Abstract
Reports of an association between ovalocytosis and protection against Plasmodium infection are inconsistent. Therefore, we aimed to synthesise the overall evidence of the association between ovalocytosis and malaria infection using a meta-analysis approach. The systematic review protocol was registered with PROSPERO (CRD42023393778). A systematic literature search of the MEDLINE, Embase, Scopus, PubMed, Ovid, and ProQuest databases, from inception to 30 December 2022, was performed to retrieve studies documenting the association between ovalocytosis and Plasmodium infection. The quality of the included studies was assessed using the Newcastle–Ottawa Scale. Data synthesis included a narrative synthesis and a meta-analysis to calculate the pooled effect estimate (log odds ratios [ORs]) and 95% confidence intervals (CIs) using the random-effects model. Our database search retrieved 905 articles, 16 of which were included for data synthesis. Qualitative synthesis revealed that over half of the studies showed no association between ovalocytosis and malaria infections or severity. Furthermore, our meta-analysis demonstrated no association between ovalocytosis and Plasmodium infection (P = 0.81, log OR = 0.06, 95% CI − 0.44 to 0.19, I2: 86.20%; 11 studies). In conclusion, the meta-analysis results demonstrated no association between ovalocytosis and Plasmodium infection. Hence, the role of ovalocytosis in relation to protection against Plasmodium infection or disease severity should be further investigated in larger prospective studies.
Similar content being viewed by others
Introduction
Malaria is caused by at least six Plasmodium species, including Plasmodium falciparum, P. vivax, P. malariae, P. ovale curtisi, P. ovale wallikeri, and P. knowlesi1,2. The parasite is transmitted between humans via the bite of the female Anopheles mosquito3. The World Health Organization estimated that there were 247 million malaria cases in 84 malaria-endemic countries in 2021, resulting in 619,000 deaths4. Plasmodium infection requires interaction with several protein receptors in the membrane of the red blood cell (RBC). The most important of these is P. falciparum erythrocyte membrane protein 1, which mediates the interaction of parasite ligands on the RBC surface5. Other important malaria parasite ligand/RBC receptors involved in RBC invasion are band 3, glycophorin A, glycophorin B, glycophorin C, Duffy antigen receptor for chemokines and semaphorin 7A6.
Southeast Asian ovalocytosis (SAO) is an RBC disorder caused by a 27-basepair deletion in the band 3 protein gene and is characterised by the presence of macro-ovalocytes and ovalostomatocytes on a blood smear7,8. Band 3 is a member of the Solute Carrier 4 family of bicarbonate transporters. It is the predominant glycoprotein of the RBC membrane, where it acts as an electroneutral anion exchanger9,10. A mutation in or decreased expression of the Band 3 gene has been associated with changes in RBC morphology, membrane instability, and blebbing11. In vitro studies have shown that SAO RBCs are relatively resistant to invasion by certain P. falciparum isolates12,13. Furthermore, an in vitro study recently revealed that P. vivax field isolates invaded SAO reticulocytes 67–71% less frequently than non-SAO reticulocytes14. Additionally, a clinical study demonstrated an association between SAO and protection against clinical infections of P. vivax and severe P. falciparum malaria15. Although ovalocytosis, particularly SAO, has been reported to confer a protective effect against malaria infection and severity, there are some inconsistencies in the association between ovalocytosis and malaria, with some studies reporting no such association16,17. Therefore, our systematic review and meta-analysis aimed to collate and pool the evidence of ovalocytosis-associated malaria infection and severity.
Methods
Reporting guidelines and registration
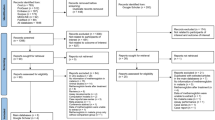
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines18. The systematic review protocol was registered with PROSPERO (CRD42023393778).
Data sources and searches
A systematic search of the MEDLINE, Embase, Scopus, PubMed, Ovid, and ProQuest databases was performed from database inception to 30 December 2022 to retrieve studies reporting cases of malaria in patients with ovalocytosis. The search strategy combined search terms with Boolean operators (AND, OR) as follows: (Elliptocyt* OR Ovalocyt*) AND (malaria OR Plasmodium OR ‘Remittent Fever’ OR ‘Marsh Fever’ OR Paludism). The searches were performed in the English language without limitations on the publication date. A search in Google Scholar was also performed on 30 December 2022 to expand the search and ensure that relevant studies were not missed in the search of the main databases. Table S1 presents the details of the literature retrieved from each database.
Eligibility criteria
The population, exposure, outcome approach19 was applied to retrieve eligible studies as follows: (i) P: participants with and without ovalocytosis, (ii) E: malaria and (iii) O: odds/risk of malarial infection. Microscopy, rapid diagnostic tests (RDTs), or molecular methods can be used to detect Plasmodium infection. The following articles were excluded with reasons: reviews, in vitro studies, case reports or series, conference abstracts without full reports, books or book chapters, letters or news articles, articles where the outcomes of interest could not be extracted and articles for which full texts were unavailable.
Study selection and data extraction
The studies retrieved from the database searches were managed using EndNote version 20.0 (Clarivate, London, UK) reference management software. The study selection began by removing duplicate studies, and the titles and abstracts of the remaining studies were screened. Those with irrelevant titles and abstracts were removed, and then the full-text versions of potentially relevant studies were examined. Studies were included based on pre-specified eligibility criteria, and ineligible studies were excluded with specific reasons. Finally, the following data were extracted and input into a data sheet before synthesis: first author, year of publication, study design, country, participants’ characteristics, Plasmodium species, age range (years) of patients, characteristics of ovalocytosis, method for investigating ovalocytosis (microscopy, RDT or molecular methods) and method for Plasmodium detection. Study selection and data extraction were independently conducted by three authors (MK, KUK and AM) and any discrepancies or disagreements between two authors were resolved through consensus.
Risk of bias assessment
Two authors (MK and KUK) independently assessed the risk of bias of the included studies using the Newcastle–Ottawa Scale (NOS)20. This tool was designed to evaluate the quality of non-randomised studies from three broad perspectives: study group selection, study group comparability and identification of the exposure or outcome of interest for case–control or cohort studies, respectively. Each item received 1 star in the categories of selection and outcome. For each item in the comparability category, a maximum of 2 stars was awarded.
Data synthesis
Both qualitative and quantitative data were synthesised. The qualitative synthesis involved a narrative synthesis of the outcomes of interest from the included studies. The quantitative synthesis involved a meta-analysis approach to pool the outcomes of interest from the included studies.
To synthesise the pooled log odds ratio (OR) and 95% confidence interval (CI), data in 2 × 2 tables (Table S2) were computed using the random-effects model as described by DerSimonian and Laird21. The consistency index (I2 statistics) and Chi-square (Q) test were used to assess the significance and levels of heterogeneity among the included studies. I2 values of < 25%, 25%–75% and > 75% were interpreted as low, moderate and high levels of heterogeneity, respectively22. Meanwhile, a P value of 0.1 for the Q statistic was considered an indication of significant heterogeneity among the included studies, as described previously23. If the heterogeneity of effect estimates among the included studies was observed, with a P value < 0.1 for the Q statistic or an I2 value > 25%, the pooled effect estimate was computed using the random-effects model. However, if there was no significant heterogeneity of effect estimates among the included studies, with a P value > 0.1 for the Q statistic or an I2 value < 25%, the pooled effect estimate was computed using the fixed-effects model.
The publication bias was assessed by visualisation of the funnel plot asymmetry and further validated using Egger’s test24. The trim-and-fill method was used to correct for publication bias25, if any. Meta-regression analysis based on study design, country, participants’ characteristics, Plasmodium species, method used to investigate ovalocytosis, and method for malaria detection was performed to assess the impact of these parameters on the pooled effect estimate. If the meta-regression analysis showed a significant impact of covariates on the pooled effect estimate, a subgroup analysis was conducted to determine the difference in the pooled effect estimate between subgroups. The leave-one-out sensitivity analysis was performed to test whether a single study affected the overall pooled estimate. All analyses were performed using the meta command in Stata v17 software (StataCorp LLC, College Station, TX).
Results
Search results
A total of 905 articles were retrieved from our database searches: MEDLINE (n = 88), Embase (n = 160), Scopus (n = 172), PubMed (n = 114), Ovid (n = 295), and ProQuest (n = 76). After removing duplicate records (n = 311), the titles and abstracts of the remaining records were screened (n = 594) to exclude non-relevant records (n = 443). Then, the remaining records (n = 151) were assessed for full-texts and eligibility. After applying the exclusion criteria, 133 records were excluded with specific reasons: reviews (n = 68), in vitro studies (n = 30), case reports (n = 10), gene mutation or polymorphism (n = 8), no abstract available (n = 4), conference abstracts (n = 2), books (n = 2), no information on ovalocytosis (n = 2), letters or news article (n = 2), inability to extract data (n = 2), unavailability of full text (n = 1), guideline (n = 1) and duplicate article (n = 1). The searches in Google Scholar identified 876 articles, none of which met the eligibility criteria. Finally, 16 studies15,16,17,26,27,28,29,30,31,32,33,34,35,36,37,38 were included for qualitative and quantitative data synthesis (Fig. 1).
General characteristics of the included studies
The included studies were published between 1977 and 2015, with the majority (43.8%) published between 2000 and 201016,17,28,31,32,35,37. Study designs included cross-sectional studies (50.0%)16,17,28,30,31,34,36,37, case–control studies (18.8%)26,27,29, cohort studies (25.0%)32,33,35,38 and both cohort and case–control studies (6.3%)15. Most studies were conducted in Papua New Guinea (68.8%)15,16,26,28,29,32,33,34,35,36,38, with the remainder in Indonesia (18.8%)17,31,37, Malaysia (6.3%)30 and Thailand (6.3%)27. Most studies enrolled patients infected with single or mixed infections of P. falciparum and P. vivax (56.3%)16,17,27,28,29,31,33,34,37, single or mixed infections of P. falciparum, P. vivax and P. malariae (18.8%)15,30,36, and infection with P. falciparum only (12.5%)26,35. The majority of study participants were children (50.0%)15,16,26,32,33,34,36,37, followed by pregnant women (18.8%)28,35,38. Most of the included studies tested for SAO using a polymerase chain reaction (PCR) assay to identify band 3 deletions (75.0%)15,16,17,26,28,31,32,33,34,35,37,38, and the remainder investigated ovalocytosis using microscopy (25.0%)27,29,30,36. Malaria parasites were mainly detected using microscopy (68.8%)16,17,26,27,28,29,30,31,34,35,36, followed by a combination of microscopy with PCR (18.8%)15,32,38, a combination of microscopy with RDT (6.3%)33 or PCR only (6.3%)37 (Table 1). Table S2 presents details of the included studies.
Risk of bias
All three case–control studies26,27,29 and three of the cohort studies15,32,33 scored the maximum of 9/9 stars. Two studies35,38 scored 8/9 stars: one did not demonstrate the outcome of interest at the start of the study35 and the other lacked selection of the non-exposed cohort38. 'The NOS scale for case–control studies was adapted to assess the risk of bias in cross-sectional studies. Six cross-sectional studies scored 8/8 stars16,28,30,31,34,36, and two17,37 scored 7/8 stars because they lacked a ‘definition of controls’ (Table S3).
Qualitative synthesis
Seven studies (43.8%) showed that ovalocytosis might protect against malaria infection15,27,29,30 or severe disease15,26,28,36. Apibal et al.27 reported that patients with malaria had an increased percentage of ovalocytes compared with uninfected patients (P. falciparum: mean, 6.3 cells; P. vivax: mean, 8.3 cells; normal individuals: mean, 0.6 cells). Benet et al.28 reported that severe malaria infections in placental tissues were less common in pregnant women with SAO than in pregnant women in the control group. Cattani et al.29 reported that patients with ovalocytosis had a lower infection rate of P. falciparum (P = 0.044), P. vivax (P = 0.009) and all species of malaria combined (P = 0.013) compared with those without ovalocytosis. Foo et al.30 demonstrated fewer ever-positive ovalocytes for P. falciparum (P < 0.05) or any parasite species (P < 0.05) compared with the controls. Additionally, malaria parasitaemia was lower in individuals with ovalocytes compared with the controls. Rosanas-Urgell et al.15 reported that SAO was associated with a statistically significant reduction of 46% in the incidence of clinical P. vivax episodes and a 52% reduction in P. vivax blood-stage reinfection. Furthermore, in the case–control study, SAO was associated with protection against severe P. falciparum malaria (OR = 0.38, P = 0.014) but not with protection against uncomplicated P. falciparum malaria. Allen et al.26 reported the absence of SAO band 3 in 68/68 (100%) of children with cerebral malaria compared with 6/68 (8.8%) matched community controls (OR = 0, 95% CI 0.0–0.85). Serjeantson et al.36 suggested that patients with ovalocytosis were more resistant to severe malaria than those with normocytes because the ratio of parasitaemia in 112 children with ovalocytes compared with 741 children with normocytes was 1.05 for P. falciparum; 0.90 for P. vivax; 0.54 for P. malariae, and 0.91 for infection with any Plasmodium species.
Eight studies (8/16, 50%) showed no association of SAO with malaria infection or severity16,17,31,32,34,35,37,38. Fowkes et al.16 found no association of SAO with P. falciparum prevalence (P = 0.29) or with mean parasite density (P = 0.66). Kimura et al.17 found no difference in the prevalence of SAO between patients with malaria and controls (P > 0.8) and no difference in the frequency of SAO between patients with P. falciparum and P. vivax malaria. Although Kimura et al.31 discovered a link between a higher rate of ovalocytes and a lower risk of malaria infection, they found that SAO did not protect against malaria infection. Lin et al.32 showed no significant associations between P. falciparum infection and SAO (P > 0.2). O’Donnell et al.34 demonstrated no difference in the proportion of SAO in acute malaria and the community controls (8.8% vs 6.6%, P = 0.57). However, the degree of ovalocytosis was significantly lower in children with SAO during acute malaria compared with the community controls (P = 0.025). O’Donnell et al.35 showed that the SAO genotype was not associated with the frequency of placental P. falciparum infection (placental parasitaemia with a normal genotype: 24.5%, placental parasitaemia with SAO: 21.1%). Shimizu et al.37 reported no significant difference in the prevalence of asymptomatic malaria infection between participants with or without SAO (P > 0.05), and Stanisic et al.38 reported no significant difference in the frequency of malaria infection among participants with or without SAO (P = 0.62). Manning et al.33 reported a frequently higher proportion of ovalocytosis in P. falciparum (5.7%) than P. vivax (3.8%) and mixed infections (4.3%).
Risk of malaria among participants with ovalocytosis
Eleven studies15,16,17,26,29,30,34,35,36,37,38 were included in the meta-analysis of the risk of malaria among participants with ovalocytosis. Overall, the results demonstrated no difference in the log OR of malaria between patients with and without ovalocytosis (P = 0.81, log OR = 0.06, 95% CI − 0.44 to 0.56, I2: 86.20%; 11 studies; Fig. 2). The meta-regression analyses using study design, country, participants’ group, Plasmodium species, method used to investigate ovalocytosis and method for malaria detection as covariates showed that none of these impacted the pooled effect estimate. Thus, the subgroup analysis was discontinued (Table S4). Since Rosanas-Urgell et al.15 showed that SAO was associated with a statistically significant reduction in the incidence of P. vivax infection, the meta-analysis was refined to P. vivax exclusively to prevent any interference from a concomitant P. falciparum infection. However, the results showed no difference in the log OR of P. vivax infection between patients with and without ovalocytosis (P = 0.83, log OR = 0.07, 95% CI: − 0.61 to 0.75, I2: 65.39%; 5 studies; Fig. 3).
Forest plot showing the pooled log odds ratio (OR) of the association between Southeast Asian ovalocytosis (SAO) and malaria infection. Abbreviations: Malaria (O) malaria infection in SAO RBCs; Malaria (non-O) malaria infection in non-SAO RBCs; CI confidence interval; blue square effect estimate (log OR); crimson diamond pooled log OR in each subgroup; green diamond pooled log OR in all included studies.
Forest plot showing the pooled log odds ratio (OR) of the association between Southeast Asian ovalocytosis (SAO) and P. vivax infection. Abbreviations: P. vivax (O), P. vivax infection in SAO RBCs; P. vivax (non-O), P. vivax infection in non-SAO RBCs; CI confidence interval; blue square effect estimate (log OR); green diamond, pooled log OR in all included studies.
Sensitivity analysis
The leave-one-out sensitivity analysis did not identify any outliers in the meta-analysis (P values in re-run analyses > 0.05; Fig. 4), indicating the robustness of the results. Meta-analysis using fixed-effect models was performed to test whether the difference in statistical models affected the pooled effect estimate. The results showed a decreased log OR of malaria among patients with ovalocytosis compared with those without ovalocytosis (P < 0.01, log OR = 0.82, 95% CI 0.49–1.14, I2: 95.10%; 3 studies; Fig. 5).
Sensitivity analysis using the fixed-effects model for the pooled log odds ratio between Southeast Asian ovalocytosis and malaria infection. Abbreviations: CI confidence interval; blue square effect estimate (log OR); crimson diamond pooled log OR in each subgroup; green diamond pooled log OR in all included studies.
Publication bias
Publication bias was assessed using a funnel plot and Egger’s test. The funnel plot showed the asymmetrical distribution of the log OR and indicated the standard error of the log OR (Fig. 6). Egger’s test demonstrated that the small-study effect was not significant (P = 0.68). The results of both tests indicated a publication bias among the included studies. Although the trim-and-fill method was applied to correct for publication bias, the subsequent results showed no difference in the log OR of malaria among patients with ovalocytosis compared with those without ovalocytosis (log OR = 0.297, 95% CI − 0.126 to 0.721).
Discussion
SAO is a disorder of the RBC membrane caused by a mutation in the gene for band 3 protein, which leads to the formation of unique linear oligomers in the RBC membrane. Our meta-analysis results demonstrated no association between SAO and malaria infection, and almost all of the included studies demonstrated no association between SAO and malaria infection16,17,26,34,35,36,37,38. Meanwhile, studies by Rosanas-Urgell et al.15 and Foo et al.30 both showed lower odds of malaria infection in SAO. Conversely, only the study by Cattani et al.29 reported higher odds of malaria infection in SAO. According to Rosanas-Urgell et al.15, SAO provides partial protection against P. vivax but not against P. falciparum infection or uncomplicated disease. Nevertheless, our meta-analysis contradicted these results, with no difference in the risk of P. vivax infection between patients with and without ovalocytosis. These findings suggest that ovalocytosis may not be a protective factor against P. vivax infection, at least for the limited studies included in this meta-analysis.
The protective mechanism of SAO against malaria is unknown, and several theories have been proposed. Firstly, modification of the RBC membrane may affect the ability of merozoites to invade RBCs and prevent the development of parasites within RBCs15. Secondly, alterations in RBC structures may impair the binding of malarial proteins from the parasite to the RBC membrane, thereby inhibiting parasite growth within RBCs39. Thirdly, SAO RBCs may provide protection against cerebral malaria due to the redistribution of sequestered infected RBCs away from the brain32. Similar to the protection against cerebral malaria, SAO RBCs may prevent parasitised RBCs from adhering to receptors in the placenta, thereby protecting against placental malaria. However, a study on placental samples of pregnant women demonstrated that SAO RBCs did not reduce the incidence of placental malaria and, therefore, did not protect against placental malaria35. Another study on pregnant women revealed that primigravidae with SAO had a lower prevalence of placental infection than primigravidae without SAO, whereas there was no difference in the prevalence and severity of placental infections between SAO and non-SAO multigravidae, indicating that the gravidae status in women with SAO confounds the association between SAO and placental infection. Thus, the mechanism by which SAO RBCs protect against placental malaria among primigravidae was suggested to be non-immune- rather than immune-based28. Since SAO RBCs protect against cerebral malaria or severe diseases but not uncomplicated diseases, this suggests that the protection involves post-invasion mechanisms, such as preventing sequestration of infected RBCs26,40,41.
Our systematic review showed heterogeneous associations between SAO and malaria in individual studies. Most studies demonstrated no association of SAO with malaria infections or severity16,17,31,32,34,35,37,38. However, some showed that ovalocytosis might protect against malaria infection15,27,29,30 or severe disease15,26,28,36. Nevertheless, our meta-analysis results demonstrated no association between SAO and malaria infection. These results were stratified according to the study design, without or with minimal heterogeneity in cohort studies35,38 and in cross-sectional studies16,17,30,34,36,37. High or substantial heterogeneity was found in three case–control studies15,26,29. Besides differences in study design, the controversial association of SAO in the literature was suggested to be caused by the presence of molecularly heterogeneous SAO because SAO without B3∆27 was associated with decreased malaria infection rates31. Additionally, another study indicated that the inconsistency of SAO-related protection against malaria might be due to the detection of SAO with low sensitivity34.
Our systematic review and meta-analysis had several limitations. Firstly, the number of studies included in the meta-analysis was limited, which might limit the interpretation of the results. Nonetheless, because the results of the studies included in the meta-analysis were consistent, the findings were sufficiently robust to support the conclusion that there is no link between SAO and malaria infection. Secondly, a meta-analysis of the odds of severe disease between severe and non-severe diseases could not be performed due to the limited number of studies reporting an association between SAO and malaria severity. Third, there was heterogeneity in the association between ovalocytosis and malaria infection between studies. Although we conducted a meta-regression analysis, no probable source of heterogeneity was found. Fourth, although our meta-analysis revealed that ovalocytosis did not protect against P. vivax malaria, some studies have suggested that SAO mainly protects against P. vivax malaria. Thus, it would be interesting for further studies to refine the investigation to that of P. vivax exclusively to assess the extent of this protection without any interference from a concomitant P. falciparum infection.
Conclusion
Our systematic review revealed the heterogeneity of individual studies regarding the association between SAO and malaria. However, our meta-analysis results demonstrated no protection of SAO RBCs against malaria infection. Hence, the association of SAO with malaria infection or disease severity should be further investigated by larger studies.
Data availability
All data relating to the present study are available in this manuscript and supplementary files.
References
Mahittikorn, A., Masangkay, F. R., Kotepui, K. U., Milanez, G. J. & Kotepui, M. Comparison of Plasmodium ovale curtisi and Plasmodium ovale wallikeri infections by a meta-analysis approach. Sci. Rep. 11(1), 6409 (2021).
Mahittikorn, A., Masangkay, F. R., Kotepui, K. U., Milanez, G. J. & Kotepui, M. Quantification of the misidentification of Plasmodium knowlesi as Plasmodium malariae by microscopy: An analysis of 1569 P. knowlesi cases. Malar. J. 20(1), 179 (2021).
Sukkanon, C. et al. Prevalence of Plasmodium spp. in Anopheles mosquitoes in Thailand: A systematic review and meta-analysis. Parasit Vectors. 15(1), 285 (2022).
WHO. World malaria report 2022. Available from: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2022. Accessed 5 February 2023.
Hviid, L. & Jensen, A. T. PfEMP1 - A parasite protein family of key importance in Plasmodium falciparum malaria immunity and pathogenesis. Adv. Parasitol. 88, 51–84 (2015).
Salinas, N. D. & Tolia, N. H. Red cell receptors as access points for malaria infection. Curr. Opin. Hematol. 23(3), 215–223 (2016).
Moulin, P. A. et al. Southeast asian ovalocytosis: The need for a carefull observation of red cell indices and blood smear. Ann. Biol. Clin. (Paris). 75(6), 699–702 (2017).
Yamsri, S., Kawon, W., Duereh, A., Fucharoen, G. & Fucharoen, S. Southeast Asian ovalocytosis and hemoglobinopathies in newborns: Prevalence, molecular, and hematologic analyses. J. Pediatr. Hematol. Oncol. 43(3), e341–e345 (2021).
Tanner, M. J. Band 3 anion exchanger and its involvement in erythrocyte and kidney disorders. Curr. Opin. Hematol. 9(2), 133–139 (2002).
Reithmeier, R. A. et al. Band 3, the human red cell chloride/bicarbonate anion exchanger (AE1, SLC4A1), in a structural context. Biochim. Biophys. Acta. 1858(7 Pt A), 1507–1532 (2016).
Kay, M. M. Band 3 and its alterations in health and disease. Cell Mol. Biol. (Noisy-le-grand) 50(2), 117–138 (2004).
Mohandas, N., Lie-Injo, L. E., Friedman, M. & Mak, J. W. Rigid membranes of Malayan ovalocytes: A likely genetic barrier against malaria. Blood 63(6), 1385–1392 (1984).
Kidson, C., Lamont, G., Saul, A. & Nurse, G. T. Ovalocytic erythrocytes from Melanesians are resistant to invasion by malaria parasites in culture. Proc. Natl. Acad. Sci. U S A. 78(9), 5829–5832 (1981).
De Meulenaere, K. et al. Band 3-mediated Plasmodium vivax invasion is associated with transcriptional variation in PvTRAg genes. Front. Cell Infect. Microbiol. 12, 1011692 (2022).
Rosanas-Urgell, A. et al. Reduced risk of Plasmodium vivax malaria in Papua New Guinean children with Southeast Asian ovalocytosis in two cohorts and a case-control study. PLoS Med. 9(9), 1–11 (2012).
Fowkes, F. J. et al. Host erythrocyte polymorphisms and exposure to Plasmodium falciparum in Papua New Guinea. Malar. J. 7, 1 (2008).
Kimura, M., Soemantri, A. & Ishida, T. Malaria species and Southeast Asian ovalocytosis defined by a 27-bp deletion in the erythrocyte band 3 gene. Southeast Asian J. Trop. Med. Public Health. 33(1), 4–6 (2002).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Moola, S. et al. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid. Based Healthc. 13(3), 163–169 (2015).
GA Wells, B Shea, D O'Connell, J Peterson, V Welch, M Losos, P Tugwell. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2021 [Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 12 April 2023.
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials. 45(Pt A), 139–145 (2015).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327(7414), 557–560 (2003).
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., Welch, V. A. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane; 2022 [Available from: www.training.cochrane.org/handbook. Accessed 5 February 2023.
Lin, L. & Chu, H. Quantifying publication bias in meta-analysis. Biometrics 74(3), 785–794 (2018).
Duval, S. & Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56(2), 455–463 (2000).
Allen, S. J. et al. Prevention of cerebral malaria in children in Papua New Guinea by southeast Asian ovalocytosis band 3. Am. J. Trop. Med. Hyg. 60(6), 1056–1060 (1999).
Apibal, S., Suwannurak, R., Bunyaratvej, A., Bunyaratvej, P. & Boonpucknavig, V. Increased ovalocytic red cells and their low parasitemia in malaria infected subjects. J. Med. Assoc. Thai. 72(3), 129–131 (1989).
Benet, A. et al. Placental malaria in women with South-East Asian ovalocytosis. Am. J. Trop. Med. Hyg. 75(4), 597–604 (2006).
Cattani, J. A., Gibson, F. D., Alpers, M. P. & Crane, G. G. Hereditary ovalocytosis and reduced susceptibility to malaria in Papua New Guinea. Trans. R. Soc. Trop. Med. Hyg. 81(5), 705–709 (1987).
Foo, L. C., Rekhraj, V., Chiang, G. L. & Mak, J. W. Ovalocytosis protects against severe malaria parasitemia in the Malayan aborigines. Am. J. Trop. Med. Hyg. 47(3), 271–275 (1992).
Kimura, M., Soemantri, A., Siswanto, J. E. & Ishida, T. Ovalocytosis without band 3 gene 27-bp deletion and malaria infection. Anthropol. Sci. 114(2), 161–164 (2006).
Lin, E. et al. Minimal association of common red blood cell polymorphisms with Plasmodium falciparum infection and uncomplicated malaria in Papua New Guinean school children. Am. J. Trop. Med. Hyg. 83(4), 828–833 (2010).
Manning, L. et al. Features and prognosis of severe malaria caused by Plasmodium falciparum, Plasmodium vivax and mixed Plasmodium species in Papua New Guinean children. PLoS ONE 6(12), 1–9 (2011).
O’Donnell, A. et al. Red cell morphology and malaria anaemia in children with Southeast- Asian ovalocytosis band 3 in Papua New Guinea. Br. J. Haematol. 101(3), 407–412 (1998).
O’Donnell, A., Raiko, A., Clegg, J. B., Weatherall, D. J. & Allen, S. J. Southeast Asian ovalocytosis and pregnancy in a malaria-endemic region of Papua New Guinea. Am. J. Trop. Med. Hyg. 76(4), 631–633 (2007).
Serjeantson, S., Bryson, K., Amato, D. & Babona, D. Malaria and hereditary ovalocytosis. Hum. Genet. 37(2), 161–167 (1977).
Shimizu, H., Tamam, M., Soemantri, A. & Ishida, T. Glucose-6-phosphate dehydrogenase deficiency and Southeast Asian ovalocytosis in asymptomatic Plasmodium carriers in Sumba island, Indonesia. J. Hum. Genet. 50(8), 420–424 (2005).
Stanisic, D. I. et al. Risk factors for malaria and adverse birth outcomes in a prospective cohort of pregnant women resident in a high malaria transmission area of Papua New Guinea. Trans. R. Soc. Trop. Med. Hyg. 109(5), 313–324 (2015).
Aikawa, M. Morphological changes in erythrocytes induced by malarial parasites. Biol. Cell. 64(2), 173–181 (1988).
Genton, B. et al. Ovalocytosis and cerebral malaria. Nature 378(6557), 564–565 (1995).
Mgone, C. S. et al. Occurrence of the erythrocyte band 3 (AE1) gene deletion in relation to malaria endemicity in Papua New Guinea. Trans. R. Soc. Trop. Med. Hyg. 90(3), 228–231 (1996).
Author information
Authors and Affiliations
Contributions
M.K., K.U.K., and A.M. carried out the study design, study selection, data extraction, and statistical analysis; and drafted the manuscript. K.U.K. and F.R.M. reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kotepui, K.U., Mahittikorn, A., Masangkay, F.R. et al. Association between ovalocytosis and Plasmodium infection: a systematic review and meta-analysis. Sci Rep 13, 7164 (2023). https://doi.org/10.1038/s41598-023-34170-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34170-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.