Abstract
The optimal management of very small vessel (reference diameter from 2.0 to 2.25 mm) in percutaneous coronary interventions (PCIs) is controversial. We aimed to compare the efficacy and safety of drug-coated balloons (DCBs) and drug-eluting stents (DESs) for de-novo very small vessel interventions. We conducted a retrospective analysis of consecutive patients who received very small vessel PCI with a DCB or DES between January 2018 and March 2021. The outcome measures were the incidence of ischemia-driven target lesion revascularization (TLR) and major adverse cardiac and cerebrovascular events (MACCEs) within 1 year after PCI. MACCEs were defined as the composite of ischemia-driven TLR, all-cause death, non-fatal acute coronary syndrome, stroke, or heart failure requiring hospitalization. A total of 205 patients undergoing PCI with a DCB or DES were enrolled in this study. The procedural complication rate was 2.5% in the DES group and 1.7% in the DCB group (P = 1.000). After 1-year of follow-up, the cumulative incidence of TLR was 7.2% in the DCB group and 4.9% in the DES group (P = 0.530). The cumulative incidence of MACCEs was 10.6% in the DCB group and 12.7% in the DES group (P = 0.769). Only female gender, acute coronary syndrome on presentation, and dual antiplatelet therapy duration < 3 months were significantly associated with MACCEs at 1 year, but the use of DCB or DES was not. The use of DCBs or DESs in de novo very small vessel intervention was not associated with different outcomes at 1 year.
Similar content being viewed by others
Introduction
Percutaneous coronary intervention (PCI) in small vessels (reference diameter < 2.5 mm) for coronary artery disease is a challenge for interventional cardiologists due to a low success rate and high rates of restenosis and adverse cardiovascular events during follow up1,2,3. Currently, there are no consensus or guidelines for interventions in small vessels, and the decision is usually left to the operator. The optimal choice of therapeutic modality for very small (reference vessel diameter, RVD: 2.0–2.25 mm) vessels is even less certain4,5.
Although ultrathin-strut drug-eluting stents (DESs) have been shown to outperform previous generations of DESs in small vessel PCI, their use in very small vessel is unproven6. Drug-coated balloons (DCBs) are initially used to treat in-stent restenosis7, however they have also been applied in de novo small vessel PCI8,9. DCBs may prevent neo-intimal formation without leaving permanent implant thickness in the vessel segment9, and thus they may be ideal for very small vessels. A recent study demonstrated that DCBs were noninferior to DESs with regards to 9-month in-segment restenosis for vessels ranging from 2.25–2.75 mm in diameter5, however very few studies have directly compared DCBs and DESs in very small vessel disease. Therefore, in this study, we performed a retrospective analysis on the safety and efficacy of DCBs versus DESs in very small vessel PCI.
Methods
Patients and target vessels
In this retrospective cohort study, we reviewed all patients receiving PCI from January 2018 to March 2021 at National Taiwan University Hospital. The inclusion criteria included (1) patients received PCI involving at least one de novo very small vessel lesion, defined as an RVD 2.0–2.25 mm, treated with either a DCB or DES; (2) the very small vessel was measured using quantitative coronary angiography (QCA), intravascular ultrasound (IVUS), or optical coherence tomography (OCT) during the index procedure. The decision on whether to use a DCB or DES was made by the operator and the adjunctive pre-treatment with semi-compliant, noncompliant, or scoring/cutting balloon angioplasties were allowed.
Clinical information was reviewed through electronic medical records from the National Taiwan University Hospital database, including baseline demographics, past medical history, complete blood counts, biochemistry studies, and medications after the index procedure. Coronary angiograms, procedural details, procedural results and complications were carefully collected and reviewed by independent interventionists. This retrospective study was approved by the Institutional Review Board of National Taiwan University Hospital, and this study was performed in accordance with relevant guidelines and regulations. The need of informed consent has been waived by the Institutional Review Board of National Taiwan University Hospital (202008020RINC).
Study devices
The available DCBs at our institution with nominal diameters of 2.0 mm and 2.25 mm for very small vessel lesions were SeQuent Please, SeQuent Please Neo (B. Braun, Berlin, Germany), and Agent (Boston Scientific, Wurselen, Germany). The available DESs with stent diameters of 2.0 mm and 2.25 mm for very small vessel lesions were sirolimus-eluting Orsiro (Biotronik, Buloch, Switzerland), everolimus-eluting Synergy (Boston Scientific, Galway, Ireland), Xience Alpine (Abbott Vascular, Tipperary, Ireland), and zotarolimus-eluting Resolute Onyx (Medtronic, Galway, Ireland). The choice of device was left to the operator or according to the patient’s preference.
Image analysis
All baseline coronary angiograms, IVUS, and OCT images were taken as routine with the application of intra-coronary nitroglycerin. The severity of stenosis and reference diameter were measured by QCA (Pie Medical Imaging, Maastricht, Netherlands), IVUS (Volcano Corporation, Alajuela, Costa Rica) or OCT (Abbott Medical, Westford, Massachusetts, United States) to determine the interventional strategy and device size. All of the procedural imaging results were carefully reviewed by two independent interventionalists not involved with the procedure.
Outcome measures
The post-PCI follow-up clinical and laboratory data were reviewed using the institutional electronic medical record system. Angiographic, procedural, and clinical outcomes were coded according to the American College of Cardiology/American Heart Association (ACC/AHA) recommendations10. Major adverse cardiac and cerebrovascular events (MACCE) were defined as the composite of ischemia-driven target lesion revascularization (TLR), all-cause death, non-fatal acute coronary syndrome (ACS), stroke, or heart failure requiring hospitalization within 1 year after PCI. Ischemia-driven TLR was defined as any repeated PCI of the target lesion or bypass surgery of the target vessel, performed for restenosis or other target lesion-related complications for chest pain or a positive test for ischemia (exercise stress test, 24-h Holter monitoring, resting electrocardiographic evidence of ST-segment depression or elevation in > 1 lead, or radionuclide study showing a reversible defect).
Statistical analysis
All data were first tested for normality using the Kolmogorov–Smirnov test. Data with normal distribution were expressed as mean ± standard deviation, and categorical data were expressed as number and percentage. Differences between proportions were calculated using the chi-square test or Fisher’s exact test. Comparisons of data between two groups were performed using the independent T test. Kaplan–Meier survival curves were plotted, and the log-rank test was used for clinical outcome analysis. Patients who were lost to follow-up and those who did not complete 1-year of follow-up were censored in the model.
Because there were substantial differences in the lesion characteristics between the DCB and DES groups, we conducted propensity score matching to balance the distribution of these lesion characteristics between the two groups. The propensity score was estimated using a multiple logistic regression model including the following possible confounding variables including lesion length, diameter, lesion severity (type B2/C) and CTO lesion. Each DCB subject was matched to a maximum of two DES patients. After propensity score matching, there were 35 DCB patients matched 35 DES patients and 12 DCB patients matched 24 DES patients. The balance of covariates between the matched groups was subsequently examined.
Kaplan–Meier survival curves were plotted, and the log‐rank test was used for comparisons of the 1-year outcomes. The Fisher’s exact test was used for comparisons of the 30-day outcomes. Univariable associations between clinical characteristics and MACCEs were assessed using univariable Cox regression. In addition, stepwise backward Cox regression analysis, using a P value ≥ 0.10 as the removal criterion, was performed for multivariable analysis. A two-sided P value < 0.05 was defined as statistically significant. Statistical analysis was performed using SPSS version 25 for Windows (SPSS Inc., IL, USA) with the R-3.3 plugin extension for the propensity score analysis (the ‘Matchit’ package).
Results
Patient characteristics
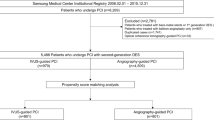
Between January 2018 and March 2021, a total of 5212 PCI procedures were performed at National Taiwan University Hospital. Among these, a total of 216 de novo very small vessel lesions in 205 patients were treated with either a DCB or DES (device diameter ≤ 2.25 mm) and were included in the analysis. The patients were stratified into DCB and DES groups according to the final coronary devices used. Fifty-five patients (58 lesions) received a DCB, and 150 patients (158 lesions) received a DES. The baseline characteristics were similar between the DCB and DES groups. Blood biochemistry, ultrasonographic left ventricular ejection fraction, and the number and location of diseased vessel were also similar. There was no significant difference in post-PCI medications, except for a lower percentage of uninterrupted dual antiplatelet therapy (DAPT) > 3 months in the DCB group. After propensity score matching, there were 47 patients received a DCB matched to 59 patients received a DES. The baseline characteristics remained to be well balanced between DCB and DES group except for the lower percentage of uninterrupted dual antiplatelet therapy (DAPT) > 3 months in the DCB group (Table 1).
Lesion characteristics
Most target lesions were in the left anterior descending artery in both groups. Significantly more ACC/AHA type B2/C lesions (58.2% vs. 36.2%, P = 0.004) and chronic total occlusion lesions (25.9% vs. 12.1%, P = 0.024) were found in the DES group compared to the DCB group. The stenotic lesion diameter was comparable between the two groups (86.6 ± 10.0% in the DCB group vs. 87.9 ± 10.8% in the DES group, P = 0.396). The reference lesion diameter was significantly smaller in the DCB group (2.0 ± 0.1 mm vs. 2.2 ± 0.1 mm in the DES group, P < 0.001). The lesion lengths were comparable between the two groups (20.2 ± 5.1 mm in the DCB group vs. 21.7 ± 5.7 mm in the DES group, P = 0.060). More 2.0 mm devices were used in the DCB group (81.0% vs. 25.3% in the DES group, P < 0.001). Although, the device length was comparable, the proportion of device length > 30 mm was significantly higher in the DES group (25.9% vs. 10.3% in the DCB group, P = 0.014). The use of rotational atherectomy was comparable in both groups, while adjunctive scoring/cutting balloons were used more frequently in the DCB group (22.4% vs. 1.3% in the DES group, P < 0.001). IVUS or OCT was used in 27.6% of the DCB group and 34.2% of the DES group (P = 0.359). There were 66.5% lesions received balloon post-dilatation after DES deployment and mean post-dilatation balloon diameter was 2.26 ± 0.17 mm. The DCB group had significantly higher lesion residual stenosis after PCI (13.5 ± 14.7% vs 0 ± 0% in DES group, P < 0.001).
After propensity score matching, there were 50 lesions in DCB matched to 61 lesions in DES group (3 patients in the DCB group received 2 DCB PCI in separate lesions and 2 patients in the DES group received 2 DES PCI in separate lesions). The lesion characteristics remained well balanced between DCB and DES groups except for the higher percentage of scoring or cutting balloon in the DCB group and the significantly higher residual stenosis in DCB group (Table 2).
Procedural outcomes
The technical success rate was 100%, and no device failure was observed. One wire-induced distal coronary perforation, one vascular access complication, one periprocedural myocardial infarction, and one in-hospital subacute stent thrombosis occurred in the DES group, compared to only one periprocedural myocardial infarction in the DCB group. There were no cases of periprocedural stroke, emergent coronary artery bypass grafting (CABG), or mortality in either group. The overall procedure-related complication rates were thus comparable (2.5% in the DES group and 1.7% in the DCB group, P = 1.000). The results were consistent after propensity score matching (Table 2).
30-day and 1-year clinical outcomes
The incidences of MACCEs at 30 days were 3.6% in the DCB group and 2.0% in the DES group (P = 0.612). There was no ischemia-driven TLR or stroke in both groups. The incidence of all-cause death or heart failure-related admission was also comparable between the two groups. The results were consistent after propensity score matching (Table 3).
The cumulative incidence of ischemia-driven TLR at 1 year was 7.2% in the DCB group and 4.9% in the DES group (P = 0.530). There was no vessel thrombosis in the DCB group, and no additional stent thrombosis in the DES group. The cumulative incidence of MACCEs was 10.6% in the DCB group and 12.7% in the DES group (P = 0.769). The cumulative incidence of all-cause death, non-fatal ACS, stroke or heart failure-related admission was also comparable between the two groups. The results were consistent after propensity score matching (Table 4 and Fig. 1).
Univariable and stepwise backward multivariable Cox regression analyses for the predictors of MACCEs at 1 year were performed. Female gender (HR 3.18 [95% CI: 1.32–7.63]; P = 0.010, ACS at presentation (HR 2.71 [95% CI: 1.20–6.11]; P = 0.016), and DAPT duration < 3 months (HR 5.90 [95% CI: 2.45–14.24]; P < 0.001) were identified as being significant predictors for MACCEs at 1 year after very small vessel PCI (Table 5).
Subgroup analysis of ACS at presentation or not
The subgroup analysis of ACS or non-ACS at presentation of the 30-day and 1-year clinical outcomes is shown in Table 6. The short-term and long-term clinical outcomes were comparable in patients with ACS or non-ACS at presentation.
Discussion
Main findings and previous studies
In the present real-world retrospective cohort, we clearly demonstrated comparable procedural and 1-year outcomes for very small vessel PCI between the DCB and DES groups. PCI for very small vessels (reference diameter 2.0–2.25 mm) is not uncommon in daily practice and remains a challenge5,6. These lesions are usually seen in patients with diabetes mellitus, female gender, older age, multi-vessel disease, peripheral vascular disease, and history of myocardial infarction or CABG11,12,13. Moreover, they are often long and diffuse, categorized as unfavorable AHA/ACC type C lesions2. Revascularization by CABG or PCI for very small vessel disease has been shown to be of limited clinical benefit due to anastomotic difficulty, poor distal run-off, and incomplete revascularization14,15. Diffuse small vessel disease is known to be related to incomplete revascularization in CABG15, and restenosis, incomplete revascularization, and worse outcomes in PCI1,2,3,4.
The higher rate of restenosis in small vessel PCI is partly explained by the inevitable neointimal hyperplasia and exaggerated relative loss in an already small vessel lumen16. DESs provide an antiproliferative effect, but the thick struts in older generation designs can lead to permanent luminal loss despite proper apposition. The evolution of stent technology may improve the results of small vessel PCI. A recent trial showed that a reduction in stent strut thickness resulted in lower TLR rates at 3 years6. A more fundamental approach may be achieved using DCBs with the concept of “leaving nothing behind”17, by the homogenous delivery of antiproliferative drugs to the vessel wall and avoiding permanent metallic implantation. Several prior studies have shown promising outcomes of DCBs with comparable results to those of DESs in vessels ranging from 2.75 to 3.0 mm18,19,20.
The results of DCBs should, in theory, be more favorable in smaller vessels. Previous retrospective studies have demonstrated comparable 1-year results between DCBs and DESs in vessels ranging from 2 to 2.5 mm5,21,22. Moreover, no vessel thrombosis occurred with DCBs. The Taiwanese National Health Insurance program only reimburses for 1 month of DAPT after DCB but 6 months after DES, and therefore the proportion of patients with > 3 months DAPT was significantly lower in the DCB group in our study. Even with this limitation, there was no vessel thrombosis in the DCB group, but one (0.6%) case of subacute stent thrombosis in the DES group. Future large-scale randomized controlled trials are needed to investigate the effect of a shorted DAPT duration.
Intravascular imaging is important in very small vessel PCI, where precise visualization of plaque morphology and vessel diameter, confirmation of adequate stent apposition and/or expansion, and checking for residual thrombus or dissection all contribute to the final outcomes. Compared with intravascular imaging, the QCA or visual estimation frequently underestimates the lesion diameter23. However, anatomical restrictions including a small vessel caliber relative to the device profile, distal location of the target, and difficulty in imaging device delivery are major drawbacks. In our cohort, 27.6% of the DCB group received intravascular imaging compared to 34.2% in the DES group. With advances in imaging device technology, the results of very small vessel PCI may be further improved.
The use of fractional flow reserve (FFR) may also be beneficial in PCI with a DCB-only strategy. After optimal lesion preparation, an acceptable angiography result consisting of no flow-limiting dissection, ≤ 30% residual stenosis, fully dilated lesion, thrombolysis in myocardial infarction (TIMI) flow grade 3, and an FFR > 0.8 will determine good outcomes9. In current study, the residual stenosis in the DCB group was low, about 13.5%, which might contribute the good clinical outcomes. In the present retrospective analysis, we could not provide information on the use of FFR. The applicability of FFR and its value in very small vessel PCI, especially when a DCB-only strategy is considered, warrants future research.
In our study, female gender, ACS at presentation and DAPT < 3 months were independent unfavorable predictors for MACCEs at 1 year. The use of a DCB or DES was not related to the 1-year outcome of very small vessel PCI. In addition, lesion characteristics, device size, and lesion complexity were also not related to clinical outcomes. Previous studies have demonstrated that, compared with men, women are at a higher risk of adverse clinical outcomes following PCI24. However, no previous study has clearly identified the risk of female gender in predicting very small vessel interventions. In the current study, we showed that female gender was an independent predictor of cardiovascular outcomes after very small vessel PCI. In current study, ACS at presentation was the significant predictor of worse MACCEs at 1 year. It has been well established that the ACS lesions were different to non-ACS lesions, and might lead to worse clinical outcomes25,26. Interestingly, the subgroup analysis of the ACS and non-ACS patients in this study still demonstrated the similar clinical outcomes in both groups but the case and event numbers were small. Further study is needed to support the DCB use in very small vessel PCI in ACS patients.
Limitations
There are several limitations to this study. First, this was a small retrospective cohort study conducted at one tertiary center. Second, multiple DES and DCB designs were included, which may have confounded the analysis. Third, the lesion characteristics and device profiles were unbalanced between the two groups. The available sizes and recommended deployment techniques of DCBs and DESs may significantly have affected the operators’ choice in different lesion subsets. Further larger multicenter prospective randomized studies are needed.
Conclusion
In the present study, we found similar clinical outcomes between DCBs and DESs in de novo very small vessel PCI. Female gender, ACS at presentation and short DAPT < 3 months were predictors of worse outcomes. With careful lesion selection and preparation, DCBs might be the alternative in very small vessel intervention.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ACS:
-
Acute coronary syndrome
- ACC/AHA:
-
American College of Cardiology/American Heart Association
- CABG:
-
Coronary artery bypass graft
- DAPT:
-
Dual antiplatelet therapy
- DCB:
-
Drug-coated balloon
- DES:
-
Drug-eluting stent
- FFR:
-
Fractional flow reserve
- IVUS:
-
Intravascular ultrasound
- MACCE:
-
Major adverse cardiac and cerebrovascular event
- OCT:
-
Optical coherence tomography
- PCI:
-
Percutaneous coronary intervention
- PSM:
-
Propensity score matching
- RVD:
-
Reference vessel diameter
- TLR:
-
Target lesion revascularization
- TIMI:
-
Thrombolysis In Myocardial Infarction
References
Akiyama, T. et al. Angiographic and clinical outcome following coronary stenting of small vessels: A comparison with coronary stenting of large vessels. J. Am. Coll. Cardiol. 32, 1610–1618 (1998).
Schunkert, H., Harrell, L. & Palacios, I. F. Implications of small reference vessel diameter in patients undergoing percutaneous coronary revascularization. J. Am. Coll. Cardiol. 34, 40–48 (1999).
Claessen, B. E. et al. Impact of lesion length and vessel size on clinical outcomes after percutaneous coronary intervention with everolimus- versus paclitaxel-eluting stents pooled analysis from the SPIRIT (Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System) and COMPARE (Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice) Randomized Trials. JACC Cardiovasc. Interv. 4, 1209–1215. https://doi.org/10.1016/j.jcin.2011.07.016 (2011).
van der Heijden, L. C. et al. Small-vessel treatment with contemporary newer-generation drug-eluting coronary stents in all-comers: Insights from 2-year DUTCH PEERS (TWENTE II) randomized trial. Am. Heart J. 176, 28–35. https://doi.org/10.1016/j.ahj.2016.02.020 (2016).
Tang, Y. et al. Drug-coated balloon versus drug-eluting stent for small-vessel disease: The RESTORE SVD china randomized trial. JACC Cardiovasc. Interv. 11, 2381–2392. https://doi.org/10.1016/j.jcin.2018.09.009 (2018).
Buiten, R. A. et al. Outcomes in patients treated with thin-strut, very thin-strut, or ultrathin-strut drug-eluting stents in small coronary vessels: A prespecified analysis of the randomized BIO-RESORT trial. JAMA Cardiol. 4, 659–669. https://doi.org/10.1001/jamacardio.2019.1776 (2019).
Neumann, F. J. et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 40, 87–165. https://doi.org/10.1093/eurheartj/ehy394 (2019).
Megaly, M. et al. Outcomes with drug-coated balloons in small-vessel coronary artery disease. Catheter Cardiovasc. Interv. 93, E277–E286. https://doi.org/10.1002/ccd.27996 (2019).
Jeger, R. V. et al. Drug-coated balloons for coronary artery disease: Third report of the international DCB consensus group. JACC Cardiovasc. Interv. 13, 1391–1402. https://doi.org/10.1016/j.jcin.2020.02.043 (2020).
Levine, G. N. et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J. Am. Coll. Cardiol. 58, e44–e122. https://doi.org/10.1016/j.jacc.2011.08.007 (2011).
Patel, H. et al. Microvascular disease and small-vessel disease: The nexus of multiple diseases of women. J. Womens Health (Larchmt) 29, 770–779. https://doi.org/10.1089/jwh.2019.7826 (2020).
Kip, K. E. et al. Coronary angioplasty in diabetic patients. The National Heart, Lung, and Blood Institute Percutaneous Transluminal Coronary Angioplasty Registry. Circulation 94, 1818–1825. https://doi.org/10.1161/01.cir.94.8.1818 (1996).
Ertan, C. et al. Association of prediabetes with diffuse coronary narrowing and small-vessel disease. J. Cardiol. 63, 29–34. https://doi.org/10.1016/j.jjcc.2013.06.015 (2014).
O’Connor, N. J., Morton, J. R., Birkmeyer, J. D., Olmstead, E. M. & O’Connor, G. T. Effect of coronary artery diameter in patients undergoing coronary bypass surgery. Northern New England Cardiovascular Disease Study Group. Circulation 93, 652–655. https://doi.org/10.1161/01.cir.93.4.652 (1996).
Head, S. J. et al. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: A subgroup analysis of 3-year SYNTAX data. Eur. J. Cardiothorac. Surg. 41, 535–541. https://doi.org/10.1093/ejcts/ezr105 (2012).
Rathore, S. Small coronary vessel angioplasty: Outcomes and technical considerations. Vasc. Health Risk Manag. 6, 915–922. https://doi.org/10.2147/VHRM.S8161 (2010).
Serra, A. Value of drug-coated balloons in small-vessel disease: Have they come of age?. JACC Cardiovasc. Interv. 11, 2393–2395. https://doi.org/10.1016/j.jcin.2018.10.018 (2018).
Latib, A. et al. A randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels: The BELLO (Balloon Elution and Late Loss Optimization) study. J. Am. Coll. Cardiol. 60, 2473–2480. https://doi.org/10.1016/j.jacc.2012.09.020 (2012).
Latib, A. et al. 3-Year follow-up of the balloon elution and late loss optimization study (BELLO). JACC Cardiovasc. Interv. 8, 1132–1134. https://doi.org/10.1016/j.jcin.2015.04.008 (2015).
Jeger, R. V. et al. Drug-coated balloons for small coronary artery disease (BASKET-SMALL 2): An open-label randomised non-inferiority trial. Lancet 392, 849–856. https://doi.org/10.1016/S0140-6736(18)31719-7 (2018).
Sinaga, D. A. et al. Drug-coated balloons: A safe and effective alternative to drug-eluting stents in small vessel coronary artery disease. J. Interv. Cardiol. 29, 454–460. https://doi.org/10.1111/joic.12333 (2016).
Sim, H. W. et al. Treatment of very small de novo coronary artery disease with 2.0 mm drug-coated balloons showed 1-year clinical outcome comparable with 2.0 mm drug-eluting stents. J. Invasive Cardiol. 30, 256–261 (2018).
Kubo, T. et al. OCT compared with IVUS in a coronary lesion assessment: The OPUS-CLASS study. JACC Cardiovasc. Imaging 6, 1095–1104. https://doi.org/10.1016/j.jcmg.2013.04.014 (2013).
Naito, R. et al. Gender difference in long-term clinical outcomes following percutaneous coronary intervention during 1984–2008. Atherosclerosis 247, 105–110. https://doi.org/10.1016/j.atherosclerosis.2015.10.088 (2016).
van Velzen, J. E. et al. Comparison of the relation between the calcium score and plaque characteristics in patients with acute coronary syndrome versus patients with stable coronary artery disease, assessed by computed tomography angiography and virtual histology intravascular ultrasound. Am. J. Cardiol. 108, 658–664. https://doi.org/10.1016/j.amjcard.2011.04.009 (2011).
Shimamura, K. et al. Difference of ruptured plaque morphology between asymptomatic coronary artery disease and non-ST elevation acute coronary syndrome patients: An optical coherence tomography study. Atherosclerosis 235, 532–537. https://doi.org/10.1016/j.atherosclerosis.2014.05.920 (2014).
Acknowledgements
We thank the staff of the Eighth Core Lab, Department of Medical Research, National Taiwan University Hospital for technical support during the study. We also acknowledge the Taiwan Health Foundation, Dr. T Y Lin's Medical Research Foundation and the Yuanta Cultural and Educational Foundation for their support.
Funding
This article was subsidized for English editing by National Taiwan University under the Excellence Improvement Program for Doctoral Students (grant number 108-2926-I-002-002-MY4), sponsored by Ministry of Science and Technology, Taiwan.
Author information
Authors and Affiliations
Contributions
H.L.K., Y.H.C. and C.H.T. conceived and designed the study. H.L.K. and Y.H.C. executed the study. C.H.T., C.F.Y., S.W.M., C.K.C. and K.P.H. collected and analyzed the data. C.H.T., C.F.Y., Y.H.C. and H.L.K. wrote the paper. M.S.L., C.C.H. and C.S.H. made scientific comments on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsai, CH., Yeh, CF., Meng, SW. et al. Comparison between drug-coated balloons and drug-eluting stents in very small coronary artery interventions. Sci Rep 12, 10679 (2022). https://doi.org/10.1038/s41598-022-14047-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-14047-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.