Abstract
The study assessed chronic myocardial, coronary and systemic effects of intracoronary supersaturated oxygen (SSO2) therapy. Left anterior descending coronary arteries of 40 swine were stented and randomized to 90-min selective intracoronary infusion of SSO2 (pO2 760–1000 mmHg) or normoxemic saline. In 20 out of 40 animals, SSO2 delivery followed a 60-min balloon occlusion to induce myocardial infarction (MI). In both normal and MI models, intracoronary treatment with hyperoxemic SSO2 therapy showed no evidence of coronary thrombosis. There were no biologically relevant differences between treatments at either time point in regard to coronary intervention site healing and neointimal growth. No signs of any myocardial or systemic toxicity were observed after 7 or 30 days. A trend was observed toward reduced incidence of microscopic MI scars and reduced infarct size in histopathology, as well as toward better recovery of echocardiographically evaluated global and regional contractility at 30 days. No treatment related infarcts or thromboemboli were observed in the downstream organs.
Similar content being viewed by others
Introduction
Myocardial infarction (MI) remains an important and common cause of morbidity and mortality. This is true despite the revolutionary role revascularization as well as secondary prevention efforts have had in the last few decades on patients’ outcomes. Reperfusion by means of percutaneous coronary intervention (PCI) is the recommended revascularization modality for patients with ST-elevation MI. It confers significant mortality benefit and has been shown to reduce the rates of recurrent ischemic events and re-infarction1. However, even with a flow of Thrombolysis in Myocardial Infarction (TIMI) grade of 3 at the epicardial level, adequate tissue reperfusion assessed by myocardial perfusion grade has only been achieved in up to 66% of patients2,3,4.
Indeed, myocardial salvage does not depend solely on restoring epicardial reperfusion. Among many different factors, microvascular dysfunction and reperfusion injury are important in the degree of residual myocardial damage, and as such have been the focus of several therapeutic approaches1. The use of supersaturated oxygen (SSO2) perfusion to the coronary arteries has been shown, definitively, to improve microvascular flow and left ventricular function in animal models of myocardial infarction5,6. These were followed by a series of clinical trials eventually leading to its marketing approval for clinical use in the US7,8,9. However, a number of detailed questions related to tissue effects and safety of SSO2 therapy have remained. Accordingly, the purpose of this study was to provide a comprehensive assessment of safety (local and systemic) and microscopic myocardial tissue effects of 60 min of intracoronary SSO2 therapy 7- and 30-days after administration in normal myocardium and in infarcted myocardium induced by temporary coronary occlusion. In contrast to previous animal studies, the present experiment involved implantation of stents in all coronary artery to also assess whether SSO2 has any influence on coronary artery healing or stent endothelialization.
Methods
Experimental design
The study was approved by the Institutional Animal Care and Use Committee of the CRF Skirball Center of Innovation, Orangeburg, NY. All animals received standard care outlined in accordance with the Guide to Care and Use of Laboratory Animals by National Academy of Science and Animal Welfare Regulations.
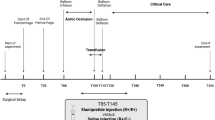
A total of 40 domestic swine (mean body weight 39 ± 4 kg) were included in this study. The mean age at the time of inclusion was 4.60 ± 0.49 months. Induction of anesthesia was achieved with a rapid acting general intramuscular anesthetic (tiletamine + zolazepam, 2–5 mg/kg) supplemented by muscarinic anticholinergic (glycopyrrolate, 0.2 mg/ml, and dosage 0.005–0.02 mg/kg). All animals underwent endotracheal intubation and were maintained with a continuous inhalation of 1–3% isoflurane. Arterial femoral access was obtained, under general anesthesia, using a cutdown technique. Anticoagulation with heparin was achieved (3,000–10,000 U) to maintain activated coagulation time ≥ 250 s. Once under anesthesia, baseline transthoracic echocardiograms (TTE) were performed to rule out any pre-existing underlying structural pathology. Following a pre-established matrix (Fig. 1), the swine were randomized to either a MI (7- or 30-day follow-up) group or to a Non-MI (7- or 30-day follow-up) group and subsequently randomized to either SSO2 therapy (hyperoxemic therapy) or a control group that received normoxemic reperfusion. All animals received a bare metal stent in the target coronary artery to mimic the clinical scenario of PCI. The essentials of study design are summarized in Fig. 1.
Model creation: non-MI animals
Using baseline angiography, suitable segments of the left anterior descending coronary artery (LAD) were selected for stent placement. A bare metal stent (BMS) of 2.5, 2.75, or 3.0 mm × 12 mm (Medtronic Cardiovascular, Santa Rosa, CA) was deployed in the selected coronary segments. Stents were placed per standard interventional procedure in mid-LAD locations comparable ot those used in the MI model (see below), with a target stent to artery ratio of approximately 1.1–1.2:1.0 by online quantitative angiography.
Model creation: MI animals
Using baseline angiography, a coronary angioplasty balloon was advanced to the mid-left LAD. The balloon was inflated to a balloon to artery diameter ratio of 1.2:1 for a total of 60 min to ensure total vascular occlusion. Balloon deflation was immediately followed by 15 min of reperfusion, during which a BMS of 2.5, 2.75, or 3.0 mm × 12 mm sizing (Medtronic Cardiovascular, Santa Rosa, CA) was deployed at the site of preceding occlusion to simulate stenting at the site of the culprit lesion responsible for the coronary occlusion causing the MI. Stents were placed per standard interventional procedure, with a target stent to artery ratio of approximately 1.1–1.2:1.0 by online quantitative angiography.
Device description and SSO2 intracoronary infusion
The TherOx DownStream® System (TherOx Inc, Irvine, California), previously described7,8, was used to deliver the SSO2 infusion. The small extracorporeal circuit pumps blood from an arterial access site (5F sheath) and mixes it with a small amount of highly oxygenated saline (pO2 ~ 30,000 mmHg), producing a hyperoxemic perfusate (pO2 level of 760–1000 mmHg) at 5–7 × the normal oxygen concentration of blood plasma. This perfusate was infused into the LAD via a 4.6 French MI Cath Infusion Catheter (through the contralateral arterial access site (7F)). The procedure required a 5–10 min setup time and a one-time, 90-min infusion at a 50 ml/min flow rate. SSO2 infusion was started immediately after stent implantation. A normoxemic (O2 150-200 mmHg) perfusate was delivered by the system to the control group. The infusion duration was 90 min in both groups.
Angiography
At Day 0 and Day 7 or 30 angiograms were assessed for structural defects (e.g. dissections, ectasia), flow abnormalities, and thrombus presence. Coronary flow was assessed by TIMI flow grade10.
Echocardiography
Two-dimensional echocardiography images for quantitative assessments were acquired in the right lateral decubitus position, using a 5-MHz probe (iE33, Philips Medical Systems, Bothell, WA) in the standard parasternal long-axis and short-axis views. Left ventricle (LV) end-diastolic diameter and end-systolic diameter were determined from short-axis planes; end-diastolic volume (EDV) and end-systolic volume (ESV) were calculated from long-axis planes. LV ejection fraction (EF) was calculated using a standard formula (EF = [(EDV − ESV) / EDV] × 100). LV septal and posterior wall thicknesses were measured at the mid-level from short-axis planes. Segmental wall motion scores were analyzed, per recommendation of the American Society of Echocardiography11, using a 16-segment model. Each segment was assigned a score based on its contractility: normal = 1, hypokinesis = 2, akinesis = 3, dyskinesis = 4. A wall motion score index (WMSI) was then calculated (WMSI = sum of wall motion scores / number of segments visualized). Since among all 16 segments of the whole heart most are normal and not affected by the myocardial infarction, a subset of segments adjacent to the infarcted area were also analyzed to determine a regional wall motion score (Anterior WMSI).
Tissue harvest and histology processing
Hearts were removed immediately following pre-determined termination (7 ± 1 or 30 ± 2 days) and arteries were flushed with Ringer’s lactate for 15 min (1 L). Pressure perfusion fixation was performed for 20 min with 10% neutral buffered formalin. The fixed heart was immersed in a formalin filled container for at least 24 h to continue further fixation. The LAD was dissected and sectioned at proximal, mid, and distal locations of the stented segment. LAD samples were embedded in SPURR resin, sectioned at 5-micron intervals and stained with hematoxylin and eosin (H&E).
Hearts were sectioned across the baso-apical axis, from apex to base, into ~ 8 mm thick slices and examined. Non-MI model hearts were examined grossly and any gross abnormalities were photographed. The 5 apical most slices were placed whole (left and right ventricle) on their basal face in oversized cassettes, processed in paraffin, cut at 5 microns serially, and stained with H&E. MI hearts were examined macroscopically. Six myocardium slices were processed in paraffin, cut at 5 microns twice serially, and stained with H&E and Masson’s Trichrome for planimetric morphometry analysis and measurement of infarct size.
Qualitative histology
All sections of myocardium were evaluated for thrombus, emboli (microemboli), inflammation, lymphohistocytic infiltrates, myocardial fibrosis (infarct scar) or other notable microscopic changes in the myocardium. For each parameter, score of 0 denoted absence, 1 = minimal presence, 2 = single focal presence, 3 = multifocal presence. In each animal, 7 myocardial regions were evaluated in each of the 6 slices for a total of 42 regions. Summary incidence values summed the scores attributed to each of the myocardial areas delineated in the data (left anterior, posterior, lateral ventricle and septum, and right anterior, posterior and lateral ventricle for a total of 7 general areas per tissue section at each of 6 sampling levels per heart equaling a total of 42 possible scoring entries per animal for each finding; with 5 animals in each group, there were 210 myocardial regions examined in each of the eight 5-animal subgroups. Summary values excluded early death animals.
To assess the biological and healing response of vascular tissue to BMS implantation and to identify any possible effects of treatment, ordinal data were collected, and a semi-quantitative scoring system was used to describe vascular tissue responses: peristrut inflammation vessel wall injury, neointima maturity, media hypocellularity, adventitial fibrosis, and endothelialization. Scores range from 0 to 3 (0 = feature absent/no change; 3 = overwhelmingly present feature or full neointima maturity or endothelialization). Specific morphologic and cellular features used to score each specific parameter are described in Online Resource 1.
Quantitative histology of myocardium (MI model)
Infarct boundaries were traced and measured with Image Pro Plus (Media Cybernetics, Bethesda, Maryland). The following morphometric data were collected and analyzed: Histology Section Myocardium Area (HMA) (mm2), Total Histology Section Infarct Area (HIA) (mm2), Total Tissue Slice Area (TSA) (mm2).
From these direct measurements, all other histomorphometric parameters were calculated: Total Number of Infarcted Areas regardless of size, Histology Section Infarct Ratio (HIR): HIR = HIA/HMA; Minimum and Maximum Area (mm2) of infarction; Average Infarct Area (mm2): ΣIA/number of infarcted areas; Infarct Volume (IV) (mm3): IA*Tissue thickness (~ 8 mm); Total Infarct Volume (TIV) (mm3): TIV = ΣIV; Absolute Infarct Area (AIA) (mm2): AIA = TSA*HIR; Absolute Heart Infarct Volume (HIV) (mm3): HIV = Σ(AIA*Tissue thickness) (~ 8 mm); Total Myocardium Volume (TMV) (mm3): TMV = Σ(TSA*Tissue thickness) (~ 8 mm) and Infarct to Myocardium Ratio (IMR): IMR = HIV/TMV.
Control of bias and statistical analysis
In general, animals were chosen for evaluation based on their Test Facility assigned identification number, in ascending order. This order was adjusted as required as a result of procedure cancellations or animal substitutions due to housing or health issues. Each animal received either test or sham infusion, per randomization (randomization order was determined prior to the study initiation using an online random number generator found online at www.randomizer.org). Due to the blinding of the echocardiography, clinical pathology and pathology analysts to the treatments, the targeted sequence of enrollment was not included in the protocol but in a separate document (enrollment matrix) accessible only by the principal investigator. TherOx system operators were informed of individual treatment assignment just prior to stent implant (i.e. post-myocardial infarction). The interventionalist could not be blinded to the study treatment because the TherOx system’s display screen and audible signal clearly indicated whether the infusion was hyperoxemic or normoxemic. The survival duration and infarct or non-infarct conditions were pre-assigned, and the interventions were guided by quantitative angiography, thus reducing operator bias. The principal investigator unblinded the echocardiography, clinical pathology and pathology analysts after completion of the raw data generation.
Summary data of continuous variables are presented as mean ± standard deviation. Summary ordinal data are presented as the median, with data variability represented by the 25th and 75th percentiles. Morphometry and microscopic data were statistically analyzed using appropriate 2-group procedures. A t-test and one-way ANOVA were performed to test the difference of outcomes. A p value of 0.05 or below was considered statistically significant.
Results
Procedural outcomes
No system failures for the DownStream System were experienced in the study. The infusion flow rate was 50 ml/min for each animal assigned to either SSO2 Therapy or Control (sham infusion). All 42 study animals received a complete 90-min. infusion. One infusion catheter was used in 40/42 (95.2%) cases and two infusion catheters were used in 2/42 (4.8%) cases. In each of the cases where multiple MI-Cath Infusion Catheters were used, no adverse effects were observed in the study animals and the 90-min infusions were completed.
No significant difference was witnessed in means of highest (196.4 ± 10.4 mmHg and 193.2 ± 11.3 mmHg) and lowest (186.1 ± 7.6 mmHg and 177.0 ± 9.4 mmHg) pO2 recordings at 30, 60 and 90 min during SSO2 or Sham LAD infusion.
Clinical outcomes
Forty-three animals were enrolled, of which 3 died early, of causes believed to be unrelated to the SSO2 Therapy. One animal died during the infarct model creation and thus received no intracoronary infusion. Another 2 animals died on Day 1 (MI cohort) and Day 5 (non-MI cohort), respectively. Necropsy revealed that the failure to control bleeding from the femoral access site was the most likely cause of death. In both swine the ACT was very volatile and excessive amount of heparin was needed to keep it in the therapeutic range above 250 s. In the MI animal, the microscopic changes in the heart were consistent with terminal hypotension and/or hypovolemia in relation with procedural bleeding and MI model creation. There were no changes in the stented LAD either that would suggest the coronary cause for the early death of this animal. In the non-MI animal, there were no microscopic changes in the myocardium or LAD sections that would suggest the cardiac cause for the early death of this animal.
The remaining 40 animals completed the study as planned without any adverse cardiovascular events, non-cardiovascular health issues or relevant clinical pathology abnormalities. The mortality in the MI study cohort was 10%, which is low but expected given relatively small infarct sizes commensurate with 60 min ischemia period.
Key myocardial outcomes
Echocardiography
As expected, the non-MI animals in the 7 days group and 30 days group had significantly higher EF and lower WMSI than animals who had MI induced. There was a slight trend toward improved left ventricular recovery by 7 days as evidenced by the regional anterior WMSI in the SSO2-treated MI animals and change in EF from post MI to 7 days follow up. This trend was more pronounced at the longer follow-up (30 days) where both EF as well as anterior WMSI differed between SSO2 and sham animals, respectively. None of these differences reached statistical significance (Table 1).
Myocardial histopathology
Myocardial histopathology findings of note are summarized in Table 2. Overall, of 210 regions evaluated in each of the eight 5-animal subgroups, majority of regions presented with no abnormal findings (score 0 for all parameters) except for infarct scars in the 4 MI subgroups, as expected of the model. When found, the abnormalities were mostly scored 1 (minimal presence) and rarely 2 (single focal presence).
The myocardium microscopic data demonstrated the expectedly high incidence of infarct scars in the MI treatment groups. The incidence of this finding was slightly reduced in the SSO2 treated groups compared to the time-matched Sham group. The magnitude of this decrease was slight on Day 7 and more definitive on Day 30 but not statistically significant at either study end point.
There was a low incidence of other background and procedure-related changes such as foreign body microemboli (particulate), microgranulomas and mixed cell infiltrates. These changes appeared at a low incidence in all groups with no evidence of direct relationship to treatment.
There were occasional small foci of myocardial depletion (micro-infarcts) that were related to minute distal ischemic events. Some of these lesions co-located with microemboli. It is likely that these foci were related in large part to particulate distal embolization. Some of the foci may also represent the attenuated expression of low-grade ischemia that may be related to model creation (infarction). However, the incidence or severity of this change did not show a relationship to model creation and/or treatment, except in SSO2 treated infarct group on Day 30. This group also showed the lowest incidence of overt infarct scarring. It is possible that the increase in myocardial depletion foci in this group represents the attenuated expression of overt infarct scars into a greater number of smaller microscopic areas of depletion, consistent with treatment efficacy.
Two animals in the 7-Day non-MI SSO2-treated group showed minimal and localized acute myocardial necrosis. The exact cause of this acute change was unclear. The morphology of the necrosis suggested a 2–3 day time course and therefore appeared unrelated to the procedure or SSO2 treatment.
Representative mid-basal left ventricle cross-sections from each of the 8 groups are shown in Fig. 2. The cross-sections from MI groups contain tracings of the infarcted areas and the number of identified infarcted areas in the particular cross-section.
Myocardial morphometry (infarcted hearts)
At Day 7, the myocardial morphometry data, graphically summarized in Fig. 3, showed an average infarct volume per heart of ~ 3.2cm3 in the Sham group and ~ 3.1cm3 in the SSO2 group (upper left panel). Infarct areas and volume, infarct-to-myocardium ratio, and the total number of infarcted areas were generally comparable between the Sham and SSO2 groups on Day 7. The total myocardium area measured on an identical number of section levels at comparable levels was slightly greater in the SSO2 group suggesting improved tissue viability.
At Day 30, the myocardial morphometry data, graphically summarized in Fig. 4, showed an average infarct volume per heart in the Sham group of ~ 1.5cm3 per heart versus ~ 0.6cm3 in the SSO2 group. There was trend toward decrease in average total infarct volume and area, infarct-to-myocardium ratio, and the total number of infarcted areas in the SSO2 group compared to the Sham group, compatible with a slight increase in total myocardium area in the SSO2 group compared to the Sham-treated hearts. Overall these variations indicated a positive trend for SSO2 in reducing infarct size compared to Sham. There was clearly no increase in infarct areas in the SSO2 group under the conditions of this study.
Key outcomes evaluation of stented arteries
Angiography
Qualitative angiography demonstrated no evidence of thrombus, dissection or ectasia in any animal either pre-treatment, post-stenting, post-infusion or terminal follow-up. As expected, the most common angiographic finding at follow-up was in-stent stenosis which was observed in 18/20 of the 30-day animals and none of the 7-day animals. There did not appear to be any consistent association of stent stenosis with treatment group. The visually estimated degree of stenosis in the 30-day animals is summarized by subgroup in Table 3. Post-infusion, TIMI flow values were all 3 in all 20 MI animals. TIMI flow grade 2 was reported in 8/20 non-MI animals post-infusion. These findings were thought to be related to the depth of anesthesia in a long procedure rather than the true flow impairment; although there was no formal angiographic quantification of myocardial blush of frame count, the angiographic analyst blinded to treatment did not report any observations suggestive of no-reflow or any other angiographically evident microvascular flow impairment. All 7-day and 30-day terminal angiographic examinations featured TIMI 3 flow grade and no other angiographically evident coronary flow abnormalities.
Histopathology
The presence or absence of MI had no impact on the arterial responses to stent placement so the results were only differentiated between SSO2 (n = 20) and Sham (n = 20) and presented in Fig. 5A (7-day outcomes) and Fig. 5B (30-day outcomes). Peri-strut inflammation was minimal and of comparable average score on Day 7 in both groups and appeared slightly increased in the SSO2 group on Day 30 compared to the Sham group. This apparent increase closely correlated with a matching increase in procedural injury that reached statistical significance, and with adventitial inflammation. These increases are believed to be related to variations in procedural injury at stent deployment and independent of SSO2 treatment. Other healing characteristics in the stented vessels in line with expectations after deployment of a bare metal stent and comparable in both the SSO2 and Sham groups. Namely, slight fibrin deposition was observed on Day 7 and was largely resolved at 30 days. Maturation of the neointima progressed comparably in both groups and the neointima was fully mature at 30 days in both groups. The minimal, yet statistically significant increase in neointima fibrin in the sham group on Day 30 compared to the SSO2 group was not considered to be biologically or toxicologically meaningful. Endothelialization was complete in both groups at 30 days. At 7 days there were a few vessels with incomplete endothelialization, namely over areas of unresorbed fibrin. This change was expected at 7 days and due to the very small magnitude of the decrease in the treated group, the variation was considered unrelated to SSO2 treatment. Examination of proximal and distal unstented LAD coronary vessels showed no microscopic changes specifically attributable to SSO2 treatment. Overall, there were no unexpected changes and no features that suggested an effect of SSO2 treatment on vascular healing at 7 or 30 days. Representative cross-sections from each group are presented in Fig. 6.
Key semiquantitative metrics of arterial healing at 7 days (A) and at 30 days (B). Overall, there is no negative impact of SSO2 therapy on the arterial healing parameters in comparison to sham. The incidental statistically significant differences in injury and fibrin deposition are discussed in the text.
Representative in-stent coronary arterial cross-sections from all 8 study subgroups. Typical histological responses to stent placement in normal porcine arteries at 7 days (upper panels) and 30 days (lower) panels. No excess early thrombus formation at 7 days or excess neointima formation at 30 days are seen as a result of SSO2 therapy in comparison to sham. Note: Figs. 1, 2 and 6 generated with Microsoft Office 365 utilizing histology and histomorphometry images generated with ImagePro Plus (MediaCybernetics). Figs. 3, 4 and 5 generated with SigmaPlot v 11.0 (Build 11.2.0.5).
Discussion
SSO2 therapy has emerged in the last decade as possible augmentation for revascularization in MI patients and it has been approved for clinical use in the US. Both animal as well as clinical studies were able to show different degrees of efficacy1,12,13. However, data providing histopathologic insight into of both normal and infarcted myocardium subjected to SSO2 therapy with a commercially established system, as well as histologic assessment of the “culprit” coronary artery, i. e. the infarct-related artery undergoing percutaneous recanalization followed by stent placement, have not been presented to date.
Accordingly, we report here an animal study designed to comprehensively evaluate safety and feasibility aspects of the SSO2 delivery procedure in healthy and infarcted domestic swine. We were able to show absence of SSO2 therapy related adverse effects on normal and non-infarcted myocardium, as well as on the stented coronary arteries. We also found a trend towards decline in MI volume and area in animals treated with SSO2 as compared to sham controls, assessed by histological examination 30 days following MI.
The acute effects of SSO2 therapy on ventricular function and infarct size in MI animal models have been previously studied and documented5,6,14,15. Following equivocal results of efficacy seen with the Acute Myocardial Infarction with Hyperoxemic Therapy (AMIHOT-I) trial, post hoc subgroup analysis of the study suggested that hyperoxemic reperfusion may reduce infarct size in patients with anterior ST-segment elevation MI treated within 6 h of symptom onset16. The follow-up AMIHOT II trial was performed and utilized a prespecified Bayesian approach to allow partial pooling of evidence from the AMIHOT-I trial to be incorporated into the analysis of data in the AMIHOT-II trial. AMIHOT II was a positive trial and met its pre-specified endpoint for infarct size reduction with SSO2 infusion as compared to controls9. Report by Hanson et al.13 described the safety and feasibility of a modified delivery system and technique using SSO2 in patients treated with PCI within 6 h of anterior STEMI. This was further validated in the single-arm IC-HOT study17, with improved 1-year clinical outcomes including lower rates of death and new-onset heart failure or heart failure hospitalizations when compared with a propensity-matched control group18.
The animal model has inherent limitations when it comes to evaluating device efficacy but serves as an excellent candidate for safety evaluations19. Similar to previous studies, we witnessed improvement in ventricular function by echocardiographic measurements in the group treated with SSO2 compared to the sham controls. Increase in EF together with decrease in anterior WMSI were recorded at 7 days and were only slightly better in the SSO2 group. The difference between the two groups became more prominent at 30 days, although without reaching statistical significance. WMSI has been reported to be a more accurate method of assessing LV functions after reperfusion because it negates the effect of non-infarct zone hyperkinesis8,20. A regional wall motion score was determined since most of the 16 segments of the whole heart were normal, hence the need to analyze a subset of the segments regionally which more accurately represents the infracted area. Though no significant difference was seen in either therapy, the trends of both the %EF and Anterior WMSI might imply better prognosis for left ventricular function with SSO2 therapy.
One of the animal model’s advantages is the ability to evaluate tissue effect of therapeutic interventions by means of direct histological exam rather than by surrogate imaging modalities. Overall, there no adverse effects attributable to SSO2 delivery were observed on myocardium of non-infarcted swine, nor on the non-infarcted myocardium in the MI swine. We observed a difference in infarct volume and areas as measured by histology, showing smaller infarcts for the SSO2 treated animals. Once again, the effect of treatment was modest after 7 days but seen clearly at the 30 days end point, without reaching statistical significance. Histological morphometric analysis showed an increase in myocardial tissue area and volume in the SSO2 group at both time points, suggesting improved viability of myocardial tissue compared to the control group. These results are in agreement with previous report by Spears et al.5 further emphasizing the favorable effect SSO2 has on the tissue level.
Concerning safety of the use of SSO2 in regard to the coronary vasculature, histological examination showed no adverse changes in stented LAD arteries and adjacent non-stented segments as a result of SSO2 treatment. The stented vessels showed expected healing and biocompatibility changes for this type of procedure and implantation with a bare metal stent, including variable degree of neointimal formation/in-stent stenosis commensurate with mechanical injury inflicted by the stent as it typical in the porcine model in absence of atherosclerosis. Although at 30 days, the injury score and the fibrin score were statistically significantly different between SSO2 and Sham, the average scores were very low in both groups (less than 0.5 on a 0–3 scale) and the fibrin trended in the opposite direction as injury and inflammation. In genuinely poorer healing, all these parameters would trend in the same direction and the scores would be at least above 1.5 on average. Thus, these differences were considered serendipitous and not related to treatment. No evidence of thrombus was noted in any stented vessels for any animals treated with either SSO2 or Sham treatment, regardless if MI was induced or not.
Evaluation of the downstream organs did not show any adverse effect such as infarcts or thromboemboli. Notwithstanding, two out of three deaths during the study were considered to be related to periprocedural bleeding. Concern regarding periprocedural bleeding was raised following the clinical trials evaluating SSO2 as well13. It is because of that the manufacturer made changes in the delivery system and technique including the use smaller vascular sheath and minimizing the number of arterial punctures needed to complete the procedure13.
Several speculations were made trying to shed light on the pathway by which SSO2 influences cardiac tissue including inhibition of leukocyte adhesions21, alteration of nitric oxide synthase expression22, quenching of lipid peroxidation23, downregulation of β2 integrin24, and reduction of capillary endothelial cell swelling25. As a debate continues about the exact role of oxygen in the treatment of patients with MI, and some evidence suggests even harmful role for it in normoxemic patients1,12, it is important to differentiate that from the use of supersaturated oxygen as a therapeutic modality. Our study design was planned to assess safety and as such was not powered for efficacy measurements. As such, the model was designed for survival and not maximum infarction. Nevertheless, the trends of improvement seen in both functional and histological measurements, add in our opinion to growing body of evidence suggesting efficacy of such treatment in the population of patients with large anterior myocardial infarctions. More importantly, absence of adverse effects on normal myocardium and the arterial response to stent placement is reassuring in view of earlier concerns that SSO2 therapy may be damaging to the myocardium via abundant generation of oxygen free radicals.
Several limitations of this investigation should be acknowledged. The study design was a compromise between the regulatory requirements the study aimed to satisfy, the very complex logistics to complete the study in a reasonably short time, and the high cost associated with this endeavor. . The small sample size of n = 5 in each of the 8 treatment arms was therefore arbitrarily decided as minimally adequate based on historic data. This decision naturally underpowered analysis, not allowing the positive trends becoming significant. Although the study was not designed to be powered for efficacy measurements but rather for proving noninferiority in safety aspects, the trend of a higher ventricular recovery in the SSO2 groups is notable. Another possible limitation in the model design is the use of an infarct model of 60 min rather than longer, which let to modest infarct sizes. On the background of modestly sized control infarcts, demonstrating statistically significant improvements by the therapy is more challenging. Freyman et al.26 reported that similar technique used in their lab resulted in an infarction affecting 20–30% of the left ventricular wall mass. Also, the study did not include an 24-h time point to assess the early response but relied on historical data in that regard6. Lastly, the study used an early delivery technique that does not include all later modifications discussed above, reported in more recent studies13,17,18 and presently used clinically.
Conclusion
In both normal and anterior MI porcine models, intracoronary treatment with hyperoxemic SSO2 therapy showed no evidence of coronary thrombosis or any toxicity (arterial, distal myocardial or systemic) after 7 or 30 days. A trend was observed toward reduced infarct size in histopathology, as well as toward better recovery of echocardiographically evaluated global and regional contractility at 30 days.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to their proprietary nature (owned by the study sponsor) but are available from the corresponding author on reasonable request.
Abbreviations
- SSO2 :
-
Supersaturated oxygen
- MI:
-
Myocardial infarction
- EF:
-
Ejection fraction
- WMSI:
-
Wall motion score index
- PCI:
-
Percutaneous coronary intervention
- TIMI:
-
Thrombolysis in Myocardial Infarction
- TTE:
-
Transthoracic echocardiograms
- BMS:
-
Bare metal stent
- LAD:
-
Left anterior descending coronary artery
- EDV:
-
End-diastolic volume
- ESV:
-
End-systolic volume
- H&E:
-
Hematoxylin and eosin
References
Fordyce, C. B., Gersh, B. J., Stone, G. W. & Granger, C. B. Novel therapeutics in myocardial infarction: Targeting microvascular dysfunction and reperfusion injury. Trends Pharmacol. Sci. 36, 605–616 (2015).
Costantini, C. O. et al. Frequency, correlates, and clinical implications of myocardial perfusion after primary angioplasty and stenting, with and without glycoprotein IIb/IIIa inhibition, in acute myocardial infarction. J. Am. Coll. Cardiol. 44, 305–312 (2004).
Ndrepepa, G. et al. Myocardial perfusion grade, myocardial salvage indices and long-term mortality in patients with acute myocardial infarction and full restoration of epicardial blood flow after primary percutaneous coronary intervention. Rev. Esp. Cardiol. 63, 770–778 (2010).
Ndrepepa, G. et al. Impact of perfusion restoration at epicardial and tissue levels on markers of myocardial necrosis and clinical outcome of patients with acute myocardial infarction. EuroIntervention 7, 128–135 (2011).
Spears, J. R. et al. Aqueous oxygen hyperbaric reperfusion in a porcine model of myocardial infarction. J. Invasive Cardiol. 14, 160–166 (2002).
Spears, J. R., Prcevski, P., Jiang, A., Brereton, G. J. & Vander, H. R. Intracoronary aqueous oxygen perfusion, performed 24 h after the onset of postinfarction reperfusion, experimentally reduces infarct size and improves left ventricular function. Int. J. Cardiol. 113, 371–375 (2006).
Bartorelli, A. L. Hyperoxemic perfusion for treatment of reperfusion microvascular ischemia in patients with myocardial infarction. Am. J. Cardiovasc. Drugs 3, 253–263 (2003).
Dixon, S. R. et al. Initial experience with hyperoxemic reperfusion after primary angioplasty for acute myocardial infarction: Results of a pilot study utilizing intracoronary aqueous oxygen therapy. J. Am. Coll. Cardiol. 39, 387–392 (2002).
Stone, G. W. et al. Effect of supersaturated oxygen delivery on infarct size after percutaneous coronary intervention in acute myocardial infarction. Circ. Cardiovasc. Interv. 2, 366–375 (2009).
Ganz, W. The thrombolysis in myocardial infarction (TIMI) trial. N. Engl. J. Med. 313, 1018 (1985).
Schiller, N. B. et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J. Am. So.c Echocardiogr. 2, 358–367 (1989).
Shuvy, M. et al. Oxygen therapy in acute coronary syndrome: Are the benefits worth the risk?. Eur. Heart J. 34, 1630–1635 (2013).
Hanson, I. D. et al. “Optimized” delivery of intracoronary supersaturated oxygen in acute anterior myocardial infarction: A feasibility and safety study. Catheter Cardiovasc. Interv. 86(S1), S51–S57 (2015).
Spears, J. R. et al. Aqueous oxygen: A highly O2-supersaturated infusate for regional correction of hypoxemia and production of hyperoxemia. Circulation 96, 4385–4391 (1997).
Spears, J. R. et al. Aqueous oxygen attenuation of reperfusion microvascular ischemia in a canine model of myocardial infarction. ASAIO J. 49, 716–720 (2003).
Warda, H. M. et al. Effect of intracoronary aqueous oxygen on left ventricular remodeling after anterior wall ST-elevation acute myocardial infarction. Am. J. Cardiol. 96, 22–24 (2005).
David, S. W. et al. Evaluation of intracoronary hyperoxemic oxygen therapy in acute anterior myocardial infarction: The IC-HOT study. Catheter Cardiovasc. Interv. 93, 882–890 (2019).
Chen, S. et al. One-year outcomes of supersaturated oxygen therapy in acute anterior myocardial infarction: The IC-HOT study. Catheter Cardiovasc Interv 97, 1120–1126 (2021).
Schwartz, R. S. et al. Drug-eluting stents in preclinical studies: Updated consensus recommendations for preclinical evaluation. Circ. Cardiovasc. Interv. 1, 143–153 (2008).
Broderick, T. M. et al. Comparison of regional and global left ventricular function by serial echocardiograms after reperfusion in acute myocardial infarction. J. Am. Soc. Echocardiogr. 2, 315–323 (1989).
Zamboni, W. A. et al. Morphologic analysis of the microcirculation during reperfusion of ischemic skeletal muscle and the effect of hyperbaric oxygen. Plast. Reconstr. Surg. 91, 1110–1123 (1993).
Buras, J. A., Stahl, G. L., Svoboda, K. K. & Reenstra, W. R. Hyperbaric oxygen downregulates ICAM-1 expression induced by hypoxia and hypoglycemia: The role of NOS. Am. J. Physiol. Cell Physiol. 278, C292-302 (2000).
Thom, S. R. & Elbuken, M. E. Oxygen-dependent antagonism of lipid peroxidation. Free Radic. Biol. Med. 10, 413–426 (1991).
Chen, G., Hanson, C. L. & Ebner, T. J. Functional parasagittal compartments in the rat cerebellar cortex: An in vivo optical imaging study using neutral red. J. Neurophysiol. 76, 4169–4174 (1996).
Hills, B. A. A role for oxygen-induced osmosis in hyperbaric oxygen therapy. Med. Hypotheses 52, 259–263 (1999).
Freyman, T. et al. A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. Eur. Heart J. 27, 1114–1122 (2006).
Funding
The study is reported in conformance with the ARRIVE Guidelines.
Author information
Authors and Affiliations
Contributions
G.L.K. oversaw the study conduct, data analysis and edited the manuscript into the final form, J.L.C. designed the study and reviewed/edited the manuscript, A.F., M.E.A., K.M., G.H.Y., Y.C., G.B.C., J.C.M. and D.B. performed the study procedures and analyzed the clinical and imaging data as well as wrote different portions of the manuscript, S.D.R. conducted the histopathology analysis, J.F.G. and D.B. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The study was funded by TherOx. J. F. Granada is the CEO and G. L. Kaluza is an employee of the Cardiovascular Research Foundation which receives research and educational grant support from TherOx and ZOLL. J. Creech and D. Blum are employees of ZOLL/TherOx. D. Burkhoff is a consultant to ZOLL/TherOx. Other authors have no conflicts to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaluza, G.L., Creech, J.L., Furer, A. et al. Chronic myocardial and coronary arterial effects of intracoronary supersaturated oxygen therapy in swine with normal and ischemic-reperfused myocardium. Sci Rep 12, 5785 (2022). https://doi.org/10.1038/s41598-022-09776-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-09776-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.