Abstract
A 75–89% expulsion rate is reported for ureteric stones ≤ 5 mm. We explored which parameters predict justified surgical intervention in cases of pain caused by < 5 mm ureteral stones. We retrospectively reviewed all patients with renal colic caused by ureteral stone < 5 mm admitted to our urology department between 2016 and 2021. Data on age, sex, body mass index, the presence of associated hydronephrosis/stranding on images, ureteral side, stone location, medical history, serum blood count, creatinine, C-reactive protein, and vital signs were obtained upon admission. XGboost (XG), a machine learning model has been implemented to predict the need for intervention. A total of 471 patients (median age 49, 83% males) were reviewed. 74% of the stones were located in the distal ureter. 160 (34%) patients who sustained persistent pain underwent surgical intervention. The operated patients had proximal stone location (56% vs. 10%, p < 0.001) larger stones (4 mm vs. 3 mm, p < 0.001), longer length of stay (3.5 vs. 3 days, p < 0.001) and more emergency-room (ER) visits prior to index admission (2 vs. 1, p = 0.007) compared to those who had no surgical intervention. The model accuracy was 0.8. Larger stone size and proximal location were the most important features in predicting the need for intervention. Altogether with pulse and ER visits, they contributed 73% of the final prediction for each patient. Although a high expulsion rate is expected for ureteral stones < 5 mm, some may be painful and drawn out in spontaneous passage. Decision-making for surgical intervention can be facilitated by the use of the present prediction model.
Similar content being viewed by others
Introduction
Renal colic due to ureteral stone is among the most common reasons for acute admissions to a hospital urology department. This may be explained by the relatively high lifetime prevalence of ureteral stone, recently estimated at 14%1. While there is almost no question about the need for surgical intervention in the case of large ureteric stones, the treatment protocol for stones < 5 mm may vary.
The English literature reports a 71–98% stone expulsion rate for distal ureteral stones < 5 mm2 and 75–89% for any ureteral stone ≤ 5 mm3,4,5. The highest odds of spontaneous expulsion are estimated for stones in the distal ureter5,6, and they generally increase as the stone location in the ureter lowers3,4.
The current European Association of Urology and Canadian Association of Urology guidelines suggest that 95% of the 4–5 mm ureteral stones are expected to pass spontaneously within 40 days7,8. The authors of a recent study revealed that most of these stones passed within 4 weeks and at an average of 17 days, and therefore recommended surgical intervention only after 4 weeks of non-expulsion of the small stone(s)3. Moreover, two recent studies found that early surgical intervention for stones < 5 mm was not recommended4,9 since 30% of early intervention cases for any ureteral stone required subsequent hospital-based care9.
Patients with renal colic due to ureteric stones < 5 mm admitted for pain fall between the cracks. The obvious purpose of their admission is to control their pain and render them entirely pain-free for discharge and outpatient follow-up. Some of them, however, will experience pain that will eventually require surgical intervention. In the present study, we sought to identify the parameters that may predict the eventual need for surgical intervention in those cases of persistent pain caused by ureteral stone(s) < 5 mm. Such information may help in guiding management decision-making to either spare a patient from undergoing surgery and hospitalization for a stone that is highly likely to pass spontaneously or, alternatively, to spare a patient from enduring weeks of pain from a stone that is not.
Patients and methods
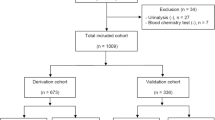
Following approval of our institutional review board (Chaim Sheba Medical Center, #SMC-20-6942), we retrospectively reviewed all admissions to our urology department between June 1, 2016 and October 31, 2021 that were coded 788.0 (renal colic) as per the International Classification of Disease, 9th edition, Clinical Modification (ICD9-CM). Out of those admissions, we retrieved all cases of renal colic caused by a ureteral stone < 5 mm according to the medical record. The relevant images (i.e., ultrasound [US] and computerized tomography [CT]) contained in each medical record were re-evaluated by a single fellowship-trained senior endourologist (DEZ). The stone’s maximal diameter was evaluated on the coronal CT plane as described elsewhere10. Given the retrospective nature of this study, informed consent has been waived by the Chaim Sheba Medical Center ethics committee.
Exclusion criteria
Excluded were individuals who were < 18 years of age, had fever on admission (i.e.: body temperature > 38 °C/100.4 °F), pregnant women, and patients with bilateral ureteral or multiple ipsilateral ureteral stones, anatomic anomalies (double complete or incomplete collecting system, horseshoe kidney, pelvic kidney, crossed-ectopic kidney), a concomitant ureteral tumor in the ipsilateral side, a single kidney and previous ureteral surgeries (e.g., re-implantation, segmental ureterectomy, or endoscopic treatment for ureteric stricture).
Skeletal contractures were also an exclusion criterion, given their potential to distort the normal ureteral course and adversely affect stone expulsion.
Features of data extraction
We conducted a meticulous review of the relevant English literature in order to identify all possible factors that could predict spontaneous stone passage and built our database in accordance with variables that had been associated with stone expulsion or were explored in earlier studies on such a possible association. The variables that were extracted and included in our current analysis were : age and sex9,10,11,12,13,14, body mass index (BMI)13, the presence of concomitant diabetes mellitus (DM)/hypertension (HTN)/dyslipidemia11,12, history of ureteral stones11,13, hydronephrosis on imaging studies9,10,12,15, perinephric stranding on imaging studies10,12,15, ureteral side14, stone location (proximal/distal ureter)3,5,9,12,14, serum white blood cell (WBC) count11,13,16, neutrophil percentage (polymorphonuclears [PMN])10,16,17, creatinine level10,11,12,13, C-reactive protein (CRP) level13,17,18, and length of hospital stay9. Additional variables included vital signs on admission (pulse, systolic/diastolic blood pressure) as well as the total number of visits to the emergency room before the index admission.
Clinical management
All of the study patients had been admitted to our urology department due to pain associated with a < 5 mm ureteral stone. The aim of the admission was pain control. Based upon the findings reported by Pickard et al.19, none of our patients received medical expulsive therapy of any kind. The patients who had been successfully treated conservatively were scheduled for a follow-up visit in our outpatient clinic with repeat US and serum creatinine level. The aim of that visit was to confirm stone expulsion and schedule another visit when it had not occurred or when the findings were not clear. Patients experiencing intractable pain—i.e.: irresponsive or partially responsive to various pain medications (including IV opiates) and did not enable home discharge—subsequently underwent in-house surgical intervention, preferably primary ureteroscopy and, whenever impossible at that time (due to tight ureter), they underwent a ureteral JJ-stent insertion procedure followed by definitive surgery at a later time.
Further considerations
Time to surgery or time to expulsion was calculated from the first presentation of renal colic11. The date of stone expulsion was defined as either the day on which the patient reported stone expulsion or the day an imaging study ruled out the presence of an obstructing stone. In our country, health system is public and centralized in an electronic health system that captures all visits in other healthcare services including auxiliary images, blood tests and surgical procedures preformed outside our hospital even if the patient failed to show up for a follow-up visit.
Statistical analysis
Data are presented as frequencies (percentages) for categorical variables or as median (interquartile range [IQR]) for continuous variables. Continuous variables were compared with the Wilcoxon rank-sum test. Categorical variables were compared with the Fisher exact test. Missing data were imputed with multivariate imputation via chained equations20. The entire cohort was randomly split into a training set (80%) and a test set (20%). Extreme Gradient Boosting (XG Boost, XG) is a machine learning algorithm for regression and classification which uses an ensemble of weak prediction models, typically decision trees. As an ensemble tree model, XG uses multiple iterative gradient boosters to construct a strong classification system. As a non-linear classifier, XG is able to capture non-linear relations between features, which logistic regression cannot. XG is fast, provides high performance and has been used extensively in the medical field. We used XG with tenfold cross validation to train the model with the training set. An automated grid search was performed to identify the optimal hyperparameters of the model. Model performance was assessed with the Receiver – Operating characteristic (ROC) curve. The optimal probability cut-point for predicting the need for intervention was assessed with the Youden's index. Shapley Additive Explanation (SHAP) scores were used to identify each variable influence on the final prediction21. We reported the SHAP score in units of change in prediction probability and defined them as ‘variable importance’. Statistical analyses were performed with R v.3.6.1: R Foundation for Statistical Computing (Vienna, Austria). Multiple comparisons were accounted for by using the false detection rate22. All tests were 2-sided, with significance considered at p < 0.05.
Ethics approval
The present study was performed in accordance with the declaration of Helsinki and was approved by Chaim Sheba Medical Center ethics committee, approval # SMC-20-6942. Given the retrospective nature of this study, informed consent has been waived by the above mentioned committee.
Results
Patients' demographics are described in Table 1. A total of 471 patients were included in this study. Their median age was 49 (41–60) years and 83% were males. Of them, 303 (64%) had no history of a ureteral stone. The majority of the stones (74%) were located in the distal ureter, and stone diameter was 3.5 (3–4.1) mm. A proximal stone location was more common in patients who needed an intervention (56% vs. 10%, respectively, p < 0.001). The operated patients had larger stones (4 mm vs. 3 mm, p < 0.001), longer length of stay (3.5 days vs. 3 days, p < 0.001) and more emergency room visits prior to index admission (2 vs. 1, p = 0.007) compared to those who had no surgical intervention. Time to surgical intervention or stone expulsion was not significantly different (7 vs. 10 days, p = 0.3).
None of the other evaluated variables were significantly different across the intervention groups.
The XG model was trained to classify patients who would and would not need surgical intervention based on their clinical features. The XG model accurately predicted the need for intervention in the training and test sets (AUC 0.8 and 0.78 respectively, Fig. 1). The optimal probability cut-point in the test set was 0.5. The accuracy, sensitivity and specificity for this cut-point were 0.88, 0.85 and 0.88 respectively. The confusion matrix with number of correct and wrong intervention prediction is depicted in Table 2. The most important features for intervention prediction were stone location and size. Specifically, proximal and larger stones increased the probability of surgical intervention. Furthermore, pulse and number of ER visits were also influential on the probability of the need for intervention. Those 4 features contributed 73% of the final prediction for each patient. Other features had smaller impact on prediction (Fig. 2).
Feature importance of the XG model. (a) SHAP values. Each dot represents a patient measurement. The figure depicts the change in prediction probability when changing a feature value. Wider range depicts higher impact on the prediction. (b) Mean feature importance. Each dot represents the features contribution to the final prediction of the model. Higher contribution represents more impact on the final prediction.
The decision curve and clinical benefit of the model are depicted in Fig. 3. Our model demonstrated a significant clinical benefit across all probability thresholds.
Discussion
Ureteral stones < 5 mm are highly likely to undergo spontaneous expulsion, and the lower they are along the ureter, the higher their chance to pass spontaneously3. This observation has dictated the conservative management recommended by urological professional associations for ureteral stones < 5 mm7,8. Nevertheless, small ureteral stones may cause persistent pain, and despite the promising expulsion statistics, it may be challenging to decide not to operate in cases that do not respond whatsoever to analgesics. Given the potential adverse effects of early surgical intervention4,9, these cases should be carefully selected. It is, therefore, of considerable importance to know what information in their initial clinical data can be used to identify the patients with pain due to any ureteral stone < 5 mm who will most likely require surgical intervention and undertake it without unnecessary delay.
Demographics
Age has been considered to negatively affect stone expulsion9,13 presumably due to decreased ureteral peristalsis with aging13. That correlation, however, was not confirmed by the results of the present study nor by those of others4,10,11,12,14. recent study found that females tend to undergo a surgical intervention more often than males9, however many studies, including the present one, failed to demonstrate that finding4,10,11,12,13,14.
BMI was rejected as a predicting factor for surgical intervention by us as well as by others13.
HTN, DM and dyslipidemia had no influence on the surgical intervention rate. Similar to us, Choi et al.12 failed to demonstrate any correlation between HTN and stone expulsion rate, however, their patients with DM were shown to have a better chance to pass their stones. The small number of their patient population (n = 26) calls for caution in accepting that conclusion.
Three studies examined previous spontaneous stone passage (SSP) and the likelihood of surgical intervention, and reached 3 different conclusions. While one study, similar to our findings, found no correlation10, another observed that a past history of nephrolithiasis directly correlated with higher odds for surgical intervention11. A third study reported a negative association between a previous SSP and the likelihood of surgical intervention13.
Imaging findings
Hydronephrosis has been widely investigated as a possible predictor of surgical intervention for ureteral stones < 10 mm. Hydronephrosis was more frequent in patients who had undergone surgery in some studies4,9,13 but neither in our study nor in others10,12.
As was the case in previous studies4,10,12, we ruled out perinephric stranding as a predicting factor for surgical intervention.
The right ureter had been associated with a higher likelihood of spontaneous expulsion14, but neither we nor others10,12 found that to be the case.
There is a consensus among all studies that explored the odds that stone size4,5,9,10,12,13,14 and location3,4,9,10,11,12,14 strongly correlated to the likelihood of spontaneous ureteral stone expulsion. In the case of distal ureteral stones 4–10 mm in size the larger the stone, the lesser the chances that it will pass spontaneously13. Another study set the threshold at a stone size of 4 mm in diameter, namely, the larger a distal ureteral stone above this threshold, the less likely it will pass spontaneously10. Interestingly, as demonstrated in our study, this applied even to cases of stones < 5 mm, which are allegedly high likely to expulse.
In the present study, patients who had undergone surgical intervention were more likely to have their stones located in the upper ureter. This finding is in line with previous studies9,11 that found the proximal ureteral location as being a strong predictor for conservative treatment failure. Similarly, a lower SSP was reported for stones located in the proximal ureter (25.4–52%) compared to the mid- and distal ureter3,4,12. Moreover, in general, the lower the stone, the higher the likelihood of SSP4,5,10,14.
Laboratory findings
The correlation between high levels of serum WBC, PMN and CRP and the likelihood of SSP has been extensively investigated with equivocal findings. Two studies found that high levels of both WBC and CRP were directly correlated with greater chance of surgical intervention13,18. This was attributed to inflammatory response around the obstructing stone13,15. Moreover, a high serum PMN level was found to be associated with a greater likelihood of surgical intervention17,18. On the other hand, 2 other studies reported the opposite, observing that higher levels of both WBC and PMN predicted a higher likelihood of SSP4,16. We, like others, found no correlation between serum WBC10, PMN10 or CRP4 levels and the likelihood of surgical intervention. In addition, the serum creatinine level was not observed by us or by others4,10,11 as being a predicting factor for surgical intervention.
Administrative information
Symptoms lasting over 3 days11 or 4 days10 correlated with a higher likelihood of surgery. Our patients who had undergone surgery, similar to those of another study9, were more likely to have a longer admission, although that factor could not serve in the present model as a predicting factor.
Alternatively, the number of ER visits prior to index admission as well as pulse rate on admission served as additional predictors for surgical intervention. We believe that they reflect pain intensity and the consequent need for surgical intervention.
The natural history of ureteral stones < 10 mm has been extensively investigated. To the best of our knowledge, this is the first study that focuses upon ureteral stones < 5 mm that are anywhere in the ureter, and that draws any conclusions with regard to the need for surgical intervention in cases essentially deemed appropriate for conservative management. The relatively large population of patients in the present study further supports its conclusions. Our prediction model has moderate-high accuracy in predicting the need for intervention (AUC-0.8), which is similar to other clinical prediction tools used in urology (i.e.: PSA and MRI for significant prostate cancer detection, 0.78 and 0.82, respectively23,24).
Since the threshold probability for intervention depends upon many factors that involve the patient, clinician and availability of hospitalization and surgical facilities, this model provides substantial clinical benefit compared to default strategies (e.g., treat all, treat none) over a wide range of likely threshold probabilities.
We are aware that these data derive from a tertiary care, high-volume center composed of highly experienced fellowship-trained teams and high availability of operating theatres. Under such conditions, the benefit of surgical intervention in selected cases outweighs its risks, a fact that is reflected in a relatively high proportion of surgical interventions in our cohort (34%). This may not be the case in other medical care facilities where team and facility availabilities are limited.
External validation may be required before this model can be implemented in clinical use.
In summary, although a high expulsion rate is expected for ureteral stones < 5 mm, some may be markedly painful and late to pass spontaneously. We determined that accounting for the 4 parameters of stone size and proximal stone location altogether with pulse rate and number of ER visits prior to index admission may facilitate decision making before embarking upon or postponing surgical intervention.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- US:
-
Ultrasound
- CT:
-
Computerized tomography
- BMI:
-
Body mass index
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- WBC:
-
White blood cell
- PMN:
-
Polymorphonuclear cells
- CRP:
-
C-reactive protein
- IQR:
-
Interquartile range
- XG Boost:
-
Extreme gradient boosting
- AUC:
-
Area under the curve
- SSP:
-
Spontaneous stone passage
References
Rukin, N. J., Siddiqui, Z. A., Chedgy, E. C. P. & Somani, B. K. Trends in upper tract stone disease in England: evidence from the hospital episodes statistics database. Urol. Int. 98, 391–396 (2017).
Segura, J. W. et al. Ureteral stones clinical guidelines pane summary report on the management of ureteral calculi. J. Urol. 158, 1915–1921 (1997).
Yallappa, S. et al. Natural history of conservatively managed ureteral stones: analysis of 6600 patients. J. Endourol. 32(5), 371–379 (2018).
Shah, T. T. et al. Factors associated with spontaneous stone passage in a contemporary cohort of patients presenting with acute ureteric colic. BJU Int. 124(3), 504–513 (2019).
Pearce, E., Clement, K. D., Yallappa, S. & Aboumarzouk, O. M. Likelihood of distal ureteric calculi to pass spontaneously: systemic review and cumulative analysis of the placebo arm of randomized-controlled trials. Urol. Int. 105, 71–76 (2021).
Hubner, W. A., Irby, P. & Stoller, M. L. Natural history and current concepts for the treatment of small ureteral calculi. Eur. Urol. 24(2), 172–176 (1993).
Turk, C., Neisius, A., Petrik, A. et al. Eau guidelines on Urolithiasis. https://uroweb.org/guideline/urolithiasis/
Ordon, M. et al. CUA guideline: management of ureteral calculi. Can. Urol. Assoc. J. 9(11–12), e837–e851 (2015).
Innes, G. D. et al. Which patients should have early surgical intervention for acute ureteral colic ?. J. Urol. 205(1), 152–158 (2021).
Modai, J. et al. Prediction of surgical intervention for distal ureteral stones. J. Endourol. 33(9), 750–754 (2019).
Bajaj, M., Yuan, L., Holmes, L., Rice, M. & Zargar-Shoshtari, K. Predictors of surgical intervention following initial surveillance for acute ureteric colic. World J. Urol. 36(9), 1477–1483 (2018).
Choi, T. et al. Analysis of factors affecting spontaneous expulsion of ureteral stones that mat predict unfavorable outcomes during watchful waiting periods: what is the influence of diabetes mellitus on the ureter ?. Korean J. Urol. 56(6), 455–460 (2015).
Ozcan, C. et al. Predictive factors for spontaneous stone passage and the potential role of serum c-reactive protein in patients with 4–10 mm distal ureteral stones: a prospective clinical study. J. Urol. 194(4), 1009–1013 (2015).
Miller, O. F. & Kane, C. J. Time to stone passage for observed ureteral calculi: a guide for patient education. J. Urol. 162(3 pt1), 688–691 (1999).
Hwang, E., Kim, Y. H., Yuk, S. M., Sul, C. K. & Lim, J. S. Factors that predict spontaneous passage of small distal ureteral stone < 5 mm. J. Endourol. 24(10), 1681–1685 (2010).
Sfoungaristos, S., Kavouras, A., Katafigiotis, I. & Perimenis, P. Role of white blood cell and neutrophil counts in predicting spontaneous stone passage in patients with renal colic. BJU Int. 110(8 Pt B), E339–E345 (2012).
Park, C. H. et al. Relationship between spontaneous passage rates of ureteral stones less than 8 mm and serum C-reactive protein levels and neutrophil percentages. Korean J. Urol. 54(9), 615–618 (2013).
Aldaqadossi, H. A. Stone expulsion rate of small distal ureteric calculi could be predicted with plasma C-reactive protein. Urolithiasis 41(3), 235–239 (2013).
Pickard, R. et al. Medical expulsive therapy in adults with ureteric colic: a multicentre, randomized, placebo-controlled trial. Lancet 386(9991), 341–349 (2015).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: multivariate imputation by chained equations in R. J. Stat. Softw. 45(3), 1–67 (2011).
Lundberg, S. M. & Lee, S. I. A unified approach to interpreting model predictions. In Proceedings of the 31st International Conference on Neural Information Processing Systems (NIPS), pp. 4768–4777 (2017).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. 57(1), 289–300 (1995).
Thompsom, I. M. et al. Operating characteristics of prostate-specific antigen in men with an initial PSA level of 3.0 ng/mL or lower. JAMA 294(1), 66–70 (2005).
Tan, C. H., Hobbs, B. P., Wei, W. & Kundra, V. Dynamic contrast enhanced MRI for the detection of prostate cancer: meta-analysis. AJR 204(4), W439–W448 (2015).
Author information
Authors and Affiliations
Contributions
M.H.: Manuscript writing, data analysis. N.K.: Manuscript editing, project development. R.H.: Data collection, data management. D.E.Z.: Protocol development, data collection, manuscript writing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Haifler, M., Kleinmann, N., Haramaty, R. et al. A machine learning model for predicting surgical intervention in renal colic due to ureteral stone(s) < 5 mm. Sci Rep 12, 11788 (2022). https://doi.org/10.1038/s41598-022-16128-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16128-z
This article is cited by
-
Prediction of spontaneous distal ureteral stone passage using artificial intelligence
International Urology and Nephrology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.