Abstract
Colorectal cancer is one of the most incident types of cancer in the world, with almost 2 million new cases annually. In Brazil, the scenery is the same, around 41 thousand new cases were estimated in the last 3 years. This increase in cases further intensifies the interest and importance of studies related to the topic, especially using new approaches. The use of machine learning algorithms for cancer studies has grown in recent years, and they can provide important information to medicine, in addition to making predictions based on the data. In this study, five different classifications were performed, considering patients’ survival. Data were extracted from Hospital Based Cancer Registries of São Paulo, which is coordinated by Fundação Oncocentro de São Paulo, containing patients with colorectal cancer from São Paulo state, Brazil, treated between 2000 and 2021. The machine learning models used provided us the predictions and the most important features for each one of the algorithms of the studies. Using part of the dataset to validate our models, the results of the predictors were around 77% of accuracy, with AUC close to 0.86, and the most important column was the clinical staging in all of them.
Similar content being viewed by others
Introduction
The analysis of the survival of cancer patients is fundamental for the planning and evaluation of health services. Additionally, the identification and validation of prognostic factors are important to guide the treatment protocol.
Epidemiological studies have used statistical models, based on pre-established predictors for the prognosis of survival in patients with colorectal cancer (CRC). Such techniques have limitations related to the adaptation of models, changes in the reality, and potential reduction in accuracy over time1. The most common statistical models are linear and depart from explicit descriptions of the relationships between data. Currently, artificial intelligence (AI) has been collaborating in the diagnosis of several diseases2,3 and in the evaluation of survival4, the machine learning technique, an application based on artificial intelligence data, in which systems learn and improve automatically without explicit programming5, has been used in the search for an evaluation that demands fewer human resources, possibly more accurate and perennial survival. They are quickly and easily adaptable to new realities and their use has been tested in cancer studies6.
Since models using machine learning do not provide structure and parameters in an explicit and easily interpretable way, it becomes crucial to test their use and their accuracy with real data. In recent years, cancer registry data, such as the US Surveillance, Epidemiology and End Results (SEER), have been used to predict mortality or survival in the US using artificial intelligence5,7.
Colorectal cancer (CRC) is among the ten most incidents in the world8. It is estimated that approximately 10% of cancer cases in the world in 2020 will be in the colon or rectum, corresponding to approximately 1.8 million new cases annually9, with an increasing trend in both genders. In Brazil, around 41 thousand new cases are estimated between 2020 and 202210. The Hospital Based Cancer Registries of São Paulo state (RHC-SP), based at the Fundação Oncocentro do Estado de São Paulo (FOSP), covers a population of approximately 30 million inhabitants, with 33,000 cases of colorectal cancer, configuring a unique opportunity to carry out of mortality or survival prediction studies for Brazilian patients. The objective of the present study is to evaluate and compare the validity of three artificial intelligence algorithms for predicting the survival of patients with CRC treated in São Paulo, the most populous state in Brazil, from 2000 to 2021, based on data from the RHC-SP.
Results
Characteristics of the population
When analyzing the patients’ survival over the years after the diagnosis, extracting this information directly from the dataset, a decay can be seen up to the fifth year, being 77% of survival in 1 year, 59% in 3 years, and 53.2% in 5 years, Supplementary Fig. S1. The selection of data, creation of columns, and pre-processing steps that were used in the analyses are shown according to the driagram in Fig. 1, 31,916 patients were eligible. For the patients’ survival studies (1, 3, and 5 years), a selection was made to remove data from patients who were not followed up for the label period, so 29,670, 26,231, and 23,338 patients were eligible for the analyzes 1-year, 3-year, and 5-year survival, respectively.
Diagram with the steps performed in the studies. All specific selections, created columns, and preprocessing steps are described, with a greater focus until the division of the data set into training and testing for each analysis. After this, we have the encoding of the features to numerical values and their normalization, followed by the steps of training and validation of the created models.
Training and validation
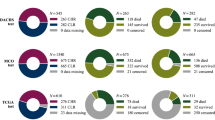
The division of the dataset into training and testing was performed randomly, with 75% for training and 25% for test data, in addition, there was no significant difference between the sets in the percentage of patients contained in each class, Table 1.
Models were trained and fitted for each analysis and validations were performed using the confusion matrix for the test data, along with the ROC curve and the corresponding training and testing AUC. For the Random Forest and XGBoost models, a search for the best hyperparameters of these models was also performed for each of the analyses, a summary of the results for the test set is presented in Table 2. Observing the AUC values, it is noticed that some of the models show a significant difference between the values for training and testing, especially the Random Forest models. This characterizes the problem of overfitting in these models, which occurred due to the search for parameters in a wider range of values. However, the XGBoost models did not show this problem so pronouncedly and obtained the best accuracy results in all studies.
Finally, some neural network possibilities were tested for these data, both sequential and more complex models, but the performance was lower than the machine learning algorithms used, obtaining lower accuracy than the Random Forest and XGBoost models in all tests performed. Therefore, the use of neural networks in this study was not further explored.
Cancer specific survival
The Naive Bayes model had the worst performance among those used, observing the accuracy of the model, we obtain an unbalanced classification, getting more data from class 1 to class 0 (Fig. 2a), in the ROC curve, the value was AUC = 0.767 for training and 0.765 for testing (Fig. 3). With the Random Forest model, the accuracy was almost 77% in both classes (Fig. 2b), the training and testing AUC values were 0.974 and 0.844, respectively (Fig. 3). Finally, using the XGBoost model, a better performance, comparing with Random Forest model was obtained, with more than 77% of accuracy in the prediction of both classes (Fig. 2c). AUC values were 0.909 for training and 0.845 for testing (Fig. 3).
(a) Naive Bayes, (b) Random Forest, (c) XGBoost. Confusion matrices of the models, cancer specific survival. The Naive Bayes model (a) had the worse performance, besides not having balanced accuracy in both classes. On the other hand, the Random Forest (b) and XGBoost (c) models had a performance with a very similar accuracy.
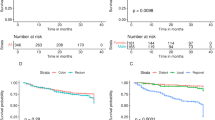
(a) Training, (b) Test. ROC curves of the models, cancer specific survival. As expected, the Naive Bayes model showed the worst AUC values, both for the training and test sets. Looking at the curves for the Random Forest and XGBoost models, it can be noticed that there is some overfitting in both models, especially in the case of the Random Forest model, due to the difference in AUC values between the training and test metrics.
The five most important features of the Random Forest model were clinical staging, presence of recurrence, year of diagnosis, service category and surgery (Fig. 4a). For the feature service category, the conclusions are similar to those of the clinical staging column, lower values have a negative impact and higher values have a positive impact. In the columns’ presence of recurrence, year of diagnosis, and surgery, higher values of these features negatively influence the prediction, contributing more to class 0, which means that the patient did not die from cancer. The lower values of the features contributed the most to class 1.
(a) Random Forest, (b) XGBoost. Feature importances of the models, cancer specific survival. The SHAP values show the most important features for the Random Forest and XGBoost models, allowing for analysis and validation, based on medical knowledge, of the algorithms’ training. Both presented similar columns among the top ten, with only the order varying, probably due to differences between the two algorithms.
Regarding the XGBoost model, four of them are similar to the conclusions of the Random Forest model (Fig. 4b), they are clinical staging, year of diagnosis, presence of recurrence, and surgery. The other column that appeared was age, which had higher values having a greater impact on patient death (class 1) and lower values for survival (class 0).
Overall survival
The Naive Bayes model had the worst performance among those used, observing its accuracy, we obtain an unbalanced classification, so the model got more data from class 0 in relation to class 1 (see Supplementary Fig. S2a), in the ROC curve, the value was AUC = 0.773 for training and 0.781 for testing (Supplementary Fig. S3). With the Random Forest model, the accuracy was 77% in both classes (see Supplementary Fig. S2b), the training and test AUC values were 0.958 and 0.852, respectively (Supplementary Fig. S3). Finally, using the XGBoost model, the best performance was obtained, with almost 78% accuracy in class prediction (see Supplementary Fig. S2c). AUC values were 0.873 for training and 0.857 for testing (Supplementary Fig. S3).
The five most important features of the Random Forest model were clinical staging, year of diagnosis, age, presence of recurrence, and surgery (Supplementary Fig. S4a). For the features age the conclusions are similar to the staging column, smaller values have a negative impact and larger values have a positive impact. In the columns’ year of diagnosis, presence of recurrence, and surgery, higher values of these features negatively influence the prediction, contributing more to class 0, which means that the patient did not die for any reason. The lower values of the features contributed the most to class 1. Regarding the XGBoost model, all of them are similar to the conclusions of the Random Forest model (Supplementary Fig. S4b), they are clinical staging, year of diagnosis, age, presence of recurrence and surgery.
One-year survival
The Naive Bayes model had the worst performance among those used, observing the accuracy, the model predicts almost all data as being of class 0 (see Supplementary Fig. S5a), in the ROC curve, the value was AUC = 0.761 for training and 0.772 for testing (Supplementary Fig. S6). With the Random Forest model, the accuracy was 77% in both classes (see Supplementary Fig. S5b), the training and test AUC values were 0.862 and 0.842, respectively (Supplementary Fig. S6). Finally, using the XGBoost model, a performance a little bit higher than Random Forest was obtained, with more than 77% accuracy in the prediction (see Supplementary Fig. S5c). AUC values were 0.865 for training and 0.846 for testing (Supplementary Fig. S6).
The five most important features of the Random Forest model were clinical staging, in-hospital treatment, surgery, presence of recurrence, and chemotherapy (Supplementary Fig. S7a). For the feature presence of recurrence, the conclusions are similar to the staging column, higher values have a negative impact and lower values have a positive impact. In the in-hospital treatment, surgery, and chemotherapy columns, we have the opposite. Regarding the XGBoost model, the conclusions are similar to the features of the Random Forest model (Supplementary Fig. S7b), they are clinical staging, in-hospital treatment, surgery, chemotherapy, and presence of recurrence.
Three-year survival
The Naive Bayes model had the worst performance among those used, observing the accuracy, almost all the predictions were for class 0, thus, the model was correct with few data from class 1 (see Supplementary Fig. S8a), in the ROC curve, the value was AUC = 0.756 for training and 0.743 testing (Supplementary Fig. S9). With the Random Forest model, the accuracy was more than 74% in both classes (see Supplementary Fig. S8b), the training and test AUC values were 0.953 and 0.823, respectively (Supplementary Fig. S9). Finally, using the XGBoost model, a better performance was obtained, with almost 75% accuracy in the prediction of both classes (see Supplementary Fig. S8c). AUC values were 0.895 for training and 0.826 for testing (Supplementary Fig. S9).
The five most important features of the Random Forest model were clinical staging, surgery, age, in-hospital treatment, and year of diagnosis (Supplementary Fig. S10a). For the features age and year of diagnosis, the conclusions are similar to those of the staging column, higher values have a negative impact and lower values have a positive impact. In the surgery, and in-hospital treatment columns, we have the opposite.
Regarding the XGBoost model, all of them are similar to the conclusions of the Random Forest model (Supplementary Fig. S10b), they are clinical staging, year of diagnosis, surgery, age, and in-hospital treatment.
Five-year survival
The Naive Bayes model had the worst performance among those used, the accuracy was unbalanced, with almost all the predictions being for class 1 (see Supplementary Fig. S11a), in the ROC curve, the value was AUC = 0.757 for training and 0.759 for testing (Supplementary Fig. S12). With the Random Forest model, the accuracy was 77% in both classes (see Supplementary Fig. S11b), the training and testing AUC values were 0.969 and 0.853, respectively (Supplementary Fig. S12). Finally, using XGBoost, the best performance was obtained, with almost 78% accuracy in class prediction (see Supplementary Fig. S11c). AUC values were 0.882 for training and 0.858 for testing (Supplementary Fig. S12).
The five most important features of the Random Forest model were clinical staging, year of diagnosis, surgery, age, and in-hospital treatment (Supplementary Fig. S13a). For the features year of diagnosis and age, the conclusions are similar to those of the staging column, higher values have a negative impact and lower values have a positive impact. In the surgery and in-hospital treatment columns, higher values positively influence the prediction, contributing more to class 1, which means that the patient survived the fifth year. The lowest values of these features contributed more to class 0.
About the XGBoost model, all of them are similar to the conclusions of the Random Forest model (Supplementary Fig. S13b), they are clinical stage, year of diagnosis, surgery, age, and in-hospital treatment.
Discussion
Our study is one of the first to predict the survival of cancer patients in a large database using AI, and to verify the validity of these models in Brazil. The algorithm with the best survival prediction was XGBoost, followed by Random Forest and Naive Bayes. In all algorithms evaluated, both for overall and specific survival, the most impacting variable was clinical stage. The variables that best predicted survival in the best model were clinical stage, surgery performed, in-hospital treatment, age, and year of diagnosis.
In all survival analyzes, the advanced clinical staging was more decisive for the death prediction, a fact expected in survival analyses and repeatedly reported in the scientific literature by other authors. The survival values found considering the total number of patients, 77%, 59%, and 53.2% for 1, 3, and 5-year survival, is a little lower than the survival found for tumors considered to have regional metastasis in developed countries whose data are available at the global cancer observatory11. The importance of the in-hospital treatment and the year of diagnosis highlights the possibility of influence of contextual factors on patient survival, indicating possible inequalities related to the capacity of health services, available resources, and qualification of human resources of centers for the specific treatment of cancer.
The use of artificial intelligence to predict survival is a current topic in the scientific literature. Recently, Jiang et al.7 found over 90% accuracy for 5-year osteosarcoma survival in the US using the XGBoost algorithm. In our study, the model with the best accuracy (XGBoost) had lower sensitivity and specificity but was comparable to studies that used cancer registry data. Changee Lee et al.5 compared the accuracy of statistical models used for prediction with artificial intelligence algorithms to predict mortality from non-metastatic prostate cancer in the USA. Leonard et al.12 compared the survival prediction of patients with resected colon cancer using machine learning models and commonly used regression models. The authors verified a similarity between the accuracy of the AI prediction using only clinical and epidemiological data with that of other models considered the most accurate to date. In our study, we only compared AI models. This finding allows further studies comparing the best AI model with other statistical models.
A strength of our study is using data from almost all cancer centers of the State of São Paulo, what reduces the probability of selection bias. A potential limitation of our research refers to the models used, which do not allow the inclusion of patients lost to follow-up. However, given the low percentage of these cases (7%, 17.8%, and 26.9% for 1, 3, and 5-year survival, respectively), it was found that there was no significant change in the results when not including these patients in the training of the models. The survival found in our study is also similar to that of other studies that used survival methods that consider the follow-up time of those lost to follow-up, such as the Kaplan Meier, with the advantage of the study allowing the prediction of survival from the variables found in the model, and not just measure it. In conditions of disruption of health services, for example, the prediction of survival can be very useful to estimate the potential loss of survival.
In conclusion, our results showed that AI models proved to be valid for predicting the patients’ survival with colorectal cancer from hospital-based cancer registry data in low and middle-income countries, with emphasis on XGBoost. More studies are needed to compare the performance of AI models with the most common statistical models for prediction.
Methods
Study population
Patients treated between 2000 and 2021, residing in São Paulo state, were evaluated, totaling 31,916 cases of both genders, diagnosed with colorectal adenocarcinoma ([topography C18-C20, morphology 8140/3]; CID-O 3ed.). Data were extracted from the Deputy Directorate of Information and Epidemiology of Fundação Oncocentro de São Paulo13, coordinator of the RHC-SP, where we have information from more than 70 hospitals, public and private, from the state of São Paulo.
Selection of variables
For survival analysis (1, 3, and 5 years), patients with the time between diagnosis and last information greater or equal than the survival time of the analysis, or who died in the period, were eligible. For example, in the 3-year survival analysis, patients with at least 3 years of treatment information and who died within the first 3 years after diagnosis were selected.
The variables alive in the first year, alive in the third year, alive in the fifth year, death by cancer and all-cause mortality are the labels of the respective analyses, so only the column that is used as the output of the classifiers will be left. The result was twenty-five columns for features and one label in all performed analyzes, the description of the features is presented in the Table 3.
Statistical analysis
The chi-square test was used to obtain the p-values for the variables used as features in the classification models. This test was chosen because there are no continuous columns in the dataset, so it is possible to use chi-square in all the features.
The p-values corresponding to each column of the dataset are shown in Table 4. There are many null values, most of which are very low values approximated by zero, showing a relationship between the features and the labels under analysis. Bigger values (close to one), show that there is no relationship between the column and the analyzed label.
Construction of the models
The models were built based on the classifiers Naive Bayes14, Random Forest14 and XGBoost15. The choice of these three models was based on the differences between the algorithms of the models, with Naive Bayes being the most elementary, based solely on probabilities. The Random Forest and XGBoost algorithms, on the other hand, are more complex and showed good results in initial tests conducted by us. Both are based on decision tree concepts, with the difference that the former trains multiple trees in parallel and the latter processes in series, with a greater focus on correcting the wrong predictions of the previous tree.
The training is performed with the training set and the validation with the test set. The output variables were generated before training the models, being death by cancer (0 = survival and 1 = death by cancer), all-cause mortality (0 = survival and 1 = death by any reason), alive in the first year (0 = death in less than 1 year and 1 = survival), alive in the third year (0 = death in less than 3 years and 1 = survival), and alive in the fifth year (0 = death in less than 5 years and 1 = survival). All categorical variables were converted to numeric values. After that, all variables were normalized to have mean zero and variance one.
The Naive Bayes is a statistical model based on Bayes’ Theorem and uses as a principle the independence between the variables of the problem16. Random Forest uses several decision trees to perform the classification with the bagging method, which uses the random selection of features and voting to combine the results of the parallel trees and generate the classification17. XGBoost combines the methods bagging and boosting, the latter uses decision tree classifiers in series, so each subsequent tree is trained using the errors of the previous one, ultimately forming a model stronger and more accurate for classification18.
The three models have a binary output, 0 and 1, which represents that the probability of survival of the patient, depending on the output under analysis, is lower or greater than 0.5 and were used to obtain a comparison between different approaches in training.
The validation was done with the confusion matrix of the test set, to verify the performance and generalization of the models in each prediction class. The ROC curves were constructed for the training and test sets, using the AUC metric to evaluate the performance of the models.
Ethical considerations
Following the Lei Geral de Proteção de Dados Pessoais (LGPD) of Law No. 13,709, August 14, 2018, Section II—Processing of Sensitive Personal Data, as it is a search with a secondary database, of public access, not containing personal data of the patients, the opinion of the Research Ethics Committee was waived.
Data availability
The raw database, with all types of cancer, are available in the FOSP website. The datasets generated and analysed, and the notebooks developed during the current study are available in the GitHub repository.
Change history
25 September 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41598-023-43248-x
References
Kourou, K., Exarchos, T. P., Exarchos, K. P., Karamouzis, M. V. & Fotiadis, D. I. Machine learning applications in cancer prognosis and prediction. Comput. Struct. Biotechnol. J. 13, 8–17 (2015).
Uddin, S., Khan, A., Hossain, M. E. & Moni, M. A. Comparing different supervised machine learning algorithms for disease prediction. BMC Med. Inform. Decis. Mak. 19, 1–16 (2019).
Battineni, G., Sagaro, G. G., Chinatalapudi, N. & Amenta, F. Applications of machine learning predictive models in the chronic disease diagnosis. J. Pers. Med. 10, 21 (2020).
Silva, G. et al. Machine learning for longitudinal mortality risk prediction in patients with malignant neoplasm in são paulo, brazil. Artif. Intell. Life Sci. 3, 100061 (2023).
Lee, C. et al. Application of a novel machine learning framework for predicting non-metastatic prostate cancer-specific mortality in men using the surveillance, epidemiology, and end results (seer) database. Lancet Digit. Heal. 3, e158–e165 (2021).
Huang, S., Yang, J., Fong, S. & Zhao, Q. Artificial intelligence in cancer diagnosis and prognosis: Opportunities and challenges. Cancer Lett. 471, 61–71 (2020).
Jiang, J. et al. Predictive model for the 5-year survival status of osteosarcoma patients based on the seer database and xgboost algorithm. Sci. Rep. 11, 5542 (2021).
Weiderpass, E. & Stewart, B. W. World cancer report. The Int. Agency for Res. on Cancer (IARC) (2020).
Sung, H. et al. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA 71, 209–249 (2021).
INCA. Estimativa 2020: Incidência de Câncer no Brasil. https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/estimativa-2020-incidencia-de-cancer-no-brasil.pdf (2019).
IARC. Global Cancer Observatory: Cancer Survival in High-Income Countries. International Agency for Research on Cancer - World Health Organization. https://gco.iarc.fr/survival/survmark/.
Leonard, G. et al. Machine learning improves prediction over logistic regression on resected colon cancer patients. J. Surg. Res. 275, 181–193 (2022).
FOSP. Diretoria Adjunta de Informação e Epidemiologia: Banco de Dados do rhc. https://fosp.saude.sp.gov.br/fosp/diretoria-adjunta-de-informacao-e-epidemiologia/rhc-registro-hospitalar-de-cancer/banco-de-dados-do-rhc/.
Pedregosa, F. et al. Scikit-learn: Machine learn-ing in python. J. Mach. Learn. Res. 12, 2835–2830 (2011).
Chen, T. & Guestrin, C. Xgboost: A scalable tree boosting system. 22nd ACM SIGKDD Int. Conf. on Knowl. Discov. Data Min. (2016).
Raschka, S. Naive bayes and text classification i-introduction and theory. arXiv preprint arXiv:1410.5329 (2014).
Denil, M., Matheson, D. & De Freitas, N. Narrowing the gap: Random forests in theory and in practice. In International Conference on Machine Learning 665–673 (PMLR, 2014).
Agrawal, K. Xgboost Classifier Algorithm in Machine Learning. LinkedIn. https://www.linkedin.com/pulse/xgboost-classifier-algorithm-machine-learning-kavya-kumar.
Funding
Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Brazil. Process number: 2021/11794-4.
Author information
Authors and Affiliations
Contributions
L.B.C., V.C.P., S.V.P. and T.N.T. conceived the study, L.B.C. and V.C.P. conducted the study, S.V.P., M.P.C., G.A.F. and T.N.T. analysed the results. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The Funding section in the original version of this Article was omitted. The Funding section now reads: “Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), Brazil. Process number: 2021/11794-4.”
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Buk Cardoso, L., Cunha Parro, V., Verzinhasse Peres, S. et al. Machine learning for predicting survival of colorectal cancer patients. Sci Rep 13, 8874 (2023). https://doi.org/10.1038/s41598-023-35649-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-35649-9
This article is cited by
-
Development and validation of machine learning models and nomograms for predicting the surgical difficulty of laparoscopic resection in rectal cancer
World Journal of Surgical Oncology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.