com16,17, was administered at T1 and T2 (see Fig. 4). The children were first instructed that a yellow token was hidden behind either a blue or red box, presented in an array of 10 boxes at the top of the computer screen. Secondly, they were instructed to make a bet on the likelihood of their decision being correct or not. Points were presented in a box on the right-hand side in 5-s increments/decrements sequences. The children touched the box to place a bet. In four of the test blocks, the bets were presented in an ascending order of 5, 25, 50, 75, and 95% portion of the points that the children would “earn” on each trial (displayed on the left-hand side of the computer screen), and in the other four blocks they were presented in a descending order (95, 75, 50, 25, and 5% portion of the points). The order of presentation (ascending or descending) was counterbalanced across individuals within the groups at both time points. The task was administered on a desktop PC and responses recorded via a touch-sensitive screen (see Sørensen et al.20 for further details). As measures of suboptimal decision making, we included the CGT generated scores of (a) risk adjustment measuring the ability in adjusting decisions according to level of risk by learning from previous choices, (b) delay aversion measured the proportion of choices made for the option available most immediately irrespective of the outcome, (c) reflection time (inhibitory control) measured the time taken to think about the options during the decision phase and was calculated based on the deliberation time between stimulus presentation and choice outcome, and (d) risk proneness was defined by the total number of points that were gambled on the most improbable outcome—reflecting the overall tendency to take risks. These scores were centralized as z-scores.
A screen shot of the Cambridge Gambling Task (CGT). The red and blue boxes at the top of the screen are hiding a yellow token and the red and blue squares at the bottom of the screen are pushed to guess which colored box the token is hidden behind. The numbers presented represent percentages of the points displayed at the left-hand side that are presented either in ascending or descending sequences. Note. The image is printed with permission from © Copyright 2023 Cambridge Cognition Limited. All rights reserved.
Social problems and conduct and anxiety/depression problems
Parents completed the Child Behavior Checklist 6–18 (CBCL)38 at T1 and T2. The CBCL is a 113-item rating scale with a 3-point response scale, from 0 for not true to 2 for very true/often true. The CBCL is a widely used instrument with excellent test–retest reliability, internal consistency, and interrater reliability38. The total score from the subscale of social problems was used as a measure of interpersonal problems. The items of this subscale relate to different areas of social functioning including peer rejection, interaction style, impact of peer rejection (feeling lonely), and behaviors that are observed with peer rejection such as clumsiness and speech problems. The subscales of social problems, anxiety/depression problems, and conduct problems have all been shown to have high test–retest reliability38 and acceptable internal consistency (≥ 0.70) with the Norwegian translation62. The standardized percentile scores were included in the statistical analyses.
Statistical analyses
All analyses were performed with SPSS, version 28. The longitudinal sample was first described by testing group differences on sample characteristics with independent sample t-tests. To test for longitudinal effects of ADHD on decision making, four analyses of variances (ANOVAs) were conducted with a 2 (ADHD vs. no ADHD) × 2 (effects of timepoint vs. no effects of timepoints) factorial design to test for between-group differences on the CGT scores of risk adjustment, delay aversion, reflection time (inhibitory control), and risk proneness. An interaction effect between ADHD and time points would suggest that the effect of ADHD on one of the CGT scores would be specific to one of the time points. Age and gender were not included as covariates in the final ANOVA models due to not changing the significant effects of ADHD on the CGT scores. See Supplemental Table 3 for the age-adjusted ANOVA results in which age only covaried with delay aversion and gender only with risk proneness (see also Supplemental Tables 4 and 5). Further, the effect of ADHD on social problems and problems of conduct behavior and anxiety/depression was investigated with independent sample t-test analyses. Bivariate correlations were estimated first on the relationship between the parent-reported problem scores and thereafter on the cross-sectional and longitudinal relationship between the CGT scores and the parent-reported scores of social problems, conduct problems, and anxiety/depression problems. The baseline CGT scores (T1) that correlated with the social and conduct and anxiety/depression problems at follow-up (T2) were further included (simultaneous) as predictors in three multiple linear regression analyses with the follow-up parent reported scores on social problems, conduct problems, and anxiety/depression problems as the outcome variables, respectively. Age was not included as a covariate in the final linear regression models due to not covarying with the parent-reported outcome scores of social problems, conduct problems, or anxiety/depression problems (see Supplemental Table 6 for the bivariate correlations between age and the CBCL scores of social problems, anxiety/depression problems, and conduct problems).
We adjusted for multiple analyses by using Bonferroni correction of alpha level (α) in the between-group analyses (ANOVAs); p = 0.05/4, (four CGT outcome scores) which gives an α corrected p level of 0.013, and in the multiple linear regression analysis with parent-reported problem scores as the outcome variables; p = 0.05/3 (three CBCL outcome scores), which gives an α corrected p level of 0.017. Outliers were defined using a ± 3 standard deviations threshold from the sample mean and replaced and included in the statistical analyses with a score of ± 3 standard deviations from the sample mean. On the CGT: One child with ADHD showed very long reflection time (z = 4.24) and two typically developing children showed very high scores on risk adjustment (z = 3.18 and z = 3.52). No outlier scores were detected on the CBCL.
A priori estimation of statistical power was performed to determine the sample size needed to estimate longitudinal statistical effects of ADHD on suboptimal decision making. Using g*power, we included the mean scores of risk adjustment of the ADHD group (0.61) and the controls (1.20), respectively, from T120, and adjusted for the statistical variance (SD = 0.65) of the ADHD group. We specified the conventional level of sufficient power to be 1 − ß = 0.80 and a significance of α = 0.05. The analysis revealed that a total number of n = 42 young people would at least be required to avoid a type II error in our study, which is below our sample size of n = 47.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
de Boo, G. M. & Prins, P. J. Social incompetence in children with ADHD: Possible moderators and mediators in social-skills training. Clin. Psychol. Rev. 27, 78–97. https://doi.org/10.1016/j.cpr.2006.03.006 (2007).
Hoza, B. et al. What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder?. J. Consult. Clin. Psychol. 73, 411–423. https://doi.org/10.1037/0022-006X.73.3.411 (2005).
Landau, S. & Miilich, R. Social communication of attention-deficit-disordered boys. J. Abnorm. Child Psychol. 16, 69–81. https://doi.org/10.1007/BF00910501 (1988).
Ros, R. & Graziano, P. A. Social functioning in children with or at risk for attention deficit/hyperactivity disorder: A meta-analytic review. J. Clin. Child Adolesc. Psychol. 47, 213–235. https://doi.org/10.1080/15374416.2016.1266644 (2018).
Aduen, P. A. et al. Social problems in ADHD: Is it a skills acquisition or performance problem?. J. Psychopathol. Behav. Assess. 40, 440–451. https://doi.org/10.1007/s10862-018-9649-7 (2018).
Huang-Pollock, C. L., Mikami, A. Y., Pfiffner, L. & McBurnett, K. Can executive functions explain the relationship between attention deficit hyperactivity disorder and social adjustment?. J. Abnorm. Child Psychol. 37, 679–691. https://doi.org/10.1007/s10802-009-9302-8 (2009).
Cunningham, C. E. & Siegel, L. S. Peer interactions of normal and attention-deficit-disordered boys during free-play, cooperative task, and simulated classroom situations. J. Abnorm. Child Psychol. 15, 247–268. https://doi.org/10.1007/BF00916353 (1987).
Winsler, A. Parent-child interaction and privarte speech in boys with ADHD. Appl. Dev. Sci. 2, 17–39. https://doi.org/10.1207/s1532480xads0201_2 (1998).
Lee, S. S. & Harris, L. T. How social cognition can inform social decision making. Front. Neurosci. https://doi.org/10.3389/fnins.2013.00259 (2013).
Thompson, K. N. et al. Do children with attention-deficit/hyperactivity disorder symptoms become socially isolated? Longitudinal within-person associations in a nationally representative cohort. JAACAP Open 1, 12–23. https://doi.org/10.1016/j.jaacop.2023.02.001 (2023).
Alkalay, S. & Dan, O. Effect of short-term methylphenidate on social impairment in children with attention deficit/hyperactivity disorder: Systematic review. Child Adolesc. Psychiatry Ment. Health 16, 93. https://doi.org/10.1186/s13034-022-00526-2 (2022).
Granger, D. A., Whalen, C. K., Henker, B. & Cantwell, C. ADHD boys’ behavior during structured classroom social activities: Effects of social demands, teacher proximity, and methylphenidate. J. Attent. Disord. 1, 16–30. https://doi.org/10.1177/108705479600100102 (1996).
Hoza, B. et al. Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. J. Clin. Child Adolesc. Psychol. 34, 74–86. https://doi.org/10.1207/s15374424jccp3401_7 (2005).
Schweren, L. et al. Long-term effects of stimulant treatment on ADHD symptoms, social-emotional functioning, and cognition. Psychol. Med. 49, 217–223. https://doi.org/10.1017/S0033291718000545 (2019).
Morris, S., Sheen, J., Ling, M., Foley, D. & Sciberras, E. Interventions for adolescents with ADHD to improve peer social functioning: A systematic review and meta-analysis. J. Atten. Disord. 25, 1479–1496. https://doi.org/10.1177/1087054720906514 (2021).
Clark, L. et al. Differential effects of insular and ventromedial prefrontal cortex lesions on risky decision-making. Brain 131, 1311–1322. https://doi.org/10.1093/brain/awn066 (2008).
Rogers, R. D. et al. Dissociable deficits in the decision-making cognition of chronic amphetamine abusers, opiate abusers, patients with focal damage to prefrontal cortex, and tryptophan-depleted normal volunteers: Evidence for monoaminergic mechanisms. Neuropsychopharmacology 20, 322–339. https://doi.org/10.1016/S0893-133X(98)00091-8 (1999).
Ochsner, K. N. & Gross, J. J. Handbook of Emotion Regulation Vol. 2nd (The Guilford Press, 2014).
Solanto, M. V. et al. Neurocognitive functioning in AD/HD, predominantly inattentive and combined subtypes. J. Abnorm. Child Psychol. 35, 729–744. https://doi.org/10.1007/s10802-007-9123-6 (2007).
Sorensen, L. et al. Suboptimal decision making by children with ADHD in the face of risk: Poor risk adjustment and delay aversion rather than general proneness to taking risks. Neuropsychology 31, 119–128. https://doi.org/10.1037/neu0000297 (2017).
Bitsakou, P., Psychogiou, L., Thompson, M. & Sonuga-Barke, E. J. Delay aversion in attention deficit/hyperactivity disorder: An empirical investigation of the broader phenotype. Neuropsychologia 47, 446–456. https://doi.org/10.1016/j.neuropsychologia.2008.09.015 (2009).
Coghill, D. R., Seth, S. & Matthews, K. A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in attention deficit hyperactivity disorder: Advancing beyond the three-pathway models. Psychol. Med. 44, 1989–2001. https://doi.org/10.1017/S0033291713002547 (2014).
Marco, R. et al. Delay and reward choice in ADHD: An experimental test of the role of delay aversion. Neuropsychology 23, 367–380. https://doi.org/10.1037/a0014914 (2009).
Sonuga-Barke, E., Bitsakou, P. & Thompson, M. Beyond the dual pathway model: Evidence for the dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 49, 345–355. https://doi.org/10.1016/j.jaac.2009.12.018 (2010).
Van Dessel, J. et al. Delay aversion in attention deficit/hyperactivity disorder is mediated by amygdala and prefrontal cortex hyper-activation. J. Child Psychol. Psychiatry 59, 888–899. https://doi.org/10.1111/jcpp.12868 (2018).
Dekkers, T. J. et al. Decision-making deficits in ADHD are not related to risk seeking but to suboptimal decision-making: Meta-analytical and novel experimental evidence. J. Atten. Disord. 25, 486–501. https://doi.org/10.1177/1087054718815572 (2021).
Bunford, N. et al. Attention-deficit/hyperactivity disorder symptoms mediate the association between deficits in executive functioning and social impairment in children. J. Abnorm. Child Psychol. 43, 133–147. https://doi.org/10.1007/s10802-014-9902-9 (2015).
Rinsky, J. R. & Hinshaw, S. P. Linkages between childhood executive functioning and adolescent social functioning and psychopathology in girls with ADHD. Child Neuropsychol. 17, 368–390. https://doi.org/10.1080/09297049.2010.544649 (2011).
Kofler, M. J. et al. Working memory deficits and social problems in children with ADHD. J. Abnorm. Child Psychol. 39, 805–817. https://doi.org/10.1007/s10802-011-9492-8 (2011).
Nixon, E. The social competence of children with attention deficit hyperactivity disorder: A review of the literature. Child Psychol. Psychiatry Rev. 6, 172–179. https://doi.org/10.1111/1475-3588.00342 (2001).
Flicek, M. Social status of boys with both academic problems and attention-deficit hyperactivity disorder. J. Abnorm. Child Psychol. 20, 353–366. https://doi.org/10.1007/BF00918981 (1992).
Hilton, D. C., Jarrett, M. A., McDonald, K. L. & Ollendick, T. H. Attention problems as a mediator of the relation between executive function and social problems in a child and adolescent outpatient sample. J. Abnorm. Child Psychol. 45, 777–788. https://doi.org/10.1007/s10802-016-0200-6 (2017).
Kofler, M. J. et al. Heterogeneity in ADHD: Neurocognitive predictors of peer, family, and academic functioning. Child Neuropsychol. 23, 733–759. https://doi.org/10.1080/09297049.2016.1205010 (2017).
Tseng, W. L. & Gau, S. S. Executive function as a mediator in the link between attention-deficit/hyperactivity disorder and social problems. J. Child Psychol. Psychiatry 54, 996–1004. https://doi.org/10.1111/jcpp.12072 (2013).
Kofler, M. J. et al. Neurocognitive and behavioral predictors of social problems in ADHD: A Bayesian framework. Neuropsychology 32, 344–355. https://doi.org/10.1037/neu0000416 (2018).
Roberts, D. K., Alderson, R. M., Betancourt, J. L. & Bullard, C. C. Attention-deficit/hyperactivity disorder and risk-taking: A three-level meta-analytic review of behavioral, self-report, and virtual reality metrics. Clin. Psychol. Rev. 87, 102039. https://doi.org/10.1016/j.cpr.2021.102039 (2021).
Dekkers, T. J. et al. Risk taking by adolescents with attention-deficit/hyperactivity disorder (ADHD): A behavioral and psychophysiological investigation of peer influence. J. Abnorm. Child Psychol. 48, 1129–1141. https://doi.org/10.1007/s10802-020-00666-z (2020).
Achenbach, T. M. & Rescorla, L. A. Manual for the ASEBA School-Age Forms & Profiles (University of Vermont Research Center for Children. Youth. & Families, 2001).
Evans, S. C. et al. Examining ODD/ADHD symptom dimensions as predictors of social, emotional, and academic trajectories in middle childhood. J. Clin. Child Adolesc. Psychol. 49, 912–929. https://doi.org/10.1080/15374416.2019.1644645 (2020).
Elowsky, J. et al. Differential associations of conduct disorder, callous-unemotional traits and irritability with outcome expectations and values regarding the consequences of aggression. Child Adolesc. Psychiatry Ment. Health 16, 38. https://doi.org/10.1186/s13034-022-00466-x (2022).
Savage, J. et al. A genetically informed study of the longitudinal relation between irritability and anxious/depressed symptoms. J. Am. Acad. Child Adolesc. Psychiatry 54, 377–384. https://doi.org/10.1016/j.jaac.2015.02.010 (2015).
Brown, V., Morgan, T. & Fralick, A. Isolation and mental health: thinking outside the box. Gen. Psychiatr. 34, e100461. https://doi.org/10.1136/gpsych-2020-100461 (2021).
Ito, S. Pharmacokinetics 101. Paediatr. Child Health 16, 535–536. https://doi.org/10.1093/pch/16.9.535 (2011).
Kimko, H. C., Cross, J. T. & Abernethy, D. R. Pharmacokinetics and clinical effectiveness of methylphenidate. Clin. Pharmacokinet. 37, 457–470. https://doi.org/10.2165/00003088-199937060-00002 (1999).
Bagwell, C. L., Molina, B. S., Pelham, W. E. Jr. & Hoza, B. Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. J. Am. Acad. Child Adolesc. Psychiatry 40, 1285–1292. https://doi.org/10.1097/00004583-200111000-00008 (2001).
Heiman, T. An examination of peer relationships of children with and without attention deficit hyperactivity disorder. School Psychol. Int. 26, 330–339. https://doi.org/10.1177/0143034305055977 (2005).
Lemiere, J. et al. Brain activation to cues predicting inescapable delay in adolescent attention deficit/hyperactivity disorder: An fMRI pilot study. Brain Res. 1450, 57–66. https://doi.org/10.1016/j.brainres.2012.02.027 (2012).
Wilbertz, G. et al. Neural and psychophysiological markers of delay aversion in attention-deficit hyperactivity disorder. J. Abnorm. Psychol. 122, 566–572. https://doi.org/10.1037/a0031924 (2013).
Thorsen, A. L., Meza, J., Hinshaw, S. & Lundervold, A. J. Processing speed mediates the longitudinal association between ADHD symptoms and preadolescent peer problems. Front. Psychol. 8, 2154. https://doi.org/10.3389/fpsyg.2017.02154 (2017).
Sonuga-Barke, E. J. The dual pathway model of AD/HD: An elaboration of neuro-developmental characteristics. Neurosci. Biobehav. Rev. 27, 593–604. https://doi.org/10.1016/j.neubiorev.2003.08.005 (2003).
Iqbal, N. & Dar, K. A. Negative affectivity, depression, and anxiety: Does rumination mediate the links?. J. Affect. Disord. 181, 18–23. https://doi.org/10.1016/j.jad.2015.04.002 (2015).
Wolf, C. & Lappe, M. Motivation by reward jointly improves speed and accuracy, whereas task-relevance and meaningful images do not. Atten. Percept. Psychophys. 85, 930–948. https://doi.org/10.3758/s13414-022-02587-z (2023).
Stratta, P., Cella, M., Di Emidio, G., Collazzoni, A. & Rossi, A. Exploring the association between the Iowa Gambling Task and community functioning in people with schizophrenia. Psychiatr. Danubina 27, 371–377 (2015).
Parker, A. M. & Fischhoff, B. Decision-making competence: External validation through an individual-differences approach. J. Behav. Decis. Making 18, 1–27. https://doi.org/10.1002/bdm.481 (2005).
Humphreys, K. L., Galan, C. A., Tottenham, N. & Lee, S. S. Impaired social decision-making mediates the association between ADHD and social problems. J. Abnorm. Child Psychol. 44, 1023–1032. https://doi.org/10.1007/s10802-015-0095-7 (2016).
Abikoff, H. et al. Symptomatic improvement in children with ADHD treated with long-term methylphenidate and multimodal psychosocial treatment. J. Am. Acad. Child Adolesc. Psychiatry 43, 802–811. https://doi.org/10.1097/01.chi.0000128791.10014.ac (2004).
DeVito, E. E. et al. The effects of methylphenidate on decision making in attention-deficit/hyperactivity disorder. Biol. Psychiatry 64, 636–639. https://doi.org/10.1016/j.biopsych.2008.04.017 (2008).
Harpin, V., Mazzone, L., Raynaud, J. P., Kahle, J. & Hodgkins, P. Long-term outcomes of ADHD: A systematic review of self-esteem and social function. J. Atten. Disord. 20, 295–305. https://doi.org/10.1177/1087054713486516 (2016).
Coghill, D., Danckaerts, M., Sonuga-Barke, E., Sergeant, J. & Group, A. E. G. Practitioner review: Quality of life in child mental health–conceptual challenges and practical choices. J. Child Psychol. Psychiatry 50, 544–561. https://doi.org/10.1111/j.1469-7610.2009.02008.x (2009).
Wechsler, D. Wechsler Intelligence Scale for Children 4th edn. (Psychological Corporation, 2023).
Kaufman, J. et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988. https://doi.org/10.1097/00004583-199707000-00021 (1997).
Jozefiak, T., Larsson, B., Wichstrom, L. & Rimehaug, T. Competence and emotional/behavioural problems in 7–16-year-old Norwegian school children as reported by parents. Nord. J. Psychiatry 66, 311–319. https://doi.org/10.3109/08039488.2011.638934 (2012).
Acknowledgements
We would like to thank the children and parents who participated in the study and Dr. Hayley MacDonald for language editing the manuscript. This work was supported by grants from the Research Council of Norway (190544/H110), the Western Norway Health Authority (MoodNet and the Network for Anxiety Disorders; 911435, 911607, 911827) to KP and by grants from the Western Norway Health Authority (911460) and the National Norwegian ADHD network to LS. This paper represents independent research part funded by the NIHR Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. Figure 4 was printed with permission from Cambridge Cognition.
Funding
Open access funding provided by University of Bergen.
Author information
Authors and Affiliations
Contributions
LS: Study design, experimental design, data collection, data analysis, interpretation, writing of the manuscript. SA: Data collection, interpretation, writing of the manuscript. EK: Data collection, revision of the manuscript. HE: Data collection, revision of the manuscript. KP: Study design, experimental design, data collection, revision of the manuscript. ESB: Guiding data analysis, interpretation, writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Lin Sørensen has received small research funding for speaking and conference support from Medice in 2023. Edmund Sonuga-Barke declares competing interest during the 3 years prior to July 2023: Speaker fees, consultancy or research funding from Medice, Takeda, Neurotech Solutions and QBTech. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sørensen, L., Adolfsdottir, S., Kvadsheim, E. et al. Suboptimal decision making and interpersonal problems in ADHD: longitudinal evidence from a laboratory task. Sci Rep 14, 6535 (2024). https://doi.org/10.1038/s41598-024-57041-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57041-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.