Abstract
To assess and analyse the knowledge of recommended antibiotic treatments, focusing on the appropriate drugs and treatment durations for the most common community-acquired infections in general medical practice in Occitanie region, France. A web-based survey was conducted over a 3-month period, from October, 2018 to January, 2019. All participants answered directly through the online platform. For the analysis of overtreatment risk, a score based system was adopted and two scores were produced: the duration score and the treatment score. 413 general practitioners completed the survey. The overall rate of concordance with guidelines in terms of both drug choice and treatment length was 2974/4956 (60%) answers. Diseases with at least 70% good answers included cystitis, group A streptococcal pharyngitis, and bacterial superficial skin infections. Diseases with fewer than 50% good answers included pyelonephritis, dog bite wounds, and community-acquired pneumonia in patients aged ≥ 65 years. Factors associated with the risk of overtreatment were age > 40 years, country setting and hospital employment. Knowledge of treatment durations is satisfactory with 60% of recommendations being met. However, varying levels were observed according to different diseases. This study highlighted a very high rate of adherence when recommendations were clear. In contrast, low levels of adherence were observed when recommendations were ambiguous or when conflicting guidelines existed.
Similar content being viewed by others
Introduction
Antibiotic over-prescription is a significant public health issue. Indeed, excessive antibiotic use escalates public expenditure and propels the spread of antibiotic-resistant bacteria1. In terms of public health, it is advisable to reduce the treatment duration to minimize the risk of selecting and proliferating resistant bacteria. Consequently, antibiotic stewardship programs focused on reducing antibiotic treatment durations. In alignment with this objective, the French Society of Infectious Diseases (Societé de Pathologie Infectieuse de Langue Française or SPILF) released guidelines in 2017 specifically aimed at reducing antibiotic treatment durations2. These guidelines were updated in 20213.
Over the past two decades, antibiotic consumption in France has followed a three-phase trend. Between 2000 and 2004, there was a notable decrease of 18.9%, coinciding with the national campaign “Antibiotics are not systematic”. This was followed by a period of stability from 2005 to 2010. However, from 2011 to 2020, there was an increase in antibiotic consumption by 8.6%4. Currently, the rate stands at 32.1 daily defined dose (DDD)/1000 habitants/day in France, compared to the European Union’s 22.4 DDD/1000 habitants/day. A staggering 93% of these prescriptions come from the outpatient sector, with general practitioners (GP) accounting for 71% of them. Primary drivers for antibiotic prescriptions include ear-nose-throat (ENT) infections (42%), lower respiratory tract infections (25%) and urinary tract infections (8%)1. These statistics place France among the top antibiotic consumers in Europe5.
Alterations in antibiotic prescription behaviours and emphasizing the appropriate use of antibiotics are fundamental aspects of antibiotic stewardship programs. The appropriate use of antibiotics refers to conditions that ensure an optimal benefit-to-risk ratio when administering a specific drug to an individual6. In practical terms, this entails a judicious antibiotic prescription, with the appropriate drug, for a set duration, and adhering to a specified dosage regimen. Nonetheless, few studies have assessed the knowledge level concerning the recommended antibiotic treatments in terms of appropriate molecule and treatment duration for community-acquired infections in general practice.
The primary objective of this study was to evaluate and analyse the knowledge level of recommended antibiotic treatments in terms of appropriate drug and treatment duration for the most common community-acquired infections encountered in general practice.
The secondary objectives included:
-
i.
Identifying the conditions most often associated with a treatment duration exceeding guideline recommendations.
-
ii.
Determining the factors associated with extended antibiotic treatment.
Materials and methods
Study design
A web-based survey was conducted over a span of three months, from October 15th, 2018, to January 15th, 2019. GPs and general medicine residents from the Occitanie region in France had free access to the survey on the WebQuest® online platform. The survey was distributed via web mails, scientific journals, and social media. Collaborative entities included: the regional union of health care professionals of Occitanie, the network of general medicine residents from Toulouse-Purpan University’s Medical Faculty, the group of referents in extra-hospital infective surveillance, and the young infectious diseases specialists. To maximize GP participation, the survey was also promoted on social media platforms. All respondents submitted their answers directly through the online platform. Submissions were fully anonymized. The survey in French language is available on reasonable request to the corresponding author. Data from all respondents were analysed without exclusions.
Survey
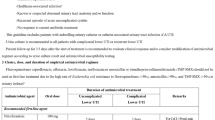
The survey was designed by two infectious diseases specialists, members of the board of the French Society of Infectious Diseases and authors of the French guidelines on antibiotic treatment duration3. The basis for the questionnaire was the study by Cecilia Costa, validated at Marseille University on May 23rd, 20187. The survey was anonymous and structured in two sections : (i) Demographic and professional characteristics of the respondent [including gender, age, setting (urban, rural, or both), and workplace (clinic, hospital medical unit, hospital emergency unit, nursing home, or independent practice)]; (ii) Clinical cases covering 12 distinct conditions: group A streptococcal pharyngitis (GASP), bacterial maxillary sinusitis, bacterial frontal sinusitis, congestive otitis in children, cystitis in women, pyelonephritis in women, urinary tract infections (UTI) in men, bacterial superficial skin infections, dog bite wounds, community-acquired pneumonia (CAP) in patients aged ≥ 65 years, and mild exacerbation of chronic obstructive pulmonary disease (COPD). Respondents were presented with open-ended questions regarding empirical antibiotic treatment and multiple-choice questions on treatment duration. The gold standard for treatment was established using the 2017 French national guidelines endorsed by the SPILF2. Exceptionally, for COPD exacerbation, guidelines from both the SPILF and the French Agency for the Sanitary Safety of Health Products (Agence Française de Sécurité Sanitaire des Produits de Santéor AFSSAPS) were referenced due to their divergent recommendations (antibiotic treatment as per SPILF vs no antibiotic treatment as per AFSSAPS)8.
To analyse the overtreatment risk, a scoring system was implemented, resulting in two scores: the duration score and the treatment score. In practice, answers to the twenty-four questions (twelve on the choice of molecules and twelve on antibiotic treatment duration) submitted by each respondent were analysed. Responses aligning with the durations and/or types of drugs suggested by the national guidelines were deemed correct. For both the duration and treatment scores, a value of 0 points was allocated for each correct answer, while 1 point was allocated for each incorrect answer. The cumulative score was then calculated. Finally, prescribers with a duration or treatment score exceeding the 75th percentile were identified.
Statistical analysis
The required number of participants was calculated based on a standard p-value of 0.05, a precision of 0.05, and an arbitrarily designed expected proportion (p) of physicians in agreement with the measures set at 20%. Using the formula n = 1.962 × p (1–p), the minimal number of physicians necessary to yield a statistically significant outcome was determined to be 245.
Diseases were categorized into three groups based on the percentage of correct answers: (i) diseases with a low level of knowledge (≤ 50% of correct answers); (ii) diseases with a moderate level of knowledge (51–69% of correct answers); (iii) diseases with a high level of knowledge (≥ 70% of correct answers).
For statistical analysis, we used Excel 2016® software and the pvalue.io© website. Descriptive analysis displayed data as either mean values or observed number of events. Student’s t test was used for inferential analysis. The following analysis were performed : (i) descriptive analysis of the characteristics of each practitioner ; (ii) descriptive analysis of the responses to all 12 questions; (iii) comparison between the characteristics of practitioners with a duration score exceeding the 75th percentile and those with a duration score equal to or below the75th percentile; (iv) comparison between the characteristics of practitioners with a treatment score above the 75th percentile and those with a duration score equal to or below the 75th percentile.
Ethical considerations
This study was conducted in accordance with the Declaration of Helsinki, as well as other national and institutional standards9,10. Methodological and ethical considerations received approval from the Medical Department of Pierre and Marie Curie University in Paris, France, on January 25th, 2018. An electronic consent form was signed by each respondent.
Results
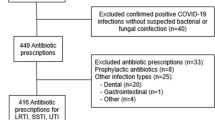
A total of 413 physicians responded to the survey. The characteristics of the participants are detailed in Table 1. The overall adherence to the guidelines, in terms of both appropriate molecule and treatment duration was 2974/4956 (60%) responses. Tables 2 and 3 summarize the results of the survey.
Diseases with a correct response rate higher or equal to 70% included cystitis, GASP, paediatric congestive otitis, and bacterial superficial skin infections. Paediatric congestive otitis (with a viral cause) was incorrectly prescribed antibiotics by 123/413 (30%) physicians.
Diseases with a correct response rate between 51 and 69% included bacterial frontal sinusitis, bacterial maxillary sinusitis, and UTIs. For bacterial sinusitis (both maxillary and frontal), the combined correct response rate was approximately 60%.
Diseases with a correct response rate lower or equal to 50% included pyelonephritis, dog bite wounds, CAP in patients aged 65 and above, and COPD exacerbations. The combined correct response rate for these diseases was 43%.
Pyelonephritis in women was accurately treated in 48% of cases, despite 30% of the prescriptions suggesting a treatment duration longer (10 to 14 days) than guidelines (7 days).
For prophylactic management of dog bite wounds, only 41% of physicians adhered to the recommended treatment duration. Treatment durations frequently exceeded guidelines, with an average of 6.1 days (+ 1.1 days) for the first-line antibiotic (Amoxicillin/clavulanic acid), 7.0 and 7.2 days (+ 2 and + 2.2 days) for the second-line antibiotics (Doxycycline and Pristinamycin). In some instances, the treatment extended to as long as 10 days in 7% of prescriptions.
As for COPD exacerbations, approximately 1/3 of the physicians adhered to the AFFSAPS recommendations, opting not to prescribe antibiotics, while 2/3 of the physicians prescribed antibiotics, in alignment with the SPILF guidelines. Within this context, an appropriate answer in terms of both drug and treatment duration was observed in 37/413 (12%) responses.
For the management of community-acquired pneumonia in elderly patients (aged ≥ 65 years), a mere one-third (27%) of physiciens adhered to the guidelines regarding the first-line antibiotic (amoxicillin/clavulanic acid) and treatment duration (7 days).
Factors associated with the propensity for overtreatment included: age over40 years, practising in rural settings, and holding a hospital-based position, as detailed in Table 4.
Discussion
This study assessed the knowledge level of GPs for recommended treatments and the factors associated with the over-prescription of antibiotics for community-acquired infections. We found that physicians aged over 40 years (p = 0.001) were associated with antibiotic over-prescription. This finding is consistent with previous data on antibiotic consumption in France, which suggests an association between antibiotic over-prescription and the age of the practitioner11,12,13. The inclination for over-treatment among hospital doctors (p < 0.001) is more challenging to interpret. One hypothesis is that their responses could be influenced by their routine exposure to critically ill patients, often requiring broad spectrum antibiotic treatments.
Heterogeneous levels of knowledge were observed according to the different diagnoses: low (≤ 50% of correct answers), mild (51–69% of correct answers) and high (≥ 70% of correct answers).
Prescription of antibiotic prophylaxis following an animal (dog) bite is a standard practice endorsed by several national guidelines, including French guidelines2,14. In our study, the duration of antibiotic prophylaxis for dog bite wounds exceeded the recommended duration (mean value 6.2 days vs 5 days). This discrepancy might be attributed to the French guidelines, which allow for an extension of treatment duration up to 10 days when signs of local or general infection are presents2. Yet, the likelihood of infection post-animal bites vary based on the context and the animal species involved. In particular, cat bite wounds tend to be more frequently infected than dog bite wounds15. Moreover, surgical intervention plays a significant role in reducing wound infection. In some instances, surgical repair proves as effective as antibiotic prophylaxis in preventing wound infection post-animal bites16,17, Further research is required in order to determine the optimal management strategy for animal bites while reducing antibiotic over-prescription.
Our research showed that over 30% of practitioners recommended a longer antibiotic treatment (10 to 14 days) than guidelines (7 days) for treating pyelonephritis in women. Such findings are of significant concern, given that fluoroquinolones (first-line antibiotics) are broad-spectrum antibiotics, which play a pivotal role in the emergence of bacterial resistance. The problem also arises, albeit to a lesser extent, with second line antibiotics (third generation cephalosporins). As part of ongoing efforts to fight antibiotic resistance, new French guidelines for the management of urinary tract infections were published in 2021. In these recommendations, fluoroquinolones have been downgraded to third-line drugs, with trimethoprim-sulfametoxazole emerging as the preferred first-line antibiotic18. Still, there’s room for improvement, especially concerning the antibiotic duration. Indeed, shorter treatment durations (5 days) for simple acute pyelonephritis are recommended by guidelines endorsed by the European Association of Urology19.
UTIs in males were generally managed appropriately in terms of antibiotic selection, but results were poor when duration of antibiotic treatment was considered. Indeed, 19% of prescriptions exceeded the recommended duration (14 days). The optimal duration for antibiotic treatment for UTIs in males remains controversial. The various presentations of UTIs in males (cystitis, pyelonephritis and prostatitis) are often difficult to define, especially in a community-based setting20.
In this study, only one-third (27%) of practitioners adhered to the guidelines regarding the choice of first line drug (amoxicillin/clavulanic acid) and duration (7 days) for managing CAP in individuals aged 65 and above. A potential confounding factor may be the older guidelines endorsed by SPILF and AFFSAPS in 2010, which recommended the use of amoxicillin for 7–14 days for both adults and the elderly9. Furthermore, prevailing medical practices might be influenced by other factors, either intrinsic (e.g. practitioner’s experience and potential gaps in ongoing training) or extrinsic (e.g. patients’ demands and pharmaceutical representatives), as corroborated by prior research21,22. Our findings emphasize the lack of information and highlight the need for improving the distribution of endorsed guidelines. New French guidelines are currently in progress considering the results of a recent trial which demonstrated the non-inferiority of 5-day treatment versus the standard treatment (7 days) for patients with a CAP and a favourable evolution23. However, improvements are required for the choice of molecules as well. Indeed, France ranks as one of the top consumers of extended spectrum penicillins ± beta lactamase inhibitors within the European Union24. One of the main indication for extended spectrum penicillins in France is pneumonia, while narrow spectrum penicillins are preferred in other European countries8,25. Moreover, guideline recommendations are predominantly shaped by hospital-based specialists who face routinely severe pneumonia cases requiring an urgent life-saving antibiotic treatment. Consequently, broad-spectrum molecules (e.g. beta-lactam + beta-lactamase inhibitor) are usually prescribed in hospital settings. Conversely, narrow-spectrum antibiotics are more fitting for non-severe outpatient cases, aligning with guidelines from other European countries. This strategy is similar to the United Kingdom’s approach, which favours amoxicillin as first-line treatment26. The variations in national guidelines can be attributed to the level of knowledge of CAP microbiology. Further research is necessary to improve knowledge of pneumonia epidemiology in France with the objective to minimize the use of broad spectrum penicillins.
This study showed moderate findings related to the treatment of ear-nose-throat infections. For bacterial sinusitis, the combined accuracy rate (for both maxillary and frontal) was almost 60%. Moreover, an inclination to prescribe a treatment exceeding the recommended duration (7 days) was observed for second line drugs (fluoroquinolones, third generation cephalosporins). For congestive otitis in children, 30% of practitioners prescribed antibiotic therapy, even though no antibiotic treatment is recommended according to SPILF guidelines, as the majority of congestive otitis cases are viral in origin2. It is possible that many practitioners would be misled by other guidelines which recommended amoxicillin as first line treatment of otitis media27. These findings are in line with those from others studies, and emphasize the necessity of improving educational interventions among GPs28. Indeed, antimicrobial stewardship programs can focus on situations where “antibiotic treatment is contraindicated or not beneficial”29. The decrease of antibiotic prescriptions after antimicrobial stewardship programs was demonstrated in case of viral infections in community30.
Exacerbations of COPD are common in a GP’s daily practice. As the general population ages, with the consequent increase in comorbidities, its burden is expected to grow in the following years31. While antibiotics are fundamental to treating COPD exacerbations, their appropriate administration in instances of severe, albeit non- life-threatening exacerbations remains a subject of debate. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines suggest using oral antibiotics in the presence of signs of infections, but the best strategy to detect infection remains controversial. The most prevalent method to evaluate infection risk during a COPD exacerbation is the evaluation of sputum purulence, though its use in a GP’s clinical practice is limited by its interpretive subjectivity. Additionally, sputum culture isn’t practical in community settings. Similarly, the use of biomarkers of infection during COPD exacerbation (C-reactive protein, procalcitonin) remains controversial, with research yielding inconclusive outcomes32. Moreover, an important confounding factor is the existence of divergent guidelines. In France, AFSSAPS 2011 guidelines did not recommend any antibiotic treatment, while SPILF 2017 guidelines recommended a 5-day antibiotic course2,8. Given this lack of clear consensus, the management of COPD exacerbations is often based more on the practitioner’s clinical experience rather than established guidelines33,34. Thus, the prescription of an antibiotic treatment during a COPD exacerbation frequently presents a conundrum for GPs. In this context of confusion, harmonization of guidelines is advisable.
For cystitis in women, GASP, and bacterial superficial skin infections, no criticisms were highlighted by this study.
This study presented several limitations: (i) the survey was diffused principally through internet and social media. Consequently, a younger population was selected (31 years old for this study vs 57.1 years old for French GP populations). Because age is a cause of over-treatment, our study likely underestimates prescription times; (ii) the absence of some data in the clinical cases included in the survey (duration of symptoms, re-evaluation after 48 h from the beginning of the antibiotic therapy) reduced the evaluation of treatment duration; (iii) The survey was designed to be completed by each prescriber in less than 15 min. For this reason, some frequent community-acquired infectious diseases were excluded, such as: cystitis in pregnant woman, acute diarrhoea, otitis media in children less than 2 years old; (iv) This study was based on a web questionnaire. Answers could attest the global knowledge of GPs rather than their attitude in daily clinical practice.
Conclusions
This study presented the answers to a Web based survey in a French region (Occitanie). It analysed the knowledge of 413 GPs about official guidelines concerning 11 infectious diseases which are routinely managed in GP’s office: GASP, bacterial maxillary sinusitis, bacterial frontal sinusitis, congestive otitis in children, cystitis in women, pyelonephritis in women, UTI in men, bacterial superficial skin infections, dog bite wounds, CAP in ≥ 65-year-old patients, COPD mild exacerbation.
According to this survey, knowledge of treatment durations is satisfactory with 60% of recommendations being met. However, heterogeneous levels were observed according to different diseases: (i) diseases with low level of knowledge (≤ 50% of correct answers) were pyelonephritis, dog bite wounds and CAP in patients ≥ 65-year-old.; (ii) diseases with mild level of knowledge (51–69% of correct answers) were bacterial frontal sinusitis, bacterial maxillary sinusitis and UTI; (iii) diseases with high level of knowledge (≥ 70% of correct answers) were cystitis, group A streptococcal pharyngitis and bacterial superficial skin infections. Moreover, the study identified age > 40-year-old, country setting and hospital job as factors associated with the risk of overtreatment.
Results of this study shows that rate of adherence is high when recommendations are clear while it falls when different guidelines existed or are not clear. According to data presented in this article, there is a limited margin of progression for the proper use of antibiotics when guidelines are clear. It is necessary to provide simplified and updated guidelines through channels accessible to GPs.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AFSSAPS:
-
French agency for the Sanitary Safety of Health Products (Agence Française de Sécurité Sanitaire des Produits de Santé)
- CAP:
-
Community-acquired pneumonia
- COPD:
-
Chronic obstructive pulmonary disease
- DDD:
-
Daily defined dose
- ENT:
-
Ear-nose-throat
- GASP:
-
Group A streptococcal pharyngitis
- GOLD:
-
Global initiative for chronic obstructive lung disease
- GP:
-
General practitioner
- SPILF:
-
French Society of Infectious Diseases (Societé de Pathologie Infectieuse de Langue Française)
- UTI:
-
Urinary tract infection
References
Agence nationale de sécurité du médicament et des produits de santé. Evolution des consommations d’antibiotiques en France entre 2000 et 2015 - Point d’Information. http://ansm.sante.fr/S-informer/Points-d-information-Points-d-information/Evolution-des-consommations-d-antibiotiques-en-France-entre-2000-et-2015-Point-d-Information (Accessed 14 December 2019) (2017).
Wintenberger, C. et al. Proposal for shorter antibiotic therapies. Med Mal. Infect. 47(2), 92–141. https://doi.org/10.1016/j.medmal.2017.01.007 (2017).
Gauzit, R. et al. Anti-infectious treatment duration: The SPILF and GPIP French guidelines and recommendations. Infect. Dis. Now 51(2), 114–139. https://doi.org/10.1016/j.idnow.2020.12.001 (2021).
Maugat S, Berger Carbonne A, Colomb Cotinat M, Dumartin C, Pefau M, Coignard B, Cavalie P, Hider Mlynarz K, Semaille C, Chevance A, Gay E, Moulin G, Madec JY, Brun Buisson C. Consommation d’antibiotiques et résistance aux antibiotiques en France : soyons concernés, soyons responsables. https://www.anses.fr/fr/system/files/2017_Brochure_Antibioresistance.pdf] (Accessed 4 March 2022) (2017).
European Centre for Disease Prevention and Control. Antimicrobial consumption database (ESAC-Net). https://www.ecdc.europa.eu/en/antimicrobial-consumption/surveillance-and-disease-data/database] (Accessed 19 April 2022).
Curtin, F. & Schulz, P. Assessing the benefit: Risk ratio of a drug–randomized and naturalistic evidence. Dialogues Clin. Neurosci. 13(2), 183–190. https://doi.org/10.31887/DCNS.2011.13.2/curtin (2011).
Cécilia Costa. Évaluation de la durée des prescriptions antibiotiques: Enquête auprès des médecins généralistes de la région Corse. Sciences du Vivant [q-bio]. ffdumas-02413055f ((FRENCH) (2018).
Chidiac, C. et al. Systemic antibiotherapy for the treatment of lower respiratory tract infections. Community acquired pneumonia, acute exacerbation of obstructive chronic bronchitis AFSSAPS/SPILF. Med. Mal. Infect. 41(5), 221–8. https://doi.org/10.1016/j.medmal.2010.10.001 (2011).
Journal officiel de la République Française : LOI n° 2012–300 du 5 mars 2012 relative aux recherches impliquant la personne humaine. https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000025441587&categorieLien=i (Accessed 9 April 2020).
Deplanque, D. et al. French Jardé’s law and European regulation on drug trials: Harmonization and implementation of new rules. Thérapie 72(1), 73–80. https://doi.org/10.1016/j.therap.2016.12.006 (2017).
Diamantis, S. et al. Prescription of antibiotics by GPs for patients with a diagnosis of SARS- CoV-2 infection: Analysis of an electronic French health record. Int. J. Antimicrob. Agents 61(5), 106778. https://doi.org/10.1016/j.ijantimicag.2023.106778.B (2023).
Bara, W., Brun-Buisson, C., Coignard, B. & Watier, L. Outpatient antibiotic prescriptions in france: Patients and providers characteristics and impact of the COVID-19 pandemic. Antibiotics 11(5), 643. https://doi.org/10.3390/antibiotics11050643 (2022).
Schmidt, M. L., Spencer, M. D. & Davidson, L. E. Patient, provider, and practice characteristics associated with inappropriate antimicrobial prescribing in ambulatory practices. Infect. Control Hosp. Epidemiol. 39(3), 307–315. https://doi.org/10.1017/ice.2017.263 (2018).
Baxter, M., Denny, K. J. & Keijzers, G. Antibiotic prescribing in patients who presented to the emergency department with dog bites: A descriptive review of current practice. Emerg. Med. Australas. 32(4), 578–585. https://doi.org/10.1111/1742-6723.13467 (2020).
Jaindl, M., Oberleitner, G., Endler, G., Thallinger, C. & Kovar, F. M. Management of bite wounds in children and adults-an analysis of over 5000 cases at a level I trauma centre. Wien Klin. Wochenschr. 128(9–10), 367–375. https://doi.org/10.1007/s00508-015-0900-x (2016).
Chávez-Serna, E. et al. Experience in the management of acute wounds by dog bite in a hospital of third level of plastic and reconstructive surgery in Mexico. Cir. Cir. 87(5), 528–539. https://doi.org/10.24875/CIRU.19000678 (2019).
Zangari, A. et al. Dog bite injuries in a tertiary care children’s hospital: A seven-year review. Pediatr. Int. 63(5), 575–580. https://doi.org/10.1111/ped.14484 (2021).
Haute Autorité de santé. Antibiothérapie des infections à entérobactéries et à Pseudomonas aeruginosa chez l’adulte : place des carbapénèmes et de leurs alternatives. https://www.has-sante.fr/upload/docs/application/pdf/2019-06/synthese_infections_enterobacteries.Pdf (Accessed 23 February 2020).
Bruyere, F. et al. Urinary tract infections in adults: Comparison of the French and the European guidelines. Prog. Urol. 30(8–9), 472–481. https://doi.org/10.1016/j.purol.2020.02.012.(FRENCH) (2020).
Soudais, B. et al. Diagnosis and management of male urinary tract infections: A need for new guidelines. Study from a French general practice electronic database. Fam. Pract. 38(4), 432–440. https://doi.org/10.1093/fampra/cmaa136 (2021).
Eggers-Kaas, L. et al. Antibiotic treatment of community-acquired pneumonia: A questionnaire survey in Danish general practice. Basic Clin. Pharmacol. Toxicol. 130(1), 151–157. https://doi.org/10.1111/bcpt.13684 (2022).
Saliba-Gustafsson, E. A., Nyberg, A., Borg, M. A., Rosales-Klintz, S. & Lundborg, C. S. Barriers and facilitators to prudent antibiotic prescribing for acute respiratory tract infections: A qualitative study with GPs in Malta. PLoS One 16(2), e0246782. https://doi.org/10.1371/journal.pone.0246782 (2021).
Uranga, A. et al. Duration of antibiotic treatment in community-acquired pneumonia: A multicenter randomized clinical trial. JAMA Intern. Med. 176(9), 1257–1265 (2016).
Bruyndonckx, R. et al. Consumption of penicillins in the community, European Union/European Economic Area, 1997–2017. J. Antimicrob. Chemother. 76(12 Suppl 2), ii14–ii21 (2021).
DANMAP. Use of Antimicrobial Agents and Occurrence of Antimicrobial Resistance in Bacteria from Food Animals, Food and Human in Denmark. www.danmap.org/reports/2022] (Accessed 12 May 2023) (2022).
National Institute for health and care Excellence. Pneumonia (community-acquired): antimicrobial prescribing. https://www.nice.org.uk/guidance/ng138/chapter/recommendations#choice-of-antibiotic] (Accessed 31 May 2023).
Societé de pathologie infectieuse de langue française. Antibiothérapie par voie generale en pratique courante dans les infections respiratoires hautes de l’adulte et l’enfant. https://www.infectiologie.com/userfiles/file/medias/recos/2011-infections-respir-hautes-recommandations.pdf (Accessed 22 March 2012).
Dallas, A. et al. Antibiotic prescribing for acute otitis media and acute sinusitis: A cross-sectional analysis of the ReCEnT study exploring the habits of early career doctors in family practice. Fam. Pract. 34(2), 180–187. https://doi.org/10.1093/fampra/cmw144 (2017).
Smieszek, T. et al. Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 73(suppl_2), ii36–ii43. https://doi.org/10.1093/jac/dkx500 (2018).
Turner, A. et al. Temporal patterns of antibiotic prescribing for sore throat, otitis media, and sinusitis: A longitudinal study of GP registrars. Fam. Pract. https://doi.org/10.1093/fampra/cmad055 (2023).
Struyf, T. et al. Burden of infections on older patients presenting to general practice: A registry-based study. Fam. Pract. 38(2), 166–172. https://doi.org/10.1093/fampra/cmaa105 (2021).
Global strategy for prevention, diagnosis and management of copd: 2023 report. https://goldcopd.org/2023-gold-report-2/ (Accessed 25 May 2023).
Perera, B., Barton, C. & Osadnik, C. General practice management of COPD patients following acute exacerbations: A qualitative study. Br. J. Gen. Pract. 73(728), e186–e195. https://doi.org/10.3399/BJGP.2022.0342 (2023).
Cousins, J. L. et al. Management of acute COPD exacerbations in Australia: Do we follow the guidelines?. ERJ Open Res. 6(2), 00270–02019. https://doi.org/10.1183/23120541.00270-2019 (2020).
Author information
Authors and Affiliations
Contributions
A.S. drafted the article; M.B. contributed in acquisition of data and drafted the article; M.C.P. contributed in analysis and interpretation of data; R.L. revised the manuscript and checked English grammar and spelling; P.L. contributed in interpretation of data; B.C. contributed in conception and design of the study; S.D. contributed in conception and design of the study and revised the article critically for important intellectual content. All authors have approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Strazzulla, A., Ballarin, M., Postorino, M.C. et al. Knowledge of recommended antibiotic treatments for community-acquired infections in general medical practice: a cross-sectional study in Occitanie region, France. Sci Rep 13, 17312 (2023). https://doi.org/10.1038/s41598-023-43809-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43809-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.