Abstract
Neonatal bloodstream infections (BSI) can lead to sepsis, with high morbidity and mortality, particularly in low-income settings. The high prevalence of third-generation cephalosporin-resistant organisms (3GC-RO) complicates the management of BSI. Whether BSI is linked to carriage of 3GC-RO, or to acquisition from the hospital environment is important for infection prevention and control, but the relationship remains unclear, especially in low-income settings. At a tertiary hospital in Mwanza, Tanzania, we screened neonatal blood and rectal samples from 200 neonates, and 400 (hospital) environmental samples. We used logistic regression to identify risk factors, and Kolmogorov–Smirnov tests and randomisation analyses to compare distributions of species and resistance patterns to assess potential routes of transmission. We found that BSIs caused by 3GC-RO were frequent (of 59 cases of BSI, 55 were caused by 3GC-RO), as was carriage of 3GC-RO, particularly Escherichia coli, Klebsiella pneumoniae, and Acinetobacter species. In the 28 infants with both a carriage and blood isolate, there were more (4 of 28) isolate pairs of the same species and susceptibility profile than expected by chance (p < 0.05), but most pairs were discordant (24 of 28). Logistic regression models found no association between BSI and carriage with either 3GC-RO or only 3GC-R K. pneumoniae. These analyses suggest that carriage of 3GC-RO is not a major driver of BSI caused by 3GC-RO in this setting. Comparison with environmental isolates showed very similar distributions of species and resistance patterns in the carriage, BSI, and the environment. These similar distributions, a high frequency of Acinetobacter spp. isolations, the lack of strong association between carriage and BSI, together with the high proportion of 3GC-RO in BSI all suggest that these neonates acquire multidrug-resistant carriage and blood isolates directly from the hospital environment.
Similar content being viewed by others
Introduction
Neonatal infections, such as blood stream infections (BSI) are known to account for a significant proportion of deaths occurring in the first 28 days of life1. Premature neonates and those with low birthweight are most vulnerable to BSI, and consequently sepsis, due to inadequate immune barriers and responses2. The most common bacteria causing BSI in low- or middle-income countries (LMICs) are different to those in high-income countries (HIC)3. In HICs, the most isolated species are Group B Streptococcus, Escherichia coli, and coagulase negative staphylococci3,4, while S. aureus, E. coli, Klebsiella pneumoniae, and Acinetobacter spp., are the most common causes of neonatal sepsis in LMICs2,3,5,6.
The diagnosis of neonatal sepsis is often delayed due to its subtle and non-specific initial signs7. Risk factors include prematurity, low birthweight, premature rupture of membranes, and maternal infections at the time of delivery8. Early-onset neonatal sepsis, typically defined as presenting within 72 h of birth, is often associated with organisms from the maternal flora, known as vertical transmission7,9. In contrast, late onset neonatal sepsis (> 72 h) is thought to be caused by pathogens acquired from elsewhere, usually the hospital environment7,10. However, this view is shifting, as difficult or unhygienic births may result in neonatal infections resulting from environmental, rather than maternal, pathogens acquired < 72 h6.
Since neonatal BSI is a life-threatening condition that can rapidly progress to septic shock, physicians prescribe empirical treatment before microbiology results are available. The World Health Organization’s (WHO) guidelines recommend intravenous ampicillin and gentamicin as prophylaxis in neonates with documented risk factors (such as maternal fever (> 38 °C) before or during delivery) for at least two days, and continuing for at least ten days in cases of suspected sepsis11. However, these guidelines were developed with no comprehensive surveillance data from neonatal units in LMIC settings12.
Antimicrobial resistance (AMR) jeopardises the effective treatment of neonatal BSI by Gram-negative organisms. The emergence and spread of extended-spectrum β-lactamases (ESBLs) pose an urgent public health risk13, as they confer resistance to third-generation cephalosporins and monobactams, while the plasmids encoding ESBLs often carry additional genes that confer resistance to aminoglycosides, tetracycline, and fluoroquinolones14,15. The WHO classifies ESBL-producing Enterobacteriaceae as critical priority I pathogens, requiring urgent research and development of new therapies16.
Third-generation cephalosporin-resistant organisms (3GC-RO) are highly prevalent in East Africa17,18,19,20. Gentamicin resistance is also a well-recognised issue here21, and has been reported to be as high as 84% in septic neonates22, with significantly more frequent resistance in 3GC-RO18.
Therefore, there is an urgent need to map the sources and transmission pathways of 3GC-RO in healthcare settings. K. pneumoniae has been shown to colonise the gastrointestinal tract of preterm infants and their immediate hospital environment, with frequent exchange between the two sources23. Whilst previous studies have shown an association between colonisation and BSI24, there is little data available for LMIC settings, and the extent to which the hospital environment versus intestinal colonisation is the source for blood stream infections with 3GC-RO remains unclear. Improved understanding of these sources and pathways would help direct infection prevention and control (IPC) measures.
The aims of this study were to quantify the burden of 3GC-RO in neonates; to identify risk factors associated with both 3GC-RO rectal carriage and BSI; and to identify potential transmission pathways by comparing the distributions of organisms and their multi-drug resistance patterns between the neonates and their environment and examining the concordance between carriage and blood isolates.
Methods
Study setting and population
Bugando Medical Center (BMC) is a 950-bed tertiary hospital in Mwanza, Tanzania. At the time of the study, there were 60 cots in the neonatal wards, of which 15 were on the neonatal intensive care unit (NICU). There were four functional hand washing sinks in total (two of these were in the NICU). Alcohol rubs were frequently used by paediatricians and infrequently by nurses. At any given time, there were four paediatricians and seven neonatal nurses on shift, of whom four worked in the NICU.
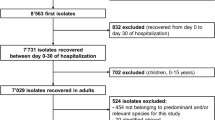
Patient and microbiology data were obtained from a previously described study25. In brief, isolates and data were collected over a four-month period. We enrolled a total of 200 neonates (under 28 days of age) born at or admitted to BMC between January and April 2019. Neonates with signs and symptoms of infections (as defined by The WHO Young Infants Study Group26) and their mothers/guardians were recruited serially until the sample size was reached. Variables collected were as previously described25. Informed parental consent was sought for participation, and a questionnaire was completed, including questions on maternal health, for example antibiotic use and fever during pregnancy or labour. Information on neonatal health, including antibiotic treatment, was obtained from the patients’ medical records. Data were stripped of all personal identifiable information prior to analyses, and all methods were carried out in accordance with the relevant guidelines and regulations set by the Declaration of Helsinki.
Sample collection and culture
A blood sample and a rectal swab were obtained from all neonates (n = 200) at the time of enrolment. This was as soon as possible after birth or admission (usually within hours). A total of 143 neonates were enrolled < 48 h of birth. The median duration of stay before sampling was 1 (IQR 1–2) days. At the time of rectal sampling, maternal hands and neonatal cots were also swabbed—these were considered to represent organisms in the hospital environment. Blood samples were cultured for all bacterial growth, while only 3GC-RO were cultured for from rectal and environmental swabs using cefotaxime-supplemented MacConkey agar. Laboratory procedures, including bacterial culture and identification, were previously described25. For blood stream samples, any bacterial growth indicated BSI; we excluded non-3GC-R isolates from further analysis.
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing (AST) of isolates was carried out by disc diffusion method using the antibiotics listed in Table 1 following the Clinical and Laboratory Standard Institute guidelines (2018 version,27). As rectal and environmental swabs were selectively grown on cefotaxime-supplemented MacConkey agar, only blood isolates were tested for cefotaxime resistance.
Data analysis
Neonatal information obtained from the questionnaires, patient records and microbiological tests were anonymised, aggregated, and analysed using R version 3.5.3 (2019-03-11).
Comparison of species distributions and resistance patterns
Distributions of species abundance were compared using a bootstrap Kolmogorov–Smirnov (KS) test. The KS test statistic was the maximum absolute difference in the cumulative distributions of the species distributions being compared. A total of 10,000 test samples, each with the same number of observations as the test distribution, were computed along with the test statistic to generate the expected distribution of the test statistic. In addition, frequencies of resistance between isolate sources were compared for the most common species isolated. The proportion of isolates resistant to a given antibiotic was compared between isolate sources using prop.test() in R. When multiple comparisons were made, the Bonferroni correction was applied.
Randomisation analysis of organisms and resistance patterns
Random resampling of the observed blood and carriage isolates was used to assess whether the observed number of matches in a neonate by organisms and resistance patterns across BSI and rectal carriage isolates were greater than expected by chance. For this, 28 (the number of neonates that had an organism isolated both from their blood and a 3GC-RO isolate from their rectal swab) organisms were randomly sampled from the set of neonatal blood isolates and 28 from the set of carriage isolates and the number of concordant pairs counted. This was done 100,000 times to obtain a distribution of the expected number of concordant pairs under a null hypothesis of no relationship between carriage and blood isolates. To assess robustness, the process of random re-sampling was repeated restricting the rectal organisms to only those found in cases of BSI.
Risk factor analyses for infection and carriage
We used two sets of logistic regression models to investigate risk factors associated with (1) neonatal carriage of 3GC-RO and (2) bloodstream infections. The outcome variables were infection/carriage with any 3GC-RO or just 3GC-R K. pneumoniae, the most prevalent 3GC-RO in carriage and blood. We included covariates that have been previously associated with infection and carriage or if a suspected biological link with the outcome existed (Table 2). Stepwise backwards model selection was then performed to identify the model with the lowest Akaike Information Criterion (AIC). Maternal antibiotic use and fever during pregnancy were found to be strongly associated (χ2 = 49.2, p < 0.001), and so the models were run including one or the other, to find the model with the lowest AIC. Residuals were assessed using standardised residuals generated using the DHARMA package28 in R and assessed for normality and dispersion.
Ethics approval and consent to participate
Protocols and procedures in this study were approved by Code of Conduct for Research Ethics of the Sokoine University of Agriculture with certificate number: SUA/CVMBS/R.1/2018/8 and ethically cleared by the joint CUHAS/ BMC Research Ethics and Review Committee (CREC) with certificate number: CREC/298/2018. All participants signed an informed consent before enrolment, except for participants aged < 18 years, where informed consent of participation was provided by their parents/guardians. Detailed microbiological reports of clinical specimens were shared in a timely manner with attending doctors in respective units for proper neonates’ management.
Results
Distributions of organisms by source
There were 59 Gram-negative organisms isolated from blood (from 59 neonates), and 108 from rectal swabs (from 86 neonates). There were 22 neonates who had two different 3GC-R organisms isolated from their rectal swab. There were 101 environmental 3GC-RO isolates: 37 from maternal hands and 64 from cots. 3GC-R K. pneumoniae was most prevalent in blood samples (n = 28), rectal swabs (n = 49), and maternal hand swabs (n = 16), and second most prevalent in cot swabs (n = 18). Acinetobacter spp. was most common in cot swabs (n = 35), and second most common in all other types of samples and swabs (Fig. 1A and B). Pairwise Kolmogorov–Smirnov tests showed no significant difference between the distributions of organisms by source (blood samples, rectal swabs, neonatal cot, maternal hands; Table 3).
Gram-negative bacteria isolated from blood, and rectal, maternal hand and cot swabs, (A) Gram-negative organisms isolated from blood samples and rectal swabs. Dark grey shows 3GC-RO, light grey 3GC-susceptible. (B) Gram-negative organisms isolated from cot (orange) and maternal hand swabs (yellow), all 3GC-R.
Resistance patterns in neonatal infection and carriage isolates
The most prescribed neonatal antibiotics were gentamicin and ampicillin. Resistance to gentamicin was frequent (> 60%) in 3GC-R blood and rectal isolates (Fig. 2A). Resistance to other antibiotics was also frequent, including trimethoprim–sulfamethoxazole (> 90% isolates resistant) and tetracycline (> 50% of isolates resistant). Amikacin resistance was rare (< 1%) in all isolate types. Frequencies of antimicrobial resistances in 3GC-R K. pneumoniae isolates (Fig. S3) were similar in blood, carriage, and environmental isolates apart from tetracycline. Tetracycline resistance was significantly more frequent in carriage compared to blood isolates (p = 0.012).
Frequencies of resistances in Gram-negative bacteria isolated from blood, and rectal, maternal hand and cot swabs. (A) Frequencies of antimicrobial resistances in blood (dark blue) and carriage (light blue), 3GC-RO only. (B) Frequencies of antimicrobial resistances in cot (orange) and maternal hand swabs (yellow), all 3GC-RO. Error bars show 95% confidence intervals. SXT trimethoprim–sulfamethoxazole.
Resistance patterns in 3GC-R organisms in environmental swabs
Multi-drug resistance, commonly defined as resistance to three or more classes of antimicrobials, was frequently detected in 3GC-RO isolated from neonatal cots and maternal hand swabs. Resistance to trimethoprim–sulfamethoxazole and gentamicin were also frequently detected (> 85% of isolates, Fig. 2B). Most isolates were susceptible to amikacin (> 90%).
Association between neonatal carriage and blood isolates
There were 28 neonates from whom both a blood and carriage isolate were obtained. Of the 28, 16 neonates had distinct 3GC-RO species in their rectal swab and blood isolates and 12 had the same 3GC-RO species (Fig. 3A).
A comparison of resistance profiles of 3GC-R Gram-negative organisms isolated from blood and rectal swabs. (A) Twelve neonates had the same organism in their blood and rectum. Dark green indicates a match in resistance/susceptibility between the two isolates, light green represents a mismatch. Four pairs had identical resistance profiles (bold). (B) Breakdown of antibiotic susceptibility profiles of the four organisms with identical resistance patterns isolated from blood and rectum. SXT trimethoprim–sulfamethoxazole, S susceptible, R resistant.
Four of these pairs shared identical resistance profiles against cefotaxime, ciprofloxacin, gentamicin, meropenem, trimethoprim–sulfamethoxazole, tetracycline, and amikacin (Fig. 3B), with most mismatches in antimicrobial resistance patterns seen in Acinetobacter spp. (Fig. 3A). Under the null hypothesis of no association between carriage and blood isolates, the probability of detecting four organisms with matching resistance patterns was < 0.05 (Fig. 4).
Risk factors associated with neonatal BSI and carriage of 3GC-R organisms
BSI due to 3GC-RO
For BSI caused by any 3GC-RO, the model that included maternal fever during pregnancy was found to be a better fit to our data (final model AIC = 224.77), compared with maternal antimicrobial use (final model AIC = 226.79). Similarly, for BSI caused by 3GC-R K. pneumoniae, the model including maternal fever during pregnancy was found to be a better fit to our data (final model AIC = 143.90), compared with maternal antimicrobial use (final model AIC = 144.81).
The final models were similar for BSI caused by any 3GC-RO and BSI caused by 3GC-R K. pneumoniae (Table 4). BSI caused by any 3GC-RO was positively associated with cot 3GC-RO contamination (OR 1.99, 95% CI 1.00–3.94), enrolment (sampling) time > 48 h (OR 2.32, 95% CI 1.14–4.69), and fever during pregnancy (OR 2.08, 95% CI 1.04–4.22). Hospital delivery was negatively associated with both BSI caused by any 3GC-RO (OR 0.30, 95% CI 0.09–1.00). BSI caused by 3GC-R K. pneumoniae positively associated with fever during pregnancy (OR 3.50, 95% CI 1.32–10.7), and negatively associated with hospital deliveries (OR 0.17, 95% CI 0.04–0.76).
Carriage of 3GC-RO
The final models were similar for carriage of any 3GC-RO and 3GC-R K. pneumoniae (Table 4). Cot 3GC-RO colonisation (OR 2.52, 95% CI 1.32–4.89) and female sex (OR 2.25, 95% CI 1.23–4.15) were positively associated with carriage of 3GC-RO, while neonatal antibiotic use was negatively associated (OR 0.29, 95% CI 0.11–0.73) with carriage of 3GC-RO. Female sex was also positively associated (OR 2.21, 95% CI 1.07–4.65) with carriage of 3GC-R K. pneumoniae.
Organisms isolated from neonates born at home versus in hospital
Although place of delivery was a significant risk factor in neonatal BSI, Pairwise Kolmogorov–Smirnov tests showed that there was no significant difference between the distribution of blood isolates or carriage isolates from neonates born at home versus in hospitals (Fig. S2, Table 3).
Discussion
To address the question of the relationship between blood stream infection, colonisation, and the hospital environment, we collected blood, rectal, and environmental (maternal hand and cot) samples from neonates admitted to BMC, a tertiary hospital in Mwanza, Tanzania, and quantified the prevalence and phenotypic resistance patterns of 3GC-R organisms. Non-invasive maternal hand swabs were considered to reflect transient microflora or organisms present in the environment, rather than maternal colonisation. We investigated risk factors associated with neonatal colonisation with and infection caused by 3GC-RO.
The most common bacteria causing BSI in LMICs are thought to be different from those in high-income countries3. In this study, K. pneumoniae and Acinetobacter spp. were the most prevalent 3GC-R organisms in blood and carriage isolates. Around a quarter of environmental samples were also positive for 3GC-RO, with 3GC-R Acinetobacter spp. and K. pneumoniae being the most frequently isolated organisms. This is not uncommon as Acinetobacter spp. has been often isolated from skin of healthy individuals29. We found no difference between the distribution of organisms across sampling sites. Studies have shown that S. aureus, E. coli, K. pneumoniae, and Acinetobacter spp. are the most common causes of sepsis in LMICs2,3 and our study confirms the predominance of K. pneumoniae, Acinetobacter spp., and E. coli in neonatal BSI, with the majority being 3GC-R. These results were also consistent with previous studies set in Tanzania30,31. Gram-negative organisms in the blood samples were significantly (p < 0.001) more prevalent than Gram-positive bacteria (59/69 vs 10/69).
Most neonates enrolled in this study were premature and/or had low birthweight (Fig. S1), putting them at high risk of BSI. Previous studies have linked a number of risk factors to neonatal BSIs, including fever during pregnancy or labour32,33, prematurity, male sex, prolonged rupture of membranes34, and colonisation of babies with microorganisms such as K. pneumoniae35. Here, fever in pregnancy and home deliveries were associated with an increased risk of BSI with any 3GC-R organism and with just 3GC-R K. pneumoniae. Delivery at home was also associated with higher neonatal mortality in a study set in Ethiopia36. However, this finding could reflect the health status of infants being admitted rather than the difference between home and hospital deliveries per se. Sampling neonates > 48 h after admission was also associated with increased risk of BSI caused by any 3GC-RO.
The risk of gastrointestinal carriage of 3GC-RO was positively associated with female sex and cot 3GC-RO colonisation, and negatively associated with neonatal antibiotic use. Carriage of such organisms has been reported to cause subsequent BSI24,35,37,38 but was not found to be a risk factor in this study.
There were four neonates with the same organism and resistance pattern in their blood and carriage isolates, which is more than expected by chance alone (p < 0.05). However, the more frequent occurrence of discordant resistant organism pairs in blood and carriage isolates suggests that carriage and BSI may be acquired independently. The potential link between rectal carriage and BSI could be further examined using whole genome sequence analysis, which provides a greater degree of discrimination between isolates. This could increase the number of discordant pairs and add support to the conclusion that colonisation is not the major source of BSI in this setting.
The current guidelines recommending the use of ampicillin and gentamicin in suspected neonatal sepsis are primarily based on clinical trials conducted in high-income settings3 where Gram-positive bacteria are the primary cause of neonatal BSI. In contrast, Fuchs et al. (2016) report that approximately 70% of pathogens isolated from paediatric sepsis in Tanzania are Gram-negative species, with K. pneumoniae (naturally ampicillin-resistant) and E. coli being the most prevalent. In addition, the common occurrence of 3GC-RO with co-resistance to gentamicin in the present and previous studies14,15 indicates that empirical treatment with ampicillin and gentamicin may not always be appropriate in these settings and may need to be altered after AST profiles become available for the isolates. In our setting, > 60% of 3GC-R organisms isolated from blood and rectal swabs and > 85% from cot and hand swabs were gentamicin resistant. The majority of 3GC-R K. pneumoniae isolated from blood samples were gentamicin resistant, as well as 58% of Acinetobacter spp. and 40% of E. coli. Among the most frequently isolated 3GC-RO in rectal swabs, Acinetobacter spp. was most frequently resistant to gentamicin, followed by K. pneumoniae and E. coli.
As previously reported, over 25% of neonates in this study had 3GC-RO in their blood19 and most blood isolates were 3GC-RO. Other than acquisition from the hospital environment, a possible explanation for the high proportion of 3GC-R organisms in blood is treatment with antibiotics clearing the non-3GC-R organisms.
Our study shows similar distributions of organisms and resistance patterns between isolates obtained from blood, carriage, and the environment, with Acinetobacter spp. frequently identified in all these isolates. Although carriage and blood isolate pairs were mostly discordant, there was more similarity between carriage and blood isolates than expected by chance. These observations support some association between carriage and BSI, which could be strengthened by sampling, AST, and genomic characterisation of multiple carriage isolates. However, frequent discordant pairs of isolates also support the hypothesis that carriage and blood isolates can be acquired independently, and more hospital environmental surveillance is needed in this respect. In addition, the frequent occurrence of Acinetobacter spp. suggests that the hospital environment may be a common source for both the carriage 3GC-R organisms and the blood organisms. Moreover, the high prevalence of 3GC-RO among the blood isolates suggests that the hospital environment may be a reservoir for 3GC-RO. Whilst previous studies have identified an association between colonisation and infection with concordant isolates, there is limited data on this relationship in low-income settings24.
Early-onset neonatal sepsis is generally defined as bacteraemia or bacterial meningitis that presents ≤ 72 h of birth, and is usually associated with organism acquired from the maternal flora7,39. Most neonates were sampled within 48 h of birth in this study, with high proportions of neonatal BSI caused by 3GC-RO. This either reflects the frequent carriage of 3GC-RO in mothers or indicates that these organisms are acquired from the hospital environment immediately after birth. The high frequency of 3GC-R Acinetobacter spp., organisms commonly associated with the hospital environment29, supports the latter. This is also concordant with a recent review by Sands et al.6, who highlight the potential role of environmental pathogens in early-onset neonatal sepsis. Nevertheless, as this study could not pinpoint the time of sepsis onset, the roles of the environment and gastrointestinal colonisation need further characterisation. In addition, we compared isolates from different sources based on phenotypic, rather than genetic data. The latter would be needed to confirm whether the same organisms are found in carriage, infection, and the hospital environment.
This study demonstrates an alarmingly high resistance to the commonly used antibiotics at neonatal wards at BMC, a major tertiary hospital in Tanzania. Given the availability of laboratory infrastructures and capacity at this institution, our findings highlight the need to provide antibiotic therapies guided by local epidemiology including antimicrobial susceptibility testing. Moreover, this study suggests that the major route of acquisition of both carriage and bloodstream isolates may be the hospital environment, rather than BSI arising from carriage organisms, indicating that improved IPC focused on the healthcare setting sources could be beneficial. These findings have implications for IPC and antibiotic treatment, indicating that IPC may need to focus on reducing hospital environmental reservoir; and that susceptibility profiling to inform antibiotic therapy might operate best at a group rather than individual level.
Data availability
The datasets generated for the current study are available by reasonable request to the corresponding author.
Abbreviations
- 3GC-R:
-
Third-generation cephalosporin-resistant
- 3GC-RO:
-
Third-generation cephalosporin-resistant organism
- AIC:
-
Akaike Information Criterion
- AST:
-
Antimicrobial susceptibility testing
- BSI:
-
Bloodstream infection
- ESBL:
-
Extended-spectrum beta-lactamase
- IPC:
-
Infection prevention and control
- KS:
-
Kolmogorov–Smirnov
- LMIC:
-
Low- and middle-income country
- NICU:
-
Neonatal intensive care unit
- SXT:
-
Trimethoprim–sulfamethoxazole
References
UNICEF. Neonatal Mortality [Internet]. 2020 [cited 2020 Aug 11]. Available from: https://data.unicef.org/topic/child-survival/neonatal-mortality/.
Zea-Vera, A. & Ochoa, T. J. Challenges in the diagnosis and management of neonatal sepsis. J. Trop. Pediatr. 61(1), 1–13 (2015).
Fuchs, A., Bielicki, J., Mathur, S. & Van Den Anker, J. N. Antibiotic Use for Sepsis in Neonates and Children: 2016 Evidence Update. WHO Review. 53 (2016).
Stoll, B. J. et al. Early-onset neonatal sepsis 2015 to 2017, the rise of Escherichia coli, and the need for novel prevention strategies. JAMA Pediatr. 174(7), e200593 (2020).
BARNARDS Group et al. Characterization of antimicrobial-resistant Gram-negative bacteria that cause neonatal sepsis in seven low- and middle-income countries. Nat. Microbiol. 6(4), 512–523 (2021).
Sands, K. et al. Early-onset neonatal sepsis in low- and middle-income countries: Current challenges and future opportunities. Infect. Drug Resist. 15, 933–946 (2022).
Kim, F., Polin, R. A. & Hooven, T. A. Neonatal sepsis. BMJ 1, m3672 (2020).
National Institute for Health and Care Excellence (Great Britain). Neonatal infection: antibiotics for prevention and treatment. https://www.nice.org.uk/guidance/ng195?UID=10709617802022426151814 (2021).
Chan, G. J., Lee, A. C., Baqui, A. H., Tan, J. & Black, R. E. Risk of early-onset neonatal infection with maternal infection or colonization: A global systematic review and meta-analysis. PLoS Med. 10(8), e1001502 (2013).
Dong, Y. & Speer, C. P. Late-onset neonatal sepsis: Recent developments. Arch. Dis. Child. Fetal Neonatal. Ed. 100(3), F257–F263 (2015).
World Health Organization. WHO Recommendations on Newborn Health: Guidelines Approved by the WHO Guidelines Review Committee [Internet] (2017). Report No.: WHO/MCA/17.08. Available from: https://www.who.int/publications/i/item/WHO-MCA-17.08.
Folgori, L., Bielicki, J., Heath, P. T. & Sharland, M. Antimicrobial-resistant Gram-negative infections in neonates: Burden of disease and challenges in treatment. Curr. Opin. Infect. Dis. 30(3), 281–288 (2017).
World Bank. Drug-Resistant Infections: A Threat to Our Economic Future [Internet] (2017). [cited 2020 Oct 16]. Available from: http://documents1.worldbank.org/curated/en/323311493396993758/pdf/final-report.pdf.
Ma, L. et al. Widespread dissemination of aminoglycoside resistance genes armA and rmtB in Klebsiella pneumoniae isolates in Taiwan producing CTX-M-type extended-spectrum-lactamases. Antimicrob. Agents Chemother. 53(1), 104–111 (2009).
Pitout, J. D. & Laupland, K. B. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: An emerging public-health concern. Lancet Infect. Dis. 8(3), 159–166 (2008).
World Health Organization. WHO Publishes List of Bacteria for Which New Antibiotics are Urgently Needed (2017). Available from: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed.
Moremi, N., Claus, H., Vogel, U. & Mshana, S. E. Faecal carriage of CTX-M extended-spectrum beta-lactamase-producing Enterobacteriaceae among street children dwelling in Mwanza city, Tanzania. PLoS ONE 12(9), e0184592 (2017).
Mshana, S. E., Kamugisha, E., Mirambo, M., Chakraborty, T. & Lyamuya, E. F. Prevalence of multiresistant gram-negative organisms in a tertiary hospital in Mwanza, Tanzania. BMC Res. Notes 2(1), 49 (2009).
Kayange, N., Kamugisha, E., Mwizamholya, D. L., Jeremiah, S. & Mshana, S. E. Predictors of positive blood culture and deaths among neonates with suspected neonatal sepsis in a tertiary hospital, Mwanza-Tanzania. BMC Pediatr. 4(10), 39 (2010).
Manyahi, J. et al. Predominance of multi-drug resistant bacterial pathogens causing surgical site infections in Muhimbili National Hospital, Tanzania. BMC Res. Notes https://doi.org/10.1186/1756-0500-7-500 (2014).
Ampaire, L. et al. A review of antimicrobial resistance in East Africa. Afr. J. Lab. Med. 5(1), 6 (2016).
Marando, R. et al. Predictors of the extended-spectrum-beta lactamases producing Enterobacteriaceae neonatal sepsis at a tertiary hospital, Tanzania. Int. J. Med. Microbiol. IJMM 308(7), 803–811 (2018).
Brooks, B. et al. Strain-resolved analysis of hospital rooms and infants reveals overlap between the human and room microbiome. Nat. Commun. 8(1), 1814 (2017).
Folgori, L. et al. The relationship between Gram-negative colonization and bloodstream infections in neonates: A systematic review and meta-analysis. Clin. Microbiol. Infect. 24(3), 251–257 (2018).
Silago, V. et al. Bacteremia in critical care units at Bugando Medical Centre, Mwanza, Tanzania: The role of colonization and contaminated cots and mothers’ hands in cross-transmission of multidrug resistant Gram-negative bacteria. Antimicrob. Resist. Infect. Control 9(1), 58 (2020).
The WHO Young Infants Study Group. Clinical prediction of serious bacterial infections in young infants in developing countries. Pediatr. Infect. Dis. J. 18(Supplement), S23–S31 (1999).
Weinstein M. P. et al. Performance standards for antimicrobial susceptibility testing, 28th edn. (2018).
Hartig, F. Residual Diagnostics for Hierarchical (Multi-level/Mixed) Regression Models. R package version 0.4.4. [Internet] (2021). Available from: https://CRAN.R-project.org/package=DHARMa.
Dijkshoorn, L., Nemec, A. & Seifert, H. An increasing threat in hospitals: Multidrug-resistant Acinetobacter baumannii. Nat. Rev. Microbiol. 5(12), 939–951 (2007).
Mkony, M. F., Mizinduko, M. M., Massawe, A. & Matee, M. Management of neonatal sepsis at muhimbili national hospital in dar es salaam: Diagnostic accuracy of c-reactive protein and newborn scale of sepsis and antimicrobial resistance pattern of etiological bacteria. BMC Pediatr. 14(1), 293 (2014).
Mshana, S. E. et al. Predominance of Klebsiella pneumoniae ST14 carrying CTX-M-15 causing neonatal sepsis in Tanzania. BMC Infect. Dis. 13(1), 466 (2013).
Herbst, A., Wolner-Hanssen, P. & Ingemarsson, I. Maternal fever in term labour in relation to fetal tachycardia, cord artery acidaemia and neonatal infection. BJOG Int. J. Obstet. Gynaecol. 104(3), 363–366 (1997).
Petrova, A. Association of maternal fever during labor with neonatal and infant morbidity and mortality. Obstet. Gynecol. 98(1), 20–27 (2001).
Masanja, H. et al. Factors associated with the decline in under five diarrhea mortality in Tanzania from 1980–2015. J. Glob. Health 9(2), 020806 (2019).
Gorrie, C. L. et al. Gastrointestinal carriage is a major reservoir of Klebsiella pneumoniae infection in intensive care patients. Clin. Infect. Dis. 65(2), 208–215 (2017).
Fenta, S. M., Biresaw, H. B. & Fentaw, K. D. Risk factor of neonatal mortality in Ethiopia: Multilevel analysis of 2016 demographic and health survey. Trop. Med. Health 49(1), 14 (2021).
Liss, B. J. et al. Intestinal colonisation and blood stream infections due to vancomycin-resistant enterococci (VRE) and extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBLE) in patients with haematological and oncological malignancies. Infection 40(6), 613–619 (2012).
Martinez, A. E. et al. ESBL-colonization at ICU admission: Impact on subsequent infection, carbapenem-consumption, and outcome. Infect. Control Hosp. Epidemiol. 40(4), 408–413 (2019).
Simonsen, K. A., Anderson-Berry, A. L., Delair, S. F. & Davies, H. D. Early-onset neonatal sepsis. Clin. Microbiol. Rev. 27(1), 21–47 (2014).
Acknowledgements
Authors would like to thank the Department of Microbiology Laboratory of the Catholic University of Health and Allied Sciences, Bugando; the healthcare workers in NICU and neonatology unit; and study participants.
Funding
This work was funded by the Antimicrobial Resistance Cross-Council Initiative through a grant from the Medical Research Council, a Council of UK Research and Innovation, and the National Institute for Health Research (Award No.: MR/S004815/1).
Author information
Authors and Affiliations
Contributions
V.S., J.S., and S.E.M. designed this study, V.S. and D.R.M. collected research data. V.S. performed laboratory procedures. D.R.M., J.S., and S.E.M. participated in patient management. D.K., K.O., and L.M. analysed and interpreted data. D.K. and L.M. prepared the manuscript which was read and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kovacs, D., Silago, V., Msanga, D.R. et al. The hospital environment versus carriage: transmission pathways for third-generation cephalosporin-resistant bacteria in blood in neonates in a low-resource country healthcare setting. Sci Rep 12, 8347 (2022). https://doi.org/10.1038/s41598-022-11626-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-11626-6
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.