Abstract
Chronic pain alters the experience of owning a body and leads to disturbances in bodily perception. We tested whether women with fibromyalgia (FM) are receptive to bodily illusions of owning a visible and progressively invisible body in immersive virtual reality (VR), and what modulates this experience. Twenty patients participated in two experimental sessions; each session included two conditions in a counterbalanced order. We found that patients with FM could indeed experience virtual embodiment. Sentiment analysis revealed significantly more positive reactions to the progressively invisible body, yet twice as many patients declared they preferred the illusion of a visible virtual body. A linear mixed model revealed that the strength of embodiment was positively associated with body perception disturbances and negatively associated with FM symptoms intensity. No effect of pain during the VR experience nor interoception awareness on embodiment was found. The results indicated that patients with FM are receptive to virtual bodily illusions and that the impact of the embodiment depends on affective reactions, the level of cognitive body distortions, and the intensity of symptoms. Importantly, there is a large variation among patients which should be considered in future VR-based interventions.
Similar content being viewed by others
Introduction
Pain is a bodily sensation that connects the neural correlates of pain perception and body representation. It is not only a distinct sensation but also a piece of information about our bodies1. In fibromyalgia (FM), the most common symptoms are a generalized chronic pain in muscles and fibrous connective tissue (ligaments and tendons) described as ‘pain of everything’, joint stiffness, and chronic fatigue. Patients tend to report multiple soft tissue ‘tender points’ that are especially painful2. While specific pain location might change from 1 day to another, pain and fatigue are felt over the whole body. Patients with FM have enhanced sensitivity to aversive and non-aversive stimuli which is linked to altered interoception3. Cognitive modulation of pain and interoceptive perception can be influenced by various factors including attention, beliefs, conditioning, expectations, mood, and the regulation of the emotional response to sensory events4,5,6.
The perception of pain, its multisensory influences, non-aversive sensations arising from within the body, and the sense of body ownership are all closely related7,8. Thus, the intensity of pain can, to a certain degree, be modulated through bodily sensations and their manipulation. For example, in patients with chronic low back pain, visual feedback of one’s low back reduces pain intensity compared with visual hand feedback or controls9. Chronic pain is associated with changes in sensorimotor processing, mostly evident in the form of motor deficits, sensory changes, and body representation distortions10,11. Brun et al.12 demonstrated a positive correlation between pain intensity and conflict-induced sensorimotor disturbances, with patients with FM and complex regional pain syndrome (CRPS) being more prone to report disturbances than patients with arthritis and healthy participants. Patients with FM often present with an unstable body schema (the representation of a body for action planning and control)13, negative attitudes toward their bodies, and increased vigilance to their bodily signals14. Altogether, the body-pain relationship in patients with FM is complicated and can be described as a paradox:
[T]he intensification of fibromyalgia pain does in fact affect different aspects of body awareness: in particular, experienced body size, weight, and localization, as well as the experience of owning one’s own body. In addition, these disruptions in patient’s body awareness have as a result, a modification of the experience of pain, leading to the apparently paradoxical experience of being in pain while not feeling it5.
The sensation of ownership of our (real) body is, under physiological conditions, a stable experience that is critical for sensorimotor interactions with the environment. Despite such stability, it can be easily modified15, for example in the well-known rubber hand illusion, in which synchronous visuotactile stimulation leads to an illusion of ownership over a rubber arm16. Immersive VR has opened up further possibilities for inducing and experiencing body illusions17. In immersive VR technology, a computer-generated 3D audiovisual environment is experienced on a head-mounted display (HMD), replacing the user’s sensory inputs from the real world. In VR, a life-sized virtual body can be programmed to substitute the participant’s real body. Hence, when looking down towards themselves they will see a virtual body rather than their real one. Through real-time tracking the virtual body can be programmed to move synchronously and in correspondence with real body movements, and when an object is seen to touch the virtual body this touch can be felt on the real body (e.g. through vibrotactile stimulation). This setup typically gives rise to a sensation of ownership over the virtual body (termed embodiment). Embodiment consists of three subcomponents: the body ownership illusion (This is my body), agency (I control my body), and the sense of self-location (I am where my body is)18. It is still possible to experience an embodiment illusion when some of these conditions are modified, for example, when the user’s point of view is outside the body (e.g. in a third-person perspective)19 or the virtual body does not resemble one’s real body (e.g. in size, colour, or gender)20. The feeling of ownership over an external dummy or virtual body (or body part) has both physiological and behavioural consequences. For example, the vision of one’s own body can modulate pain perception21. Furthermore, seeing a virtual arm can significantly increase the thermal pain threshold, independently of attentional and stimulus adaptation processes22,23. When a subject observes the skin colour of their virtual arm dynamically changing, this can modulate pain sensitivity. In particular, a reddened arm significantly decreases the pain threshold compared with normal and bluish skin23.
A key feature of VR is the possibility of inducing manipulations that are otherwise impossible, such as making the body (semi)transparent, what can modulate the threshold to pain. In a study on healthy participants, Martini et al.24 demonstrated that viewing one’s semi-transparent body may reduce the ownership over that body. Still, participants that did report stronger body ownership of a semi-transparent body had a lower pain threshold in this condition, an observation that was suggested to be related to the unpredictability of potential harmful stimuli.
If owning a semi-transparent virtual body increased pain sensitivity (or decreased pain threshold), this would not seem a good strategy to treat chronic pain. However, the modulation of pain threshold that was observed in healthy subjects is not a good predictor of how such manipulations influence chronic pain. For example, making a virtual arm semi-transparent diminished pain ratings in patients with CRPS, but had no effect in patients with peripheral nerve injury25. This suggests that body transparency may modulate pain under certain conditions, and such manipulations are increasingly being tested in pain research and treatment26,27,28.
Some fibromyalgia patients report a disruption in their body perception, leading to disembodiment5, as a result of the body in FM being painful and ‘problematic’. Here, our aim was to evaluate whether it is possible for patients with FM to experience being embodied in a virtual body and then disembodied by observing it progressively becoming invisible. In a second step, we investigated this potential dual role of progressive invisibility in lowering pain threshold (as demonstrated in the pain-free population) while decreasing pain intensity (as demonstrated in patients with CRPS). Since the population of patients with FM is characterized by high heterogeneity of both psychological and physiological characteristics29, we applied a mixed methods design which allowed for a deeper understanding of the unique experience.
Methods
The study was carried out in compliance with the Declaration of Helsinki (Fortaleza, Brazil, October 2013) in addition to the Law 14/2007 of July 3 on Biomedical Research. The experimental protocol was approved by the Clinical Research Ethics Committee of the Hospital Clínic of Barcelona (HCB/2021/0501). Written informed consent was obtained from all patients before being included in the study.
We carried out a within-group experiment with two conditions, the visible and progressively invisible bodies, presented in a counterbalanced order across two sessions. Repeated measures were used to control for the inference of the novelty effect of VR, the order of conditions, and daily fluctuations of symptoms.
Sample
Twenty-one female patients with FM were recruited for the study. The sample size was established on the basis of the minimal sample size (N = 15) calculated in g*Power 3.1 for a repeated-measures ANOVA (within factors), assuming effect size d = 0.4 and power 0.80.
The inclusion and exclusion criteria can be found in Supplementary Information (p.1). One patient withdrew from the study, due to the physical discomfort experienced in the first session, and thus 20 patients were included in the analyses. The mean age of the group was 43 (SD = 5) years (min = 36, max = 55), and the mean number of years lived with the diagnosis of FM was 9 (SD = 12). Two patients claiming that they had symptoms all their life, but the majority (12 patients) were diagnosed within the last 5 years. The group had diverse levels of education, from primary school (N = 5) to secondary or high school (N = 8) to a university degree (N = 5; other N = 1).
Study design and experimental procedure
The experiment consisted of two identical sessions that lasted approximately 30 min each. There was 1 week between the sessions. The study was carried out at the Hospital Clinic Barcelona, and a COVID-19 protocol was applied to minimise cross-infection risk. Data were collected from April to September 2021. Participants were greeted by the experimenter and asked to read and sign the patient information sheet and the informed consent form. The demographic data were collected separately from the consent form. Patients then filled in the pre-study questionnaires and were instructed how to use the head-mounted display (HMD). Finally, the VR scene was displayed (Fig. 1).
There were two scenes, one with a visible body and one with the progressively invisible body condition (called invisible body) presented in a pseudo-randomized order (Fig. 2). During the experience, participants were asked three times about their current pain level (immediately after donning the HMD and after each scene). After each condition, they were also asked to respond out loud and describe how they felt during the experience. Their answers were recorded in an audio format. After the last pain measurement, the experience ended, and the experimenter assisted participants with the removal of the equipment. Finally, participants answered several embodiment-related questions and indicated their preferred scene. Finally, they were debriefed and thanked for their participation.
Procedure in virtual reality
-
1.
Participants saw a calibration screen (10 s).
-
2.
Participants were asked about their pain level (baseline) and responded by selecting a number from 0 to 100 on a visual analogue scale (15 s).
-
3.
The virtual room scene was displayed, and participants could see their virtual body sitting on the chair from the first-person perspective that moved in synchrony with their real body (15 s).
-
4.
Participants were asked to do simple movements (30 s) (“look at your right hand, look at your left hand, look at yourself in the mirror, stretch your right arm, stretch your left arm”).
-
5.
Four cubes appeared in front of the participant, who was asked to touch them with their virtual hands. When touched, the object disappeared, the corresponding controller vibrated, and a short sound was played.
-
6.
Then, depending on the group and the condition, participants observed one of the following:
-
a.
their normal virtual body (visible body condition) (100 s);
-
b.
how their body gradually becomes transparent (invisible body condition) (30 s of gradually increasing transparency + 70 s 100% transparency);
-
a.
-
7.
Participants were asked about their level of pain.
-
8.
Participants were asked an open question to explain their sensations and thoughts during the scene.
-
9.
The second scene loaded in a pseudo-randomized order. After the scene, the experience ended.
Measurements
Measures before the VR experience (pre-study)
The Fibromyalgia Impact Questionnaire (FIQ) is a questionnaire developed to estimate the current health status of women with FM syndrome in clinical and research settings. The FIQ has been translated and validated into 14 different languages and has been used in hundreds of research articles as an outcome measure. A Spanish version of the latest, revised FIQ was validated in 2013 by Salgueiro et al.30 It consists of 21 questions that measure functioning, overall impact, and symptoms. In this study, to keep the procedure as short as possible, we used only part 3, which estimates the severity of the 10 most common symptoms in the last 7 days. Total scores range from 0 to 100 points.
Interoceptive awareness was measured with the Multidimensional Assessment of Interoceptive Awareness (MAIA) scale, a self-report questionnaire evaluating various aspects of interoceptive awareness. There are eight subscales: Noticing, Not Distracting, Not Worrying, Attention Regulation, Emotional Awareness, Self-Regulation, Body Listening and Trusting. We used the 30-item Spanish adaptation of the scale31. Individual scores range from 0 to 150.
Body perception distortions were measured with the Fremantle Back Awareness Questionnaire (FBAQ)32,33 in a slightly adapted version, where we replaced the word back with the word body (Supplementary Table S1). The unidimensional scale measures distortions of body image, including perceived changes in size, swallowing, or lack of control over one’s movements. The minimal total score is 0 and the maximum is 36.
Measures during the VR experience
Pain was measured on a visual analogue scale ranging from 0 (no pain) to 100 (most intense pain imaginable)34:
-
Please indicate the intensity of pain you are feeling right now. A value of 0 means "no pain", and a value of 100 means "the worst pain imaginable". Select the desired value using the joystick on the right controller and confirm by pressing the trigger.
During the VR experience, after each condition, participants responded out loud to one of the corresponding questions: What did you feel when you had a virtual body? and What did you feel when your body became transparent and disappeared? Answers to the open questions asked during the VR experience were recorded in audio form and then manually transcribed.
Measures after VR experience (post-study)
Some measures were taken afterwards to shorten the time spent in HMD and reduce the overall difficulty of the experimental procedure. The illusion of virtual body ownership was measured after the virtual reality experience on three Likert scale questions, using a scale from 1 (not at all), to 7 (very much):
-
I felt that the virtual body I saw when I looked down was my own body (ownership).
-
I felt that the movements of my virtual body were caused by my own movements (agency).
-
To what extent were the sensations of your real body surprising and unexpected? (surprising reactions).
Open questions were asked to better understand the experience of patients and determine their preferred scenario.
-
Which of the two scenes did you prefer, which one did you like the most, and why?
Apparatus
The Oculus Quest headset uses an OLED panel with a resolution of 1600 × 1440 per eye display. It has a refresh rate of 72 Hz and weighs 470 g, 6 degrees of freedom, and rotational and positional tracking. To track hand movements, we used the Oculus Quest controllers, which are comfortable and easy to use. Oculus Quest does not need a computer to run the applications and has a comfortable in-ear speaker system, which makes use of the system user-friendly.
We used CleanBox CX1 to disinfect the system. It uses ultraviolet C light-emitting diodes to disinfect surfaces from viruses, bacteria, and fungi.
Statistical analyses
We adapted a mixed methods approach to analyse the answers to the open questions transcribed verbatim by running a sentiment analysis (sentiment-analysis-spanish v0.0.25 python library) and clustering the content of the answers into nine main themes related to affective and physiological states. A repeated-measures ANOVA was used to test the differences in sentiment between session and conditions. Differences in symptoms, interoception awareness, body perception disturbances, and embodiment between sessions were verified with the Friedman test. A random intercepts and random slopes mixed linear model was built to estimate the effect of ongoing pain, symptom intensity, interoceptive awareness, and body perception disturbances on embodiment (python statsmodels library)35. The model assumptions were tested visually and formally with the Shapiro–Wilk test for normality and the White Lagrange multiplier test for heteroscedasticity.
Results
Sample characteristics and their influence on embodiment and pain
There were no differences between session 1 and 2 in any of the baseline questionnaire scores. Patients evaluated the intensity of their symptoms (FIQ-3) as medium to high (M = 6.09, SD = 1.30, and M = 6.02, SD = 1.85 in session 1 and 2 respectively) (Table 1). Moreover, the body perception disturbances were experienced by them rarely or occasionally, although the variance was large, with some patients reporting no disturbances and others scoring almost the maximal possible score (max score in session 1 = 3.78 and in session 2 = 1.87). The mean level of interoceptive awareness was slightly above the middle of the scale (session 1: M = 3.06, SD = 0.55, session 2: M = 2.99, SD = 0.61).
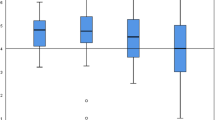
Embodiment was scored on a Likert (ordinal) scale and the data points were not normally distributed (p < 0.05), thus we applied non-parametric tests. In any case non-parametric tests are more conservative than parametric, in the sense that null hypothesis rejected by a parametric test might not be rejected by the equivalent appropriate non-parametric test. In both sessions, patients rated their overall embodiment (Fig. 3d) as medium to high (session 1: M = 4.78, SD = 1.67, session 2: M = 4.37, SD = 1.93) (Table 1). Looking at the answers to each embodiment question, we found that the lowest scores and the largest variance were observed for ownership (Fig. 3a; median = 3, IQR = 5) with a large group of participants scoring either very low (< 2) or very high (> 5), while agency (Fig. 3b) and vivid reactions (surprising, unexpected; Fig. 3c) were rated mostly high, especially in session 1, perhaps due to the fact that participants were unfamiliar with the scenarios and because they had actual agency over their virtual body, since their virtual body moved with them.
(a) Distribution of body ownership values on a Likert scale (1–7) in the sample. (b) Distribution of agency over the virtual body on a Likert scale (1–7). (c) Surprising responses on a Likert scale (1–7). In (a–c) the first and second sessions are represented. The red line corresponds to the median. (d) Embodiment levels and the preference for bodily illusion.
Half of the participants in sessions 1 and 2 preferred the experience of the visible body experience (N = 11 and N = 10, respectively). This group reported a wide range of embodiment scores (min. 1, max 7), with a median of 4.3 (IQR = 3) in session 1 and 5 (IQR = 1.3) in session 2. The 25% of the group who chose the scene where their body became progressively invisible reported a high level of embodiment (session 1: median = 6, IQR = 1.3; session 2; median = 6.2, IQR = 0.6). Some patients did not respond (N = 3) or preferred both or none of the sessions equally (Fig. 3).
Content analysis
We analysed the content of the answers to the open questions by selecting words and short phrases which described affective reactions, physiological states, or were related to bodily experiences. Next, we grouped them into nine general categories and counted the frequencies of their content (Fig. 4).
Overall, responses were very diverse and stretched from very negative (e.g. horror, anguish, fear, tension) to neutral (strange, different) to very positive (relief, calm, light, good feeling). Looking at the complete answers, we noticed an important role for the meaning or interpretations patients gave to the virtual scenarios. For example, a few patients associated their disappearance with death, which resulted in overall negative affective reactions. Others, who had a more neutral or no interpretation, reacted in a neutral or even positive manner. Many patients had various physical reactions, from dizziness to a weightlessness, from increased pain to no pain. Four patients said they felt nothing and four did not respond at all (Table 2).
Sentiment analysis
In the second step, we calculated the sentiment scores in the answers to open questions for each condition on a scale from 0 (very negative) to 1 (very positive). The mean sentiment was rather negative (mean = 0.11, SD = 0.19). Furthermore, repeated measures ANOVA yielded significant differences between bodily illusions (F(1,15) = 5.21, p = 0.037, eta squared = 0.258), with the invisible body evoking more positive reactions (mean = 0.14, SD = 0.23) than the visible one (mean = 0.07, SD = 0.14). There were no differences between sessions. However, the most positive sentiment was recorded among patients who indicated that visible body conditions were preferred (Fig. 5).
Factors modulating the embodiment illusion
To test the influence of measured variables on embodiment, we built a mixed effects model using the mixedlm in python statsmodels library, following Harrison et al.36. In the first step, we standardized the questionnaire scores (FIQ-3, FBAQ, MAIA) so that they had M = 0 and SD = 137. Next, we fitted a random intercept and random slope model for session, with observations clustered in individuals and fixed (session) and random (mean pain during VR, fiq_z, fbaq_z, maia_z) factors. The model formula included the embodiment as a dependent variable, and the mean pain in VR, FBAQ, FIQ, MAIA, and session as factors. (model = "emb_z ~ pain_mz + fbaq_z + fiq_z + maia_z + C(session)", re_formula = "C(session)").
Normality of the residuals and heteroscedasticity check
Both visual analysis and formal statistical tests confirmed that the assumptions were not violated. In particular, the Shapiro–Wilk test for normality of the residuals (W = 0.952, p = 0.087) and the White’s Lagrange multiplier test for heteroscedasticity (LM = 25.95, p = 0.132, F = 1.94, p = 0.074) were not significant.
Model parameters
We calculated the intraclass correlation coefficient (ICC), which measures the similarity of the responses within a random effect (Table 3). In our model, the ICC for the session is equal to 0.490, suggesting a moderate correlation. The random effect of the participant was 0.600, and the embodiment varied on average 0.775, which indicated a large variation between and within participants. The estimated correlation coefficient between the random intercepts and random slopes was − 0.658 which indicated that patients experiencing high embodiment in the first session experienced lower embodiment in the second session. Following Westfall et al. (2014), we calculated the effect size for a design with random participants and random items d = 0.34, which is small.
We found significant random effects of fbaq_z and fiq_z, indicating that more body perception disturbances led to higher embodiment levels, while more intensive FM symptoms (reported for the last 7 days) had the opposite effect (Fig. 6). Neither pain nor interoception awareness were significant.
To obtain the explained variance, we followed the approach proposed by Nakagawa and Schielzeth38 and calculated the marginal and conditional R2GLMM, which allows separation of the contributions of fixed and random effects. In our model, the marginal R2GLMM = 18.86% of the variance explained by fixed factors and the conditional R2GLMM = 67.84%, which can be interpreted as the variance explained by the entire model (both fixed and random factors).
Discussion
FM is an intriguing and still rather poorly understood chronic pain condition. In this study, we explored the experience of owning a body and observing it become progressively invisible in women with FM. We found that patients with FM can experience embodiment illusions in immersive VR in both visible and invisible conditions, and in spite of their chronic pain. We also observed that these experiences led to diverse reactions on both affective and physiological levels and that cognitions, and perhaps also metacognitions39, may be involved in modulation of these reactions. Many patients described their state as anxious or strange, while others felt relaxed. A wide range of bodily sensations was also mentioned, including changes in weight, such as a feeling of weightlessness or floating, in contrast to the commonly experienced feeling of heaviness or swelling40. Although the progressively invisible body illusion evoked more positive sentiment, it was not reflected in behaviour, operationalized here as the preference of one of the illusions, as patients more frequently chose the visible body condition.
Fuchs and Schlimme41 distinguished two forms of disturbed body awareness in the context of schizophrenia, namely disembodiment and hyper-embodiment. The first is experienced as a disconnection with one’s body (alienation) and the latter refers to the experience of being totally immersed in it, a feeling of the physiological experiences being “too real”, which can be both pleasant and painful, depending on the context. Such hyper-embodiment is a daily experience of patients with FM, as their bodies are often felt to be an unavoidable obstacle, rigid and heavy42. In our study, the progressive invisibility triggered in several participants a feeling of weightlessness and relief. We speculate that in these patients the constant experience of hyper-embodiment was broken or transformed into a pleasant feeling of virtual disembodiment (“no body” ownership). Nonetheless, for other participants the experience was rather unpleasant and attracted their attention towards their symptoms, perhaps due to the multisensory conflict caused by the absence of visual cues (invisible body) during ongoing proprioceptive and painful stimulation.
The most important result was that higher levels of body perception disturbance predicted a higher embodiment. While the cause of this is not known, we can speculate. Valenzuela-Moguillansky5 hypothesized that disruption of implicit knowledge of the topography of patients’ bodies leads to a paradoxical feeling of being in pain while not feeling it. A disturbed body image is a signal of a desynchronization of brain and body, which is one of the main characteristics of FM43. We speculate that body distortions are a form of plasticity in body representation, and thus some patients with FM may be more prone to incorporate virtual bodies, which is also a form of plasticity17,44. Importantly, FM not only affects interoception, but also exteroception, and reduces the tendency to actively listen to the body for insight45. We suggest that disturbances in body awareness might lead to increased sensitivity to external cues such as strong visual stimulation in VR. However, more studies are required to validate this preliminary result.
Interestingly, while stronger fibromyalgia symptoms (including pain) in the prior week decreased embodiment, the pain ratings reported during the virtual experience had no effect on the embodiment. This suggests that ongoing musculoskeletal pain can be partially overridden by strong synchronous visuomotor and visuotactile stimulation, confirming that chronic pain does not completely prevent embodiment27. However, whether very intense or acute pain prevents virtual embodiment, deserves further investigation.
We observed a large variation between participants and sessions. The patients who reported higher embodiment in the first session rated the strength of the illusion as lower in the second session. We speculate that in the first session, some participants were surprised or baffled with the illusion, but the novelty effect had worn off in the second exposure.
An important contribution of this study is a demonstration of usefulness of the mixed methods in chronic pain research, obtained here by combining sentiment analysis with a quantitative and qualitative text analysis and multilevel modelling. The collected data helped us to improve our understanding of the bodily experiences among patients with FM and added context to the large variability of variance observed in the questionnaires.
The study had several limitations. We chose to keep the duration of the procedure as short as possible to minimize fatigue and discomfort of the patients28. For the same reasons, we only measured overall pain, without specifying the location or type of pain. Future studies dedicated to embodiment and pain modulation should apply a standardized scale, such as the one proposed by Gonzalez-Franco & Peck46 and the short form of the Brief Pain Inventory47. We also take note of the weak effects obtained in the mixed linear model. Although the sample was sufficient to obtain a converged model with satisfactory parameters, a larger sample is recommended in future studies.
Four patients reported that they did not feel embodied because the virtual avatar did not look like them. Although the embodiment illusion is normally triggered automatically at a low level if the basic conditions are accomplished (namely a first-person perspective, human-shaped body, congruent visuomotor/visuotactile cues48), a greater similarity of the avatar to the subject may be important in the case of chronic pain patients who are less sensitive to virtual embodiment. Thus, future studies should investigate the role of look-alike avatars in embodiment among patients with FM.
Future studies should also investigate the sources of variability among patients with FM in the context of body perception and embodiment to identify potential subgroups of patients who may be more sensitive to specific types of virtual bodily illusion. Although several subtypes of patients have already been identified29, it is unclear whether these profiles can explain the differences observed in experiencing virtual embodiment. Another interesting research path which has not received much attention until now is the role of cognition and metacognition in embodiment among both clinical and healthy populations, especially in scenarios which offer limited context and broad space for interpretation. Moreover, in future more attention should be paid to the rich affective reactions patients present during the virtual experience. In general, virtual embodiment is a promising tool for diagnosing and treating some of the least understood symptoms of FM related to the bodily self and its disturbances which have a severe impact on patients’ quality of life.
Conclusions
Women with fibromyalgia are characterized by a large intra- and interpersonal variety which leads to diverse affective reactions to the same bodily illusion in virtual reality. Fibromyalgia symptoms intensity may negatively affect the proneness to virtual embodiment. Paradoxically, more disturbed body perception may strengthen the embodiment illusion. Moreover, pain reported during the virtual experience as well as interoception awareness did not affect the strength of virtual body illusions.
Data availability
Data are available on request from the corresponding author.
References
Haggard, P., Iannetti, G. D. & Longo, M. R. Spatial sensory organization and body representation in pain perception. Curr. Biol. 23, R164–R176 (2013).
Park, D. C., Glass, J. M., Minear, M. & Crofford, L. J. Cognitive function in fibromyalgia patients. Arthritis Rheum. 44, 2125–2133 (2001).
Borg, C., Emond, F. C., Colson, D., Laurent, B. & Michael, G. A. Attentional focus on subjective interoceptive experience in patients with fibromyalgia. Brain Cogn. 101, 35–43 (2015).
Taylor, S. S., Davis, M. C., Yeung, E. W., Zautra, A. J. & Tennen, H. A. Relations between adaptive and maladaptive pain cognitions and within-day pain exacerbations in individuals with fibromyalgia. J. Behav. Med. 40, 458–467 (2017).
Valenzuela-Moguillansky, C. An exploration of the bodily experience of persons suffering from fibromyalgia. Constr. Found. 8, 339–350 (2013).
Ziadni, M. S., Sturgeon, J. A. & Darnall, B. D. The relationship between negative metacognitive thoughts, pain catastrophizing and adjustment to chronic pain. Eur. J. Pain 22, 756–762 (2018).
Kinsbourne, M. Awareness of one’s own body: An attentional theory of its nature, development, and brain basis. In The Body and the Self (ed. Kinsbourne, M.) 205–223 (The MIT press, 1995).
Moseley, G. L., Gallace, A. & Spence, C. Bodily illusions in health and disease: Physiological and clinical perspectives and the concept of a cortical ‘body matrix’. Neurosci. Biobehav. Rev. 36, 34–46 (2012).
Diers, M. et al. Site-specific visual feedback reduces pain perception. Pain 154, 890–896 (2013).
Harris, A. J. Cortical origin of pathological pain. Lancet 354, 1464–1466 (1999).
Vittersø, A. D., Halicka, M., Buckingham, G., Proulx, M. J. & Bultitude, J. H. The sensorimotor theory of pathological pain revisited. Neurosci. Biobehav. Rev. 139, 104735 (2022).
Brun, C. et al. Sensory disturbances induced by sensorimotor conflicts are higher in complex regional pain syndrome and fibromyalgia compared to arthritis and healthy people, and positively relate to pain intensity. Eur. J. Pain 23, 483–494 (2019).
de Vignemont, F., Pitron, V. & Alsmith, A. J. T. What is the body schema? In Body Schema and Body Image: New Directions (eds de Vignemont, F. et al.) (Oxford University Press, 2021).
Martínez, E. et al. Embodied pain in fibromyalgia: Disturbed somatorepresentations and increased plasticity of the body schema. PLoS One 13, e0194534 (2018).
Lackner, J. R. Some proprioceptive influences on the perceptual representation of body shape and orientation. Brain 111, 281–297 (1988).
Botvinick, M. & Cohen, J. Rubber hands ‘feel’ touch that eyes see. Nature 391, 756–756 (1998).
Slater, M. & Sanchez-Vives, M. V. Transcending the self in immersive virtual reality. Computer 47, 24–30 (2014).
Kilteni, K., Groten, R. & Slater, M. The sense of embodiment in virtual reality. Presence Teleoper. Virtual Environ. 21, 373–387 (2012).
Heydrich, L. et al. Cardio-visual full body illusion alters bodily self-consciousness and tactile processing in somatosensory cortex. Sci. Rep. 8, 9230 (2018).
Tajadura-Jiménez, A., Banakou, D., Bianchi-Berthouze, N. & Slater, M. Embodiment in a child-like talking virtual body influences object size perception, self-identification, and subsequent real speaking. Sci. Rep. 7, 9637 (2017).
Longo, M. R., Betti, V., Aglioti, S. M. & Haggard, P. Visually induced analgesia: Seeing the body reduces pain. J. Neurosci. 29, 12125–12130 (2009).
Martini, M., Perez-Marcos, D. & Sanchez-Vives, M. V. Modulation of pain threshold by virtual body ownership: Virtual body ownership and pain threshold. Eur. J. Pain 18, 1040–1048 (2014).
Martini, M., Perez-Marcos, D. & Sanchez-Vives, M. V. What color is my arm? Changes in skin color of an embodied virtual arm modulates pain threshold. Front. Hum. Neurosci. https://doi.org/10.3389/fnhum.2013.00438 (2013).
Martini, M., Kilteni, K., Maselli, A. & Sanchez-Vives, M. V. The body fades away: Investigating the effects of transparency of an embodied virtual body on pain threshold and body ownership. Sci. Rep. https://doi.org/10.1038/srep13948 (2015).
Matamala-Gomez, M., Diaz Gonzalez, A. M., Slater, M. & Sanchez-Vives, M. V. Decreasing pain ratings in chronic arm pain through changing a virtual body: Different strategies for different pain types. J. Pain 20, 685–697 (2019).
Trost, Z., France, C., Anam, M. & Shum, C. Virtual reality approaches to pain: Toward a state of the science. Pain 162, 325–331 (2021).
Matamala-Gomez, M. Immersive virtual reality and virtual embodiment for pain relief. Front. Hum. Neurosci. 13, 12 (2019).
Donegan, T., Ryan, B. E., Swidrak, J. & Sanchez-Vives, M. V. Immersive virtual reality for clinical pain: Considerations for effective therapy. Front. Virtual Real. 1, 9 (2020).
Loevinger, B. L., Shirtcliff, E. A., Muller, D., Alonso, C. & Coe, C. L. Delineating psychological and biomedical profiles in a heterogeneous fibromyalgia population using cluster analysis. Clin. Rheumatol. 31, 677–685 (2012).
Salgueiro, M. et al. Validation of a Spanish version of the revised fibromyalgia impact questionnaire (FIQR). Health Qual. Life Outcomes 11, 132 (2013).
Valenzuela-Moguillansky, C. & Reyes-Reyes, A. Psychometric properties of the multidimensional assessment of interoceptive awareness (MAIA) in a Chilean population. Front. Psychol. https://doi.org/10.3389/fpsyg.2015.00120 (2015).
Pascual, Ó. S. A. Evaluación de la Agudeza Táctil Lumbar en Pacien- tes con Lumbalgia Aguda y su Efecto Sobre el Dolor, Imagen Corporal y Movilidad Lumbar (Escuela Universitaria de Fisioterapia Gimbernat-Cantabria, 2016).
Wand, B. M. et al. Disrupted self-perception in people with chronic low back pain. Further evaluation of the fremantle back awareness questionnaire. J. Pain 17, 1001–1012 (2016).
Hawker, G. A., Mian, S., Kendzerska, T. & French, M. Measures of adult pain: Visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF. Arthritis Care Res. 63, S240–S252 (2011).
Seabold, S. & Perktold, J. Statsmodels: Econometric and Statistical Modeling with Python. In 92–96 (2010). https://doi.org/10.25080/Majora-92bf1922-011.
Harrison, X. A. et al. A brief introduction to mixed effects modelling and multi-model inference in ecology. PeerJ 6, e4794 (2018).
Gelman, A. & Hill, J. Data Analysis using Regression and Multilevel Hierarchical Models Vol. 1 (Cambridge University Press, 2007).
Nakagawa, S. & Schielzeth, H. A general and simple method for obtaining R2 from generalized linear mixed-effects models. Methods Ecol. Evol. 4, 133–142 (2013).
Stuifbergen, A. K., Phillips, L., Voelmeck, W. & Browder, R. Illness perceptions and related outcomes among women with fibromyalgia syndrome. Womens Health Issues 16, 353–360 (2006).
Viceconti, A. et al. Body perception distortions correlate with neuropathic features in Italian fibromyalgic patients: Findings from a self-administered online survey. Musculoskelet. Sci. Pract. 60, 102570 (2022).
Fuchs, T. & Schlimme, J. E. Embodiment and psychopathology: A phenomenological perspective. Curr. Opin. Psychiatry 22, 570–575 (2009).
Calsius, J., Courtois, I., Stiers, J. & De Bie, J. How do fibromyalgia patients with alexithymia experience their body? A qualitative approach. SAGE Open 5, 2158244015574631 (2015).
Perrot, S. Fibromyalgia: A misconnection in a multiconnected world?. Eur. J. Pain 23, 866–873 (2019).
Kilteni, K., Normand, J.-M., Sanchez-Vives, M. V. & Slater, M. Extending body space in immersive virtual reality: A very long arm illusion. PLoS One 7, e40867 (2012).
Valenzuela-Moguillansky, C., Reyes-Reyes, A. & Gaete, M. I. Exteroceptive and interoceptive body-self awareness in fibromyalgia patients. Front. Hum. Neurosci. https://doi.org/10.3389/fnhum.2017.00117 (2017).
Gonzalez-Franco, M. & Peck, T. C. Avatar embodiment. Towards a standardized questionnaire. Front. Robot. AI https://doi.org/10.3389/frobt.2018.00074 (2018).
Cleeland, C. S. The brief pain inventory. Pain Res. Group 20, 143–147 (2009).
Maselli, A. & Slater, M. The building blocks of the full body ownership illusion. Front. Hum. Neurosci. https://doi.org/10.3389/fnhum.2013.00083 (2013).
Acknowledgements
IDIBAPS is funded by the CERCA program (Generalitat de Catalunya). Partially funded by Departament de Recerca i Universitats de la Generalitat de Catalunya with the code AGAUR 2021 SGR 01165, Grup NEUROVIRTUAL. We thank Xavi Navarro Muncunill for his help with the implementation of the scenario and Prof. Mel Slater for his valuable feedback. We also thank Tony Donegan for language edition.
Author information
Authors and Affiliations
Contributions
J.S. designed the research; A.A. and M.V.S.V. consulted on the research design and implementation; J.S. carried out the experiment, the analysis, and wrote the first version of the manuscript; E.R. implemented the scenario; all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Świdrak, J., Arias, A., de la Calle, E.R. et al. Virtual embodiment in fibromyalgia. Sci Rep 13, 10719 (2023). https://doi.org/10.1038/s41598-023-36861-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36861-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.