Abstract
Breast cancer causes morbidity and mortality among women worldwide, despite much research illuminating the genetic basis of this disease. Anti-angiogenesis therapies have been widely studied, although the association between angiopoietin-2 (ANGPT2) single nucleotide polymorphisms (SNPs) and breast cancer subtypes remains unclear. This case–control study included 464 patients with malignant breast neoplasms and 539 cancer-free females. We explored the effects of ANGPT2 SNPs on the susceptibility for a malignant breast neoplasm in a Chinese Han population. Five ANGPT2 SNPs (rs2442598, rs734701, rs1823375, 11,137,037, and rs12674822) were analyzed using TaqMan SNP genotyping. Carriers of the variant GG allele of rs1823375 were less likely than wild-type carriers to be diagnosed with clinically staged breast cancer, while females with human epidermal growth factor receptor 2 (HER2)-enriched disease carrying the CG or the CG+GG genotype at rs1823375 were significantly less likely than CC genotype carriers to be of lymph node status N1–N3. We also found that the T-T-C-A-T ANGPT2 haplotype significantly increased the risk for developing a malignant breast neoplasm by 1.385-fold (95% CI: 1.025–1.871; p < 0.05). Our study is the first to document a correlation between ANGPT2 polymorphisms and the development and progression of a malignant breast neoplasm in females of Chinese Han ethnicity.
Similar content being viewed by others
Introduction
The latest GLOBOCAN estimates of cancer incidence have revealed that female breast cancer is the most commonly diagnosed cancer worldwide, with around 2.3 million cases in 2020, which equates to 11.7% of all cancer cases1. Thus, female breast cancer is a critical component of the global health burden and this disease is particularly problematic for China, because Chinese women have the highest age-standardized rates of cancer incidence worldwide (39.10 per 100,000 population)1,2 and breast cancer was the most commonly diagnosed type of tumor in women living in China in the year 20152,3.
Despite recent improvements in 5-year patient survival rates (from 73% between 2003–2005 to 82% in 2012–2015)4, increasing numbers of women who are detected early in the disease process, as well as increased access to effective treatments for breast cancer and greater amounts of government funding for cancer control1,3,4, breast cancer remains a major health issue among Chinese women3. The current situation regarding the high burden of malignant breast neoplasms in China leaves much room for improvement.
The precise etiology of breast cancer remains unclear, although the main risk factors have been identified as female gender, older age and having a family history of breast cancer5. Several genome-wide association studies have identified gene-environment interactions and breast cancer susceptibility single nucleotide polymorphisms (SNPs) that are associated with breast cancer risk6,7. Thus, exploring risk-associated SNPs may help to estimate individual risks for developing breast cancer and assist with its earlier diagnosis.
Angiopoietin-2 (ANGPT2) is a protein coding gene found on chromosome 8 that is capable of serving as a permissive angiogenic signal in the presence of the angiogenic inducer, vascular endothelial growth factor (VEGF), as this combination may facilitate endothelial cell migration and proliferation, whereas in the absence of VEGF, ANGPT2 induces endothelial cell apoptosis and subsequent vascular regression8,9. Interestingly, a case–control study involving Turkish patients with gynecological cancers found no evidence in support of DNA sequence variations in VEGF and ANGPT2 genes and their contribution to ovarian, cervical and endometrial cancers10. In contrast, in a study involving 421 critically ill patients with acute kidney injury (AKI) who were of European ancestry, a genetic variant (rs2920656) near the ANGPT2 gene significantly lowered the risk of developing the AKI sub-phenotype AKI-SP2 and lowered plasma Ang2 levels11. In a study that enrolled Chinese Han subjects, those who had the ANGPT2 SNP rs12674822 were at increased risk for rheumatoid arthritis12, while another investigation that also involved Chinese Han subjects reported that two ANGPT2 SNPs, rs12674822 and rs11137037, were correlated with the development of lung cancer and its progression13. These findings suggest that it is worth exploring a possible correlation between ANGPT2 gene polymorphisms and breast cancer diagnosis.
This case–control study is based on blood samples obtained from 539 healthy, cancer-free women and from 464 women with malignant breast neoplasms. It sought to determine whether Chinese Han women with ANGPT2 SNPs are susceptible to developing a malignant breast neoplasm and whether these SNPs correlate with clinical disease status.
Materials and methods
Study participants
Between 2013 and 2018, we enrolled 464 female patients (cases) diagnosed with a malignant neoplasm of the breast at Dongyang People's Hospital (Dongyang, Zhejiang, China) and 539 healthy, cancer-free females (controls), each of whom provided one 5-mL blood sample. The control group inclusion criteria specified that the enrolled patients underwent physical examination in the same hospital. A healthy status was defined as an absence of cancer history or other chronic diseases. Fully informed written consent was obtained from all study participants before study entry. The trial was performed in accordance with the principles of the Declaration of Helsinki14, Good Clinical Practices, and all local laws. The Ethics Committee of Dongyang People's Hospital approved the study protocol (Approval No.2020-YX-117). Clinicopathological data included age, cigarette smoking status, alcohol consumption, clinical stage, pathological grade, estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2) and Ki-67 status. Pathohistological diagnosis relied on the World Health Organization breast tumor classification criteria and tumors were graded by the Scarff-Bloom-Richardson method15,16. Malignant breast neoplasms were classified into the following 4 subgroups: Luminal A (ER-positive [+] and/or PR+, HER2-negative [−], Ki-67 < 14%); Luminal B (ER+ and/or PR+, HER2−, Ki-67 ≥ 14%, ER+ and/or PR+, HER2+); HER2-enriched (ER−, PR−, HER2+), or as triple-negative breast cancer (TNBC; ER−, PR−, HER2−)17,18,19. A standardized questionnaire at study entry collected sociodemographic data and electronic medical records provided clinicopathological information.
Selection of ANGPT2 polymorphisms
The ANGPT2 SNPs selected for this study were identified from multi-allelic copy number variation (CNV) profiles encompassing the q23 region of chromosome 8 containing ANGPT2 genes. We screened some of these ANGPT2 SNPs with minor allele frequencies > 5% from the records held on the 1000 Genome Projects website (https://www.internationalgenome.org/), to ensure the accuracy of our genotyping. Finally, nonsynonymous SNPs rs2442598, rs734701, rs1823375, 11,137,037, and rs12674822 were selected and validated by the Single Nucleotide Polymorphism database (dbSNP) (https://www.ncbi.nlm.nih.gov/snp/), as previously described20.
Genomic DNA extraction and genotyping by real-time PCR
Total genomic DNA was extracted from peripheral blood leukocytes using a QIAamp DNA blood mini kit (Qiagen, CA, USA), according to the manufacturer’s instructions20. Extracted DNA was stored at − 20 °C and prepared for genotyping by polymerase chain reaction (PCR). DNA was dissolved in TE buffer (10 mM Tris pH 7.8, 1 mM EDTA) and stored at − 20 °C until quantitative PCR analysis. Five ANGPT2 SNP probes were purchased from Thermo Fisher Scientific Inc. (USA), and allelic discrimination analysis of ANGPT2 SNPs was assessed using a QuantStudio™ 5 Real-Time PCR system (Applied Biosystems, CA, USA), according to the manufacturer’s instructions. Data were further analyzed with QuantStudio™ Design & Analysis Software (Applied Biosystems)21,22,23. Genotyping PCR was carried out in a total volume of 10 μL containing 20–70 ng genomic DNA, 1 U Taqman Genotyping Master Mix (Applied Biosystems) and 0.25 μL probes. The protocol included an initial denaturation step at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min.
Statistical analysis
Testing for Hardy–Weinberg equilibrium was performed to examine the genotypic frequencies of ANGPT2 rs2442598, rs734701, rs1823375, rs11137037 and rs12674822 in the cancer-free controls (2 degrees of freedom [df2]). Between-group differences were considered significant if p-values were less than 0.05. Since the data were independent and normally distributed, chi-square analysis or the Fisher’s exact test was used to compare relationships between ANGPT2 SNPs and clinicopathological parameters. Odds ratios (ORs) with their 95% confidence intervals (CIs) calculated associations between genotype frequencies and the risk of a malignant breast neoplasm. To further exclude the impact of confounding variables, adjusted odds ratios (AORs) with 95% CIs were estimated by multiple logistic regression models that controlled for age. Analysis of variance (ANOVA) was used to compare the age distribution of the cases and controls, and the Scheffé test was applied for post hoc analysis. The linkage disequilibrium (LD) haplotype analysis was observed using Haploview software (version 4.2) analysis.
Results
All of the study participants were of Chinese Han ethnicity. Table 1 presents their demographic characteristics and clinical parameters. The mean age was 55.05 ± 11.75 years in the breast cancer cohort and 52.89 ± 11.36 years in the controls (p < 0.05). The majority of study participants did not smoke cigarettes or consume alcohol; among those who did, smoking was significantly more common in the control cohort than in the case cohort (2.2% vs 0.2%; p < 0.05), while alcohol consumption was more common among cases than controls (7.1% vs 3.9%; p > 0.05). Most cases were diagnosed with clinical stage I/II disease (78.7%), but pathological grade II/III (90.3%). Tumors were mostly ER+ (71.8%), PR+ (59.7%), or HER2– (66.6%) (Table 1).
ANGPT2 genotyping results of distribution frequencies for all blood samples are listed in Table 2. The genotypic frequency of the ANGPT2 genetic variant rs2442598 conformed to the Hardy–Weinberg equilibrium (χ2 value, 0.386, p = 0.825; df2) in controls. The frequencies of rs734701, rs1823375, rs11137037 and rs12674822 also satisfied the Hardy–Weinberg equilibrium (χ2 value, 4.679, p = 0.096; χ2 value, 0.889, p = 0.641; χ2 value, 0.494, p = 0.781 and χ2 value, 2.473, p = 0.290; respectively). In cases and controls, most of those with the rs2442598 SNP and rs11137037 SNP were homozygous for the AA genotype, most of those with the rs734701 SNP were homozygous for the TT genotype, most of those with the variant rs1823375 were homozygous for CC, while most of those with the variant rs12674822 were homozygous for GG (Table 2). Distributions of ANGPT2 variants rs2442598, rs734701, rs1823375, rs11137037 and rs12674822 did not differ significantly between cases and controls, even after controlling for age (Table 2).
Next, ANGPT2 alleles in patients with malignant breast neoplasms were examined to clarify the role of ANGPT2 polymorphisms in clinical stage, primary tumor size, lymph node metastasis, distant metastasis, and pathological grade. For the 464 patients with malignant breast neoplasms, a significant correlation between rs1823375 homozygous variants (CC vs GG) and clinical stage (OR: 0.274, 95% CI: 0.081–0.927, p < 0.05) was observed, which persisted when estimated by multiple logistic regression models (AOR: 0.255, 95% CI: 0.074–0.876, p < 0.05) (Table 3).
We further analyzed the correlation between clinical parameters and rs2442598, rs734701, rs1823375, rs11137037 and rs12674822 genotyping frequencies for the different breast cancer subtypes (Luminal A, Luminal B, HER2-enriched and TNBC) (Table 4). Among patients with the HER2-enriched subtype, those carrying the CG or the CG+GG allele at rs1823375 were significantly less likely than CC allele carriers to be of lymph node status N1–N3 (OR: 0.325; 95% CI: 0.112–0.940 and 0.313; 0.114–0.862, respectively) (Table 4).
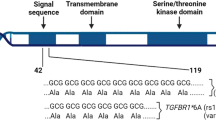
We further explored the haplotypes to evaluate the combined effects of the ANGPT2 polymorphisms on malignant breast neoplasm susceptibility. The most common haplotype in the control cohort was A-C-C-A-G (21.4%), which was therefore chosen as the reference. Compared with the reference, the T-T-C-A-T ANGPT2 haplotype significantly increased the risk for developing a malignant breast neoplasm by 1.385-fold (95% CI: 1.025–1.871; p < 0.05) (Table 5). A reconstructed linkage disequilibrium (LD) plot of the five ANGPT2 SNPs is shown in Fig. 1. Our reconstructed results illustrate one haploblock in which rs734701 and rs2442598 showed 69% LD (Fig. 1).
Discussion
Several genome-wide association studies have used genetic SNPs as potential markers for early diagnosis and targeted therapy in breast cancer24,25,26. A recent investigation attributed 18% of the familial risk of breast cancer risk to SNPs6, although any potential correlation between ANGPT2 gene polymorphisms and malignant breast neoplasms has not been explored so far. Previous studies have reported finding similar genetic characteristics in breast tumors for Chinese Han women and women of European ancestry27,28. ANGPT1, ANGPT2 and FGF2 have been linked in a US study to pathological complete responses to bevacizumab, the first approved recombinant humanized monoclonal antibody for breast cancer29, although most investigations into breast cancer genetic polymorphisms have focused on BRCA1/230,31. Our previous work found nonsynonymous ANGPT2 gene polymorphisms in lung and colorectal cancers13,20, which suggests that ANGPT2 SNPs might also be associated with a risk for breast cancer. It is therefore important and appropriate to investigate the impacts of ANGPT2 genetic variants upon the risk of malignant breast neoplasms among women of Chinese Han ethnicity.
Based on blood samples from 539 healthy, cancer-free women and 464 women with malignant breast neoplasms, we found no significant between-group distribution frequencies for any of the five ANGPT2 SNPs. We therefore sought to determine whether any of the ANGPT2 SNPs correlated with clinical status or the pathological grade of the tumors. In analyses adjusted for confounding factors, patients carrying the GG allele at rs1823375 were at lower risk for developing clinically staged breast cancer. Interestingly, our previous research revealed that this variant rs1823375 increased the risk of colorectal cancer in a Chinese Han cohort20. A possible explanation for this difference in risk between different cancer types is that gender has disparate effects, but this requires further research.
We also found that the variant rs1823375 lowered the risk of developing lymph node metastasis in patients with HER2+ disease. A recent study reported that stromal overexpression of the SNAIL transcription factor SNAI2 is linked to poor prognosis in patients with Luminal B HER2+ breast cancer, while the absence of SNAI2 in the stroma of Luminal B HER2+ breast tumor cells is associated with lower levels of plasma Ang232. Another study has indicated that ANGPT2 variants rs2515409 and rs13269021 are associated with pathological complete responses to bevacizumab treatment in breast cancer29. Accordingly, ANGPT2 mRNA levels and survival rates in women with breast cancer deserve more investigation in future clinical trials.
LD in the human genome is critical for genetic variation and features in the detection and treatment of disease33. Haplotype analyses can provide significant statistical power for clarifying the contribution of genes to disease susceptibility34. To analyze the common haplotypes, we used Haploview software and the PHASE program. As shown in Fig. 1, we identified three LD haploblocks (rs2442598, rs734701 and rs12674822) that were minimally associated with the risk of malignant breast neoplasms; other SNPs were outside the haploblock. Details of the underlying mechanisms require further investigations. When we analyzed the contributions of different haplotype combinations of the five ANGPT2 variants investigated in this study upon the risk of a malignant breast neoplasm, we found that the TTCAT haplotype increased the risk. It is possible that the ANGPT2 TTCAT haplotype is in LD with other functional polymorphisms that increase the susceptibility for a malignant breast neoplasm.
The main strength of our study is its systematic analysis of ANGPT2 SNPs and susceptibility to malignant breast neoplasms in our study population. Potential limitations include the possibility that the study observations merely reflect a cross-sectional relationship instead of actual causality. Moreover, the study participants were all enrolled from only one hospital, which gives rise to possible selection bias. Lastly, our modest sample size requires a larger, independent cohort study to confirm our findings.
Conclusion
In conclusion, our systematic genotyping results demonstrate an association between ANGPT2 gene variants and susceptibility for a malignant breast neoplasm and its progression among Chinese Han women. In this study, the ANGPT2 rs1823375 polymorphism appeared to be protective against clinically staged breast cancer and also lymph node disease, while the T-T-C-A-T ANGPT2 haplotype appeared to significantly increase the risk for developing a malignant breast neoplasm. These findings suggest that the rs1823375 polymorphism can serve as a diagnostic marker for malignant breast neoplasms.
Data availability
The data are not publicly available due to the records containing private information of the study participants. However, data are available from the authors upon reasonable request and with permission of Chao-Qun Wang and Chen-Ming Su. The datasets generated and/or analyzed during the current study are available in the 1000 Genome Projects repository (https://www.internationalgenome.org/) and the dbSNP repository (https://www.ncbi.nlm.nih.gov/snp/).
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Qiu, H., Cao, S. & Xu, R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun. (Lond.) 41(10), 1037–1048 (2021).
Cao, M., Li, H., Sun, D. & Chen, W. Cancer burden of major cancers in China: A need for sustainable actions. Cancer Commun. (Lond.) 40(5), 205–210 (2020).
Zeng, H. et al. Changing cancer survival in China during 2003–15: A pooled analysis of 17 population-based cancer registries. Lancet Glob. Health 6(5), e555–e567 (2018).
Practice Bulletin Number 179. Breast cancer risk assessment and screening in average-risk women. Obstet. Gynecol. 130(1), e1–e16 (2017).
Lilyquist, J., Ruddy, K. J., Vachon, C. M. & Couch, F. J. Common genetic variation and breast cancer risk-past, present, and future. Cancer Epidemiol. Biomark. Prev. 27(4), 380–394 (2018).
Fanale, D. et al. Breast cancer genome-wide association studies: There is strength in numbers. Oncogene 31(17), 2121–2128 (2012).
Carmeliet, P. & Jain, R. K. Molecular mechanisms and clinical applications of angiogenesis. Nature 473(7347), 298–307 (2011).
Saharinen, P., Eklund, L. & Alitalo, K. Therapeutic targeting of the angiopoietin-TIE pathway. Nat. Rev. Drug Discov. 16(9), 635–661 (2017).
Konac, E. et al. Lack of association between − 460 C/T and 936 C/T of the vascular endothelial growth factor and angiopoietin-2 exon 4 G/A polymorphisms and ovarian, cervical, and endometrial cancers. DNA Cell Biol. 26(7), 453–463 (2007).
Bhatraju, P. K. et al. Genetic variation implicates plasma angiopoietin-2 in the development of acute kidney injury sub-phenotypes. BMC Nephrol. 21(1), 284 (2020).
Dai, C. et al. Correlation between genetic polymorphism of angiopoietin-2 gene and clinical aspects of rheumatoid arthritis. Int. J. Med. Sci. 16(2), 331–336 (2019).
Hu, W. et al. Correlations between angiopoietin-2 gene polymorphisms and lung cancer progression in a Chinese Han population. J. Cancer 10(13), 2935–2941 (2019).
World Medical, A. World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310(20), 2191–2194 (2013).
Elston, C. W. & Ellis, I. O. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: Experience from a large study with long-term follow-up. Histopathology 19(5), 403–10 (1991).
Elston, C. W. & Ellis, I. O. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: Experience from a large study with long-term follow-up. Histopathology 41(3A), 154–61 (2002).
Wang, C. Q. et al. Impacts of RETN genetic polymorphism on breast cancer development. J. Cancer 11(10), 2769–2777 (2020).
Wang, C. Q. et al. Fascin-1 as a novel diagnostic marker of triple-negative breast cancer. Cancer Med. 5(8), 1983–1988 (2016).
Wang, C. Q. et al. FSCN1 gene polymorphisms: Biomarkers for the development and progression of breast cancer. Sci. Rep. 7(1), 15887 (2017).
Du, Z. et al. Angiopoietin-2 gene polymorphisms are biomarkers for the development and progression of colorectal cancer in Han Chinese. Int. J. Med. Sci. 17(1), 97–102 (2020).
Zhang, L., Zhang, Y., Tang, C. H. & Su, C. M. RAD52 gene polymorphisms are associated with risk of colorectal cancer in a Chinese Han population. Medicine (Baltimore) 96(49), e8994 (2017).
Yang, Y. C. et al. Melatonin reduces lung cancer stemness through inhibiting of PLC, ERK, p38, beta-catenin, and Twist pathways. Environ. Toxicol. 34(2), 203–209 (2019).
Chen, Y. A. et al. Simvastatin sensitizes radioresistant prostate cancer cells by compromising DNA double-strand break repair. Front. Pharmacol. 9, 600 (2018).
King, M. C., Marks, J. H., Mandell, J. B., New York Breast Cancer Study, G. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302(5645), 643–6 (2003).
Stratton, M. R. & Rahman, N. The emerging landscape of breast cancer susceptibility. Nat. Genet. 40(1), 17–22 (2008).
Fanfani, V., Zatopkova, M., Harris, A. L., Pezzella, F. & Stracquadanio, G. Dissecting the heritable risk of breast cancer: From statistical methods to susceptibility genes. Semin. Cancer Biol. 72, 175–184 (2021).
Yu, K., Lee, C. H., Tan, P. H. & Tan, P. Conservation of breast cancer molecular subtypes and transcriptional patterns of tumor progression across distinct ethnic populations. Clin. Cancer Res. 10(16), 5508–5517 (2004).
Fan, L. et al. Breast cancer in China. Lancet Oncol. 15(7), e279–e289 (2014).
Makhoul, I. et al. Germline genetic variants in TEK, ANGPT1, ANGPT2, MMP9, FGF2 and VEGFA are associated with pathologic complete response to bevacizumab in breast cancer patients. PLoS One 12(1), e0168550 (2017).
Robson, M. et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N. Engl. J. Med. 377(6), 523–533 (2017).
Chai, Y. et al. Homologous recombination deficiency (HRD) and BRCA 1/2 gene mutation for predicting the effect of platinum-based neoadjuvant chemotherapy of early-stage triple-negative breast cancer (TNBC): A systematic review and meta-analysis. J. Pers. Med. 12(2), 323 (2022).
Blanco-Gomez, A. et al. Stromal SNAI2 Is required for ERBB2 breast cancer progression. Cancer Res. 80(23), 5216–5230 (2020).
Devlin, B. & Risch, N. A comparison of linkage disequilibrium measures for fine-scale mapping. Genomics 29(2), 311–322 (1995).
Shifman, S. et al. A highly significant association between a COMT haplotype and schizophrenia. Am. J. Hum. Genet. 71(6), 1296–1302 (2002).
Acknowledgements
We thank Iona J. MacDonald from China Medical University for her English language editing of this manuscript.
Funding
This work was supported by grants from National Natural Science Foundation of China (No. 81802660) and China Medical University (CMU-108-MF-111).
Author information
Authors and Affiliations
Contributions
Conceptualization, G.-N.H., C.-Q.W., and C.-M.S.; formal analysis, C.-H.T., L.-L.J.; resources, Y.W., B.-F.H., Q.W., J.-K.S.; writing—C.-M.S.; writing—review and editing, C.-Q.W. and C.-M.S. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, GN., Wang, Y., Tang, CH. et al. The impact of Angiopoietin-2 genetic polymorphisms on susceptibility for malignant breast neoplasms. Sci Rep 12, 14522 (2022). https://doi.org/10.1038/s41598-022-18712-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18712-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.