Abstract
Evidence on the influence of patient characteristics on HbA1c treatment response for add-on medications in patients with type 2 diabetes (T2D) is unclear. This study aims to investigate the predictors of HbA1c treatment response for three add-on medications (sulfonylureas (SU), dipeptidyl peptidase-4 (DPP-4) and sodium–glucose cotransporter-2 (SGLT-2) inhibitor) in metformin monotherapy treated patients with T2D. This retrospective cohort study was conducted using the electronic health record data from six primary care clinics in Singapore. A total of 9748 adult patients with T2D on metformin monotherapy receiving SU, DPP-4 or SGLT-2 add-on were 1:1 propensity score matched to patients receiving other add-on medications. Patient demographics, laboratory results, diabetes related complications, comedications, and treatment response at two endpoints (HbA1c reduction ≥ 1% at 6th month, HbA1c goal attainment < 7% at 12th month) were examined. Multiple logistic regression analyses were used to identify patient characteristics associated with the treatment responses. After matching, there were 1073, 517, and 290 paired cohorts of SU, DPP-4 and SGLT-2 respectively. Besides baseline HbA1c, patients with longer hypertension disease duration and higher cholesterol HDL were associated with better treatment response to SU medication add-on. Lower estimated glomerular filtration rate (eGFR), and angiotensin-II receptor medications were associated with better treatment response to DPP-4 add-on. Lower cholesterol HDL, higher creatinine serum, absence of renal complications and beta-blockers medications were associated with better treatment response to SGLT-2 add-on. The cholesterol HDL, creatinine serum, eGFR, hypertension disease duration, angiotensin-II receptors and beta-blockers class of medications can influence the HbA1c treatment response for SU, DPP-4 and SGLT-2 add-on medications. Knowing the patients’ characteristics that influence treatment response can assist in guiding clinical decisions when selecting the appropriate add-on medication, ultimately helping to prevent the development of diabetes-related complications.
Similar content being viewed by others
Introduction
Type 2 diabetes (T2D) is a progressive disease characterized by elevated levels of blood glucose and the need to gradually intensify therapy due to deficiency in insulin secretion and/or insulin resistance1. Patients with T2D are at high risk of multiple comorbidities, including obesity, hyperlipidaemia, hypertension and kidney disease2. Proper glycaemic control is essential to prevent vascular complications3. Metformin is the first-line therapy recommended to most patients given its long-term safety profile, availability, and low cost4, 5. However, metformin monotherapy can maintain an optimal glycaemic control only for a short term6. Previous studies suggest that as the disease progresses, metformin monotherapy may fail to control blood glucose due to increased insulin resistance and other metabolic events7, 8. Patients who fail to response to monotherapy often require an intensified treatment such as combination therapy to achieve adequate glycaemic control.
With newer oral medications, combinations of different medications may help to further improve glycaemic control9. Sulfonylureas (SU), dipeptidyl peptidase-4 inhibitors (DPP-4), and sodium glucose cotransporter 2 (SGLT-2) inhibitors are popular add-on medication options to metformin10. Each class of medications differs in their mechanisms of action, side effects, cost, risk and benefit profiles. For instance, DPP-4 have a lower risk of hypoglycaemia while SGLT-2 confers cardiorenal benefits and are associated weight loss11, 12.
For patients who require an add-on medication to metformin, the choice of add-on medication is often not obvious. The American and European guidelines on T2D management suggest tailoring the choice of the add-on medication based on individual demographics and clinical profile such as degree of hyperglycaemia, cardiovascular risk, renal function, and other comorbidities13, 14. While numerous clinical trials and observational studies have examined the efficacies of various antidiabetic medications in lowering HbA1c levels alongside with weight gain, risk of hypoglycaemia and major adverse cardiovascular events, few studies have investigated how patient characteristics such as demographics, laboratory results, concomitant comorbidities, and comedications are associated with treatment response to add-on medications in a metformin therapy treated population15,16,17. Furthermore, clinical trials that examined patient characteristics associated with add-on medication treatment response were mostly conducted on Western population and/or otherwise, limited by the small study number. Treatment response to an add-on medication may be influenced by ethnicity with underlying factors such as genetic constitution, lifestyle and living environment. Hence, findings from these studies may not generalize to other populations due to biological and ethnic differences.
This study examines the predictors that determine patient response to three add-on medications (SU, DPP-4 and SGLT-2) in a metformin monotherapy multi-ethnic Asian population. Knowing the significant predictors that influence treatment response can assist in guiding clinical decisions when selecting the appropriate add-on medication, ultimately helping to prevent the development of diabetes-related complications.
Methods
Settings and study population
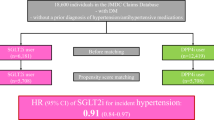
This retrospective cohort study was conducted using electronic health record (EHR) data obtained from six primary care clinics in Singapore. Ethics approval for this study was obtained from Institutional Review Board (IRB) of SingHealth (Reference Number: 2019/2604). The need for informed consent was waived by the ethics committee of SingHealth as the analysis was conducted on de-identified data. All methods were performed in accordance with relevant guidelines and regulations. As in previous study18, the study cohort comprises multi-ethnic Asians adult patients, aged ≥ 21 years, having T2D, hypertension (HTN) and/or hyperlipidaemia (HLD). Patient demographics, disease history, laboratory test results and medications prescriptions were extracted over a 10-year period from 1 January 2010 to 31 December 2019. Baseline was defined as the patient’s most recent EHR record prior to receiving an add-on medication for SU, DPP-4 and SGLT-2 after 1 January 2010. Patients were on metformin monotherapy if they were prescribed with metformin alone at baseline. Patients included in this study were (1) on metformin monotherapy at baseline, (2) have at least two HbA1c measurements within one year, and (3) were initiated only one add-on medication of either SU, DPP-4 or SGLT-2. Patients (n = 58) with extreme values (beyond 4 standard deviations) in clinical measurements were excluded from analysis. In total, the study cohort consisted of 9748 patients. (See Fig. 1 Flowchart of study population).
Flowchart of study population. 1Other refers to patients receiving alpha-glucosidase inhibitors or insulin add-on medications. Patients initiated with a medication add-on were matched 1:1 using a greedy nearest neighbour process without replacement, within a calliper distance of 0.2 SD of the logit of the propensity score to patients initiated with another type of add-on medication.
Patient variables
Demographic and clinical variables including age, sex, ethnicity, and BMI were obtained at baseline. Clinical variables consisted of blood pressure, comorbidities of HLD and HTN, duration of the three diseases diabetes, HTN and HLD, laboratory test results of HbA1c, cholesterol, triglycerides (TG), creatinine serum, potassium serum and alanine transaminase (ALT) serum; and estimated glomerular filtration rate (eGFR) calculated using Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation19. We also included complications involving macrovascular, renal, eye and foot based on a pre-defined set ICD-10 codes, medications and patient referrals in Supplement Table S1 and Text S1. Finally, we considered the dose intensity of metformin and medications for HLD and HTN in our study. The total daily dose (TDS) of metformin is categorized into three intensity levels: low (L) for doses up to 1000 mg, moderate (M) for doses over 1000 mg but up to 2000 mg, and high (H) for doses exceeding 2000 mg. Medications for HLD and HTN were grouped by their classes. For example, losartan or valsartan belong to the medication class angiotensin-II-receptor. The list of medication classes can be found in Supplement Table S2.
Outcome
The therapeutic efficacy of the add-on medications were evaluated based on two treatment responses of patients. The first response is whether they achieve a reduction in HbA1c of at least 1% at the 6-month mark compared to baseline. The second response is whether they reach the HbA1c goal of less than 7% at the 12-month mark. The 6-month HbA1c reduction is considered a measure of short-term efficacy, while the 12-month HbA1c attainment reflects long-term efficacy. Clinical investigation guidelines for T2D medicinal products recommend a minimum duration of 16 weeks for add-on medication to achieve its maximum effect and for HbA1c levels to stabilize20. Clinical practice guideline on diabetes recommend HbA1c testing every 6–12 months for patients with stable glycaemic control21. In addition to the two treatment responses, we have conducted an additional analysis using a more modest outcome: HbA1c reduction of > 0.5% at the 6-month point. This supplementary criterion is to account for the differing potencies of various medications, thereby enhancing the comprehensiveness of our assessment on the shorter-term treatment response.
Statistical analysis
To reduce data irregularities caused by variations in patients' visit schedules, such as delayed appointments or irregular testing, we employed interpolation techniques to generate monthly HbA1c measurements22. In cases where a month had multiple HbA1c values, the average of all values were used. The monthly data points provide a more consistent and granular dataset for analysis. Missing data on all other variables in the baseline EHR were imputed using the Multiple Imputation by Chained Equation (MICE)23. See Supplement Table S3 for the percentage of missing data in the variables. Propensity score analysis was conducted to balance covariates, including age, sex, ethnicity, BMI, diabetes duration, and baseline metformin TDS, between patient groups (i.e., SU add-on versus non-SU add-on, DPP-4 add-on versus non-DPP-4 add-on, and SGLT-2 add-on versus non-SGLT-2 add-on) at baseline. The propensity score was calculated as the predicted probability of receiving an add-on medication using a multivariable logistic regression model. The variables used for matching included age, gender, ethnicity, BMI, diabetes duration and baseline metformin TDS. Matching was performed for each type of add-on medications with the use of a 1:1 greedy nearest neighbor process without replacement, within a calliper distance of 0.2 SD of the logit of the propensity score24. The choice of 1:1 matching was made to enable a direct comparison of outcomes between the two groups (i.e., patients initiated with SU and non-SU medication add-on groups) and to provide straightforward and interpretable results25. Univariate analyses were used to identify variables associated with the two treatment outcomes. Variables that were found to be significant at p-value < 0.05 were selected for multivariable logistic regression analysis. All variables were normalized to a mean of 0 and a standard deviation of 1. Goodness of fit for all multivariable logistic regression model were evaluated using concordance statistic (C statistics). Multicollinearity among variables was assessed using Variance Inflation Factor (VIF). Variables with VIF > 10 were excluded from multivariate regression models. The odds ratios and 95% confidence interval (CI) for all variables on the two treatment outcomes were reported. All the analysis was performed using Python version 3.8.8, psmpy 0.3.13, tableone 0.7.12 and statmodel 0.12.2 libraries.
Ethical approval
Ethics approval was obtained from SingHealth Centralized Institution Review Board (CIRB) in 2019 (SingHealth CIRB Reference: 2019/2604). Patient consent was not obtained as the analysis was conducted on de-identified data.
Results
Characteristics of the study population
Before matching, the average age of patients was 60.8 years (± 10.6), with 50.7% being male. Over a 10-year period, each patient had an average of 27.8 (± 9.4) HbA1c measurements, with an average time interval of 3.9 months (± 2.2) between visits. At baseline, 88.6% of patients were initiated on a SU add-on, 5.3% on a DPP-4 add-on, and 3.0% on an SGLT-2 add-on. After matching, the analysis included 1,073 patients initiated with SU, 517 patients with DPP-4, and 290 patients with SGLT-2 add-on therapy. The baseline characteristics of the matched pairs are summarized in Table 1, and the distribution of propensity scores for the three add-on medications is illustrated in Supplement Fig. S1.
Patients who received SU add-on medication had a mean age of 60.9 (± 10.5) years, with 44.9% being male. In the matched cohort, patients had longer diabetes disease duration compared to the unmatched cohort. Among those who received SU add-on, 88.3% were on HMG-CoA reductase inhibitors class of medications and over a third had eye complications. Patients who received DPP-4 add-on were slightly older, have a lower BMI and over 40% of them were on ACE inhibitors and angiotensin-II receptor class of medications. 42.7% and 38.9% of patients who received DPP-4 add-on also have foot and renal complications. Patients who received SGLT-2 add-on have lower baseline HbA1c, better renal function with lower creatinine serum, higher eGFR and fewer renal complications at baseline compared to patients who received other add-on medication. Similar to those on SU add-on medication, over 80% of patients who received SGLT-2 add-on were on HMG-CoA reductase inhibitors class of medications and around 40% were on angiotensin-II receptor and calcium antagonists’ class of medications.
Univariate analysis
In the univariate analysis, for SU add-on, the baseline HbA1c and disease duration of HTN were found to be significant factors for both HbA1c reduction and HbA1c goal attainment. Additionally, variables such as age, disease duration of DM and HLD, cholesterol HDL, LDL and TG, eGFR, creatinine, potassium and ALT serum, number of HTN medications, and calcium antagonist medications class were associated with HbA1c goal attainment but not with HbA1c reduction. In the case of DPP-4 add-on medication, most variables appeared insignificant except baseline HbA1c, cholesterol LDL and number of HLD medications. Variables such as age, BMI, disease duration of HLD and HTN, creatinine serum, eGFR, number of HTN medications, and HTN medication class of angiotensin-II receptor and other lipid-lowering medications (i.e. ezetimibe, cholestyramine) were associated with HbA1c goal attainment but not with HbA1c reduction. For SGLT-2 add-on medication, baseline HbA1c, diastolic blood pressure and cholesterol HDL were associated with HbA1c reduction. While baseline HbA1c, creatinine serum, existing renal complications, and HTN medications of beta blockers were associated with HbA1c goal attainment. All results of the univariate analysis can be found in Supplement Table S5–S7. The findings on the supplementary criterion HbA1c reduction of > 0.5% at 6-month point were detailed in Supplemental materials—Text S2 and Fig. S2.
Multivariate analysis
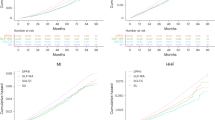
In the multivariate analysis, patient variables associated with treatment response for SU add-on are shown in Fig. 2A,B. Higher HbA1c and longer HTN disease duration were independently associated with increased odds of HbA1c reduction. Lower baseline HbA1c, longer HTN duration, higher cholesterol HDL and HTN medication class calcium antagonists were independently associated with increased odds of HbA1c goal attainment. The effect estimates and 95%CI for all variables at the 6th and 12th months can be found in Supplement Tables S8–S9. The C-statistics for HbA1c reduction and HbA1c goal attainment are provided in Supplement Fig. S3A,B. Figure 2C,D shows the patient variables associated with treatment response for DPP-4 add-on. Only higher baseline HbA1c were associated with increased odds of HbA1c reduction; while patients with lower baseline HbA1c, lower eGFR and having HTN medication class angiotensin-II receptor were more likely to achieve HbA1c goal attainment at 12th month.
Patient variables associated with treatment response for add-on medication. (A) For SU add-on, HbA1c reduction ≥ 1% measured at 6th month. (B) For SU add-on, HbA1c goal attainment < 7% measured at 12th month. (C) For DPP-4 add-on, HbA1c reduction ≥ 1% measured at 6th month. (D) For DPP-4 add-on, HbA1c goal attainment < 7% measured at 12th month. (E) For SGLT-2 add-on, HbA1c reduction ≥ 1% measured at 6th month. (F) For SGLT-2 add-on, HbA1c goal attainment < 7% measured at 12th month. Column in right indicates odds ratio and its 95% confidence interval (CI) in brackets. Black box represents the odds ratio, and the horizontal line represents the 95%CI. Dotted vertical indicates line of null effect. All models were adjusted for age, sex, race, BMI, disease duration of diabetes and baseline metformin total daily dose.
Lastly, Fig. 2E, Fshows the patient variables associated with treatment response for SGLT-2 add-on. Higher HbA1c, lower cholesterol HDL at baseline were associated with increased odds of HbA1c reduction and higher creatinine serum, absence of renal complications and HTN medication class of beta blockers were associated with increased odds of HbA1c goal attainment.
Discussion
In this retrospective study of metformin monotherapy treated Asian population, baseline HbA1c, HTN disease duration, cholesterol HDL, creatinine serum, eGFR, existing renal complications, and HTN medication class of calcium antagonists, angiotensin-II receptor and beta blockers were independently associated with HbA1c outcome and were predictive of treatment response for SU, DPP-4 and SGLT-2 add-on medications.
Consistent with the previous studies26,27,28, our regression models demonstrated that baseline HbA1c was a significant predictor of treatment response for all three add-on medications. Patients with higher baseline HbA1c were more likely to achieve a reduction of ≥ 1% in HbA1c levels at the 6th-month mark after initiating add-on medication. These findings aligned with studies investigating the use of SU, DPP-4 and SGLT-2 as add-on for patients on metformin monotherapy17, 27. In our study, baseline HbA1c were observed to be inversely associated with HbA1c goal attainment. This suggest that patients with higher baseline HbA1c were less likely to achieve HbA1c of < 7% at 12th month after second medication was added.
BMI showed a moderate association (p-value < 0.10) with HbA1c treatment response for SU and DPP-4 add-on medications in the univariate analysis. When considering other factors, BMI maintained a moderate association (p-value < 0.08) with HbA1c goal attainment specifically for DPP-4 add-on medications. The finding suggests that for every unit of decrease in BMI, there was approximately 96% (1/odd ratio of 0.51) increase in odds of patient achieving HbA1c goal attainment. Our finding on BMI concurred with the TriMaster clinical trial on DPP-4 and SGLT-2 as second- or third-line therapy among T2D patients on metformin monotherapy or metformin and SU therapy. The study found patients with BMI ≤ 30 kg/m2 achieved greater reduction in HbA1c when treated with DPP-4 add-on medication compared to those with BMI > 30 kg/m229.
For DPP-4 add-on, we observed that patients with lower eGFR had a higher likelihood of achieving HbA1c goal attainment. Limited studies have compared HbA1c treatment response among patients with varying degrees of renal impairment. However, a study conducted on 1101 Asian patients with T2D and mild impaired renal function concluded that DPP-4, when used alone or in combination with other glucose-lowering medications, provides protection against the decline in renal function30. This finding was further supported by a clinical review that suggest DPP-4 medications were safe and well tolerated in T2D patients with renal impairment11.
For SGLT-2 add-on, eGFR was not significantly associated with treatment response in our multivariable model. Instead, we found patients without renal complications at baseline were more likely to achieve an HbA1c goal attainment of < 7%, compared to patients with existing renal complications. The reduced glucose filtration and resulting modest glycosuria with SGLT-2 therapy among patients with impaired renal function may explain the attenuated glucose-lowering efficacy compared to patients without established renal impairment31, 32. The TriMaster study supported our findings, showing that lower eGFR was associated with a reduced glucose-lowering response to SGLT-2 inhibitors29. Nevertheless, previous clinical studies have provided evidence that SGLT-2 inhibitors can delay the progression of chronic kidney disease (CKD) and can be administered to patients with heart failure or CKD, or at risk for adverse cardiac or renal pathologies12. In this study, we observed that patients with higher serum creatinine levels were more likely to achieve their HbA1c goal than patients with lower serum creatinine levels at baseline. Preliminary findings showed that patients initiated with SGLT-2 add-on medications had lower baseline serum creatinine levels (67.2 ± 16.5) compared to patients using other add-on medications, such as SU (72.8 ± 18.3) and DPP-4 (72.5 ± 19.6). Hence, we caution that the findings related to serum creatinine may not be generalized beyond the range defined by the characteristics of the patients in this dataset.
In our multivariable models, variables such as cholesterol HDL and disease duration of HTN were predictive of HbA1c treatment response. However, previous studies have shown mixed results regarding the predictive value of these variables. A systematic review33 on the clinical predictors of treatment response to metformin and SU found that blood pressure, cholesterol, triglycerides, and macrovascular complications influenced the response to add-on medications; whereas the study conducted on an Asian population with T2D34 concluded that blood pressure, cholesterol, and comorbidities were not significant predictors. We reasoned that these discrepancies may be attributed the underlying differences in the sample size, study population, medication initiated and other factors such as diet and lifestyle.
The current study also found potential associations between several HTN medication classes, such as beta blockers, calcium antagonists and angiotensin-II receptor blockers, and HbA1c treatment response, indicating a possible link between HTN medications and HbA1c response. Another study suggested that certain HTN medication classes, like channel blockers, provide protection against hypoglycaemia when used with insulin secretagogues like SU35. However, further detailed analysis is required to better understand the mechanism and establish a more conclusive link between HTN medications and add-on medication treatment response.
The study has several strengths that contribute to its robustness and generalizability. Firstly, this study draws data from primary care clinics in Singapore that serve large and diverse patient populations. Patients comprise of individuals representative of the community, including individuals of different ages, ethnic groups, socioeconomic backgrounds, and health conditions. Secondly, the use of data from multiple clinics also reduces the risk of selection bias, which can occur when data is collected from a single site. Thirdly, the large sample size enabled the examination of various factors such as demographics, laboratory results, comorbidities, and medication classes related to HLD and HTN and their impact on HbA1c treatment response.
This study also has several limitations that should be considered. First, majority of T2D patients on metformin monotherapy who visited the polyclinic during the period 2010–2019 were prescribed SU add-on medication. This was because the local committee’s recommendations for dual therapy with DPP-4 and SGLT-2 inhibitors alongside metformin were introduced relatively recently in 2016 and reaffirmed in 2020. Hence, changes in prescription practice will take time to be reflected in EHR records. Second, the list of medications analysed was limited to those included on the institution's approved drug list. Specific medications, such as glibenclamide under SU, were absent in our analysis due to recommendations by the local health authority regarding its use, which is associated with a higher risk of hypoglycaemia compared to other SUs. Third, the choice and dosage of the add-on medication in the EHR were subjected to clinician's judgment, the cost of medications, and the patient's preferences, rather than being based solely on clinical outcomes. To minimize potential bias from baseline differences, propensity score matching was employed in our study. Other factors, such as demographics and the total daily dosage of metformin at baseline that could affect glycaemic response, were controlled by adding potential confounding variables in multivariable models. Fourth, bias may have been introduced by excluding patients with fewer than two HbA1c measurements within one year and those who were prescribed two or more add-on medications concurrently, potentially affecting the generalizability of our study findings. Fifth, our study focused on several a priori known risk factors for T2D and its complications. Additional factors such as diet, lifestyle, genetic risk factors, medication contraindications, and compliance that might influence add-on medication treatment response were not accounted for in the present study. Finally, the polyclinic patients primarily consist of individuals without or with limited private health insurance coverage, as they offer more affordable healthcare options compared to specialized/private facilities. Therefore, the findings of this study may not fully generalize to patients attending specialized facilities. Despite these limitations, this study incorporated real-world data and provides clinicians with evidence to select the optimal choice of add-on medication for better glycaemic control.
Implications for research and practice
Findings from this study can potentially be used to support clinicians in selecting the optimal add-on medication and avoid development of diabetes related complications. A future avenue for our study is to develop a system that recommends an optimal add-on medication following metformin monotherapy. It will be integrated into our existing PERsonalized DIabetes Counselling Tool using Artificial Intelligence to support clinical decision-making in a multi-site trial22, 36.
Conclusions
In this multi-ethnic Asian population with T2D treated with metformin therapy, longer HTN disease duration, lower cholesterol HDL and calcium antagonists medication class were associated with better treatment response to SU medication add-on. Lower eGFR and angiotensin-II receptor medications were associated with better treatment response to DPP-4 add-on. Lower cholesterol HDL, higher creatinine serum, absence of renal complications and beta-blockers medications were associated with better treatment response to SGLT-2 add-on. These findings highlight the importance of considering cholesterol profile, renal function, presence of hypertension comorbidity, and comedications when selecting add-on medications.
Data availability
The datasets analysed in the current study are not publicly available as they contain information that are sensitive to the institution. They may be made available from the corresponding author on reasonable request.
Abbreviations
- AG:
-
Alpha-glucosidase inhibitors
- ALT:
-
Alanine transaminase
- BMI:
-
Body mass index
- CPG:
-
Clinical practice guidelines
- DPP-4 inhibitor:
-
Dipeptidyl peptidase-4 inhibitor
- DHL:
-
Diabetes, hyperlipidaemia and hypertension
- EHR:
-
Electronic health records
- eGFR:
-
Estimated glomerular filtration rate
- HbA1c :
-
Glycated haemoglobin
- HDL:
-
Cholesterol high-density lipoprotein
- HLD:
-
Hyperlipidaemia
- HTN:
-
Hypertension
- ICD:
-
International classification of diseases
- LDL:
-
Cholesterol high-density lipoprotein
- SGLT-2 inhibitor:
-
Sodium–glucose cotransporter-2 inhibitor
- SU:
-
Sulfonylureas
- T2D:
-
Type 2 diabetes
- TDS:
-
Total daily dose
References
Cahn, A. & Cefalu, W. T. Clinical considerations for use of initial combination therapy in type 2 diabetes. Diabetes Care 39, S137–S145. https://doi.org/10.2337/dcS15-3007 (2016).
Saleem, Z. et al. Association of hypertension and dyslipidaemia with increasing obesity in patients with Type 2 Diabetes Mellitus. Braz. J. Pharm. Sci. https://doi.org/10.1590/s2175-97902019000118136 (2019).
Group, U.P.D.S. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). The Lancet 352, 854–865. https://doi.org/10.1016/S0140-6736(98)07037-8 (1998).
Rojas, L. & Gomes, M. Metformin: An old but still the best treatment for type 2 diabetes. Diabetol. Metab. Syndr. https://doi.org/10.1186/1758-5996-5-6 (2013).
Association, A. D. Pharmacologic approaches to glycemic treatment. Diabetes Care 40, S64–S74. https://doi.org/10.2337/dc17-S011 (2017).
Turner, R., Cull, C. & Frighi, V. Holman RRGroup for the UKPDS (UKPDS). Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitusprogressive requirement for multiple therapies (UKPDS 49). JAMA 281, 2005–2012. https://doi.org/10.1001/jama.281.21.2005 (1999).
Scheen, A. Pathophysiology of type 2 diabetes. Acta Clin. Belg. 58, 335–341. https://doi.org/10.1179/acb.2003.58.6.001 (2003).
Group, U. UK Prospective Diabetes Study 33 Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 352, 837–853. https://doi.org/10.1016/S0140-6736(98)07019-6 (1998).
Florence, J. A. & Yeager, B. F. Treatment of type 2 diabetes mellitus. Am. Fam. Physician 59(2835–2844), 2849–2850 (1999).
Wyncott, D., Lyon, C., Mounsey, A. & Stevermer, J. J. PURLs: Need an add-on to metformin? Consider this. J. Family Pract. 66, 42–44 (2017).
Gallwitz, B. Clinical use of DPP-4 inhibitors. Front. Endocrinol. (Lausanne) https://doi.org/10.3389/fendo.2019.00389 (2019).
Salvatore, T. et al. An overview of the cardiorenal protective mechanisms of SGLT2 inhibitors. Int. J. Mol. Sci. 23, 3651. https://doi.org/10.3390/ijms23073651 (2022).
Health, N. I. f. & Excellence, C. Type 2 Diabetes in Adults: Management. NICE Guideline. https://www.nice.org.uk/guidance/ng28 (2015).
Bahar, A. Pharmacologic approaches to glycemic treatment. Diabetes Care 40, S64–S74. https://doi.org/10.2337/dc17-S011 (2017).
Hougen, I. et al. Safety of add-on sulfonylurea therapy in patients with type 2 diabetes using metformin: A population-based real-world study. BMJ Open Diabetes Res. Care 9(1), e002352. https://doi.org/10.1136/bmjdrc-2021-002352 (2021).
Cho, Y. Y. & Cho, S.-I. Metformin combined with dipeptidyl peptidase-4 inhibitors or metformin combined with sulfonylureas in patients with type 2 diabetes: A real world analysis of the South Korean national cohort. Metabolism 85, 14–22. https://doi.org/10.1016/j.metabol.2018.03.009 (2018).
Wilding, J. et al. Changes in HbA1c and weight, and treatment persistence, over the 18 months following initiation of second-line therapy in patients with type 2 diabetes: Results from the United Kingdom Clinical Practice Research Datalink. BMC Med. 16, 1–12. https://doi.org/10.1186/s12916-018-1085-8 (2018).
Fang, H. S. A. et al. The effect of oral diabetes medications on glycated haemoglobin (HbA1c) in Asians in primary care: A retrospective cohort real-world data study. BMC Med. 20, 1–12. https://doi.org/10.1186/s12916-021-02221-z (2022).
Levey, A. S., Inker, L. A. & Coresh, J. GFR estimation: From physiology to public health. Am. J. Kidney Dis. 63, 820–834. https://doi.org/10.1053/j.ajkd.2013.12.006 (2014).
Use, C. f. M. P. F. H. Guideline on Clinical Investigation of Medicinal Products in the Treatment or Prevention of Diabetes Mellitus. https://www.ema.europa.eu/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-treatment-prevention-diabetes-mellitus-revision_en-0.pdf (2012).
Goh, S. Y. et al. Ministry of health clinical practice guidelines: Diabetes mellitus. Singap. Med. J. 55, 334. https://doi.org/10.11622/smedj.2014079 (2014).
Tan, W. Y. et al. Diabetes medication recommendation system using patient similarity analytics. Sci. Rep. 12, 20910. https://doi.org/10.1038/s41598-022-24494-x (2022).
Zhang, Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann. Transl. Med. 4, 30. https://doi.org/10.3978/j.issn.2305-5839.2015.12.63 (2016).
Austin, P. C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 46, 399–424. https://doi.org/10.1080/00273171.2011.568786 (2011).
Allan, V. et al. Propensity score matching and inverse probability of treatment weighting to address confounding by indication in comparative effectiveness research of oral anticoagulants. J. Comp. eff. Res. 9, 603–614. https://doi.org/10.2217/cer-2020-0013 (2020).
Malek, M., Aghili, R., Valojerdi, A. E. & Khamseh, M. E. Predictors of glycemic response and change in HbA1c following newly initiated basal insulin among insulin naive adults with type 2 diabetes. Acta Med. Iran. 55, 556–562 (2017).
Strain, W. D. et al. What next after metformin in type 2 diabetes? Selecting the right drug for the right patient. Diabetes Ther. 11, 1381–1395. https://doi.org/10.1007/s13300-020-00834-w (2020).
Lee, J.-Y. et al. Predictors of the therapeutic efficacy and consideration of the best combination therapy of sodium–glucose co-transporter 2 inhibitors. Diabetes Metab. J. 43, 158–173. https://doi.org/10.4093/dmj.2018.0057 (2019).
Shields, B. M. et al. Patient stratification for determining optimal second-line and third-line therapy for type 2 diabetes: The TriMaster study. Nat. Med. 29, 376–383. https://doi.org/10.1038/s41591-022-02120-7 (2023).
Hsu, W.-C., Lin, C.-S., Chen, J.-F. & Chang, C.-M. The effects of dipeptidyl peptidase 4 inhibitors on renal function in patients with type 2 diabetes mellitus. J. Clin. Med. 11, 2653. https://doi.org/10.3390/jcm11092653 (2022).
Thomas, M. C. & Cherney, D. Z. The actions of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia 61, 2098–2107. https://doi.org/10.1007/s00125-018-4669-0 (2018).
Miyoshi, H., Kameda, H., Yamashita, K., Nakamura, A. & Kurihara, Y. Protective effect of sodium–glucose cotransporter 2 inhibitors in patients with rapid renal function decline, stage G3 or G4 chronic kidney disease and type 2 diabetes. J. Diabetes Investig. 10, 1510–1517. https://doi.org/10.1111/jdi.13064 (2019).
Home, P. D. et al. Predictive and explanatory factors of change in HbA1c in a 24-week observational study of 66,726 people with type 2 diabetes starting insulin analogs. Diabetes Care 37, 1237–1245. https://doi.org/10.2337/dc13-2413 (2014).
Martono, D. et al. Predictors of response in initial users of metformin and sulphonylurea derivatives: A systematic review. Diabet. Med. 32, 853–864. https://doi.org/10.1111/dme.12688 (2015).
Nam, Y. H. et al. Association between serious hypoglycemia and calcium-channel blockers used concomitantly with insulin secretagogues. JAMA Netw. Open 4, e2124443–e2124443. https://doi.org/10.1001/jamanetworkopen.2021.24443 (2021).
(IDS), N. I. o. D. S. JARVIS DHL Transforming Chronic Care for Diabetes, Hypertension and hyperLipidemia with AI, https://ids.nus.edu.sg/aiinhealth.html (2019).
Funding
This research is funded by the National Research Foundation, Singapore under its AI Singapore Programme (AISG Award No: AISG-GC-2019-001-2A). Any opinions, findings and conclusions or recommendations expressed in this material are those of the authors and do not reflect the views of National Research Foundation, Singapore.
Author information
Authors and Affiliations
Contributions
W.Y.T., W.H. and M.L.L. conceptualized and formulated the method. W.Y.T. performed the formal data analysis and wrote the original draft. W.H. and M.L.L. supervised, reviewed, and edited the manuscript. N.C.T. reviewed and edited the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tan, W.Y., Hsu, W., Lee, M.L. et al. Predictors of HbA1c treatment response to add-on medication following metformin monotherapy: a population-based cohort study. Sci Rep 13, 20891 (2023). https://doi.org/10.1038/s41598-023-47896-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47896-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.