Abstract
It remains unknown whether the recent trend of short dual antiplatelet therapy (DAPT) followed by P2Y12 inhibitor monotherapy can simply be applied to patients undergoing complex percutaneous coronary intervention (PCI). We performed a systematic review and meta-analysis to evaluate P2Y12 inhibitor monotherapy vs. conventional DAPT in patients undergoing complex PCI and non-complex PCI (PROSPERO: CRD42022335723). Primary endpoint was the 1-year Net Adverse Clinical Event (NACE). Among 5,323 screened studies, six randomized trials fulfilled the eligibility criteria. A total of 10,588 complex PCI patients (5,269 vs. 5,319 patients) and 25,618 non-complex PCI patients (12,820 vs 12,798 patients) were randomly assigned to P2Y12 inhibitor monotherapy vs. conventional DAPT. In complex PCI patients, P2Y12 inhibitor monotherapy was associated with a lower risk of NACE than conventional DAPT [Odds ratio (OR) 0.76, 95% confidence interval (CI) 0.63–0.91, P = 0.003], whereas in non-complex PCI patients, P2Y12 inhibitor monotherapy was associated with a trend toward lowering the risk of NACE (OR 0.86, 95% CI 0.72–1.02, P = 0.09). This meta-analysis across randomized trials demonstrated that a strategy of short DAPT followed by P2Y12 inhibitor monotherapy reduces the risk of 1-year NACE in patients undergoing complex PCI.
Similar content being viewed by others
Introduction
The Academic Research Consortium (ARC) proposed the new practical definition of patients at high bleeding risk (HBR)1. These ARC-HBR criteria have been validated worldwide2,3,4,5,6. Although bleeding risk is now under intensive discussion in the interventional field, a thrombotic event remains an important concern for interventional cardiologists. In particular, complex PCI is considered to be an important thrombotic risk factor, and many interventional cardiologists believe that patients undergoing complex PCI should be prescribed relatively long dual antiplatelet therapy (DAPT) to prevent stent thrombosis. This was true in the era of DAPT followed by aspirin monotherapy7. In 2016, for example, Giustino et al. conducted a large-scale patient-level meta-analysis involving 6 randomized controlled trials7, and reported that compared with short-term DAPT, long-term DAPT yielded significant reductions in major adverse cardiovascular events (MACE) in the complex PCI group vs. the non-complex PCI group. However, the current mainstream of antithrombotic therapy is a short DAPT followed by P2Y12 inhibitor monotherapy. Bianco et al. performed a meta-analysis of recent trials comparing long DAPT vs. short DAPT followed by P2Y12 inhibitor monotherapy8. The study showed that short DAPT followed by P2Y12 inhibitor monotherapy was associated with a lower incidence of clinically relevant bleeding compared to 12-month DAPT with no significant differences in terms of cardiovascular events at 1-year follow-up. Nevertheless, it remains unknown whether this can simply be applied to patients undergoing complex PCI.
Several sub-analyses focusing on P2Y12 inhibitor monotherapy in patients with complex PCI have recently been reported9,10,11,12,13,14. Here, we performed a systematic review and meta-analysis to investigate the impact of short DAPT followed by P2Y12 inhibitor monotherapy on clinical outcomes in patients undergoing complex PCI.
Methods
Study search and eligibility criteria
We performed a systematic review and meta-analysis to evaluate P2Y12 inhibitor monotherapy vs. conventional DAPT in patients undergoing complex PCI and non-complex PCI (PROSPERO: CRD42022335723). P2Y12 inhibitor monotherapy was defined as a short DAPT (up to 3 months) followed by P2Y12 inhibitor monotherapy. Conventional DAPT was defined as a standard course of DAPT of 6–12 months followed by either aspirin or P2Y12 inhibitor monotherapy. Inclusion criteria were as follows: (1) randomized design comparing short DAPT (up to 3 months) followed by P2Y12 inhibitor monotherapy against standard DAPT, (2) use of contemporary drug-eluting stents, (3) follow-up duration ≥ 12 months, and (4) stratified analysis according to complex PCI. PubMed and Web of Science were searched from the inception of each database up to June 8th, 2022, with no restriction on language or publication status. Two investigators (YS and YM) independently assessed publications for eligibility at the title and/or abstract level, with divergences resolved by a third investigator (SH). We performed the systematic search using the following code: ((complex PCI) OR (high ischemic risk)) AND ((antiplatelet therapy) OR (monotherapy)). Because the present meta-analysis was based on data extracted from previously published research, the data and study materials are available to other researchers for purposes of reproducing the results or replicating the procedure. The analytic methods are outlined as follows.
Data extraction and quality assessment
The following data were extracted independently by two reviewers using a standardized data abstraction form: the study year of publication, study design, inclusion and exclusion criteria, sample size, patients’ baseline characteristics, P2Y12 inhibitor used, endpoint definitions, complex PCI definitions, clinical outcomes, and follow-up duration. Quality assessment of RCTs was based on the Cochrane risk of bias tool for randomized controlled trials considering the following criteria: random sequence generation, allocation concealment, selective reporting, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and other sources of bias. We classified bias of the trials as low, high, or unclear.
Study endpoints
Primary endpoint was the Net Adverse Clinical Event (NACE), which is a composite of major bleeding and major adverse cardiac and cerebrovascular events (MACCE) (Table 1) at 1-year follow-up. Secondary endpoints were bleeding endpoint (major bleeding) and all individual components of MACCE (all-cause death, myocardial infarction, stent thrombosis, and stroke) at 1-year follow-up. Since definitions of clinical endpoints were as prespecified in the individual trials, several discrepancies in definitions were present. Specifically, repeat revascularization was included in NACE in the GLOBAL LEADERS and TICO trials but not in the other trials. Stroke reported by TWILIGHT did not include hemorrhagic stroke but only ischemic stroke. Stent thrombosis was reported according to the Academic Research Consortium (ARC) definite or probable definition, except for data from GLOBAL LEADERS in which it was reported as ARC definite. Bleeding events were according to the Bleeding Academic Research Consortium (BARC) or Thrombolysis in Myocardial Infarction (TIMI) definitions. Event rates reported by TWILIGHT were at 15 months rather than 12 months. Due to limited access to the outcome data, we used these reported data as summarized in Table 1.
Complex PCI
The original definitions used in each trial are summarized in Table 2. Complex PCI was previously defined as including at least one of the following criteria: (1) chronic total occlusion, (2) stent length > 60 mm, (3) bifurcation with 2 stents, (4) ≥ 3 lesions treated, (5) ≥ 3 stents implanted, and (6) ≥ 3 vessels treated7. All trials used similar definitions, with slight differences. For the current analysis, we used the original definition in each trial. In the sub-analysis of the TICO trial only, patients were divided into high-ischemic vs. non-high-ischemic groups, in which the definition of high-ischemic included not only complex PCI but also diabetes mellitus and chronic kidney disease.
Statistical analysis
We performed the present systematic review and meta-analysis in accordance with the recommendations of the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Analysis was performed on an intention-to-treat basis. Categorical variables are reported as percentages, and continuous variables as mean ± SD or median (interquartile range), as appropriate. A weighted average of odds ratios (OR) and 95% confidence intervals (CI) was calculated using a random-effects model, with the estimate of heterogeneity obtained using the Mantel–Haenszel method. The presence of heterogeneity among studies and subgroups was evaluated with the I2 statistic and the Cochran’s Q test. I2 values of 25%, 50%, and 75% represents mild, moderate, and severe inconsistency, respectively. A P value < 0.05 for the Cochran’s Q test was considered to indicate heterogeneity. The possibility of small study effects resulting from publication bias or other biases was examined for all endpoints by means of visual inspection of funnel plots of the ORs of individual trials against their standard errors15,16. We performed several sensitivity analyses to confirm the robustness of the findings. First, a sensitivity analysis was performed excluding the MASTER-DAPT trial, because the trial included patients treated with aspirin monotherapy at approximately 30%. Second, the TICO trial divided patients into high-ischemic vs non-high-ischemic risk groups, in which the high-ischemic risk included not only complex PCI but also clinical risk factors (diabetes mellitus and chronic kidney disease). In the main analysis, we used the original categorization of high-ischemic risk. Based on the published data, we could compute the event rates in patients exclusively with complex PCI only for the endpoints of NACE, MACCE, and major bleeding, and not for the other endpoints. Therefore, we performed sensitivity analyses with these computed data only for the available endpoints. Third, we conducted a sensitivity analysis without TWILIGHT trial for the NACE because NACE for complex and non-complex PCI subgroups was not reported in the trial. We calculated the event numbers as the sum of ischemic and bleeding events in a non-hierarchical manner. Lastly, since only GLOBAL LEADERS and TICO included revascularization in NACE and MACCE, we repeated the analysis without these trials. All analyses were performed using RevMan (Review Manager Version 5.3, The Cochrane Collaboration, Copenhagen, Denmark). A P value < 0.05 was considered significant. This study is registered with PROSPERO, CRD42022335723.
Results
Study subjects
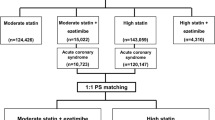
Among 5323 records screened from our search strategy, we finally included 6 studies in the meta-analysis (Fig. 1). Major characteristics of the trials are tabulated in Supplemental Table S1. Quality assessment of the trials is summarized in the Supplemental Table S2. A total of 10,588 complex PCI patients (5269 vs. 5319 patients) and 25,618 non-complex PCI patients (12,820 vs 12,798 patients) were randomly assigned to short DAPT followed by P2Y12 inhibitor monotherapy vs. conventional DAPT. Baseline characteristics of the clinical trials are summarized in Table 3. Around half of the overall population presented with acute coronary syndrome (ACS). The funnel plots are presented in Supplemental Fig. S1. Certain funnel plots exhibited asymmetrical patterns, potentially attributable to factors such as publication bias, variations in the characteristics of the included patients, and disparities in the employed P2Y12 inhibitors.
Impact of P2Y12 inhibitor monotherapy in complex PCI and non-complex PCI
Primary endpoint
Results of the primary endpoint are summarized in Fig. 2. In complex PCI patients, P2Y12 inhibitor monotherapy was associated with a lower risk of NACE than conventional DAPT [7.6% vs. 9.8%, Odds ratio (OR) 0.76, 95% confidence interval (CI) 0.63–0.91, P = 0.003], whereas in non-complex PCI patients, P2Y12 inhibitor monotherapy was associated with a trend toward lowering the risk of NACE (6.3% vs. 6.7%, OR 0.86, 95% CI 0.72–1.02, P = 0.09). No heterogeneity was found between complex and non-complex PCI patients (I2 = 0%, P = 0.33).
Bleeding endpoint
Results of bleeding event are summarized in Fig. 3. Both in complex and non-complex PCI patients, P2Y12 inhibitor monotherapy was associated with a lower risk of major bleeding than conventional DAPT (complex PCI, OR 0.65, 95% CI 0.47–0.91, P = 0.01; non-complex PCI, OR 0.68, 95% CI 0.50–0.92, P = 0.01). The results were consistent across complex and non-complex PCI patients (I2 = 0%, P = 0.86).
MACCE and its individual components
Results of the ischemic endpoint are summarized in Fig. 4. P2Y12 inhibitor monotherapy was associated with a lower risk of MACCE in complex PCI patients (OR 0.81, 95% CI 0.69–0.94, P = 0.005), but was not associated with a lower risk in non-complex PCI patients (OR 1.02, 95% CI 0.91–1.14, P = 0.71) (I2 = 83.6%, P = 0.01). The endpoints of all-cause death, myocardial infarction, stent thrombosis, and stroke did not differ between P2Y12 inhibitor monotherapy and conventional DAPT in both complex PCI and non-complex PCI patient groups.
Sensitivity analyses
All these analyses were repeated following exclusion of the MASTER-DAPT trial as a sensitivity analysis. Overall, results were found to be consistent (Supplemental Figs. S2, S3, S4). Results of another sensitivity analysis with computed results of pure population with complex PCI in the TICO trial were also totally consistent with the main analysis (NACE, Supplemental Fig. S5; MACCE, Supplemental Fig. S6; Major bleeding, Supplemental Fig. S7). Another sensitivity analysis for NACE without TWILIGHT trial is illustrated in Supplemental Fig. S8. The result was consistent with the main analysis. The final sensitivity analyses for NACE and MACCE, excluding GLOBAL LEADERS and TICO, are presented in Supplemental Figs. S9 and S10, respectively. While the point estimates for NACE suggested a beneficial impact of P2Y12 inhibitor monotherapy in individuals undergoing complex PCI and non-complex PCI, these findings did not attain statistical significance. Moreover, there were no notable disparities in MACCE rates between the P2Y12 inhibitor monotherapy and conventional DAPT groups within both the complex PCI and non-complex PCI patient cohorts.
Discussion
We conducted this meta-analysis to investigate whether a short DAPT followed by P2Y12 inhibitor monotherapy influences clinical outcome in patients undergoing complex or non-complex PCI. Compared with conventional DAPT, short DAPT followed by P2Y12 inhibitor monotherapy was (1) associated with a lower risk of 1-year NACE in complex PCI patients; (2) associated with a trend toward lowering the risk of NACE in non-complex PCI patients; (3) associated with a lower risk of 1-year major bleeding both in complex and non-complex PCI patients; and (4) associated with a lower risk of 1-year MACCE in complex PCI patients only, and not in non-complex PCI patients.
The most recent large-scale analysis on this topic was reported by Giustino et al.7, who found that that prolonged (12–24 months) DAPT reduced major adverse cardiac events and coronary thrombotic events compared with short (3–6 months) DAPT after complex PCI in the patient-level pooled analysis of 6 RCTs7. Accordingly, European Society of Cardiology and Japanese Circulation Society guidelines have suggested that complex PCI is a risk factor of stent-driven recurrent ischemic events17,18. Given this background, many interventional cardiologists seem reluctant to choose a short DAPT strategy in patients undergoing complex PCI despite the recent favorable data of P2Y12 inhibitor monotherapy. However, recent sub-analyses from the GLOBAL LEADERS, STOPDAPT2, TICO, TWILIGHT, SMART-CHOICE, and MASTER-DAPT trials showed consistent and somewhat unexpected results for interventional cardiologists9,10,11,12,13,14, namely that the short DAPT strategy works even better in complex PCI patients than in non-complex PCI patients. To confirm the robustness of this finding, we conducted the current meta-analysis. Along the same line with the recent meta-analyses without MASTER-DAPT trial19,20, we found that short DAPT followed by P2Y12 inhibitor monotherapy was associated with a lower risk of NACE, MACCE, and major bleeding than conventional DAPT in complex PCI patients. In non-complex PCI patients, P2Y12 inhibitor monotherapy was associated with a trend toward lowering the risk of NACE and a lower risk of major bleeding, but not with MACCE. The discrepancy between the previous and this meta-analysis might be explained by the use of P2Y12 inhibitor monotherapy after DAPT in the recent trials over aspirin used in the previous trials7. The recent antiplatelet regimen with an initial short-term duration of DAPT to prevent stent-related thrombotic events followed by a long-term course of a potent P2Y12 inhibitor alone has been expected to reduce the excess of aspirin-related bleeding without reducing anti-ischemic efficacy. The antiplatelet effect of P2Y12 inhibitor monotherapy might be strong enough to afford protection against ischemic events regardless of PCI complexity.
It has been reported that patients with complex PCI were at higher bleeding risk than those without because of overlapping risk factors9,17,18. Indeed, in this meta-analysis, patients undergoing complex PCI more frequently experienced major bleeding events than those undergoing non-complex PCI [2.40% (254/10,588) vs 1.61% (412/25,618), Fig. 3]. This may be because the more complex CAD a patient has, the more comorbidity burdens the patient is likely to have. Complex CAD is attributed to such comorbidities, but these often exist as bleeding risks at the same time. Patients with multiple HBR criteria have a higher bleeding risk than those with a single HBR criterion21,22,23. Therefore, if we consider the balance between bleeding and thrombotic events, bleeding risk may be particularly weighted in complex PCI patients.
It is worth mentioning that the utilization of P2Y12 inhibitor monotherapy was associated not only with a decreased risk of bleeding but also with a reduction in MACCE occurrence in patients undergoing complex PCI. However, it is important to note that this finding, which exhibited consistency across the trials included in this meta-analysis (I2 = 0%), was primarily driven by the outcomes of the GLOBAL LEADERS and TICO trials, wherein repeat revascularization was considered within the composite endpoint. Our sensitivity analysis, excluding these trials, revealed an insignificant impact of P2Y12 inhibitor monotherapy, in contrast to the main findings. Similarly, a meta-analysis conducted by Gragnano et al., employing pooled patient-level data, also failed to demonstrate a significant effect of short-DAPT followed by P2Y12 inhibitor monotherapy in relation to ischemic composite endpoints (comprising all-cause death, myocardial infarction, and stroke) when compared to the conventional DAPT strategy in both complex and non-complex PCI patients (complex PCI, hazard ratio [HR] 0.87, 95% confidence interval [CI] 0.64–1.19; non-complex PCI, HR 0.91, 95% CI 0.76–1.09)24. Therefore, while this antithrombotic regimen may provide protection against bleeding complications, its impact on severe ischemic events, as suggested by the individual trial results, may not be statistically significant.
Clinical implications
The most important message of this meta-analysis is that PCI complexity does not justify a more prolonged course of DAPT, or rather that it warrants short DAPT followed by P2Y12 inhibitor monotherapy. This is supported by the report from Urban et al. showing that a complex PCI procedure was significantly associated with increased risk of both thrombotic and bleeding events25. However, the generalizability of the current findings should be carefully considered. First, the applicability of our results to ACS patients should be carefully considered. Although a recent meta-analysis of 9 RCTs consisting of 25,907 ACS patients suggested that 1–3 months of DAPT has similar efficacy in preventing ischemic events with reduced bleeding risk compared with 6 to 12 months of DAPT26, ACS with complex PCI is likely to be a strong ischemic risk factor. Second, ticagrelor or clopidogrel were mainly evaluated in the included trials. However, this meta-analysis did not address any preferred P2Y12 inhibitors. Further research should investigate which P2Y12 inhibitor is the drug of choice after discontinuing DAPT in complex PCI patients. Third, although the extent and complexity of complex PCI was not found to be associated with MACCE (all-cause death, MI, or stroke) in the TWILIGHT trial10, the relationship between PCI complexity and clinical events could not be precisely assessed in this study-level meta-analysis. Patient-level meta-analysis will provide important insights into this point.
Study limitations
Several limitations of this meta-analysis should be acknowledged. First, the study designs of the 6 included trials differed, including in their use of placebo, choice of P2Y12 inhibitor, use of oral anticoagulation, proportion of acute coronary syndrome, and timing of randomization. Second, the study was conducted as a study-level meta-analysis, and not as a patient-level meta-analysis. Third, the definition of primary endpoint differed slightly among the included trials (Table 1); in particular, GLOBAL-LEADERS and TICO included revascularization in the endpoint, resulting in relatively larger event numbers than the other trials. Stroke reported from TWILIGHT included only ischemic stroke, and not hemorrhagic stroke. The MASTER DAPT trial included approximately 30% patients taking aspirin monotherapy. This small proportion of aspirin monotherapy may have resulted in noise in the analysis, albeit that the population with aspirin monotherapy is markedly limited compared to the overall population. To confirm the robustness of the findings, we performed several sensitivity analyses and found that the overall results were consistent with the main results. Fourth, because the report from the TWILIGHT did not provide NACE, we computed the event numbers using the data for ischemic and bleeding events. However, this calculation was non-hierarchical. The numbers used in this meta-analysis are therefore likely overestimated to a certain degree. Fifth, the TICO trial divided patients into high-ischemic vs non-high-ischemic risk groups, wherein the high-ischemic risk included not only complex PCI but also clinical risk factors (diabetes mellitus and chronic kidney disease). This may have somewhat influenced the results, although our sensitivity analysis demonstrated consistent findings. Lastly, around 10% of patients in the standard DAPT arm in MASTER-DAPT trial received short DAPT and subsequent P2Y12 inhibitor monotherapy (with complex PCI, 11.8%; with non-complex PCI, 9.1% at 3 months visit)14. Although there were instances of crossovers across all the studies, the specific details regarding these crossovers and their distribution within the subgroups of complex PCI and non-complex PCI were not available.
Conclusions
This meta-analysis across randomized trials demonstrated that a strategy of short DAPT followed by P2Y12 inhibitor monotherapy reduces the risk of NACE in patients undergoing complex PCI. PCI complexity does not justify a more prolonged course of DAPT, or rather warrants short DAPT followed by P2Y12 inhibitor monotherapy.
Data availability
The authors confirm that the data supporting the findings of this study are available within the referenced articles and their supplementary materials.
References
Urban, P. et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention. Circulation 140, 240–261. https://doi.org/10.1161/CIRCULATIONAHA.119.040167 (2019).
Cao, D. et al. Validation of the academic research consortium high bleeding risk definition in contemporary PCI patients. J. Am. Coll. Cardiol. 75, 2711–2722. https://doi.org/10.1016/j.jacc.2020.03.070 (2020).
Nakamura, M. et al. High bleeding risk and clinical outcomes in East Asian patients undergoing percutaneous coronary intervention: The PENDULUM registry. EuroIntervention 16, 1154–1162. https://doi.org/10.4244/EIJ-D-20-00345 (2021).
Ueki, Y. et al. Validation of the Academic Research Consortium for High Bleeding Risk (ARC-HBR) criteria in patients undergoing percutaneous coronary intervention and comparison with contemporary bleeding risk scores. EuroIntervention 16, 371–379. https://doi.org/10.4244/EIJ-D-20-00052 (2020).
Watanabe, H. et al. Details on the effect of very short dual antiplatelet therapy after drug-eluting stent implantation in patients with high bleeding risk: Insight from the STOPDAPT-2 trial. Cardiovasc. Interv. Ther. 36, 91–103. https://doi.org/10.1007/s12928-020-00651-9 (2021).
Natsuaki, M. et al. Application of the academic research consortium high bleeding risk criteria in an all-comers registry of percutaneous coronary intervention. Circ. Cardiovasc. Interv. 12, e008307. https://doi.org/10.1161/CIRCINTERVENTIONS.119.008307 (2019).
Giustino, G. et al. Efficacy and safety of dual antiplatelet therapy after complex PCI. J. Am. Coll. Cardiol. 68, 1851–1864. https://doi.org/10.1016/j.jacc.2016.07.760 (2016).
Bianco, M. et al. P2Y12 inhibitors monotherapy after short course of dual antiplatelet therapy in patients undergoing percutaneous coronary intervention: A meta-analysis of randomized clinical trials including 29 089 patients. Eur. Heart J. Cardiovasc. Pharmacother. 7, 196–205. https://doi.org/10.1093/ehjcvp/pvaa038 (2021).
Serruys, P. W. et al. Impact of long-term ticagrelor monotherapy following 1-month dual antiplatelet therapy in patients who underwent complex percutaneous coronary intervention: Insights from the Global Leaders trial. Eur. Heart J. 40, 2595–2604. https://doi.org/10.1093/eurheartj/ehz453 (2019).
Dangas, G. et al. Ticagrelor with or without aspirin after complex PCI. J. Am. Coll. Cardiol. 75, 2414–2424. https://doi.org/10.1016/j.jacc.2020.03.011 (2020).
Roh, J. W. et al. P2Y12 inhibitor monotherapy in complex percutaneous coronary intervention: A post-hoc analysis of SMART-CHOICE randomized clinical trial. Cardiol. J. 28, 855–863. https://doi.org/10.5603/CJ.a2021.0101 (2021).
Yamamoto, K. et al. Very short dual antiplatelet therapy after drug-eluting stent implantation in patients who underwent complex percutaneous coronary intervention: Insight from the STOPDAPT-2 trial. Circ. Cardiovasc. Interv. 14, e010384. https://doi.org/10.1161/CIRCINTERVENTIONS.120.010384 (2021).
Lee, S. J. et al. Ticagrelor monotherapy versus ticagrelor with aspirin in acute coronary syndrome patients with a high risk of ischemic events. Circ. Cardiovasc. Interv. 14, e010812. https://doi.org/10.1161/CIRCINTERVENTIONS.121.010812 (2021).
Valgimigli, M. et al. Duration of antiplatelet therapy after complex percutaneous coronary intervention in patients at high bleeding risk: A MASTER DAPT trial sub-analysis. Eur. Heart J. https://doi.org/10.1093/eurheartj/ehac284 (2022).
Sterne, J. A. et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343, d4002. https://doi.org/10.1136/bmj.d4002 (2011).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. https://doi.org/10.1136/bmj.315.7109.629 (1997).
Nakamura, M. et al. JCS 2020 guideline focused update on antithrombotic therapy in patients with coronary artery disease. Circ. J. 84, 831–865. https://doi.org/10.1253/circj.CJ-19-1109 (2020).
Valgimigli, M. et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The task force for dual antiplatelet therapy in coronary artery disease of the European society of cardiology (ESC) and of the European association for cardio-thoracic surgery (EACTS). Eur. Heart J. 39, 213–260. https://doi.org/10.1093/eurheartj/ehx419 (2018).
Oliva, A. et al. P2Y12 inhibitors monotherapy in patients undergoing complex vs non-complex percutaneous coronary intervention: A meta-analysis of randomized trials. Am. Heart J. 255, 71–81. https://doi.org/10.1016/j.ahj.2022.10.006 (2023).
Nicolas, J. et al. Efficacy and safety of P2Y12 inhibitor monotherapy after complex PCI: A collaborative systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Pharmacother. https://doi.org/10.1093/ehjcvp/pvac071 (2022).
Sotomi, Y. et al. Prevalence of the Japanese high bleeding risk criteria and its prognostic significance for fatal bleeding in patients with acute myocardial infarction. Heart Vessels 36, 1484–1495. https://doi.org/10.1007/s00380-021-01836-9 (2021).
Sotomi, Y. et al. Practical assessment of the tradeoff between fatal bleeding and coronary thrombotic risks using the academic research consortium for high bleeding risk criteria. J. Atheroscler. Thromb. https://doi.org/10.5551/jat.62999 (2021).
Natsuaki, M. et al. Application of the modified high bleeding risk criteria for japanese patients in an all-comers registry of percutaneous coronary intervention—from the CREDO-Kyoto Registry Cohort-3. Circ. J. 85, 769–781. https://doi.org/10.1253/circj.CJ-20-0836 (2021).
Gragnano, F. et al. P2Y(12) inhibitor monotherapy or dual antiplatelet therapy after complex percutaneous coronary interventions. J. Am. Coll. Cardiol. 81, 537–552. https://doi.org/10.1016/j.jacc.2022.11.041 (2023).
Urban, P. et al. Assessing the risks of bleeding vs thrombotic events in patients at high bleeding risk after coronary stent implantation: The ARC-high bleeding risk trade-off model. JAMA Cardiol. 6, 410–419. https://doi.org/10.1001/jamacardio.2020.6814 (2021).
Park, D. Y. et al. Shortening the duration of dual antiplatelet therapy after percutaneous coronary intervention for acute coronary syndrome: A systematic review and meta-analysis. Am. Heart J. 251, 101–114. https://doi.org/10.1016/j.ahj.2022.05.019 (2022).
Author information
Authors and Affiliations
Contributions
Y.S., Y.M., and S.H. conceived of the study concept and design. Y.S. and Y.M. did the literature searches and analyzed the data. Y.S., Y.M. and S.H. wrote the draft of manuscript. All authors reviewed the manuscript and approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sotomi, Y., Matsuoka, Y., Hikoso, S. et al. P2Y12 inhibitor monotherapy after complex percutaneous coronary intervention: a systematic review and meta-analysis of randomized clinical trials. Sci Rep 13, 12608 (2023). https://doi.org/10.1038/s41598-023-39213-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-39213-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.