Abstract
Reducing hypotension is crucial as hypotension is the most common side effect of spinal anesthesia, and in older patients with various comorbidities, it can lead to fatality. We hypothesized that continuous infusion of norepinephrine could effectively prevent hypotension in older patients undergoing hip surgery under spinal anesthesia with propofol sedation. The study randomly assigned patients aged ≥ 70 years to either a control (Group C, n = 35) or a norepinephrine group (Group N, n = 35). After spinal anesthesia, continuous infusion of propofol and normal saline or norepinephrine was initiated. The number of hypotensive episodes, the primary outcome, as well as other intraoperative hemodynamic events and postoperative complications were compared. In total, 67 patients were included in the final analysis. The number of hypotensive episodes was significantly higher in Group C than in Group N (p < 0.001). Furthermore, Group C required a greater amount of fluid to maintain normovolemia (p = 0.008) and showed less urine output (p = 0.019). However, there was no difference in postoperative complications between the two groups. Continuous intravenous infusion of prophylactic norepinephrine prevented hypotensive episodes, reduced the requirement of fluid, and increased the urine output in older patients undergoing unilateral hip surgery under spinal anesthesia with propofol sedation.
Clinical trial registration number: KCT0005046 (https://cris.nih.go.kr). IRB number: 2020-0533 (Institutional Review Board of Asan Medical Center, approval date: 13/APR/2020).
Similar content being viewed by others
Introduction
Hypotension is the most common side effect of spinal anesthesia (SA), especially in older individuals. High-segment sensory nerve block and advanced age are major risk factors for hypotension after SA1. Propofol, which is widely used for sedation, acts as a vasodilator by decreasing sympathetic activity, and can reduce blood pressure when injected intravenously. Therefore, if propofol is injected intravenously for sedation during surgery in patients receiving SA, the incidence of hypotension may increase. In addition, in older patients with various comorbidities, postoperative complications resulting from intraoperative hypotension (IOH) can lead to fatalities. In the past, phenylephrine was commonly used for the management of SA-induced hypotension2,3,4,5. Recently, however, norepinephrine has been described as an effective alternative to phenylephrine for the prevention and treatment of hypotension during SA for cesarean delivery6,7,8,9,10,11. Relatively few studies have evaluated the effectiveness of continuous infusion of norepinephrine in preventing IOH in older patients12,13. Therefore, in this study, we aimed to investigate whether norepinephrine administration can effectively prevent hypotension in older patients aged ≥ 70 years undergoing unilateral primary hip surgery under SA with propofol sedation. Moreover, we evaluated the effect of continuous norepinephrine infusion on the intraoperative hemodynamic events and postoperative outcomes.
Results
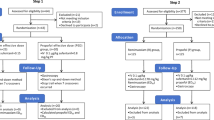
In total, 67 patients were included in the final analysis (Fig. 1). All data were expressed as means ± standard deviations or medians [interquartile ranges]. There was no difference in the demographic data, co-existing disease, or preoperative laboratory data between the two groups, except for the albumin level (Table 1).
Table 2 presents the surgery-related data of the two groups. We found no significant differences in the type of surgery, anesthesia time, operation time, propofol infusion time, and intraoperative blood loss. However, the two groups showed significant differences in the total amount of crystalloid solution and urine output during surgery. The control group (Group C) required a greater amount of crystalloid solution to maintain normovolemia based on the value of the pleth variability index (PVi) compared to the norepinephrine group (Group N) (Group C, 795.7 ± 312.3 mL; Group N, 579.7 ± 336.9 mL; p = 0.008). Urine output was also greater in Group N than in Group C (Group N, 70.0 [42.5–155.0] mL; Group C, 40.0 [0.0–80.0] mL; p = 0.019). No adverse events were observed related to the peripheral vein route of norepinephrine administration.
The primary outcome and the number of hypotensive episodes during surgery were significantly higher in Group C than in Group N (Group C, 7 [3–15]; Group N, 0 [0–0.5]; p < 0.001, Table 3). The number of patients who experienced one or more hypotensive episodes during surgery was also greater in Group C (Group C, 31, 89%; Group N, 8, 25%). Although the times to the first injection of phenylephrine showed no difference, the rescue phenylephrine doses were greater in Group C. However, the two groups demonstrated no difference in the occurrence of hypertension, tachycardia, and bradycardia. Among the nine patients who experienced hypertension in Group N, there was no need to reduce the dose of norepinephrine. Additionally, there were no differences in hypotensive events during the postoperative 1-h period between the two groups.
Linear mixed model showed that the change of the mean blood pressure (MBP) was affected by both the group effect and time effect (all p-values < 0.001, Fig. 2a), which demonstrated that the MBP decreased over time, and the change of the MBP was significantly greater in Group C compared to that in Group N. The interaction of group and time was not significant (p = 0.054). In the analysis of the change in the heart rate (HR) using a linear mixed model, time was the only significant factor identified (p < 0.001, Fig. 2b). In terms of postoperative morbidity and the length of hospital stay, there were no significant differences between the two groups (Table 4 and Supplementary Table 1).
Discussion
We found that infusing norepinephrine under SA with propofol sedation during hip surgery in patients aged ≥ 70 years was effective in decreasing the number of hypotensive episodes per patient and the incidence of hypotension during SA with intravenous propofol infusion.
Lower extremity surgery represents 24% of all interventions among patients aged ≥ 75 years14. Particularly, hip fracture surgery in older patients is reportedly associated with high rates of morbidity and mortality15. Although SA is often preferred to general anesthesia owing to several benefits for patients with hip fracture15,16, hypotension is a relatively frequent complication during SA. SA-induced hypotension is more common in older patients, with a reported incidence of 65–75%17,18. The frequent incidence of hypotension following SA in the older patients is a notable anesthetic concern, as this patient population often has multiple comorbidities and is vulnerable to organ hypoperfusion due to reduced functional reserve19. Hypotension results from the sympathetic blockade after induction of SA, which sequentially decreases systemic vascular resistance and cardiac output (CO)20.
As the degree of hypotension is proportional to the height of the sympathetic nerve block20, it is important to limit the block height to the greatest extent possible. Therefore, in our study, a small amount of bupivacaine (10 mg) with 15 µg of fentanyl was injected intrathecally for SA, and the block height of SA was adjusted to approximately T10 to reduce the risk for hypotension. Nevertheless, hypotensive events occurred in 89% of patients in Group C. Patients undergoing surgery under SA often ask to be sedated during surgery to relieve anxiety, even though there is no surgery-related pain. Agents, such as propofol and dexmedetomidine, are commonly used for sedation during SA. Notably, propofol has been demonstrated to be significantly associated with IOH, likely owing to its vasodilating effect, especially when compared to dexmedetomidine21,22,23. In contrast, Shin et al. highlighted a higher incidence of hypotension in the postanesthetic care unit among patients administered dexmedetomidine, compared to those receiving propofol23. Additionally, the onset and offset times of the sedative effect of dexmedetomidine were longer than those of propofol21. Considering these characteristics, propofol offers certain advantages over dexmedetomidine. However, when administering propofol sedation during SA, it is advisable to minimize the dose of propofol and maintain light sedation24. Although low-dose propofol was injected to maintain light sedation with bispectral index (BIS) between 60 and 80 in our study, the use of propofol may still have contributed to the high incidence of hypotension25.
Several strategies, including intravenous fluid administration and vasopressors, have been considered to prevent the occurrence of hypotension after SA induction. Prophylactic administration of crystalloid before SA is effective at preventing hypotension, at least in some patients26,27. However, it should be considered that the decrease in systemic vascular resistance cannot be prevented by the administration of fluids alone, and that the increase in preload and CO may be insignificant despite the administration of fluids in older individuals. In addition, large amounts of fluid administration can be dangerous in older patients with poor cardiac or pulmonary reserves28. Therefore, it is necessary to restore systemic vascular resistance using vasopressors, such as alpha agonists6. Hence, in our study, intravenous co-hydration with only 300 mL of crystalloid and continuous infusion of norepinephrine were initiated immediately after the completion of intrathecal injection29.
The use of alpha-agonists to treat hypotension associated with SA has been extensively studied in the field of obstetrics. Phenylephrine, a pure alpha1-adrenergic receptor agonist that has no direct effect on HR, showed a beneficial effect during SA for cesarean delivery2,3,4,5. However, phenylephrine is associated with a dose-dependent decrease in the HR and CO30,31. This has stimulated the recent investigation of norepinephrine as an alternative option6,7,8,9,10,11. Norepinephrine acts as an alpha-receptor agonist and exhibits weak beta-receptor agonist activity. Consequently, norepinephrine has a lower tendency to decrease HR, resulting in improved maintenance of CO when compared with phenylephrine in patients undergoing cesarean section11. Nevertheless, caution should be exercised when extrapolating these findings from obstetric patients to older patients, as the former are typically younger and have relatively fewer comorbidities. In our study, which included older patients, Group N showed a significantly lower incidence of hypotension, and there was a trend toward a lower incidence of bradycardia compared to Group C. A previous study also noted a higher tendency of bradycardia without statistical significance when phenylephrine was infused after SA in older patients19. Based on these findings, we cautiously predict that, similar to obstetric patients, norepinephrine will effectively prevent hypotension during SA with propofol sedation, while reducing the occurrence of bradycardia compared to phenylephrine in older patients.
Although more than 100 definitions of hypotension are mentioned in the literature, Salmasi et al. found that there was no advantage to using relative over absolute thresholds32. In addition, pain and presurgical anxiety may cause an overestimation of BP readings in hip fracture patients. Hence, this study defined hypotensive episodes based on absolute thresholds rather than patient-specific baselines. Moreover, a previous study identified that the increased time with MBP < 65 mmHg or any exposure to MBP < 55 mmHg was significantly associated with moderately or highly elevated postoperative risk33. In our study, which used an absolute threshold as the criterion for hypotension, the exposure time to hypotension in Group C would have been longer, which may also have increased postoperative complication risks. However, despite the difference in the incidence of hypotension between the two groups, there was no disparity in postoperative clinical outcomes. The latter could be explained by the immediate treatment of hypotension in our study protocol. Based on these results, we conclude that both prevention and prompt treatment of hypotension are important; however, considering its frequency in older patients, prevention appears to be the more rational approach. Therefore, continuous infusion of norepinephrine should be considered in older patients receiving SA with propofol sedation.
This study had several limitations. First, PVi values were measured during spontaneous breathing. PVi is a measure of the variations in the pulse oximeter waveform over respiratory cycles in non-invasive and continuous manner. When mechanical ventilation is employed, PVi can be considered reliable34. However, PVi clearly showed a significant association with the hemodynamic changes in spontaneous breathing volunteers35. Second, we used a fixed dose of 0.05 µg/kg/min of norepinephrine. Hasanin et al. previously suggested that the optimal dose of norepinephrine infusion for preventing SA-induced hypotension was 0.05 µg/kg/min, and that there was no advantage in using the highest dose of 0.075 µg/kg/min36. However, as the responses of the patients to norepinephrine may vary, clinicians can adjust the dose of norepinephrine based on the individual responses. If the infusion dose of norepinephrine is adjusted based on individual responses, the hemodynamic variables could be more stable than those in this study. Furthermore, there might be concerns regarding tissue ischemia when administering norepinephrine via a peripheral vein in our study protocol. However, a previous study demonstrated that there was no significant morbidity associated with norepinephrine infusion via the peripheral line37. Therefore, our protocol could be safely applied in real clinical settings with minimal concern. Finally, the distribution of patients with and without hip fracture between the two groups was not identical. Given the distinct characteristics of patients with and without hip fracture, the incidence of IOH might have varied between the two groups. However, as statistical analysis revealed no significant difference in the proportion of patients with hip fracture to those without hip fracture, this disparity likely had a minimal impact on the study results.
In conclusion, the present study showed that prophylactic norepinephrine continuous intravenous infusion prevented hypotensive episodes, reduced the occurrence of hypotension and the requirement of fluid, and increased the urine output in older patients undergoing unilateral hip surgery under SA with propofol sedation.
Methods
This single-center, prospective, randomized controlled trial study was performed in a tertiary center in Seoul, Republic of Korea. After receiving approval from the Institutional Review Board of Asan Medical Center (approval date: April 13, 2020), this trial was registered on the Clinical Research Information Service (http://cris.nih.go.kr, KCT0005046, 21/05/2020). Written informed consent was obtained from all patients for participation, and this study was conducted in accordance with the Declaration of Helsinki.
Study population and preparation
All older patients scheduled for unilateral primary hip surgery in the lateral position between 2020 August and 2021 June in the host institution were considered eligible for the study. Among them, we included patients who met the following criteria: (1) American Society of Anesthesiologists physical status class 1–3, and (2) age ≥ 70 years. We excluded patients with uncontrolled hypertension, hyperthyroidism, dementia, or symptomatic coronary disease; hemoglobin levels < 10 g/dL; a previous history of allergy to propofol, fentanyl, or bupivacaine; and those who were contraindicated for SA, including coagulopathy, severe aortic stenosis, severe mitral stenosis, and active infection on the lumbar region. Patients who refused to participate in this study or for whom norepinephrine was contraindicated were also excluded.
All included patients were randomly allocated into Group C (n = 35) and Group N (n = 35). Randomization was conducted using a computer-generated randomization program (https://randomization.com) by the corresponding author. Based on the randomization table, nurses who were not involved in this study were informed about the study drug just before the surgery and prepared it as follows: Group C, normal saline 0.3 mL/kg/h; Group N, norepinephrine (norepinephrine 2 mg [Norpin, Hwa-Seong, Korea] mixed in dextrose 5% in water 198 mL) 0.3 mL/kg/h (0.05 µg/kg/min). Neither the anesthesiologists performing the anesthesia nor the patients were aware of the allocated group.
Preoperative management
The preoperative management was not strictly controlled in this study. However, according to our center's preoperative management protocol for surgical patients, all patients fasted from midnight on the day of surgery. Meanwhile, a maintenance volume of fluid was administered. In patients with hip fracture, pain management was provided during the preoperative period. The patients were instructed to remain at bed rest for stabilization, and if their pain score using numerical rating scale was > 4 points, tramadol hydrochloride 50 mg was administered as a first-line treatment, followed by hydromorphone hydrochloride 1 mg as a secondary treatment. Premedication was not administered to any of the patients preoperatively.
Anesthesia and surgery
After patients arrived in the operating room, standard monitoring, including non-invasive blood pressure, electrocardiography, and pulse oximetry was initiated. Non-invasive blood pressure (NIBP) was measured in the contralateral arm to the surgical site with 2.5-min intervals throughout the surgery, while electrocardiography, and pulse oximetry were monitored continuously. To maintain normovolemia, PVi (Radical-7®, Masimo Corp., Irvine, CA, USA), a dynamic index of fluid responsiveness, was also continuously monitored on ipsilateral arm to the surgical site. Oxygen was supplied at 5–6 L/min via a simple facemask.
An intravenous peripheral line was accessed at the ipsilateral hand or forearm, and the patients were positioned into their lateral decubitus position. The standard practice was to position patients in a lateral decubitus position with the surgical site downward. However, if the patients expressed discomfort regarding the position, they were placed in a lateral decubitus position with the surgical site upward. SA was performed with hyperbaric bupivacaine 10 mg and fentanyl 15 µg, using 25-gauge needle after skin disinfection. Then, the patients were returned to the supine position, and the insertion of the foley catheter was performed. Intravenous co-hydration with 300 mL of crystalloid was initiated immediately after completion of the intrathecal injection. The success and level of SA was examined on both the left and right sides at 5 min after the intrathecal injection. As all surgeries were conducted in the lateral decubitus position, patients were positioned laterally with the surgical site facing upward. Norepinephrine or normal saline and propofol were connected, and the continuous infusion of norepinephrine or normal saline was initiated through the inserted peripheral line. Propofol was also infused using a target-controlled infusion system (effect-site concentration 1.0–1.5 µg/mL), and was adjusted to maintain a BIS between 60 and 80 and modified observer’s alertness/sedation scale of 3 (responds only after name is called loudly and/or repeatedly). The intraoperative volume status was monitored using PVi values. Considering that the patients were spontaneously breathing and referencing the results of a previous study, fluid was administered to maintain PVi < 19%35. Infusion of propofol and norepinephrine was immediately stopped once all surgical procedures were finished.
Definition of hemodynamic events and management
Hypotension was defined as MBP < 65 mmHg. When a hypotensive event occurred, phenylephrine 100 µg was injected intravenously as a rescue drug, regardless of the group. Measurements of NIBP were performed until 1 h postoperatively, during which time phenylephrine 100 µg was also administered in case of hypotension. Hypertension was defined as systolic blood pressure (SBP) > 160 mmHg, or an increase in MBP > 20% from the baseline value. Baseline MBP (MBPBL) was defined as the average of three NIBP values measured in the general ward or emergency room the day before surgery when the patient was in a stable condition. If a hypertensive event occurred, continuous infusion of the study drug was discontinued, and nicardipine 5 µg/kg was injected when the SBP was > 160 mmHg. After the return of MBP within the normal range (80% of MBPBL < MBP < 120% of the MBPBL), continuous infusion of the study drug was restarted. When hypertensive events occurred twice, the infusion rate of the study drug was reduced by half. In cases of tachycardia (HR > 120 beats/min) and bradycardia (HR < 50 beats/min), esmolol 0.5 mg/kg and atropine 0.5 mg were administered, respectively.
Outcome measures and data collections
The primary outcome of this study was the number of hypotensive episodes that occurred during surgery. The secondary outcomes were other hemodynamic events during surgery and postoperative complications during the hospitalization. Postoperative complications included cardiovascular complications (i.e., acute coronary syndrome, congestive heart failure, hypotension, and arrhythmia), neurologic complications (i.e., transient ischemic accident and cerebrovascular accident), respiratory complications (i.e., pneumonia, pulmonary edema, pleural effusion, and desaturation), delirium, renal dysfunction (i.e., acute kidney injury based on Kidney Disease: Improving Global Outcomes criteria), and other complications.
Statistical analysis
No prior study has clearly identified hypotensive episodes in older patients undergoing SAwith propofol sedation. Therefore, we determined the sample size using Poisson means. The Poisson means were derived from the retrospective review of our clinical experiences. There were 4.75 hypotensive episodes during a single surgery in older patients who underwent hip surgery under SA with propofol sedation without any continuous infusion of vasopressor, whereas there were 1.67 hypotensive episodes with the continuous infusion of norepinephrine. However, as we had only limited experience on the preventive use of norepinephrine, to ensure a sufficient number of patients, we assumed a Poisson mean of double that of 1.67, which is 3.34, for the treatment group. The calculated sample size, with α = 0.05 and power = 80% using a two-sample and two-sided equality test, was 32 patients in each group. Therefore, after considering possible dropouts, we decided to assign 35 patients into each group.
The Poisson test was used to analyze the number of hypotensive episodes. Other continuous variables were analyzed using Student’s t-test or Wilcoxon rank-sum test as appropriate, and categorical variables were compared using Fisher’s exact test. In addition, the linear mixed model was applied to evaluate the longitudinal changes of MBP and HR. In the model, we tested group and time effects and interactions of group and time. All analyses were performed using SAS®, version 9.4 (SAS Institute Inc., Cary, NC, USA) was used. A p-value < 0.05 was considered statistically significant.
Data availability
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
References
Carpenter, R. L., Caplan, R. A., Brown, D. L., Stephenson, C. & Wu, R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology 76, 906–916 (1992).
Ngan Kee, W. D. & Khaw, K. S. Vasopressors in obstetrics: what should we be using?. Curr. Opin. Anaesthesiol. 19, 238–243 (2006).
Ngan Kee, W. D., Khaw, K. S. & Ng, F. F. Prevention of hypotension during spinal anesthesia for cesarean delivery: An effective technique using combination phenylephrine infusion and crystalloid cohydration. Anesthesiology 103, 744–750 (2005).
Xu, C. et al. Phenylephrine vs ephedrine in cesarean delivery under spinal anesthesia: A systematic literature review and meta-analysis. Int. J. Surg. 60, 48–59 (2018).
Lee, J. E., George, R. B. & Habib, A. S. Spinal-induced hypotension: Incidence, mechanisms, prophylaxis, and management: summarizing 20 years of research. Best Pract. Res. Clin. Anaesthesiol. 31, 57–68 (2017).
Ferre, F. et al. Control of spinal anesthesia-induced hypotension in adults. Local Reg. Anesth. 13, 39–46 (2020).
Hasanin, A. M. et al. Norepinephrine infusion for preventing postspinal anesthesia hypotension during cesarean delivery: A randomized dose-finding trial. Anesthesiology 130, 55–62 (2019).
Ngan Kee, W. D. Norepinephrine for maintaining blood pressure during spinal anaesthesia for caesarean section: A 12-month review of individual use. Int. J. Obstet. Anesth. 30, 73–74 (2017).
Ngan Kee, W. D., Lee, S. W. Y., Ng, F. F. & Khaw, K. S. Prophylactic norepinephrine infusion for preventing hypotension during spinal anesthesia for cesarean delivery. Anesth. Analg. 126, 1989–1994 (2018).
Onwochei, D. N. et al. Norepinephrine intermittent intravenous boluses to prevent hypotension during spinal anesthesia for cesarean delivery: A sequential allocation dose-finding study. Anesth. Analg. 125, 212–218 (2017).
Sharkey, A. M. et al. Comparison of intermittent intravenous boluses of phenylephrine and norepinephrine to prevent and treat spinal-induced hypotension in cesarean deliveries: Randomized controlled trial. Anesth. Analg. 129, 1312–1318 (2019).
Liang, T., Yu, J., Li, L., Xie, Y. & Wu, F. Prophylactic norepinephrine infusion reduces postoperative complications and hospitalization time in elderly patients undergoing posterior lumbar spinal fusion. Biomed. Res. Int. 2021, 2161036 (2021).
Mostafa, M. et al. Hemodynamic effects of norepinephrine versus phenylephrine infusion for prophylaxis against spinal anesthesia-induced hypotension in the elderly population undergoing hip fracture surgery: A randomized controlled trial. Korean J. Anesthesiol. 74, 308–316 (2021).
Auroy, Y. et al. Anesthetics according to characteristics of patients, establishments and indications. Ann. Fr. Anesth. Reanim. 17, 1311–1316 (1998).
Urwin, S. C., Parker, M. J. & Griffiths, R. General versus regional anaesthesia for hip fracture surgery: A meta-analysis of randomized trials. Br. J. Anaesth. 84, 450–455 (2000).
Radcliff, T. A. et al. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J. Bone Joint Surg. Am. 90, 34–42 (2008).
Meyhoff, C. S., Haarmark, C., Kanters, J. K. & Rasmussen, L. S. Is it possible to predict hypotension during onset of spinal anesthesia in elderly patients?. J. Clin. Anesth. 21, 23–29 (2009).
Nishikawa, K., Yamakage, M., Omote, K. & Namiki, A. Prophylactic IM small-dose phenylephrine blunts spinal anesthesia-induced hypotensive response during surgical repair of hip fracture in the elderly. Anesth. Analg. 95, 751–756 (2002).
Ferré, F. et al. Prophylactic phenylephrine infusion for the prevention of hypotension after spinal anesthesia in the elderly: A randomized controlled clinical trial. J. Clin. Anesth. 35, 99–106 (2016).
Hartmann, B. et al. The incidence and risk factors for hypotension after spinal anesthesia induction: An analysis with automated data collection. Anesth. Analg. 94, 1521–1529 (2002).
Shah, P. J., Dubey, K. P., Sahare, K. K. & Agrawal, A. Intravenous dexmedetomidine versus propofol for intraoperative moderate sedation during spinal anesthesia: A comparative study. J. Anaesthesiol. Clin. Pharmacol. 32, 245–249 (2016).
Joe, H. B., Chae, Y. J., Song, S. H. & Yi, I. K. Comparison of the effects of dexmedetomidine and propofol on the cardiovascular autonomic nervous system during spinal anesthesia: Preliminary randomized controlled observational study. J. Clin. Monit. Comput. 37, 1541–1551 (2023).
Shin, H.-J. et al. Postoperative delirium after dexmedetomidine versus propofol sedation in healthy older adults undergoing orthopedic lower limb surgery with spinal anesthesia: A randomized controlled trial. Anesthesiology 138, 164–171 (2023).
Sieber, F. E. et al. Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin. Proc. 85, 18–26 (2010).
Marik, P. E. Propofol: Therapeutic indications and side-effects. Curr. Pharm. Des. 10, 3639–3649 (2004).
Ueyama, H., He, Y. L., Tanigami, H., Mashimo, T. & Yoshiya, I. Effects of crystalloid and colloid preload on blood volume in the parturient undergoing spinal anesthesia for elective cesarean section. Anesthesiology 91, 1571–1576 (1999).
Teoh, W. H. & Sia, A. T. Colloid preload versus coload for spinal anesthesia for cesarean delivery: The effects on maternal cardiac output. Anesth. Analg. 108, 1592–1598 (2009).
Buggy, D. J. et al. Prevention of spinal anaesthesia-induced hypotension in the elderly: i.m. methoxamine or combined hetastarch and crystalloid. Br. J. Anaesth. 80, 199–203 (1998).
Priebe, H. J. The aged cardiovascular risk patient. Br J Anaesth 85, 763–778 (2000).
Dyer, R. A. et al. Hemodynamic effects of ephedrine, phenylephrine, and the coadministration of phenylephrine with oxytocin during spinal anesthesia for elective cesarean delivery. Anesthesiology 111, 753–765 (2009).
Stewart, A. et al. The dose-dependent effects of phenylephrine for elective cesarean delivery under spinal anesthesia. Anesth. Analg. 111, 1230–1237 (2010).
Salmasi, V. et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: A retrospective cohort analysis. Anesthesiology 126, 47–65 (2017).
Wesselink, E. M., Kappen, T. H., Torn, H. M., Slooter, A. J. C. & van Klei, W. A. Intraoperative hypotension and the risk of postoperative adverse outcomes: A systematic review. Br. J. Anaesth 121, 706–721 (2018).
Liu, T., Xu, C., Wang, M., Niu, Z. & Qi, D. Reliability of pleth variability index in predicting preload responsiveness of mechanically ventilated patients under various conditions: A systematic review and meta-analysis. BMC Anesthesiol. 19, 67 (2019).
Keller, G., Cassar, E., Desebbe, O., Lehot, J. J. & Cannesson, M. Ability of pleth variability index to detect hemodynamic changes induced by passive leg raising in spontaneously breathing volunteers. Crit. Care 12, R37 (2008).
Fu, F. et al. A randomised double-blind dose-response study of weight-adjusted infusions of norepinephrine for preventing hypotension during combined spinal-epidural anaesthesia for caesarean delivery. Br. J. Anaesth 124, e108–e114 (2020).
Medlej, K. et al. Complications from administration of vasopressors through peripheral venous catheters: An observational study. J. Emerg. Med. 54, 47–53 (2018).
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
H.K. and H.J.K. conceived and designed the study. S.L. collected clinical samples and data. H.K., W.U.K., J.C., S.W.P., K.S.K., and H.J.K. analyzed the data and contributed to data interpretation. H.K. and H.J.K. wrote the first draft of the manuscript. H.K., W.U.K., Y.J.R., and H.J.K. reviewed the manuscript. All authors approved the final manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H., Lee, S., Koh, W.U. et al. Norepinephrine prevents hypotension in older patients under spinal anesthesia with intravenous propofol sedation: a randomized controlled trial. Sci Rep 13, 21009 (2023). https://doi.org/10.1038/s41598-023-48178-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48178-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.