Abstract
Immunity-related GTPase family M (IRGM), located on human chromosome 5q33.1, encodes a protein that promotes autophagy and suppresses the innate immune response. The minor allele of rs13361189 (−4299T>C), a single nucleotide polymorphism in the IRGM promoter, has been associated with several diseases, including Crohn’s disease and tuberculosis. Although patterns of linkage disequilibrium and minor allele frequency for this polymorphism differ dramatically between subjects of European and African descent, studies of rs13361189 have predominantly been conducted in Europeans and the mechanism of association is poorly understood. We recruited a cohort of 68 individuals (30 White, 34 African American, 4 other race) with varying rs13361189 genotypes and assessed a panel of immune response measures including whole blood cytokine induction following ex vivo stimulation with Toll-like Receptor ligands. Minor allele carriers were found to have increased serum immunoglobulin M, C-reactive protein, and circulating CD8+ T cells. No differences in whole blood cytokines were observed between minor allele carriers and non-carriers in the overall study population; however, minor allele status was associated with increased induction of a subset of cytokines among African American subjects, and decreased induction among White subjects. These findings underline the importance of broad racial inclusion in genetic studies of immunity.
Similar content being viewed by others
Introduction
Genes have been estimated to account for ~ 20–40% of the variation in immunologic function across humans, contributing to temporally stable immunologic phenotypes1,2. Identifying genetic polymorphisms that modify disease risk through altering immune cell function is one of the tenets of modern personalized medicine. Multiple genes orchestrate autophagy, an evolutionarily conserved process by which cells clear invasive pathogens and damaged organelles. Autophagy has been shown to suppress the pro-inflammatory functions of immune cells through multiple mechanisms, and also to serve as an effector arm of cell-autonomous antimicrobial host defense3,4. A growing number of polymorphisms in autophagy-related genes have recently been associated with inflammatory and infectious diseases5,6,7.
Immunity-related GTPase family M (IRGM), located on human chromosome 5q33.1, encodes a protein that plays a central role in autophagy by coupling core autophagy proteins to innate immunity receptors8. IRGM is required for autophagy induction by bacterial lipopolysaccharide (LPS) and for autophagic killing of intracellular bacteria9,10,11,12. Silencing IRGM by RNA interference augments LPS induction of TNFα and IL-1β through increasing activation of nuclear factor-κB and p38 and stabilizing NLRP39,13. IRGM silencing also reduces autophagic degradation of TLR3, RIG-I, and CGAS, thereby augmenting immune responses to ligands for these nucleic acid receptors14.
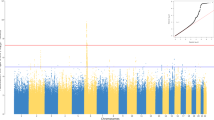
Several reports have shown that rs13361189 (−4299T>C) and rs10065172 (+313C>T), two single nucleotide polymorphisms (SNPs) that are in high linkage disequilibrium (LD) with a presumed causal 20 kb copy number variation (CNV) deletion upstream of IRGM, associate with increased risk for Crohn’s disease (CD)12,15,16,17,18,19. rs13361189 has also been associated with leprosy20 and autoimmune thyroid disease21, and rs10065172 with tuberculosis22 and sepsis mortality23, collectively suggesting that IRGM regulates a wide spectrum of human disease. A major limitation of the studies performed to date on IRGM and CD risk, however, is that nearly all have been conducted in Europeans17,24,25. Compared to Europeans, Africans have much higher IRGM expression and IRGM rs13361189 risk (C) allele frequency (~ 0.50 vs. 0.10 [useast.ensembl.org]), and much lower LD of rs13361189 to the upstream CNV deletion16.
We and others have reported that IRGM expression is reduced in immune cells of subjects with the rs13361189 risk allele13,16, suggesting that changes in IRGM expression may mediate the association of the risk allele with disease by impacting immune cell function. To date, few reports have investigated whether rs13361189 associates with altered cytokine induction, with divergent results and few stimuli tested20,26,27. Higher IFN-γ and IL-4, but unchanged IL-6 and IL-1β were seen in peripheral blood mononuclear cells from Asian risk allele carriers after M. leprae infection20, whereas minimal differences in cytokines were seen after C. albicans27, and none after M. tuberculosis26 in two papers that did not report race.
To better define possible race-specific effects of IRGM polymorphism on immune cell function, we recruited 30 White and 34 African American (AA) healthy subjects in the NIEHS Personalized Environment and Genes Study (PEGS), a North Carolina-based study of > 18,000 subjects with archived DNA13,28. Subjects were immunophenotyped, including cytokine profiling of whole blood. We report that rs13361189 risk (C) allele carriers have a race-specific alteration in cytokines. Specifically, risk allele status is associated with increased induction of a small subset of cytokines in AA subjects, but reduced induction among White subjects. We propose that our findings have implications for IRGM biology and that they underline the importance of broad racial inclusion in studies of genetic determinants of disease.
Results
Study cohort of human subjects with varying IRGM genotypes
A cohort of subjects with varying genotypes at rs13361189 was prospectively recruited to investigate the effect of IRGM polymorphism on immune phenotypes. Exclusion criteria included age < 18 years, active smoking, use of anti-inflammatory or immunosuppressive medications, confirmed/suspected immunodeficiency, and recent gastrointestinal or respiratory illness. As shown in Table 1, a predominantly female cohort of 68 individuals (n = 35 [T/T]; n = 20 [T/C]; n = 13 [C/C]) was recruited. Age and sex were comparable across genotypes. Whereas subjects with a rs13361189 homozygous major allele genotype T/T were predominantly (60%) White, consistent with the racial composition of the PEGS study population (https://www.niehs.nih.gov/research/clinical/studies/pegs/index.cfm), the two minor allele genotypes (T/C, C/C) were predominantly AA, likely reflecting the higher minor allele frequency at rs13361189 in AAs (http://useast.ensembl.org).
Static immune phenotypes across IRGM genotypes
Static immune metrics were first assessed, including complete blood cell count with differential, serum C-reactive protein (CRP) concentration, serum immunoglobulin (Ig) levels, and peripheral blood mononuclear cell profile by flow cytometry (Figs. S1, S2). Here and in all analyses that follow, we selected a dominant genetic model, comparing the T/T genotype to minor allele carriers (i.e., T/C and C/C subjects) by robust linear regression. This model was chosen both because of our prior finding of reduced whole blood IRGM expression in minor allele carriers13 and because of the limited N, in particular, for C/C subjects. Of note, as shown in Table 2, minor allele carriers had higher serum IgM than T/T subjects. Minor allele carriers also had numerical elevations of CRP (p = 0.06), an inflammatory biomarker, and CD8+ T cell count (p = 0.06). Upon race stratification, no significant differences between minor allele carriers and non-carriers were noted among AA subjects. Among White subjects, minor allele carriers exhibited increases in IgM (p = 0.02), IgE (p = 0.05), and CRP (p = 0.06), and a decrease in percentage of circulating plasmablasts (p = 0.005) (data not shown).
In order to assay steady state cytokine production by circulating immune cells, whole blood was incubated ex vivo at 37 °C for 3 h, after which the cells were centrifuged and 13 cytokines were quantified in the serum fraction by multiplex assay. As shown in Table S1, no significant differences were observed between T/T and minor allele subjects in the overall cohort. Hypothesizing that genotype-dependent effects on cytokine production might be race-specific, we analyzed steady state cytokine levels after race stratification. Of interest, we found that, among White subjects, nearly all of the cytokines assayed exhibited significant reductions in minor allele carriers (Table S2, Fig. 1). Although robust analysis of White C/C subjects was prevented by their very small number (n = 2), some cytokines exhibited potential allele dose-dependent effects, with lowest levels in C/C subjects (TNF, IL-12, RANTES, IL-4).
Cytokine levels in unstimulated whole blood of White subjects of different rs13361189 genotypes. Whole blood from 30 White subjects of the rs13361189 genotypes shown (n = 20 [T/T]; n = 6 [T/C]; n = 2 [C/C]) was incubated ex vivo for 3 h, after which cytokine concentrations were quantified by multiplex assay. Box and whisker plots depict median and interquartile ranges, and y-axis units depict log-transformed pg/mL values. P values were determined by robust linear regression using a dominant genetic model (T/T vs. T/C and C/C).
Conversely, among AA subjects, a subset of cytokines was increased among minor allele carriers, namely, IL-4, IFNγ, and RANTES (Table S3, Fig. 2). Race interaction p-values were highly significant for nearly all of the cytokines (Table 3), suggesting that the minor allele-cytokine relationship is modified by race. Taken together, these findings suggest that there is a generally opposite relationship of the rs13361189 minor allele to steady state cytokine levels in AA and White subjects, with increases in some cytokines in AA minor allele carriers and decreased cytokines in White minor allele carriers.
Cytokine levels in unstimulated whole blood of African American subjects of different rs13361189 genotypes. Whole blood from 34 African American subjects of the rs13361189 genotypes shown (n = 12 [T/T]; n = 11 [T/C]; n = 8 [C/C]) was incubated ex vivo for 3 h, after which cytokine concentrations were quantified by multiplex assay. Box and whisker plots depict median and interquartile ranges, and y-axis units depict log-transformed pg/mL values. P values were determined by robust linear regression using a dominant genetic model (T/T vs. T/C and C/C).
IRGM risk alleles regulate Toll-like Receptor (TLR)-induced cytokines
To test whether rs13361189 minor-allele carriers have altered inflammatory responsiveness, whole blood was incubated with ligands for TLR2 (Pam3CSK4, heat-killed L. monocytogenes [HKLM]), TLR4 (LPS), TLR5 (flagellin [FLA]), TLR7 (imiquimod [IMIQ]), TLR7/8 (CLO75), and TLR9 (oligodeoxynucleotide [ODN]) and the serum fraction assayed for cytokines. As shown in Table S4, very few genotype-dependent differences in cytokines were observed in the full study cohort. However, stratifying by race, we found that, in White subjects, a subset of TLR ligand-cytokine relationships were significantly altered in rs13361189 minor allele carriers, in almost all cases, with minor allele carriers exhibiting an attenuated response in pro-inflammatory cytokines (Table S5, Fig. 3). In response to Pam3CSK4, induction of the anti-inflammatory cytokine IL-10 was higher in minor allele carriers, whereas RANTES and GM-CSF were lower. Similar attenuated responses in minor allele carriers were observed for FLA (IL-2, RANTES), CLO (IL-2, RANTES), and ODN (IL-2, IL-4, RANTES).
Cytokine levels in whole blood of White subjects of different rs13361189 genotypes stimulated with select TLR ligands. Whole blood from 30 White subjects of the rs13361189 genotypes shown (n = 20 [T/T]; n = 6 [T/C]; n = 2 [C/C]) was stimulated ex vivo for 3 h with the depicted Toll-like Receptor ligands, after which the cytokines indicated were quantified by multiplex assay. Box and whisker plots depict median and interquartile ranges, and y-axis units depict log-transformed pg/mL values. P values were determined by robust linear regression using a dominant genetic model (T/T vs. T/C and C/C). FLA = flagellin; GM-CSF = granulocyte macrophage-colony stimulating factor; HKLM = heat-killed Listeria monocytogenes; IFN = interferon; IL = interleukin; IMIQ = imiquimod; LPS = lipopolysaccharide; MCP = monocyte chemoattractant protein; ODN = oligodeoxynucleotide; RANTES = regulated on activation normal T cell expressed and secreted.
By contrast, among AA subjects, several TLR ligands elicited higher cytokines in minor allele carriers (Table S6, Fig. 4). These included HKLM (IL-2, IFNγ, IL-10), IMIQ (IL-2, IFNγ, IL-12), FLA (IL-1, IL-2, IFNγ, IL-10, RANTES), and CLO75 (IL-2, IFNγ, MCP-1, IL-4, RANTES). Formal interaction analysis revealed several TLR-cytokine relationships that were significantly different between White and AA subjects. Most striking in this regard was RANTES induction, which displayed opposite genotype-dependent responses between White and AA subjects across ligands for TLR2, TLR4, TLR5, and TLR7/8 (HKLM, FLA, LPS, Pam3CSK4, CLO75) (Table S7, Figs. 3, 4). A similar phenomenon was noted for IL-2 (IMIQ, FLA, Pam3CSK4, CLO75) and IFNγ (HKLM, FLA, CLO75). Taken together, minor allele status at rs13361189 is associated in White and AA subjects with opposite directional relationships to steady state and TLR-induced cytokines, with White minor allele carriers in many cases having attenuation of cytokines, whereas AA minor allele carriers exhibit increased induction of cytokines.
Cytokine levels in whole blood of African American subjects of different rs13361189 genotypes stimulated with select TLR ligands. Whole blood from 34 African American subjects of the rs13361189 genotypes shown (n = 12 [T/T]; n = 11 [T/C]; n = 8 [C/C]) was stimulated ex vivo for 3 h with the depicted Toll-like Receptor ligands, after which the cytokines indicated were quantified by multiplex assay. Box and whisker plots depict median and interquartile ranges, and y-axis units depict log-transformed pg/mL values. P values were determined by robust linear regression using a dominant genetic model (T/T vs. T/C and C/C). FLA = flagellin; GM-CSF = granulocyte macrophage-colony stimulating factor; HKLM = heat-killed Listeria monocytogenes; IFN = interferon; IL = interleukin; IMIQ = imiquimod; LPS = lipopolysaccharide; MCP = monocyte chemoattractant protein; ODN = oligodeoxynucleotide; RANTES = regulated on activation normal T cell expressed and secreted.
Discussion
IRGM polymorphisms have been associated with a wide range of human disease, but the preponderance of studies reported to date have been conducted in White populations and very few have directly examined primary immune response phenotypes in subjects with varying IRGM genotypes. Compared to Europeans, African populations have higher IRGM expression and much higher IRGM rs13361189 CD risk allele frequency (~ 0.50 vs. 0.10 [http://useast.ensembl.org]), but lower LD of rs13361189 to the upstream CNV deletion that has been presumed to causally impact IRGM expression16, collectively suggesting that rs13361189 might associate with distinct phenotypes in White and Black subjects. Here, we report that in the overall study population C allele carriers exhibited higher serum IgM, CRP, and CD8+ T cell count. Race stratification revealed that the IgM and CRP changes were largely driven by White subjects, and that White minor allele carriers also displayed increased IgE and decreased frequency of circulating plasmablasts. We also found that the rs13361189 C allele associates with increases in a subset of cytokines in whole blood of AA subjects, but reduced cytokine expression in White subjects.
Intriguing race-specific differences in the amplitude of the innate immune response have recently been documented. Nearly 10% of macrophage-expressed genes exhibit ancestry-related differences in induction during infection, with subjects of African ancestry tending to have stronger inflammatory responses and more robust restriction of intracellular bacterial growth29. These race-specific differences are thought to arise at least in part from higher frequencies in Black than White subjects of alleles associated with increased pro-inflammatory responses29,30. In addition, Africans and AAs reportedly have a higher degree of genetic diversity than other racial groups31 and high genetic diversity of populations has been shown to be associated with more robust immune responses32,33,34,35. African genetic ancestry is associated with a protective effect in infections such as Dengue36.
Several prior examples of race-specific associations of SNPs with infectious diseases have been reported, but the molecular mechanisms have rarely been defined. For example, specific polymorphisms in TLR1, TLR2, and TLR4 associate with tuberculosis risk in some racial groups but not others37, and select TLR1 SNPs are associated with candidemia in Whites but not AAs38. One report also found that the rs10065172 IRGM CD risk allele is associated with tuberculosis in AAs but not Whites22. While there are fewer examples of SNPs with directionally opposite disease associations in different racial/ethnic groups, several have been reported. Thus, the A allele of TLR2 rs5743708 is associated with increased susceptibility to tuberculosis among Asian subjects, but protection among Hispanic subjects39. IL-6 rs1800795 is associated with allergic disease susceptibility among Asians and Caucasians in opposite directions40. The peroxisome proliferator-activated receptor gamma 2 Pro12Ala polymorphism has opposite associations with incident obesity in AAs and Whites41. In other cases, directionally opposite gene × environment interactions have been noted for polymorphisms, such as the C allele of CD14 −260, which associates with higher levels of allergic IgE in children with regular pet contact but lower levels in children regular contact with stable animals42.
The mechanism by which rs13361189 and other polymorphisms confer opposite phenotypic outcomes in different racial/ethnic groups is unclear, but, in principle, could be genetic and/or biochemical. Given the much lower LD of rs13361189 in African populations (r2 = 0.66–0.70) than European populations (r2 = 0.95) with a large CNV deletion upstream of IRGM that has been presumed to causally impact IRGM expression16, it is plausible that there is another linked, causal locus in AAs that drives the association of rs13361189 with cytokine expression. Precedence for this possibility has been shown for the MCP-1 −2581G polymorphism, which associates with increased susceptibility to tuberculosis in Mexican and Korean subjects, but resistance to tuberculosis in Ghanaian subjects, a paradox that has been posited to arise from differences between the populations in LD of the locus to MCP-1 −362C43. Although the IRGM upstream CNV deletion has been shown to associate with directionally opposite changes in IRGM expression in different cell types/lines12, it has been confirmed that the rs13361189 risk allele associates with reduced IRGM expression in African populations similarly to that in White populations16. Studies to date, however, have not directly addressed whether rs13361189 associates differentially with expression of the several reported isoforms of IRGM protein, much less whether it does so in a race-specific manner. Of four described splice isoforms, the IRGMd protein isoform reportedly induces mitochondrial fragmentation and cell death in a concentration-dependent manner44. Given reported large differences in steady state IRGM mRNA expression between White and AA subjects, it is plausible that allele-specific changes in protein expression of select isoforms could lead to differential effects between races on cell biology.
While our study is the first to phenotype cell-level immune function in subjects with different IRGM polymorphisms stratified by race, it nonetheless had several limitations. Due to limited study size, the various cytokine measurements were not adjusted for multiple testing. Although the possibility of false discovery cannot be excluded, the opposing directionality of cytokine expression between White and AA subjects across several treatment conditions was very consistent. Our study was also not adequately powered to address the possibility of sex-specific effects on cytokine expression. Cytokines were also measured in response to a single concentration of stimulus and at a single timepoint, thus not allowing for detection of dose-dependent or temporal effects.
Taken together, we report that the rs13361189 CD risk allele, which has largely been studied at the population level and predominantly in White populations, associates with intriguing changes in the immunophenotype of human subjects. Future, larger studies are warranted, as are fine mapping studies of the IRGM locus that might allow for better understanding of race-specific LD patterns and allelic associations to IRGM isoform expression. Our findings suggest that broad racial inclusion is important in functional studies of the genetic underpinnings of immunity.
Methods
Clinical protocol
Subjects were recruited from the NIEHS Personalized Environment and Genes Study (PEGS), formerly the Environmental Polymorphisms Registry (EPR), which is a repository of DNA and associated demographic data from a cohort of > 18,000 human subjects (~ 2/3 non-Hispanic White, ~ 1/4 non-Hispanic Black, remainder Asian, Hispanic, and Other) in North Carolina45,46. The study was approved by the National Institute of Environmental Health Sciences Institutional Review Board and all participants gave informed consent. All methods were performed in accordance with relevant guidelines and regulations. Exclusion criteria for the participants in the present analysis included age < 18 years, active smoking, use of anti-inflammatory (e.g., non-steroidal anti-inflammatory drugs) or immunosuppressive (e.g., corticosteroids) agents, confirmed/suspected immunodeficiency, and recent gastrointestinal or respiratory illness.
Genotyping of IRGM
DNA was extracted from blood using the Autopure LS system (Qiagen) and IRGM SNPs were genotyped using fluorescence-based allelic TaqMan SNP Genotyping Assays (Applied Biosystems, Life Technologies, Grand Island, NY). TaqMan SNP Genotyping Assays were used, as follows: rs10065172, Assay ID C__30593568_10; rs13361189, Assay ID C__31986315_10; and rs9637876, custom assay. Polymerase chain reactions were performed using 30 ng of genomic DNA isolated from whole blood in a 10ul reaction volume using an Applied Biosystems ViiA-7 Real time PCR machine.
Flow cytometry
In brief, anticoagulated peripheral blood was collected and immediately processed. 100uL of blood was stained with a broad immunophenotyping panel consisting of CD19 APC-Cy7, CD14 AF488, CD56 PE, CD45 PerCP-Cy5.5, CD4 PE-Cy7, CD3 V450, and CD8 BV510 antibodies (BD Biosciences), to identify CD8+ and CD4+ T lymphocytes, CD14+ monocytes, CD56+ NK cells, and CD19+ B lymphocytes. Neutrophils, eosinophils, and basophils were estimated based on SSC vs CD45. After 30 min on ice, the sample was treated with FACS Lyse (BD Biosciences) for 10 min at room temperature, washed, and resuspended in stain buffer. To identify B lymphocyte subsets, 900 µL of blood was lysed with ACK lysis buffer, washed twice with PBS, then stained for 30 min on ice with CD19 APC-Cy7, IgD FITC, CD27 BV786, CD38 PerCP-Cy5.5, CD24 PE-CF594, CD3 V450, and CD95 APC antibodies (BD Biosciences). Antibody details are shown in Table S8. The cells were washed and stained with Zombie Yellow Viability Dye (BioLegend) for 20 min at room temperature. Cells were washed with stain buffer and fixed. CD27+ switched memory, CD27- switched memory, unswitched memory, naïve, transitional, and plasmablast B lymphocyte subsets could be determined from this panel. Thirty thousand CD45+ cells were recorded for the immunophenotyping sample. For the B lymphocyte subset analysis, the entire sample was recorded (~ 2–3 × 106 cells). Samples were acquired on a BD FACS Aria II (BD Biosciences), and analyzed using FlowJo software (Treestar, Ashland, OR). Exemplary flow cytometry gating is shown in Figs. S1 and S2.
Ex vivo whole blood stimulation
As previously described28, blood was drawn from fasting subjects before 10 AM and was anticoagulated with pyrogen-free citrate (0.1 mol/L, pH 7.2), diluted 1:1 with RPMI 1640 medium, and then added to each well of a 96-well plate containing TLR ligands (1 μg/mL Pam3CSK4, 8 × 107 heat-killed Listeria monocytogenes, 1 ng/mL E. coli 0111:B4 LPS, 1 μg/mL flagellin, 1 μg/mL CL075) in quadruplicate. After incubation (3 h, 37 °C, 5% CO2), cells were centrifuged, and supernatants were harvested and stored at − 80 °C until analysis.
Luminex assay
Cytokines were quantified using a multiplex assay (Bio-Plex; Bio-Rad Laboratories, Hercules, CA), as previously described28. Cytokine values were log-transformed and batch-corrected across plates using plate controls (pooled samples present on all plates) with limma’s “removeBatchEffect” (https://doi.org/10.1093/nar/gkv007) using plate identities as batches in R4.1.1.
Clinical laboratory analyses
Complete blood cell count and differentiation, CRP, IgA, IgM, and IgG were run on a Roche Cobas 6000 Analyzer, and IgE by chemiluminescent immunometric assay on Siemens Immulite 2000 XPI (Siemens Healthcare Diagnostics, Flanders, NJ).
Statistical analysis
For analysis of clinical values, variables were first tested for normality and were log-transformed if non-normal. For univariate analysis, we used Fisher’s exact test to compare categorical variables across the genotypes and ANOVA to compare continuous variables. For multivariate regression analysis, robust linear regression47 was used to assess the association between genotypes and cytokine levels, adjusting for age, sex, and race. The regression analysis was performed in the full study population and also separately in AA and White subjects. We also assessed genotype by race (AA vs. White) interaction effects.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Liston, A. & Goris, A. The origins of diversity in human immunity. Nat. Immunol. 19, 209–210. https://doi.org/10.1038/s41590-018-0047-9 (2018).
Arcaroli, J., Fessler, M. B. & Abraham, E. Genetic polymorphisms and sepsis. Shock 24, 300–312 (2005).
Deretic, V. & Levine, B. Autophagy balances inflammation in innate immunity. Autophagy 14, 243–251. https://doi.org/10.1080/15548627.2017.1402992 (2018).
Deretic, V. Autophagy in leukocytes and other cells: Mechanisms, subsystem organization, selectivity, and links to innate immunity. J. Leukoc. Biol. 100, 969–978. https://doi.org/10.1189/jlb.4MR0216-079R (2016).
Brain, O., Cooney, R., Simmons, A. & Jewell, D. Functional consequences of mutations in the autophagy genes in the pathogenesis of Crohn’s disease. Inflamm. Bowel Dis. 18, 778–781. https://doi.org/10.1002/ibd.21832 (2012).
Hua, Y., Shen, M., McDonald, C. & Yao, Q. Autophagy dysfunction in autoinflammatory diseases. J. Autoimmun. 88, 11–20. https://doi.org/10.1016/j.jaut.2017.10.012 (2018).
Lassen, K. G. & Xavier, R. J. Genetic control of autophagy underlies pathogenesis of inflammatory bowel disease. Mucosal Immunol. 10, 589–597. https://doi.org/10.1038/mi.2017.18 (2017).
Chauhan, S., Mandell, M. A. & Deretic, V. IRGM governs the core autophagy machinery to conduct antimicrobial defense. Mol. Cell 58, 507–521. https://doi.org/10.1016/j.molcel.2015.03.020 (2015).
Mehto, S. et al. The Crohn’s disease risk factor IRGM limits NLRP3 inflammasome activation by impeding its assembly and by mediating its selective autophagy. Mol. Cell 73, 429-445.e427. https://doi.org/10.1016/j.molcel.2018.11.018 (2019).
Singh, S. B., Davis, A. S., Taylor, G. A. & Deretic, V. Human IRGM induces autophagy to eliminate intracellular mycobacteria. Science 313, 1438–1441. https://doi.org/10.1126/science.1129577 (2006).
Brest, P. et al. A synonymous variant in IRGM alters a binding site for miR-196 and causes deregulation of IRGM-dependent xenophagy in Crohn’s disease. Nat. Genet. 43, 242–245. https://doi.org/10.1038/ng.762 (2011).
McCarroll, S. A. et al. Deletion polymorphism upstream of IRGM associated with altered IRGM expression and Crohn’s disease. Nat. Genet. 40, 1107–1112. https://doi.org/10.1038/ng.215 (2008).
Ajayi, T. A. et al. Crohn’s disease IRGM risk alleles are associated with altered gene expression in human tissues. Am. J. Physiol. Gastrointest. Liver Physiol. 316, G95–G105. https://doi.org/10.1152/ajpgi.00196.2018 (2019).
Jena, K. K. et al. Autoimmunity gene IRGM suppresses cGAS-STING and RIG-I-MAVS signaling to control interferon response. EMBO Rep. 21, e50051. https://doi.org/10.15252/embr.202050051 (2020).
Parkes, M. et al. Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn’s disease susceptibility. Nat. Genet. 39, 830–832. https://doi.org/10.1038/ng2061 (2007).
Prescott, N. J. et al. Independent and population-specific association of risk variants at the IRGM locus with Crohn’s disease. Hum. Mol. Genet. 19, 1828–1839. https://doi.org/10.1093/hmg/ddq041 (2010).
Palomino-Morales, R. J. et al. Association of ATG16L1 and IRGM genes polymorphisms with inflammatory bowel disease: A meta-analysis approach. Genes Immun. 10, 356–364. https://doi.org/10.1038/gene.2009.25 (2009).
Fisher, S. A. et al. Genetic determinants of ulcerative colitis include the ECM1 locus and five loci implicated in Crohn’s disease. Nat. Genet. 40, 710–712. https://doi.org/10.1038/ng.145 (2008).
Li, Y. et al. Correlation between IRGM genetic polymorphisms and Crohn’s disease risk: A meta-analysis of case-control studies. Genet. Mol. Res. 13, 10741–10753. https://doi.org/10.4238/2014.December.18.15 (2014).
Yang, D., Chen, J., Shi, C., Jing, Z. & Song, N. Autophagy gene polymorphism is associated with susceptibility to leprosy by affecting inflammatory cytokines. Inflammation 37, 593–598. https://doi.org/10.1007/s10753-013-9773-1 (2014).
Yao, Q. M. et al. Polymorphisms in autophagy-related gene IRGM are associated with susceptibility to autoimmune thyroid diseases. Biomed. Res. Int. 2018, 7959707. https://doi.org/10.1155/2018/7959707 (2018).
King, K. Y. et al. Polymorphic allele of human IRGM1 is associated with susceptibility to tuberculosis in African Americans. PLoS ONE 6, e16317. https://doi.org/10.1371/journal.pone.0016317 (2011).
Kimura, T. et al. Autophagy-related IRGM polymorphism is associated with mortality of patients with severe sepsis. PLoS ONE 9, e91522. https://doi.org/10.1371/journal.pone.0091522 (2014).
Liu, J. Z. et al. Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nat. Genet. 47, 979–986. https://doi.org/10.1038/ng.3359 (2015).
Lu, Y., Li, C. Y., Lin, S. S. & Yuan, P. IRGM rs13361189 polymorphism may contribute to susceptibility to Crohn’s disease: A meta-analysis. Exp. Ther. Med. 8, 607–613. https://doi.org/10.3892/etm.2014.1736 (2014).
Kleinnijenhuis, J. et al. Autophagy modulates the Mycobacterium tuberculosis-induced cytokine response. Immunology 134, 341–348. https://doi.org/10.1111/j.1365-2567.2011.03494.x (2011).
Rosentul, D. C. et al. Role of autophagy genetic variants for the risk of Candida infections. Med. Mycol. 52, 333–341. https://doi.org/10.1093/mmy/myt035 (2014).
Gale, S. C. et al. APOε4 is associated with enhanced in vivo innate immune responses in human subjects. J. Allergy Clin. Immunol. 134, 127–134. https://doi.org/10.1016/j.jaci.2014.01.032 (2014).
Nedelec, Y. et al. Genetic ancestry and natural selection drive population differences in immune responses to pathogens. Cell 167, 657-669.e621. https://doi.org/10.1016/j.cell.2016.09.025 (2016).
Ness, R. B., Haggerty, C. L., Harger, G. & Ferrell, R. Differential distribution of allelic variants in cytokine genes among African Americans and White Americans. Am. J. Epidemiol. 160, 1033–1038. https://doi.org/10.1093/aje/kwh325 (2004).
Tishkoff, S. A. et al. The genetic structure and history of Africans and African Americans. Science 324, 1035–1044. https://doi.org/10.1126/science.1172257 (2009).
Hawley, D. M., Sydenstricker, K. V., Kollias, G. V. & Dhondt, A. A. Genetic diversity predicts pathogen resistance and cell-mediated immunocompetence in house finches. Biol. Lett. 1, 326–329. https://doi.org/10.1098/rsbl.2005.0303 (2005).
Meagher, S. Genetic diversity and Capillaria hepatica (Nematoda) prevalence in Michigan deer mouse populations. Evolution 53, 1318–1324. https://doi.org/10.1111/j.1558-5646.1999.tb04547.x (1999).
Whiteman, N. K., Matson, K. D., Bollmer, J. L. & Parker, P. G. Disease ecology in the Galapagos Hawk (Buteo galapagoensis): Host genetic diversity, parasite load and natural antibodies. Proc. Biol. Sci. 273, 797–804. https://doi.org/10.1098/rspb.2005.3396 (2006).
Yuan, D. et al. Scoring the collective effects of SNPs: Association of minor alleles with complex traits in model organisms. Sci. China Life Sci. 57, 876–888. https://doi.org/10.1007/s11427-014-4704-4 (2014).
Chacon-Duque, J. C. et al. African genetic ancestry is associated with a protective effect on Dengue severity in colombian populations. Infect. Genet. Evol. 27, 89–95. https://doi.org/10.1016/j.meegid.2014.07.003 (2014).
Zhou, Y. & Zhang, M. Associations between genetic polymorphisms of TLRs and susceptibility to tuberculosis: A meta-analysis. Innate Immun. 26, 75–83. https://doi.org/10.1177/1753425919862354 (2020).
Plantinga, T. S. et al. Toll-like receptor 1 polymorphisms increase susceptibility to candidemia. J. Infect. Dis. 205, 934–943. https://doi.org/10.1093/infdis/jir867 (2012).
Schurz, H., Daya, M., Moller, M., Hoal, E. G. & Salie, M. TLR1, 2, 4, 6 and 9 variants associated with tuberculosis susceptibility: A systematic review and meta-analysis. PLoS ONE 10, e0139711. https://doi.org/10.1371/journal.pone.0139711 (2015).
Yang, Y. et al. Effects of IL-6 polymorphisms on individual susceptibility to allergic diseases: A systematic review and meta-analysis. Front. Genet. 13, 822091. https://doi.org/10.3389/fgene.2022.822091 (2022).
Fornage, M. et al. Inverse effects of the PPAR(gamma)2 Pro12Ala polymorphism on measures of adiposity over 15 years in African Americans and whites. The CARDIA study. Metabolism 54, 910–917. https://doi.org/10.1016/j.metabol.2005.02.005 (2005).
Eder, W. et al. Opposite effects of CD 14/-260 on serum IgE levels in children raised in different environments. J. Allergy Clin. Immunol. 116, 601–607. https://doi.org/10.1016/j.jaci.2005.05.003 (2005).
Thye, T. et al. MCP-1 promoter variant -362C associated with protection from pulmonary tuberculosis in Ghana, West Africa. Hum. Mol. Genet. 18, 381–388. https://doi.org/10.1093/hmg/ddn352 (2009).
Singh, S. B. et al. Human IRGM regulates autophagy and cell-autonomous immunity functions through mitochondria. Nat. Cell Biol. 12, 1154–1165. https://doi.org/10.1038/ncb2119 (2010).
Chulada, P. C. et al. The Environmental Polymorphisms Registry: A DNA resource to study genetic susceptibility loci. Hum. Genet. 123, 207–214. https://doi.org/10.1007/s00439-007-0457-5 (2008).
Chulada, P. C. et al. The Environmental Polymorphism Registry: A unique resource that facilitates translational research of environmental disease. Environ. Health Perspect. 119, 1523–1527. https://doi.org/10.1289/ehp.1003348 (2011).
Venables, W. N. & Ripley, B. D. Modern Applied Statistics with S (Springer, 2002).
Acknowledgements
This research was supported by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences (Z01 ES102005).
Funding
Open Access funding provided by the National Institutes of Health (NIH).
Author information
Authors and Affiliations
Contributions
T.A., P.R., K.G., J.M.M., K.K., and J.H.M. performed treatments and analyses of whole blood cells, analyzed data, and contributed to writing of the manuscript. M.S., P.K., S.H.S., and M.B.F. graphed and analyzed data and contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ajayi, T., Rai, P., Shi, M. et al. Race-specific association of an IRGM risk allele with cytokine expression in human subjects. Sci Rep 13, 12911 (2023). https://doi.org/10.1038/s41598-023-40313-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40313-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.