Abstract
Handgrip strength (HGS) now draws attention as one of the predictors of outcomes following geriatric hip fracture; however, its effectiveness and the optimal time to assess HGS remain unknown. Herein, we aimed to determine the usefulness of HGS in predicting the outcomes of geriatric hip fracture and to find the most effective time to measure HGS in both the low muscle strength and normal hip fracture groups. The study was performed prospectively for 79 geriatric hip fracture patients. HGS was measured during the admission period and the one-week postoperative period. Walking ability and quality of life were assessed using Koval scores and the European Quality of Life Five Dimension (EQ-5D) scale at the admission period and postoperatively at 3, 6, and 12 months, respectively. The relationship between pre/postoperative HGS and functional outcomes was assessed, and the functional score between the “low muscle strength” and “normal muscle strength” groups was compared. The association between HGS asymmetry and low strength with functional limitations was determined. For the preoperative HGS, the Koval score showed a significant relationship in the postoperative 6-month (r = −0.295, P = 0.008) and 12-month (r = −0.266, P = 0.019) periods; also, the EQ-5D score showed a significant relationship in the postoperative 6-month and 12-month periods (r = 0.344, P < 0.001, and r = 0.386, P = 0.001, respectively). For the postoperative HGS, the Koval score showed a significant relationship in the 6-month (r = −0.432, P < 0.001) and 12-month (r = −0.344, P = 0.002) postoperative periods. Also, the EQ-5D score showed a significant relationship in the 3-month (r = 0.340, P = 0.010), 6-month (r = 0.476, P < 0.001), and 12-month (r = 0.471, P < 0.001) postoperative periods. The incidence of preoperative and postoperative low HGS was 78.5% and 70.9%, respectively. The “low-strength” group had poor Koval scores and EQ-5D at postoperative month 12 and poor functional outcomes earlier in the follow-up (postoperative 6- and 12-month Koval scores and postoperative 3-, 6-, and 12-month EQ-5D), respectively (P = 0.008 and P = 0.003; P = 0.003, P = 0.001, and P = 0.001). The effect of HGS asymmetry and low strength on functional limitations remained undetermined. Both preoperative and postoperative HGS reflected functional outcomes of patients with hip fracture during the 12-month follow-up. Postoperative HGS had a higher prognostic value than preoperative HGS.
Similar content being viewed by others
Introduction
Hip fracture is a common but serious injury that increases in incidence with the aging of the population1. As the older adult population increases worldwide, hip fracture incidence is expected to increase 1.7-fold from 2016 to 2025, and threefold between 2016 and 20502,3. Hip fracture is a major health problem associated with high mortality, morbidity, and cost4,5,6. An effort to identify prognostic factors for hip fracture has revealed that sarcopenia, age, previous functional status, medical history of dementia, and delirium during admission as predictors of functional recovery7,8. Sarcopenia, an important quantifiable factor, is a geriatric syndrome characterized by the loss of muscle mass and function with aging9. Hand grip strength (HGS) has been used as an important index of low muscle strength to diagnose sarcopenia10, and is promising because it is a simple and reliable prognostic indicator for hip fractures11.
Various studies have investigated the relationship between HGS and the functional outcome of geriatric hip fractures; however, there are still a lot of controversial results12,13,14,15,16,17,18,19,20. Although some studies have demonstrated no relationship between HGS and functional outcomes16,20, most were retrospective studies with relatively short follow-up periods of less than 6 months. Additionally, a difference in HGS according to the timing of the measurement (preoperative vs. postoperative) has been observed, begging the question of which measurement would hold better predictive value for functional outcomes after hip fracture. Some researchers measured the HGS of patients with hip fractures immediately after hospital admission based on the maintained muscle mass during the acute post-fracture stage14,15,19,21. Other studies that used HGS data after surgery to predict hip fracture risk or investigate hip fracture prognosis showed contradictory results13,17.
Therefore, this study aimed to clarify the effectiveness of HGS by analyzing its relationship with functional outcomes, such as Koval scores and the European Quality of Life Five Dimension (EQ-5D) scale, in patients with geriatric hip fracture and to demonstrate the optimal timing for HGS measurement as a prognostic indicator for functional outcomes.
Materials and methods
Study design and patients
This was a prospective, observational study of patients with hip fracture in a single center (university hospital) from June 2018 to December 2019. The study was approved by our institutional review board, and all patients provided their written informed consent. All of the consecutive patients meeting the following inclusion criteria were enrolled: (i) aged ≥ 60 years; (ii) had undergone operative treatment of proximal femoral fracture, which was defined as a femur neck fracture or intertrochanteric femoral fracture (AO/OTA 31)22, and subtrochanteric fracture (fractures extending 5 cm below the lower border of the lesser trochanter)23; and (iii) low-energy injury due to falls from heights of 1 m or less24. We excluded patients with: (i) pathologic fracture, (ii) inability to walk before fracture, (iii) multiple fractures, such as combined fragility upper extremity fractures, ipsilateral lower extremity fractures, or bilateral hip fractures, (iv) prophylactic fixation, (v) periprosthetic fracture, and (vi) delayed surgery with neglected fracture.
Treatment details
Patients with femoral neck fracture underwent bipolar hemiarthroplasty or internal fixation with multiple screws, whereas those with intertrochanteric and subtrochanteric fractures underwent intramedullary nailing. All patients underwent the same standardized postoperative rehabilitation program and were encouraged to practice early assisted ambulation. Patients underwent wheelchair ambulation on the first postoperative day, followed by standing exercises and tolerable weight-bearing exercises with a walking aid (walker or crutches) supervised by a physiatrist and a therapist. All patients were generally discharged 5–7 days after admission and were followed up at postoperative week 4, and month 3, 6, and 12.
Data collection
Patient demographics were collected, including age, sex, height, weight, body mass index (BMI), diagnosis (fracture site), time between admission and surgery, and length of stay.
Measurement of HGS
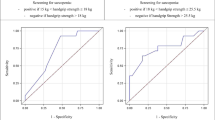
HGS was measured according to the 2019 AWGS recommendation6, using a Takei digital grip strength dynamometer (Model T.K.K.5401, Takei, Niigata, Japan). Patients performed isometric contraction a total of six times by alternating both hands. The patients were instructed to grip as hard as possible25, and the data from the best performance HGS from both hands were used for the analyses. The HGS was measured with 90° elbow flexion in the sitting position on a bed or chair. However, the preoperative test was performed in the supine position due to pain limiting the sitting position. The preoperative HGS was measured at initial ward admission, and postoperative (pre-discharge) HGS was measured at approximately 1 week post-fracture. According to the diagnostic cutoff value of the 2019 Asian Working Group for Sarcopenia (AWGS)6, HGS is defined as “low strength” when the weight is less the 26 kg for men and 18 kg for women. Patients who had a HGS ratio of < 0.90 or > 1.10 were considered to have asymmetric HGS, whereas those with a HGS ratio of 0.90–1.10 had HGS symmetry26.
Evaluation of functional outcomes
Functional outcomes were measured by the Koval score to assess walking ability as a patient-reported outcome and the EQ-5D VAS scale, an international method that reflects the quality of life. The Koval score ranges from 1 to 7, indicating physical condition according to the degree of walking27. A higher score reflects a poorer walking ability28. The Koval score was measured during the admission period (preoperative period: initial ward admission), at 6 and 12 months post-fracture. The EQ-5D scale was evaluated at admission, 3, 6, and 12 months post-fracture. Functional limitation was defined in the analysis by categorizing patients with “functional limitation” when their Koval score was IV, V, VI, and VII or their EQ-5D was less than 0.529,30.
Statistical analysis
The correlations between HGS and Koval scores and EQ-5D for each period were assessed to investigate the relevance to functional recovery. We evaluated the Spearman’s rank correlation coefficient for the relationship between preoperative and postoperative HGS and functional outcomes. After performing the Kolmogorov–Smirnov normality analysis and confirming non-normal distribution, the Mann–Whitney U test was conducted to assess the differences in functional outcomes between the low-strength and normal groups. Patients were classified into four groups according to their handgrip asymmetry and strength: (1) low strength only, (2) asymmetry only, (3) asymmetry and low strength, and (4) symmetric and normal strength. Logistic regression models were used to determine the associations between the low strength and HGS asymmetry on functional limitations using group ‘symmetric and normal strength’ as a reference. All logit models were adjusted for sex, age, height, weight, BMI, psoas muscle volume, and preoperative diagnosis using multivariate analysis. All the statistical analyses were performed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA), and significance was accepted for P-values of < 0.05.
Ethical approval
All procedures involving human participants were performed in accordance with the ethical standards of the institutional committee. This study was approved by the Institutional Review Board of Asan Medical Center (protocol no. 2018-0932).
Informed consent
Informed consent was obtained from all participants.
Results
The details of patient selection and the number of patients included in the following steps are shown in Fig. 1. A total of 79 patients with a mean age of 76.1 ± 7.9 years (range, 60–96 years) participated in the study, 75.1% of whom were women. The mean BMI was 23.0 ± 3.8 kg/m2 (range, 15.2–35.7 kg/m2). There were 38 cases (48.1%) of femur neck fracture, 29 (36.7%) of intertrochanteric fracture, and 12 cases (15.2%) of subtrochanteric fracture. The average time interval from admission to surgery was 1.8 ± 2.5 days (range, 0.2–16.8), and the length of stay was 9.3 ± 7.0 days (range, 4–56). After preoperative HGS assessment, 62 patients were assigned to the low-strength group, while postoperative HGS analysis assigned a further 56 cases (70.9%). Two patients died during follow-up at postoperative months 6 and 12. Their data were collected up to 6 months after fracture (Table 1).
The relationships between pre/postoperative HGS and Koval scores are shown in Table 2. Both HGS was negatively correlated with Koval scores at postoperative months 6 (−0.295 in preoperative and −0.432 in postoperative) and 12 (−0.266 in preoperative and −0.344 in postoperative), with a stronger correlation and higher correlation coefficient observed at the postoperative HGS assessment (P = 0.001). The relationships between pre/postoperative HGS and EQ-5D scores are shown in Table 3. Patients with higher preoperative HGS had higher EQ-5D scores at postoperative months 6 and 12 (P = 0.008 and P = 0.003), whereas higher postoperative HGS was correlated with higher EQ-5D scores at postoperative months 3, 6, and 12 (P = 0.003, P = 0.001, and P = 0.001).
We compared the functional outcomes between the low and normal strength groups (Tables 4 and 5). The low-strength group had higher Koval scores and lower EQ-5Ds scores at postoperative month 12 (Table 4). When compared based on postoperative HGS, the low-strength group had higher Koval scores at postoperative months 6 and 12. The EQ-5D score was significantly lower in the low-strength group at postoperative months 3, 6, and 12 (Table 5).
The effect of low strength or weakness on functional limitations represented by the Koval score was not identified (Table 6). Patients with low strength, HGS asymmetry, or both showed no significant difference in functional limitations compared with patients with HGS symmetry and normal strength.
Discussion
Our study demonstrated that both preoperative and postoperative HGS reflected postoperative walking ability and quality of life; however, postoperative HGS had a higher prognostic value with functional outcomes than preoperative HGS. The absolute values of the correlation coefficients of postoperative HGS related with Koval scores at postoperative months 6 and 12 and the correlation coefficients of postoperative HGS related with EQ-5D scores at postoperative months 6 and 12 were higher than those at preoperative HGS analysis. In addition, the rate of low strength was significantly lower at postoperative HGS.
This study reconfirmed the importance of HGS as a prognostic factor of functional outcome in patients with hip fracture. The results are consistent with those from previous studies, confirming the prognostic role of HGS after hip fracture12,13,14,15,17,18,19. However, there was no consensus on the timing of HGS measurement, and measurements were taken at inconsistent times throughout these studies. Several studies evaluated preoperative HGS. Monaco et al. demonstrated that grip strength better predicted short-term functional outcomes in women than appendicular lean mass assessed by dual-energy X-ray absorptiometry12. Álvarez et al. concluded that HGS measured at admission for hip fracture was directly related to functional recovery in older patients19. Selakovic et al. showed that HGS measured preoperatively was associated with Barthel index scores at months 3 and 6 post-fracture15. Furthermore, Wehren et al. found a moderate correlation between grip strength and functional outcomes18. Savino et al. also concluded that high HGS at admission was related to a higher probability of independent walking recovery within 1 year of surgery14. Other studies revealed the relationship between postoperative HGS and functional outcomes. Monaco et al. assessed HGS before rehabilitation and observed the prognostic ability of functional outcome of inpatient rehabilitation and at 6 months follow-up in women with hip fractures13. Beloosesky et al. demonstrated that HGS measured 1 week after surgery was associated with the recovery of walking ability at postoperative month 617.
Only two studies found no relationship between grip strength and functional outcome. Steihaug et al. demonstrated that postoperative HGS was not significantly associated with the preoperative Barthel index16. Their study differed from the current study in the relationship between HGS and ‘pre-injury’ functional status was demonstrated, rather than functional outcome after fracture. Gonzalez-Montalvo et al. also failed to show the association between sarcopenia and short-term functional outcome in patients with hip fracture20. Limited comparisons can be drawn between this study and our present study because they did not assess the direct relationship between HGS and long-term functional outcome, including walking ability and activity of daily living, and their functional outcome was measured only at discharge at an average of 10.1 days, without further follow-up.
With respect to the time of HGS assessement, the current study revealed that postoperative HGS reflected prognosis better than preoperative HGS. The correlation coefficient of postoperative HGS with functional outcome was higher than that of preoperative HGS. In addition, postoperative HGS showed a moderate correlation with postoperative 6-month walking ability and postoperative 6- and 12-month EQ-5D. In contrast, preoperative HGS showed a weak correlation with postoperative 6- and 12-month walking ability and EQ-5D score. Although the low strength group based on preoperative HGS showed a lower walking ability and quality of life only at postoperative month 12, the same group based on postoperative HGS had lower walking abilities at postoperative months 6 and 12 and lower EQ-5D scores at postoperative months 3, 6, and 12. Therefore, we believe that postoperative HGS better reflects functional outcomes after hip fracture and is useful in predicting postoperative 6- and 12-month walking ability and quality of life.
The higher prognostic value of postoperative HGS may be attributed to the following reasons. Muscle mass is maintained during the first 10 days after fracture and begins to decrease thereafter31,32. The time difference between pre- and postoperative HGS was approximately 6 days (< 10 days); thus, the difference in HGS may not have resulted from the change in muscle mass between the measurements. First, preoperative HGS was highly influenced by pain, which would have restricted the maximum force exercised by the patients in the preoperative setting. Moreover, preoperative HGS was measured in the supine position due to hip pain, which is not the standard measurement method advocated by the American Society of Hand Therapists33. Teraoka34 reported that HGS in the supine position was weaker than that in the standing or sitting positions, owing to the influence of gravity. Therefore, we believe that the preoperative HGS could have been underestimated.
Additionally, postoperative 1-year mortality rates in geriatric hip fractures are 16% in South Korea35. One-year mortality in the current study was 2.5%, which is much lower than that of studies in the literature. We suggest that two factors might have attributed to lower mortality rates in our study. This study was a prospective cohort study, excluding patients unable to walk before fracture or delayed fracture; agreeing participants were therefore relatively healthy and active. Second, the current study was performed in a well-organized center for geriatric patients, with all surgeries performed as soon as possible by an experienced orthopedic surgeon. Integrated co-management for elderly patients and experience of the surgeon with hip fracture would reduce hospital mortality.
We also examined the associations between HGS asymmetry and weakness in functional limitations. Our analysis revealed the effect of low strength or weakness on the functional relationship, although none were statistically significant. Our study has therefore been unable to determine whether asymmetry or low strength affects functional limitation before surgery. The reliability of the study may also have been impacted due to the large difference in the number of patients in each group; (1) low strength only (n = 28), (2) asymmetry only (n = 4), (3) asymmetry and low strength (n = 28), and (4) symmetric and normal strength. (n = 19). A follow-up study would include an increase in the number of patients and intentions to study the effect of asymmetry and low strength on functional limitations before and after fracture.
There are several limitations to this study. First, this was a single-center study in a tertiary hospital, with all admitted patients of Asian descent. External validity is therefore required to support the global application of our findings. Second, two patients were lost to follow-up at 12 months, which may have affected the statistical analysis. Additionally, admission to surgery and length of stay intervals varied substantially. Patients with long hospital stays (especially 56 days) were included because of their poor condition and rehabilitation requirements. We confirmed that this did not affect the results, but the reliability may have been impacted. In addition, the functional outcomes in our study differed from those in previous studies. The following modalities were used in previous studies: Barthel index12,13,15,16,19,20; Functional Ambulation Category20; Functional Independence Measure17; Activities of Daily Living18; and Instrumental Activities of Daily Living14. Further studies may be needed to determine the most effective scoring system for measuring functional outcome in patients with hip fracture, or to determine whether the type of scoring system affects the relationship with HGS.
This study also had several strengths. First, we provided postoperative 1-year functional outcomes. Among previous studies, few had follow-up periods of 12 months14,18, of those that did, most were less than 6 months12,13,15,16,17,19. Second, previous studies were limited to one-time measurements of HGS12,13,16,17,19; however, the current study evaluated preoperative and postoperative HGS and determined the most meaningful measurement. To the best of our knowledge, this is the first study to compare the prognostic value of preoperative and postoperative HGS. In addition, we increased the validity of our study by using two indicators, walking ability and quality of life, as the functional outcomes. Our study has clinical importance in that by evaluating the value of HGS as a prognostic factor and providing an appropriate timing of HGS measurement, its value is maximized. In clinical practice, postoperative HGS measurement would be more valuable and convenient for patients and physicians when the patient is stable and in a comfortable environment without pain.
Conclusion
In this study, we confirmed that preoperative and postoperative HGS are correlated with postoperative walking ability and quality of life after hip fracture. The postoperative HGS had a higher prognostic value for functional outcomes in patients with hip fractures than preoperative HGS. Thus, postoperative HGS is recommended to better predict the functional status of patients with hip fractures in a comfortable postoperative setting.
Data availability
We did not add supplement data and materials in submission but they are available upon request to the corresponding author if required.
References
Ulrica, B. et al. The hip fracture incidence curve is shifting to the right. Acta Orthop. 80, 520–524. https://doi.org/10.3109/17453670903278282 (2009).
Cooper, C., Campion, G. & Melton, L. J. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 2, 285–289. https://doi.org/10.1007/BF01623184 (1992).
Abrahamsen, B., Staa, T. V., Ariely, R., Olson, M. & Cooper, C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos. Int. 20, 1633–1650. https://doi.org/10.1007/s00198-009-0920-3 (2009).
Braithwaite, R. S., Col, N. F. & Wong, J. B. Estimating hip fracture morbidity, mortality and costs. J. Am. Geriatr. Soc. 51, 364–370. https://doi.org/10.1046/j.1532-5415.2003.51110.x (2003).
Lloyd, B. D. et al. Recurrent and injurious falls in the year following hip fracture: A prospective study of incidence and risk factors from the sarcopenia and hip fracture study. J. Gerontol. A Biol. Sci. Med. Sci. 64, 599–609. https://doi.org/10.1093/gerona/glp003 (2009).
Chen, L. K. et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 21, 300–307. https://doi.org/10.1016/j.jamda.2019.12.012 (2020).
Pascual-Carra, M. D. et al. Fractura de cadera en el paciente anciano: factores pronóstico de mortalidad y recuperación funcional al año [Hip fracture in the elderly patient: Prognostic factors for mortality and functional recovery at one year]. Rev. Esp. Geriatr. Gerontol. 53, 247–254. https://doi.org/10.1016/j.regg.2018.04.447 (2018).
Benichou, O. & Lord, S. R. Rationale for strengthening muscle to prevent falls and fractures: A review of the evidence. Calcif. Tissue Int. 98, 531–545. https://doi.org/10.1007/s00223-016-0107-9 (2016).
Santilli, V., Bernetti, A., Mangone, M. & Paoloni, M. Clinical definition of sarcopenia. Clin. Cases Miner. Bone Metab. 11, 177–180 (2014).
Lauretani, F. et al. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 1985(95), 1851–1860. https://doi.org/10.1152/japplphysiol.00246.2003 (2003).
Lee, S. H. & Gong, H. S. Measurement and interpretation of handgrip strength for research on sarcopenia and osteoporosis. J. Bone Metab. 27, 85–96. https://doi.org/10.11005/jbm.2020.27.2.85 (2020).
Di Monaco, M. et al. Handgrip strength but not appendicular lean mass is an independent predictor of functional outcome in hip-fracture women: A short-term prospective study. Arch. Phys. Med. Rehabil. 95, 1719–1724. https://doi.org/10.1016/j.apmr.2014.04.003 (2014).
Di Monaco, M. et al. Handgrip strength is an independent predictor of functional outcome in hip-fracture women: A prospective study with 6-month follow-up. Medicine (Baltimore) 94, 542. https://doi.org/10.1097/md.0000000000000542 (2015).
Savino, E. et al. Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am. J. Med. 126, 1068-1075.e1061. https://doi.org/10.1016/j.amjmed.2013.04.017 (2013).
Selakovic, I. et al. Can early assessment of hand grip strength in older hip fracture patients predict functional outcome?. PLoS ONE 14, e0213223. https://doi.org/10.1371/journal.pone.0213223 (2019).
Steihaug, O. M. et al. Sarcopenia in patients with hip fracture: A multicenter cross-sectional study. PLoS ONE 12, e0184780–e0184780. https://doi.org/10.1371/journal.pone.0184780 (2017).
Beloosesky, Y., Weiss, A., Manasian, M. & Salai, M. Handgrip strength of the elderly after hip fracture repair correlates with functional outcome. Disabil. Rehabil. 32, 367–373. https://doi.org/10.3109/09638280903168499 (2010).
Wehren, L. E., Hawkes, W. G., Hebel, J. R., Orwig, D. L. & Magaziner, J. Bone mineral density, soft tissue body composition, strength, and functioning after hip fracture. J. Gerontol. A Biol. Sci. Med. Sci. 60, 80–84. https://doi.org/10.1093/gerona/60.1.80 (2005).
Neira Álvarez, M. et al. Grip strength and functional recovery after hip fracture: An observational study in elderly population. Eur. Geriatr. Med. 7, 556–560. https://doi.org/10.1016/j.eurger.2016.05.002 (2016).
González-Montalvo, J. I. et al. Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr. Gerontol. Int. 16, 1021–1027. https://doi.org/10.1111/ggi.12590 (2016).
Menendez-Colino, R. et al. Baseline and pre-operative 1-year mortality risk factors in a cohort of 509 hip fracture patients consecutively admitted to a co-managed orthogeriatric unit (FONDA Cohort). Injury 49, 656–661. https://doi.org/10.1016/j.injury.2018.01.003 (2018).
Meinberg, E. G., Agel, J., Roberts, C. S., Karam, M. D. & Kellam, J. F. Fracture and dislocation classification compendium-2018. J. Orthop. Trauma 32(Suppl 1), S1-s170. https://doi.org/10.1097/bot.0000000000001063 (2018).
Loizou, C. L., McNamara, I., Ahmed, K., Pryor, G. A. & Parker, M. J. Classification of subtrochanteric femoral fractures. Injury 41, 739–745. https://doi.org/10.1016/j.injury.2010.02.018 (2010).
Bergstrom, U., Bjornstig, U., Stenlund, H., Jonsson, H. & Svensson, O. Fracture mechanisms and fracture pattern in men and women aged 50 years and older: A study of a 12-year population-based injury register, Umea, Sweden. Osteoporos. Int. 19, 1267–1273. https://doi.org/10.1007/s00198-007-0549-z (2008).
Wang, C.-Y., Olson, S. L. & Protas, E. J. Test-retest strength reliability: Hand-held dynamometry in community-dwelling elderly fallers. Arch. Phys. Med. Rehabil. 83, 811–815. https://doi.org/10.1053/apmr.2002.32743 (2002).
Collins, K. et al. Handgrip strength asymmetry and weakness are differentially associated with functional limitations in older Americans. Int. J. Environ. Res. Public Health 17, 3231. https://doi.org/10.3390/ijerph17093231 (2020).
Koval, K. J., Skovron, M. L., Aharonoff, G. B., Meadows, S. E. & Zuckerman, J. D. Ambulatory ability after hip fracture: A prospective study in geriatric patients. Clin. Orthop. Relat. Res. 310, 150–159 (1995).
Group T.E. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 16, 199–208. https://doi.org/10.1016/0168-8510(90)90421-9 (1990).
Yoon, B. H. et al. Poor prognosis in elderly patients who refused surgery because of economic burden and medical problem after hip fracture. J. Korean Med. Sci. 28, 1378–1381. https://doi.org/10.3346/jkms.2013.28.9.1378 (2013).
Hoyle, C. K., Tabberer, M. & Brooks, J. Mapping the COPD assessment test onto EQ-5D. Value Health 19, 469–477. https://doi.org/10.1016/j.jval.2016.01.005 (2016).
D’Adamo, C. R. et al. Short-term changes in body composition after surgical repair of hip fracture. Age Ageing 43, 275–280. https://doi.org/10.1093/ageing/aft198 (2014).
Fox, K. M. et al. Loss of bone density and lean body mass after hip fracture. Osteoporos. Int. 11, 31–35. https://doi.org/10.1007/s001980050003 (2000).
Fess, E. E. Grip strength. in Clinical Assessment Recommendations (Casanova, J.S. ed.). 2nd edn. 41–45 (The American Society of Hand Therapists, 1992).
Teraoka, T. Studies on the peculiarity of grip strength in relation to body positions and aging. Kobe J. Med. Sci. 25, 1–17 (1979).
Ahn, S. H. et al. Osteoporosis and osteoporotic fracture fact sheet in Korea. J. Bone Metab. 27, 281–290. https://doi.org/10.11005/jbm.2020.27.4.281 (2020).
Funding
This research was supported by the Student Research Grant (2020) of University of Ulsan, College of Medicine, Seoul, Korea and by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2021R1A2C1012972).
Author information
Authors and Affiliations
Contributions
J.H.: Methodology, investigation, data curation, validation, formal analysis, writing—original draft, and visualization. C.-H.K.: investigation, formal analysis, review & editing. J.W.K.: Conceptualization, methodology, writing—original draft, review & editing, supervision, and funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Han, J., Kim, CH. & Kim, J.W. Handgrip strength effectiveness and optimal measurement timing for predicting functional outcomes of a geriatric hip fracture. Sci Rep 12, 20600 (2022). https://doi.org/10.1038/s41598-022-25177-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25177-3
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.