Abstract
Comprehensive prediction of urolithiasis using available factors obtained in the emergency department may aid in patient-centered diagnostic imaging decisions. This retrospective study analyzed the clinical factors, blood chemistry and urine parameters of patients who underwent nonenhanced urinary computed tomography for suspected urolithiasis. A scoring system was developed from a logistic regression model and was tested using the area under the curve (AUC). The prevalence of urolithiasis and important possible causes in the three risk subgroups were determined. Finally, the scoring model was validated. In the derivation cohort (n = 673), 566 patients were diagnosed with urolithiasis. Age > 35 years, history of urolithiasis, pain duration < 8 h, nausea/vomiting, costovertebral angle tenderness, serum creatinine ≥ 0.92 mg/dL, erythrocytes ≥ 10/high power field, no leukocytes ≤ + , and any crystalluria were retained in the final multivariable model and became part of the score. This scoring model demonstrated good discrimination (AUC 0.808 [95% CI, 0.776–0.837]). In the validation cohort (n = 336), the performance was similar (AUC 0.803 [95% CI, 0.756–0.844]), surpassing that of the STONE score (AUC 0.654 [95% CI, 0.601–0.705], P < 0.001). This scoring model successfully stratified patients according to the probability of urolithiasis. Further validation in various settings is needed.
Similar content being viewed by others
Introduction
Urolithiasis is a commonly encountered problem in the emergency department (ED)1. The lifetime prevalence of urolithiasis is approximately 10–15% in developed countries2, and the relapse rate is approximately 75% within 20 years3,4. Moreover, the incidence of urolithiasis has been reported to be increasing globally5,6.
Since unenhanced computed tomography (CT) was first introduced for the diagnosis of urolithiasis in 19957, it has become the gold-standard diagnostic tool for suspected ureteric colic8,9. The advantage of this diagnostic tool is that it is rapid and accurate, identifies the exact size and location of urolithiasis and has been successful at detecting other pathologic conditions10. Its main disadvantages are cost problems and radiation doses, which are coupled with the possible complications of an increased risk of cancer. Furthermore, recent literature shows that CT scans do not lead to improvements in patient outcomes11,12. Therefore, to optimize the diagnostic efficiency and determine patient-centered diagnostic strategies, with the recent increase in the use of point-of-care ultrasound (POCUS), several clinical prediction tools have been developed13,14,15,16. The best known and the most widely used is the STONE score13, which is the sum of integer points of five factors: sex (male), timing (duration of pain to presentation), origin, nausea, and erythrocytes in the urine dipstick test. Scores ranging from 0 to 5, 6–9 and 10–13 represent a low, moderate, and high probability of urolithiasis, respectively. The STONE score functions well and has been externally validated. However, contrary to the STONE score, which was derived from patients undergoing a nonenhanced CT (NECT) protocol for suspected urolithiasis, some validation studies have been conducted with various inclusions16,17,18. Furthermore, this scoring system does not include various test results available in the ED.
Therefore, we hypothesized that among consecutive patients undergoing a NECT protocol for suspected urolithiasis, a new comprehensive score based on clinical factors, blood chemistry and urinalysis (UROLITHIASIS score), would provide a more rational diagnostic strategy and aid in patient-centered diagnostic imaging decisions. The primary aim of this study was to develop and validate this comprehensive scoring model for patients who were highly suspected of having urolithiasis. The secondary aim was to validate and compare the published scoring system.
Results
Patients selection
Among the 1043 patients who underwent the urinary NECT protocol with suspected urolithiasis, 34 were excluded due to the lack of urinalysis (n = 27) or blood chemistry results (n = 7) (Fig. 1). The remaining 1009 patients were divided into derivation (n = 673) and validation cohorts (n = 336).
Derivation cohort
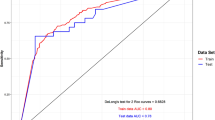
In the derivation cohort, 566 patients (84.1%) were diagnosed with urolithiasis and were categorized into the urolithiasis group, and 107 patients (15.9%) were categorized into the nonurolithiasis group. Table 1 shows that several factors were significantly different between the two groups. According to the univariate analyses, sex, age, history of urolithiasis, pain duration, pain score on to the visual analog scale (VAS), nausea and vomiting, costovertebral angle (CVA) tenderness, serum blood urea nitrogen (BUN), creatinine, serum C-reactive protein (CRP), pyuria, hematuria and crystalluria were associated with the presence of urolithiasis. The multivariate analysis yielded 9 factors that were independent predictors of urolithiasis: age > 35 years, history of urolithiasis, pain duration < 8 h, nausea/vomiting, CVA tenderness, red blood cells (RBCs) ≥ 10/high-power field (HPF), no leukocyte ≤ + , any crystalluria and creatinine ≥ 0.92 mg/dL (Table 2). This final model showed good discrimination with an area under the curve (AUC) of 0.809 (95% confidence interval [CI], 0.778–0.838) (Fig. 2A).
The UROLITHIASIS score was developed based on these independent predictors. The regression coefficients of the 9 predictors were converted to integer points, which are listed in Table 2. The minimum sum of points was 0, and the maximum was 20. The performance of the UROLITHIASIS score was similar to that of the multivariate model (AUC 0.808 [95% CI, 0.776–0.837]) (Fig. 2A).
Figure 3 represents the prevalence of urolithiasis and important alternate causes of symptoms in the 3 risk-stratified groups. A total of 94.9% of the patients in the high-probability (12–20) group were diagnosed with urolithiasis. In the moderate (7–11) and low (0–6) groups, the prevalence of urolithiasis decreased to 83.5 and 33.9%, respectively. On the other hand, as the score decreased from the high- to the moderate- and low-probability groups, the prevalence of important alternate causes increased by 1.1, 1.2, and 7.1%, respectively. The findings of important alternate causes of symptoms are presented in Table 3.
Validation cohort
Of the 336 patients, 288 were diagnosed with urolithiasis. The AUC of the UROLITHIASIS score was 0.803 (95% CI, 0.756–0.844) (Fig. 2B). The prevalence of urolithiasis and important alternate causes by the three groups was 97.7 and 2.3% in the high-probability group, 81.9 and 3.2% in the moderate-probability group, and 31.3 and 6.3% in the low-probability group, respectively (Fig. 3 and Table 3).
We next investigated whether the STONE score could reliably predict urolithiasis in our validation cohort. The AUC of the STONE score in our cohort was 0.654 (95% CI, 0.601–0.705), which was significantly lower than that of the UROLITHIASIS score (vs. 0.803 [95% CI, 0.756–0.844], P < 0.001) (Fig. 2B). According to the STONE score, the prevalence of urolithiasis and important alternate causes was 91.0% and 3.3% in the high-probability group (n = 184), 81.6 and 2.7% in the moderate-probability group (n = 147), and 40.0 and 0.0% in the low-probability group (n = 5), respectively (Table 4).
When comparing our validation cohort with the original STONE score validation cohort, there was a significant difference in the proportion of each probability group (P < 0.001) (Table 4). In contrast, the proportions of urolithiasis and alternate causes in each category were not significantly different between two cohorts, except for urolithiasis in the moderate group.
The UROLITHIASIS score did not show a correlation with stone size (r = 0.007, p = 0.909) or an association with stone location (Supplementary Tables S1 and S2).
Discussion
In this retrospective analysis in a large population of patients who were highly suspected of having urolithiasis, a comprehensive clinical prediction score using data easily obtained at the time of ED admission accurately estimated the risk of urolithiasis. Simultaneously, this tool can be inversely associated with the likelihood of an important alternative cause of symptoms. In the validation cohort, the diagnostic performance of the UROLITHIASIS score was significantly higher than that of the STONE score.
In the present study, we developed a new clinical scoring system for urolithiasis that consists of nine independent predictors. Among these, a short duration of pain, a history of urolithiasis, hematuria and nausea/vomiting have also been used in the STONE score or modified STONE score13,16. In particular, the presence or absence of hematuria is a point of interest, as its absence may prompt physicians to order more diagnostic CTs to narrow the list of differential diagnoses19,20. Hematuria is identified as the most robust predictor of urolithiasis not only clinically but also in scoring systems21,22, but different studies define it differently13,16. Positive hematuria on the dipstick test is simply a color change due to oxidation of a test-strip reagent, and this does not confirm the presence of RBCs in urine. Various factors can cause false-positive results on a dipstick test23. Thus, finding hematuria on the dipstick must be confirmed by microscopic examination. In contrast, if the specific gravity of the urine is very low, microscopy can fail to detect urinary RBCs because they can be lysed with hemoglobin release23. Comparing urine dipstick and microscopic examinations to derive our scoring system, we found that the latter had a higher diagnostic value, and the presence of 10 or more RBCs was calculated as a cutoff for urolithiasis, which is a higher value than the positive microhematuria definition according to the American Urological Association (AUA) guidelines (≥ 4 to 9 RBCs/HPF)24. A possible explanation for this is that our cohort was selected by the physician gestalt, which can be defined as a physician’s implicit probability estimation based on experience and clinical perception (i.e., presence of microhematuria). This aspect should be taken into account in the interpretation of our results.
Several factors missing from other scoring systems were included in the UROLITHIASIS score. Crystalluria is considered a marker of urine supersaturation, which may be the result of certain metabolic disorders and disproportional urinary inhibitors and promoters, which may ultimately lead to the formation of urolithiasis25. From routine serum biochemistry results, we found a significant association between the serum creatinine levels and urolithiasis. Elevated serum levels of creatinine may indicate a high degree of urinary tract obstruction by urolithiasis. Biomarkers for infection may help physicians exclude urinary tract infections (UTIs) that commonly mimic urolithiasis. While Kim et al. revealed the usefulness of serum CRP16, leukocyte esterase was included in our final scoring model. Reports regarding urinary markers for UTI are conflicting, some studies showing comparable performance between urine dipstick and microscopy and other studies showing comparable but better sensitivity and diagnostic performance of leukocyte esterase26,27. The prevalence of urolithiasis increases with age, and CVA tenderness is present in 25–52% of patients21,28. Finally, our comprehensive scoring system showed excellent overall performance in both the derivation and validation cohorts.
Our finding that the overall performance of the STONE score was fair (AUC 0.654) is inconsistent with previous studies14,16,17,18,29,30,31,32. The majority of analyses have showed that the STONE score can predict urolithiasis well: its AUCs have ranged from 0.75 to 0.92, and the prevalence of urolithiasis in the high-risk group ranges from 72.7 to 98.7%. However, in contrast to the original study that included only patients undergoing NECT for suspected uncomplicated urolithiasis, several researchers analyzed patients with flank pain, and various CT protocols to evaluate the abdomen were used regardless of contrast use16,17,18. In this study, we validated the STONE score by evaluating patients to undergo urinary NECT scan imaging as a clinical pathway for a patient with suspected urolithiasis. This group likely represents those patients for whom attending emergency physicians (EPs) have greater certainty about the diagnosis of urolithiasis compared with those who received enhanced abdominal CT imaging and were excluded from this analysis. Therefore, patients deemed to have a very high probability of urolithiasis may have been more likely to be included, which was partially confirmed by our rate of urolithiasis and hematuria. The overall prevalence of urolithiasis in the study population was approximately 85%, which is higher than those of the original study (49.5%) and other validation studies. Furthermore, only 67 (10%) of the patients did not present with hematuria according to the AUA guidelines24.
According to the UROLITHIASIS score, the distribution of urolithiasis probabilities in our validation cohort was 39.3, 56.6, and 4.8% in the high-, moderate-, and low-probability groups, in which the high- and low-probability groups had corresponding prevalences of urolithiasis and alternate causes, respectively. When we applied the STONE score to our validation cohort, more than half of the patients were categorized in the high-probability group, and 91.0% of them had urolithiasis. Interestingly, the proportions of urolithiasis in the high- and low-probability group were similar to those of the original validation cohort13. However, the STONE score indicated that additional CT imaging was necessary for only 1.5% of the patients (low-probability group), of whom 40% had urolithiasis. We believe that our comprehensive score would be more informative for EPs in deciding upon NECT imaging for patients with highly suspected urolithiasis.
There are several limitations to this study. First, it was from a single hospital, and it was a retrospectively designed study. During the study period, suspected urolithiasis patients were managed through the same clinical pathway, but patients were not included if they did not have a CT scan. Additionally, patients with suspected abdominal disease who underwent contrast-enhanced CT were not enrolled in this study, which could lead to selection bias. However, considering the purpose of this score, we believe that the development of the score by evaluating selected patients is more suitable for the future application of this score. Second, increasing the number of clinical factors within a predictive scoring model could lead to a reduction in its practicality even as its predictive power is enhanced. While the STONE score comprises five factors, which are relatively easily to ascertain, the UROLITHIASIS score encompasses nine independent predictors. Furthermore, it encompasses the results of laboratory tests and urinalysis, including parameters such as crystalluria. Nonetheless, considering the excellent predictive performance demonstrated by the UROLITHIASIS score, this comprehensive clinical prediction score could provide even more valuable information, especially about emergency patients with a suspected urolithiasis who have already undergone comprehensive blood tests and urinalysis. Third, the UROLITHIASIS score was primarily designed for diagnostic purposes and is not associated with additional information such as stone size and location, so it cannot guide additional therapeutic decisions. Fourth, urolithiasis may differ in prevalence according to race/ethnicity, geographical conditions, lifestyle, and dietary factors33,34, and race is one of the factors of the STONE score, but our score did not include these epidemiological variables. Finally, there was a lack of an assessment of the reliability of the predictor variables. Further prospective studies in different settings should validate this risk score to show the generalizability of our results.
In conclusion, we derived and validated a comprehensive urolithiasis prediction score using various factors, including clinical, blood chemistry and urinalysis parameters in patients with suspected urolithiasis. This clinical scoring system accurately predicted the likelihood of urolithiasis and can aid in patient-centered diagnostic imaging decisions. Further external validation in different settings is warranted.
Methods
Study design and patients
We performed a retrospective analysis of consecutive patients admitted to a large urban ED from 2014 to 2015. During the study period, our institution had a clinical pathway for patients with suspected urolithiasis, a protocol that included pain management and urinary NECT scanning by an EP and outpatient follow-up after discharge. The use of POCUS for these patients was not recommended. Accordingly, the attending EP or senior emergency medicine resident examined all adult patients and decided to perform urinary NECT when urolithiasis was suspected. If another abdominal disease or complicated urolithiasis was suspected, a CT scan with the intravenous administration of contrast medium was done.
This study included adult patients (> 18 years) who underwent the urinary NECT protocol. The exclusion criteria included patients without urinalysis or blood biochemistry tests.
The study protocol was approved by the Institutional Review Board (IRB) of the Seoul St. Mary’s hospital (KC17RESI0747) and was performed in accordance with the ethical guidelines of the Declaration of Helsinki. Informed consent was waived by IRB of the Seoul St. Mary’s hospital because of the retrospective nature of the study.
Data collection
We retrieved the records of patients who underwent the urinary NECT protocol from the picture archiving and communication system. One author reviewed the patients’ medical charts, and all CT scan reports were dictated by board-certified radiologists. From the medical records, clinical variables (sex, age, preexisting disease, body temperature, pain duration, pain scale according to VAS, presence or absence of nausea with/without vomiting and the CVA tenderness) and blood chemistry results (CRP, BUN, creatinine) were collected for all included patients. We analyzed both results that were obtained by the dipstick test and those obtained by microscopic inspection. The following dipstick findings were evaluated: specific gravity, nitrite, occult blood, and leukocyte esterase positivity. The urine samples were also evaluated with a high magnification (400×) microscope after centrifugation at 1500 rpm for 5 min and were recorded as follows: RBC and white blood cell counts/HPF and the presence of any crystals.
Outcome measures
We acquired CT scans on a multidetector computed tomography scanner (SOMATOM Sensation 64, Siemens AG, Forchheim, Germany), which scanned all patients with a 2-mm slice from the upper pole of the kidneys to the lower edge of the bladder without intravenous contrast medium. Urolithiasis was defined as the presence of one or more attenuation foci in any location from the collecting system to the bladder that was consistent with the patient’s subjective symptoms. Patients having an indirect stone sign (without a visualized stone in the urinary tract but with any acute obstructive signs on urinary NECT) were also considered to have urolithiasis. Because renal pelvic stones can be detected as incidental findings21, renal stones without obstructive signs that were located on the opposite side from the pain were considered incidental, and these patients were classified into the nonurolithiasis group. We also documented important alternative causes of the patients’ symptoms from the dictated reports.
Statistical analysis
All data are presented as the number (percentage) of patients in each group for categorical variables and the mean ± standard deviation or median with interquartile range for continuous variables. To compare the variables between the urolithiasis and nonurolithiasis groups, we used the chi-square test for categorical variables and Student’s t-test for continuous variables.
The enrolled patients were randomly divided into a derivation cohort consisting of 2/3 of the patients and an internal validation cohort with the remaining 1/3 of patients. To derive the risk score models for urolithiasis, we performed univariate analyses between the two groups, and variables with a possible predictive value (p < 0.05) in the univariate analyses were included in the multivariate logistic regression analysis. The optimum cutoffs for continuous variables having statistical significance were calculated using Youden’s J statistic. Finally, to simplify this score, the β coefficients of the significant variables were converted to integer points. The UROLITHIASIS score represented the sum of the weighted scores.
To assess the model performance, the developed score was evaluated using receiver operating characteristic (ROC) curve analysis. According to the UROLITHIASIS score, patients were stratified into low-, moderate-, and high-probability groups, and the prevalence of urolithiasis and important alternative diagnoses were determined for each group. Finally, using the validation cohort, we validated the UROLITHIASIS score and the STONE score. Pairwise AUC comparisons were performed between the prediction models. The association between the UROLITHIASIS score and stone size was assessed as Pearson’s correlation coefficient.
All statistical analyses were performed using SPSS version 24 (IBM, SPSS Inc., Chicago, IL, USA). A p value < 0.05 was regarded as statistically significant.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ghani, K. R. et al. Emergency department visits in the United States for upper urinary tract stones: Trends in hospitalization and charges. J. Urol. 191, 90–96. https://doi.org/10.1016/j.juro.2013.07.098 (2014).
Pak, C. Y. Kidney stones. Lancet 351, 1797–1801. https://doi.org/10.1016/s0140-6736(98)01295-1 (1998).
Trinchieri, A. et al. A prospective study of recurrence rate and risk factors for recurrence after a first renal stone. J. Urol. 162, 27–30. https://doi.org/10.1097/00005392-199907000-00007 (1999).
Sutherland, J. W., Parks, J. H. & Coe, F. L. Recurrence after a single renal stone in a community practice. Miner Electrolyte Metab. 11, 267–269 (1985).
Romero, V., Akpinar, H. & Assimos, D. G. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev. Urol. 12, e86-96 (2010).
Kirkali, Z., Rasooly, R., Star, R. A. & Rodgers, G. P. Urinary stone disease: Progress, status, and needs. Urology 86, 651–653. https://doi.org/10.1016/j.urology.2015.07.006 (2015).
Smith, R. C. et al. Acute flank pain: Comparison of non-contrast-enhanced CT and intravenous urography. Radiology 194, 789–794. https://doi.org/10.1148/radiology.194.3.7862980 (1995).
Nachmann, M. M. et al. Helical CT scanning: The primary imaging modality for acute flank pain. Am. J. Emerg. Med. 18, 649–652. https://doi.org/10.1053/ajem.2000.16292 (2000).
Worster, A., Preyra, I., Weaver, B. & Haines, T. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: a meta-analysis. Ann. Emerg. Med. 40, 280–286. https://doi.org/10.1067/mem.2002.126170 (2002).
Ather, M. H., Faizullah, K., Achakzai, I., Siwani, R. & Irani, F. Alternate and incidental diagnoses on noncontrast-enhanced spiral computed tomography for acute flank pain. Urol. J. 6, 14–18 (2009).
Moore, C. L., Daniels, B., Singh, D., Luty, S. & Molinaro, A. Prevalence and clinical importance of alternative causes of symptoms using a renal colic computed tomography protocol in patients with flank or back pain and absence of pyuria. Acad. Emerg. Med. 20, 470–478. https://doi.org/10.1111/acem.12127 (2013).
Westphalen, A. C., Hsia, R. Y., Maselli, J. H., Wang, R. & Gonzales, R. Radiological imaging of patients with suspected urinary tract stones: National trends, diagnoses, and predictors. Acad. Emerg. Med. 18, 699–707. https://doi.org/10.1111/j.1553-2712.2011.01103.x (2011).
Moore, C. L. et al. Derivation and validation of a clinical prediction rule for uncomplicated ureteral stone–the STONE score: Retrospective and prospective observational cohort studies. BMJ 348, g2191. https://doi.org/10.1136/bmj.g2191 (2014).
Daniels, B. et al. STONE PLUS: Evaluation of emergency department patients with suspected renal colic, using a clinical prediction tool combined with point-of-care limited ultrasonography. Ann. Emerg. Med. 67, 439–448. https://doi.org/10.1016/j.annemergmed.2015.10.020 (2016).
Fukuhara, H. et al. Internal validation of a scoring system to evaluate the probability of ureteral stones: The CHOKAI score. Am. J. Emerg. Med. 35, 1859–1866. https://doi.org/10.1016/j.ajem.2017.06.023 (2017).
Kim, B. et al. External validation of the STONE score and derivation of the modified STONE score. Am. J. Emerg. Med. 34, 1567–1572. https://doi.org/10.1016/j.ajem.2016.05.061 (2016).
Schoenfeld, E. M. et al. Validity of STONE scores in younger patients presenting with suspected uncomplicated renal colic. Am. J. Emerg. Med. 34, 230–234. https://doi.org/10.1016/j.ajem.2015.10.036 (2016).
Rohat, A. K., Kurt, E. & Şenel, Ç. The comparison of two prediction models for ureteral stones: CHOKAI and STONE scores. Am. J. Emerg. Med. 44, 187–191. https://doi.org/10.1016/j.ajem.2020.08.099 (2021).
Carter, M. R. & Green, B. R. Renal calculi: Emergency department diagnosis and treatment. Emerg. Med. Pract. 13, 1–17 (2011).
Mefford, J. M. et al. A comparison of urolithiasis in the presence and absence of microscopic hematuria in the emergency department. West J. Emerg. Med. 18, 775–779. https://doi.org/10.5811/westjem.2017.4.33018 (2017).
Ingimarsson, J. P., Krambeck, A. E. & Pais, V. M. Jr. Diagnosis and management of nephrolithiasis. Surg. Clin. N. Am. 96, 517–532. https://doi.org/10.1016/j.suc.2016.02.008 (2016).
Bove, P. et al. Reexamining the value of hematuria testing in patients with acute flank pain. J. Urol. 162, 685–687. https://doi.org/10.1097/00005392-199909010-00013 (1999).
Bacârea, A., Fekete, G. L., Grigorescu, B. L. & Bacârea, V. C. Discrepancy in results between dipstick urinalysis and urine sediment microscopy. Exp. Ther. Med. 21, 538. https://doi.org/10.3892/etm.2021.9971 (2021).
Grossfeld, G. D. et al. Evaluation of asymptomatic microscopic hematuria in adults: The American Urological Association best practice policy–part I: Definition, detection, prevalence, and etiology. Urology 57, 599–603. https://doi.org/10.1016/s0090-4295(01)00919-0 (2001).
Almannie, R. M. et al. Neural network analysis of crystalluria content to predict urinary stone type. Res. Rep. Urol. 13, 867–876. https://doi.org/10.2147/rru.S322580 (2021).
Taneja, N. et al. Validity of quantitative unspun urine microscopy, dipstick test leucocyte esterase and nitrite tests in rapidly diagnosing urinary tract infections. J. Assoc. Physicians India 58, 485–487 (2010).
Belay, G. et al. Diagnostic performance of reagent strips and microscopy for the diagnosis of urinary tract infection among pregnant women at the University of Gondar comprehensive specialized Hospital, Northwest Ethiopia a cross sectional study. Ethiop. J. Health Biomed. Sci. 9, 105–114 (2018).
Gottlieb, M., Long, B. & Koyfman, A. The evaluation and management of urolithiasis in the ED: A review of the literature. Am. J. Emerg. Med. 36, 699–706. https://doi.org/10.1016/j.ajem.2018.01.003 (2018).
Hernandez, N., Song, Y., Noble, V. E. & Eisner, B. H. Predicting ureteral stones in emergency department patients with flank pain: An external validation of the STONE score. World J. Urol. 34, 1443–1446. https://doi.org/10.1007/s00345-016-1760-3 (2016).
Wang, R. C. et al. External validation of the STONE score, a clinical prediction rule for ureteral stone: An observational multi-institutional study. Ann. Emerg. Med. 67, 423-432.e422. https://doi.org/10.1016/j.annemergmed.2015.08.019 (2016).
Safaie, A., Mirzadeh, M., Aliniagerdroudbari, E., Babaniamansour, S. & Baratloo, A. A clinical prediction rule for uncomplicated ureteral stone: The STONE score; a prospective observational validation cohort study. Turk. J. Emerg. Med. 19, 91–95. https://doi.org/10.1016/j.tjem.2019.04.001 (2019).
Malik, A., Mohkumuddin, S., Yousaf, S., Baig, M. A. R. & Afzal, A. Validity of STONE score in clinical prediction of ureteral stone disease. Pak. J. Med. Sci. 36, 1693–1697. https://doi.org/10.12669/pjms.36.7.2625 (2020).
Siener, R., Bitterlich, N., Birwé, H. & Hesse, A. The impact of diet on urinary risk factors for cystine stone formation. Nutrients https://doi.org/10.3390/nu13020528 (2021).
Abufaraj, M., Al Karmi, J. & Yang, L. Prevalence and trends of urolithiasis among adults. Curr. Opin. Urol. 32, 425–432. https://doi.org/10.1097/mou.0000000000000994 (2022).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization and drafting the text; H.J.K. contributed to the acquisition and analysis of data; S.H.O. contributed to design of the study and preparing the figures; all authors critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H.J., Oh, S.H. Comprehensive prediction of urolithiasis based on clinical factors, blood chemistry and urinalysis: UROLITHIASIS score. Sci Rep 13, 14885 (2023). https://doi.org/10.1038/s41598-023-42208-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-42208-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.