Abstract
The Enhanced Recovery After Surgery (ERAS) protocol affected traditional cardiac surgery processes and COVID-19 is expected to accelerate its scalability. The aim of this study was to assess the impact of an ERAS-based protocol on the length of hospital stay after cardiac surgery. From January 2019 to June 2020, 664 patients underwent consecutive cardiac surgery at a Latin American center. Here, 46 patients were prepared for a rapid recovery through a multidisciplinary institutional protocol based on the ERAS concept, the “TotalCor protocol”. After the propensity score matching, 46 patients from the entire population were adjusted for 12 variables. Patients operated on the TotalCor protocol had reduced intensive care unit time (P < 0.025), postoperative stay (P ≤ 0.001) and length of hospital stay (P ≤ 0.001). In addition, there were no significant differences in the occurrence of complications and death between the two groups. Of the 10-central metrics of TotalCor protocol, 6 had > 70% adherences. In conclusion, the TotalCor protocol was safe and effective for a 3-day discharge after cardiac surgery. Postoperative atrial fibrillation and renal failure were predictors of postoperative stay > 5 days.
Similar content being viewed by others
Introduction
Over time, cardiac surgeries have become more complex, although safer and more effective. Along with technology, advances in teamwork have been responsible for these improvements1. However, the length of hospital stay after cardiac surgery has remained constant in recent decades, mainly in underdeveloped countries2,3.
In this regard, we highlight the impact of Enhanced Recovery After Surgery (ERAS)4, an innovative concept that has disrupted the traditional surgical care through the application of protocols that focus on enhancing patient recovery and generate value in surgeries through implement an optimized perioperative pathway. Evidence on the reduction on hospital length of stay and costs, as well as the reduction of morbimortality, start to gain strength, this time focused on cardiac surgery5,6,7,8.
For a long time, the care of patients admitted to the hospital to perform cardiac surgery focused only on decreasing surgical aggressiveness or on optimizing isolated anesthetic processes. Minimally invasive surgeries with smaller incisions or without the use of CPB started to be performed to reduce hospitalization times9, even so, fast-track protocols for early extubation on adult cardiac surgery10 were also not able to reduce the length of hospital stay in isolation. Suggesting that processes within the system need to be connected and synchronized.
Thus, in the current context, the decrease in hospital stay becomes one of the most potential weapons to cardiac surgery, aiming at lower risk of complications, increasing the bed turnover, decreasing the consumption of hospital resources, and helping the sustainability of cardiac surgery programs. The aim of this study was to evaluate whether this protocol based on ERAS was effective and safe in reducing the length of hospital stay after cardiac surgery.
Material and methods
Patients and sample
This is an observational and prospective study with a cohort of 664 patients undergoing cardiac surgery at a Brazilian referral center, part of the STS Adult Cardiac Surgery Database11, between January 2019 to June 2020. This service line to cardiac surgery patients is engaged in the hospital's quality and safety program12, the same accredited by the National Accreditation Organization (ONA) and the Joint Commission. For application of this protocol, the study’s executive committee defined the following criteria.
Inclusion criteria
All patients scheduled for cardiac surgery were invited to be part of the protocol after acceptance by the surgical teams responsible for the case.
Exclusion criteria
Patients with STS score > 2, emergency status, use of vasoactive drugs, history of psychiatric disorders, drug addict and/or impaired ambulation.
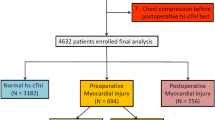
For the Propensity matching, patients who received mechanical valve prostheses (need for anticoagulation), procedures in the aorta and combined surgeries (coronary artery bypass grafting [CABG] + heart valve surgery, mitral valve + aortic valve surgery, etc.) were excluded. Figure 1 shows the types of analyzes performed to compare outcomes of complications, readmission, and operative mortality.
All patients who agreed to be part of the study were analyzed, so it was an analysis by intention to treat. Operative mortality was defined as (1) all deaths occurring during the hospitalization in which the operation was performed, even if after 30 days; and (2) all deaths occurring after discharge from the hospital, but before the end of the thirtieth postoperative day. The definition of variables and other outcomes follows the STS ACSD version 2.9.
During the study period, there were no changes in the surgical team (surgeons, anesthesiologists, cardiologists, and intensive care physicians) dedicated to this line of care.
Implementation of TotalCor protocol and team building
After institutional approval, the TotalCor protocol was discussed with the hospital team to implement a multidisciplinary care line. Weekly classes, meetings and training sessions were held to disseminate the concept in the hospital and discuss solutions to the identified obstacles. Implementation, training and simulation of this flow took approximately 6 months.
Patient data related to the study were collected in a single database. The protocol was coordinated by the Hospital's Cardiac Surgery Quality Program, in multidisciplinary collaboration with anesthesiologists, perfusionists, intensivists, cardiologists, physiotherapists, nutritionists and nursing groups. Thus, in July 2018, this taskforce developed a pragmatic strategy of gradual implementation, which involved the implantation of the TotalCor protocol including the pre-hospitalization phase (elective patients), perioperative care phases in the hospital and follow-up after discharge. Specific measures for the different processes were included in the protocol based on a combination of literature review and institutional experience, and finally approved by the coordinators of the participating groups together with the hospital board. These guidelines consist of metrics for patient care processes (Fig. 2). TotalCor patients were intended to receive these guidelines, unless contraindicated based on existing comorbidities or due to occurrences. Even when any specific intervention was suspended or changed, patients continued to be assessed according to the TotalCor protocol and maintained the ERAS concept. Adherence rates to the process measurements, as well as relevant STS ACS v2.9 variables, were also analyzed. The primary endpoint was the postoperative time after cardiac surgery, as it becomes more suitable for the inclusion of non-elective patients who had to wait for surgery due to preoperative exams, use of anticoagulants and/or antiaggregants, renal protection, etc.
Finally, the TotalCor protocol incorporates Lean Six Sigma concepts13 to eliminate waste from traditional surgical flow. Thus, the protocol was designed to be safe for a 3-day perioperative period. In summary, the TotalCor protocol in relation to the routine has minor changes in surgical technique and important changes in anesthesia, perfusion, and care outside the operating room (Supplemental file 1 for protocol details).
Statistical analysis
In the descriptive analysis, continuous variables were expressed in terms of summary measures (mean, median, standard deviation and quartiles), while categorical variables were expressed as percentages. Bar charts were used to illustrate categorical variables, while boxplots were used to illustrate continuous variables. The propensity score matching (PSM) was used to pair the groups using the nearest neighbor method, available in the "matchit" package of the R software. For the comparison of two groups in continuous variables, the t-test was used for variables that followed the normal distribution (Anderson–Darling test) and for the others, the non-parametric Mann–Whitney and Brunner-Munzel tests were used, respectively, for homogeneous and heterogeneous variables (Bartlett’s test). Fisher's exact test was used for categorical variables. A logistic regression analysis was performed to identify the variables related to a postoperative stay > 5 days after cardiac surgery in the non-TotalCor group. Considering only the variables that were significant in simple regressions, the multiple model was developed. It was validated through the Hosmer–Lemeshow test for the calibration phase and the ROC curve test for the discrimination phase. The level of significance adopted in the tests was 0.05. Two-tailed hypotheses were considered. The software R version 3.6.0 was used to perform all analyzes14.
Ethics and consent
The project was submitted and approved by the Research Ethics Committee of the Hospital Pró-Cardíaco (CAAE: 25123519.6.0000.5533), email address available at: comite.etica@procardiaco.com.br . The free and informed consent was waived by the Ethics Committee due to the analysis of pre-established data logs. We declare that all methods were performed in accordance with relevant guidelines and regulations.
Results
Of the 664 patients in the registry, 3 were excluded from the TotalCor group and 176 from the non-TotalCor group, resulting in 485 patients (46 TotalCor and 439 non-TotalCor). In general, there were younger patients, with a lower STS risk score and a higher left ventricular ejection fraction (LVEF) in the TotalCor group. These patients also had shorter cardiopulmonary bypass (CPB) time and shorter intensive care unit (ICU), postoperative and total hospital stays, as well as receiving less red blood cell concentrates (Supplemental Material 2). After the PSM, we compared these TotalCor patients with other 46 non-TotalCor patients adjusted for 12 variables: age, gender, functional class, insulin dependence, atrial fibrillation, STS risk score, LVEF, creatinine, type of admission, CPB time, recent acute myocardial infarction (< 21 days) and CABG surgery. Here, we observed that both groups had no significant difference in relation to complications and death, except for ICU stay (days), postoperative hospital stay (days) and length of hospital stay (days) (Supplemental Material 3).
It is worth mentioning that the extubation time in both groups had a median of less than 3 h, an indicator that has encouraged us since the beginning to implement our rapid recovery protocol. The adherence to the goals established for TotalCor patients is shown in Table 1, where the adhesion of 6 metrics was > 70%.
A regression analysis was performed to identify the predictors of a postoperative stay > 5 days after cardiac surgery in non-TotalCor patients who survived. Using the variables that were significant in the simple regressions, the multiple model was built (Table 2).
To test the model’s performance, the Hosmer–Lemeshow test (P = 0.285) showed that the model was well calibrated. Moreover, C statistics (0.74, 95% CI 0.69–0.79) revealed that the multiple model is appropriate to predict postoperative stay > 5 days after cardiac surgery (Fig. 3).
Discussion
As far as we know, this is the first study using a protocol based on ERACS in Latin America. The TotalCor protocol was safe and effective for hospital discharge 3 days after cardiac surgery. The success achieved in reducing the length of hospital stay is similar to that presented by Chris Malaisrie at STS 202015. Therefore, these findings become an opportunity to redesign the traditional flow of cardiac surgery in the world.
The measures proposed by the enhanced recovery protocols are innovative, break paradigms and directly confront pre-established measures3. For this reason, they are being applied slowly and gradually despite evidence of their effectiveness3,4.
At first, the ERAS protocol was applied only in colorectal surgeries, generating a considerable volume of scientific evidence within the context of this specialty. With the encouragement of excellent results, other medical specialties started to become interested and to adopt the ERAS concept; with cardiac surgeries, it was not different. Since 2017, professionals from different fields came together to establish the guideline of “Enhanced Recovery After Cardiac Surgery” (ERACS)1,5,6,7,16,17,18,19. To add knowledge to the scientific community, we decided to share the results of the TotalCor protocol at Hospital Samaritano Paulista, from São Paulo, Brazil.
Teamwork was essential for the successful implementation of the protocol and can represent a challenge for some institutions20. Implementation must be cautious since habits and paradigms are difficult to change21. For this, our team took held classes/meetings and training to disseminate the concept and discuss solutions about possible obstacles, and after implementation, our group continues to meet weekly to discuss the process, once the communication between professionals in the different phases of hospitalization is the main factor for the “key” to success.
The average length of postoperative hospital stays after isolated primary elective CABG in one of the reference hospitals in our region is 8.5 days22. Therefore, this protocol would have the potential to rotate the bed almost 3 times faster. In the new era, models like this could help maintain essential surgeries, and reducing the consumption of resources for patients hospitalized23. We believe that the implementation of an enhanced recovery protocol would be necessary to resume elective cardiac surgeries, as suggested by other surgical specialties24,25.
In the 92 patients analyzed in the propensity score, besides the significant reduction in postoperative time, there was a decrease in the appearance of atrial fibrillation from 8.7% in the non-TotalCor group to 4.4% in the TotalCor group, however, although a reduction > 2 times, this was not significant (P = 0.159). Perhaps the sample size was not enough to show the results achieved by Malaisrie in Chicago15 and by Fleming in London17. It should be noted that, although not significant, there was also a decrease in the number of hospital readmissions from 7.1 to 2.2% (P = 0.344) in the TotalCor group. For analysis of the metrics, 10 central processes were chosen to assess whether adherence to them was the reason for the success in the application of the protocol, and it was found that there was an adherence greater than 80% in the abbreviation of fasting, elimination of the preoperative use of anxiolytics/sedatives, and application of opioid less/opioid-free concept and postoperative ≤ 5 days. It is worth mentioning that all patients in the TotalCor group underwent medical reevaluations in the afternoon, which, together with the standardization of multidisciplinary practices, must have influenced the preparation and recovery of patients26,27.
Goeddel28 showed that early extubation improves results; differently, Kandasamy29 reported that, even though early extubation offers an advantage over accelerated recovery and shorter ICU and hospital length of stay, it showed no significant difference in patient results. In our analysis, the median extubation time in both groups was less than 3 h and had no significant difference (P = 0.477). However, this metric did not affect the reduction in ICU time, postoperative stay and length of hospital stay in the TotalCor group. Here, we found that 91% of patients were extubated within 6 h and 39% within 2 h. As the metric used for this flow was up to 2 h, it becomes an opportunity to improve and revise our flow.
Analyzing the predictors of a postoperative stay > 5 days after cardiac surgery, there are some characteristics of the patients that would help to weigh in the planning of a specific hospitalization. The preoperative and non-modifiable variables were female gender, presence of atrial fibrillation, urgency surgery and an increased STS risk score. Here, perhaps the urgency status and STS value could be improved. However, in practice, it is difficult to find time for clinical optimization, hospital discharge and elective readmission for surgery. Finally, the two outcomes related to a postoperative stay > 5 days were atrial fibrillation and renal failure, which could be mitigated through risk identification and prevention strategies and, in the case of atrial fibrillation, we also have the option of concomitant treatment during the treatment of underlying heart disease, as recently supported by the European guideline30.
Limitations
1. The study is unicentric and coming from a hospital that reports to the STS Cardiac Surgery since 2011. Therefore, is likely that the results may be difficult to be achieved by other centers in other regions. However, the protocol is objective, clear and includes central processes in the journey of the patient who is hospitalized for cardiac surgery. We believe that adherence to the metrics will bring significant results regardless of the characteristics of the hospital. 2. Due to the current COVID-19 pandemic, our rate of inclusion of patients in the protocol has dropped to an average of 2 to 3 patients per month. 3. This was not a randomized study. However, a PSM analysis was performed from a structured, audited, and validated database for cardiac surgery. 4. The group of patients enrolled in the TotalCor Protocol was less than 10%, which limits its impact on the system. To improve this, and after the initial results, we obtained support from the executive management of the hospital so that, from July 2020, all patients with cardiac surgery schedule will be approached within the ERAS concept. Currently, the majority, and not the minority, of patients receive shortening of fasting, modular anesthesia with spinal erector block, as well as intensified physiotherapy protocols. To facilitate the advancement of this culture of patient preparation and optimization, the KAMAY health app is being built with the purpose of engaging patients and hospital staff to improve adherence to metrics.
This new bundled approach to perioperative care is based on the philosophy that patients do better when emotional and physiological stresses are minimized during surgery. The goal of this concept is to return patients to normal functional status as soon as possible. For this, the protocol involves a methodical shift in culture, sustaining a meaningful organizational change, and pivoting to a patient-centered care system. Herein we detail the crucial team building, education, planning, and the processes needed to develop and maintain a successful program.
In conclusion, the TotalCor protocol based on ERAS concept significantly reduced the postoperative hospital stay after cardiac surgery in a safe and effective way. Improvements in team communication through applications, as well as in interaction with patients and family members, should be introduced to increase adherence to the protocol, as well as to continuously improve results.
Further studies should be conducted to balance the advantages and disadvantages of the TotalCor protocol, as well as its sustainability and scalability.
References
Wilson, J. L., Whyte, R. I., Gangadharan, S. P. & Kent, M. S. Teamwork and communication skills in cardiothoracic surgery. Ann. Thorac. Surg. 103, 1049–1054 (2017).
Zheng, Z. et al. Comparing outcomes of coronary artery bypass grafting among large teaching and urban hospitals in China and the United States. Circ. Cardiovasc. Qual. Outcomes 10, 1–8 (2017).
Almashrafi, A., Alsabti, H., Mukaddirov, M., Balan, B. & Aylin, P. Factors associated with prolonged length of stay following cardiac surgery in a major referral hospital in Oman: a retrospective observational study. BMJ Open 6, 1–7 (2016).
Ljungqvist, O., Scott, M. & Fearon, K. C. Enhanced recovery after surgery a review. JAMA Surg. 152, 292–298 (2017).
Engelman, D. T. et al. Guidelines for perioperative care in cardiac surgery: enhanced recovery after surgery society recommendations. JAMA Surg. 154, 755–766 (2019).
Grant, M. C. et al. Results from an enhanced recovery program for cardiac surgery. J. Thorac. Cardiovasc. Surg. 159, 1393-1402.e7 (2020).
Li, M. et al. Enhanced recovery after surgery pathway for patients undergoing cardiac surgery: a randomized clinical trial. Eur. J. Cardio-thoracic Surg. 54, 491–497 (2018).
Williams, J. B. et al. One-year results from the first US-based enhanced recovery after cardiac surgery (ERAS Cardiac) program. J. Thorac. Cardiovasc. Surg. 157, 1881–1888 (2019).
Sellke, F. W. et al. Comparing on-pump and off-pump coronary artery bypass grafting: numerous studies but few conclusions. A scientific statement from the American Heart Association council on cardiovascular surgery and anesthesia in collaboration with the interdisciplinary working group on quality of care and outcomes research. Circulation 111, 2858–2864 (2005).
Wong, W.T., Lai, V.K.W., Chee, Y.E. & Lee, A. Fast‐track cardiac care for adult cardiac surgical patients. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No.: CD003587. https://doi.org/10.1002/14651858.CD003587.pub3. Accessed 04 Apr 2021.
de Silva, P. G. M. B. et al. Improving indicators in a Brazilian hospital through quality-Improvement programs based on STS database reports. Braz. J. Cardiovasc. Surg. 30, 660–663 (2015).
de Barros Silva, P. G. M. et al. Improvement in quality indicators using NCDR registries: first international experience. Int. J. Cardiol. 267, 13–15 (2018).
Mason, S. E., Nicolay, C. R. & Darzi, A. The use of Lean and Six Sigma methodologies in surgery: a systematic review. Surgeon 13, 91–100 (2015).
Team, R. C. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing (2019).
Malaisrie, C. Safer, Quicker Discharge With Protocols for Enhanced Recovery After Surgery. Yael L. Maxwell 1–5 (2020). https://www.tctmd.com/news/safer-quicker-discharge-protocols-enhanced-recovery-after-surgery.
Lilot, M. et al. Variability in practice and factors predictive of total crystalloid administration during abdominal surgery: retrospective two-centre analysis. Br. J. Anaesth. 114, 767–776 (2015).
Fleming, I. O. et al. Aggregation of marginal gains in cardiac surgery: feasibility of a perioperative care bundle for enhanced recovery in cardiac surgical patients. J. Cardiothorac. Vasc. Anesth. 30, 665–670 (2016).
de Martins, M. V. D. C. Are we ready for the implantation of the ERAS protocol?. Rev. Col. Bras. Ciric. 44, 314–315 (2017).
Jessica K Brown, M.D., Karanbir Singh, M.D., Razvan Dumitru, C.R.N.A., D.N.P., Edward Chan, M.D., and Min P. Kim, M. D. Benefits of ERAS programs and their application in Cardiothoracic surgery. Methodist Debakey Cardiovasc J. 14, (2018).
Mejía, O. A., Lisboa, L. A. & Jatene, F. B. Continuous quality improvement programme in cardiovascular surgery: the Latin American perspective. Eur. J. Cardio-thoracic Surg. 50, 4–5 (2016).
Mejia, O. A. V. et al. Analysis of >100,000 cardiovascular surgeries performed at the heart institute and a new era of outcomes. Arq. Bras. Cardiol. 114, 603–612 (2020).
da Silva, G. S., Colósimo, F. C., de Sousa, A. G., Piotto, R. F. & Castilho, V. Coronary artery bypass graft surgery cost coverage by the Brazilian unified health system (SUS). Braz. J. Cardiovasc. Surg. 32, 253–259 (2017).
Engelman, D. T. et al. Ramping up delivery of cardiac surgery during the COVID-19 pandemic: a guidance statement from the society of thoracic surgeons COVID-19 task force. Ann. Thorac. Surg. 110, 712–717 (2020).
Fantola, G., Nagliati, C., Foletto, M., Balani, A. & Moroni, R. Is there a role for ERAS program implementation to restart bariatric surgery after the peak of COVID-19 pandemic?. Obes. Surg. https://doi.org/10.1007/s11695-020-04676-0 (2020).
Borghi, F., Pellegrino, L., Pruiti, V., Donati, D. & Giraudo, G. Feasibility of enhanced recovery after surgery program in colorectal surgery during COVID-19 pandemic in Italy: should we change something?. Updates Surg. 72, 319–320 (2020).
Mustafa, A. & Mahgoub, S. Understanding and overcoming barriers to timely discharge from the pediatric units. BMJ Qual. Improv. Reports 5, u209098.w3772 (2016).
Safavi, K. C. et al. Development and validation of a machine learning model to aid discharge processes for inpatient surgical care. JAMA Netw. open 2, e1917221 (2019).
Goeddel, L. A., Hollander, K. N. & Evans, A. S. Early extubation after cardiac surgery: a better predictor of outcome than metric of quality?. J. Cardiothorac. Vasc. Anesth. 32, 745–747 (2018).
Ashok Kandasamy, S. K. R., Hariharan, A. S., Sukumar, A. & Bakthavatsala, D. R. H. K. Ultra fast—tracking versus a conventional strategy in valve replacement surgery. Indian J. Anaesth. 57, 298–300 (2013).
Hindricks, G. et al. ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur. Heart J. https://doi.org/10.1093/eurheartj/ehaa612 (2020).
Acknowledgements
Nelson Yamazaki, Ivo Richter, Paulo Chaccur, Gil Vicente Lico e Cividanes, Honório Palma, Thays Antunes, Debora Cristina Di Donato, Fernanda Nakazato, Gianni Manzo, Luciana Seabra, Paula Cremasco, Sonia Batista, Nelson Saruhashi, Viviane Fernandes, Douglas Ribeiro, Felipe Malafaia, Marcelo Jamus Rodrigues and Antonio Baruzzi.
Author information
Authors and Affiliations
Contributions
Conception and design of the research: O.A.V.M., G.B.B.; Acquisition of data: O.A.V.M., N.L., T.S., M.Y.O., M.S.B.G., M.L.N.N.F., H.P.G.B., L.M.G.M., M.C.S.; Analysis and interpretation of the data: O.A.V.M., G.B.B., J.C.T.G.; Statistical analysis: O.A.V.M., G.B.B.; Writing of the manuscript: O.A.V.M., G.B.B.; Critical revision of the manuscript for intellectual content: O.A.V.M., P.G.M.B.S., J.C.T.G., V.F.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mejia, O.A.V., Borgomoni, G.B., Lasta, N. et al. Safe and effective protocol for discharge 3 days after cardiac surgery. Sci Rep 11, 8979 (2021). https://doi.org/10.1038/s41598-021-88582-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-88582-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.