Abstract
Polymerase chain reaction (PCR) using deoxyribonucleic acid (DNA) extracted from dried blood spots (DBS) provides a fast, inexpensive, and convenient method for large-scale epidemiological studies. This study compared the performance of PCR between DNA extracted from DBS and DNA obtained from whole blood for detecting malarial parasites. Primary studies assessing the diagnostic performance of PCR using DNA extracted from DBS and whole blood for detecting malarial parasites were obtained from the ISI Web of Science, Scopus, and PubMed databases. Odds ratios (ORs) and 95% confidence intervals (CIs) were plotted in forest plots using Review Manager version 5.3. Statistical analysis was performed via random-effects meta-analysis. Data heterogeneity was assessed using the I2 statistic. Of the 904 studies retrieved from the databases, seven were included in this study. The pooled meta-analysis demonstrated no significant difference in the comparative performance of PCR for detecting malaria parasites between DNA extracted from DBS and that extracted from whole blood (OR 0.85; 95% CI 0.62–1.16; I2 = 78%). However, subgroup analysis demonstrated that PCR using DNA extracted from DBS was less accurate in detecting Plasmodium vivax than that using DNA extracted from whole blood (OR = 0.85; 95% CI 0.77–0.94). In conclusion, a significant difference in detecting P. vivax was observed between PCR using DNA extracted from DBS and that using DNA extracted from whole blood. Therefore, P. vivax in endemic areas should be identified and detected with care with PCR using DNA obtained from DBS which potentially leads to a negative result. Further studies are required to investigate the performance of PCR using DBS for detecting P. vivax and other malarial parasites to provide data in research and routine surveillance of malaria, especially with renewed efforts towards the eradication of the disease.
Similar content being viewed by others
Introduction
The gold standard method for detecting malarial parasites in routine laboratories is based on the examination of thick and thin blood films under light microscopy1. The microscopic method provides several advantages for the diagnosis of malarial parasites including a relatively simple technique, low cost, and the ability to identify Plasmodium species and its parasite density; however, the microscopic method provides a low limit of detection (LOD) of malarial parasites with a sensitivity of 50–500 parasites/μl2. Another malarial detection method is the use of rapid diagnostic tests (RDTs) that detect malarial antigens in the blood of patients with a sensitivity of ~ 100 parasites/μl2. The commonly targeted RDT antigens are histidine-rich protein 2 (HRP2), lactate dehydrogenase (pLDH), and aldolase, among which HRP2 is the most commonly used target in commercial kits due to its specificity to P. falciparum3. Although RDTs have been used in remote parts of malaria-endemic areas, they present several disadvantages like false positives in the blood of patients who were cured of malaria infections4. Also, RDTs can provide false-positive results for non-P. falciparum malaria if patients have a high-parasite density of P. falciparum5. RDTs can provide false-negative results due to gene deletions6 or a low parasite density of malarial parasites in the blood samples3. The introduction of molecular assays such as polymerase chain reaction (PCR) has improved the sensitivity and specificity of malarial diagnosis7,8,9. Molecular assays have allowed the detection of submicroscopic Plasmodium infection in parasite carriers with high sensitivity as well as the identification of all five malarial species10,11. Therefore, PCR is particularly valuable when subjective microscopy does not permit the identification of certain malarial species. Moreover, it can indicate monoinfections and mixed infections and serves as a useful tool for the epidemiological understanding of malarial infections. The principle of PCR is to amplify a targeted malarial DNA in whole blood samples via venipuncture or finger-prick. Although blood collection using a standard venipuncture technique provides a large amount of blood, it has several limitations including patient reluctance, transportation of blood samples, and prolonged freezing of blood, making it difficult to conduct malarial epidemiological surveys among patients or residents in resource-limited settings. To overcome the limitations of venous blood collection, dried blood spots (DBSs) were introduced as a blood collection technique for a minute amount of blood. DBSs require a small amount of blood to be dropped onto a filter paper which is collected using the finger-prick method that is less invasive than venous blood collection12. Therefore, it is a blood collection technique that is conveniently performed in large-scale epidemiological studies13,14. Although DBS has advantages over venous blood collection in large-scale studies and surveys undertaken in remote areas, several studies have demonstrated that the PCR method using DNA extracted from DBS had a lower sensitivity than PCR using DNA extracted from venous blood collection14,15,16,17. Because the collection and transport of blood samples are critical for studies targeting malarial parasites, assessing the performance of PCR using extracted DNA from DBS and whole blood is critical for providing confidence in using DBS, which is currently used in different studies. Thus, this study assessed the performance of PCR using DNA from DBS and whole blood for detecting malarial parasites in patients. The results of this study will determine the advantages and disadvantages of using DBS, which are essential considerations in research and routine surveillance of malaria, especially with renewed efforts toward the eradication of the disease.
Methods
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines18.
Eligible studies
Primary studies that assessed the diagnostic accuracy of PCR using DNA obtained from both DBS and whole blood for the detection of malaria parasites were eligible. The inclusion criteria were as follows: studies including febrile patients seeking care at health facilities or residents in communities in malaria-endemic regions and studies comparing the performance of PCR using DNA from DBS and whole blood to confirm cases of malaria. Animal studies, case reports, case series, clinical drug trials, experimental studies, vector studies, polymorphism studies, short reports, and reviews were excluded, as well as studies not written in the English language, those without full text, and those with incomplete data for extraction.
Search strategy
The search strategy began with electronic databases including ISI Web of Science, Scopus, and PubMed with the provided search terms (Table S1). Literature searches were started and ended at 4 March 2020. To avoid missing studies, the search terms were kept broad and provided as ‘dried blood spot’ AND (‘polymerase chain reaction’ OR PCR) AND (malaria OR Plasmodium). In addition, the reference lists of the selected studies, reviews, and systematic reviews were manually checked for other possible related studies.
Selection criteria
The selection criteria were based on title and abstract selections by two independent authors (AM and MK). Any duplicate studies were removed by Endnote software (Clarivate Analytics). Studies that were not related to Plasmodium species or malaria and those in which PCR was not used for detection were removed following title and abstract screening. All studies considered relevant to the eligibility criteria were selected, and the full text was evaluated. Disagreements between the two reviewers were resolved by consulting a third author (GM or FM). Study information and fulfilment of the inclusion criteria were recorded in Microsoft Excel spreadsheets (Microsoft Corporation, CA, USA) for further analysis.
Data extraction
Two authors (AM and MK) selected and extracted data from the included studies independently into Microsoft Excel spreadsheets. The extracted information was as follows: authors, year of publication, participants, age range, gender, blood storage for PCR, DNA extraction methods, investigated gene, and the results of PCR using both filter paper and whole blood.
Statistical analysis and data synthesis
A meta-analysis was performed to assess the comparative performance of PCR using DNA extracted from DBS and DNA extracted from whole blood for malarial detection. Odds ratios (ORs) and 95% confidence intervals (CIs) were plotted in forest plots using Review Manager (RevMan) Version 5.3 (The Cochrane Collaboration). Statistical analysis was performed using random-effects meta-analysis if unexplained heterogeneity was frequently present. Subgroup analysis of Plasmodium species was performed. Data heterogeneity was assessed using the I2 statistic, and values exceeding 25% indicated moderate or high heterogeneity among the included studies.
Quality of the included studies
The quality of included studies was assessed using the Newcastle–Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses19, and the highest score was eight stars.
Publication bias
The publication bias of the included studies was assessed by funnel plot symmetry.
Results
Characteristics of the included studies
The searches of PubMed, ISI Web of Science, and Scopus databases retrieved 59, 44, and 801 studies, respectively. After removing duplicates, 816 studies were screened using the title and abstract. Then, the full text of 331 studies was screened. Of these studies, 324 were excluded for several reasons, as detailed in Fig. 1. Finally, seven studies9,12,14,15,16,20,21 were included in the present study (Table 1). All included studies were published between 2008 and 2017, and 4001 malaria positive-patients as identified using DNA extracted from DBS and 3878 malaria positive-patients as identified using DNA extracted directly from whole blood were included. Most of the included studies (6/7, 85.7%) were conducted in Asian countries including Saudi Arabia15, Iran14, Cambodia9, Thailand16, Canada20, and Myanmar21, whereas one study was conducted in Tanzania12. Among 7 studies, 3 studies12,15,16 (42.9%) recruited only febrile participants for the experiments. Five studies12,14,16,20,21 did not specify the age range and four studies12,16,20,21 did not specify the gender of patients in their studies. The Chelex extraction method was used to extract DNA from DBS in 3 studies (42.9%)12,16,20, whereas the 4 studies9,14,15,21 used a QIAamp DNA blood mini kit to extract DNA from whole blood (5/7, 71.4%). Six studies12,14,15,16,20,21 used nested PCR to amplify the malarial 18S rRNA gene in their studies, whereas only one study9 used nested PCR to amplify the malarial cytochrome b gene. In the present study, we attempted to perform subgroup analysis even though only a few included studies were selected to explore the association between the study characteristics and the primary outcome of this study.
Quality of included studies
All seven included studies were given scores of eight stars on the NOS based on their fit to the inclusion and exclusion criteria (Table 2).
Comparative performance of PCR using DNA extracted from DBSs and whole blood samples
Regarding the results of individual studies, two studies illustrated that DNA extracted from DBS had lower performance for detecting malaria parasites (OR 0.41, 95% CI 0.28–0.61; OR 0.86, 95% CI 0.77–0.96)12,21, whereas one study demonstrated that DNA from DBS had higher performance (OR 1.99, 95% CI 1.20–3.30)16. The pooled meta-analysis revealed no significant difference in the comparative performance of PCR for detecting malaria parasites between using DNA from DBS and whole blood (OR 0.85, 95% CI 0.62–1.16, P = 0.3). There was high heterogeneity among the included studies (I2 = 78%, P = 0.0001; Fig. 2).
Subgroup analysis
Subgroup analysis demonstrated that PCR using DNA extracted from DBS was lower in performance for detecting Plasmodium vivax than PCR using DNA extracted from whole blood (OR 0.85, 95% CI 0.77–0.94, P = 0.002). No difference was noted in the detection of P. falciparum or mixed infection between DBS and whole blood (Fig. 3).
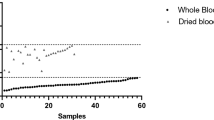
Publication bias
Publication bias was assessed in the present study using a funnel plot. The symmetry of the plot indicated that no publication bias was present (Fig. 4).
Discussion
In the present study, the performance of PCR using DNA from DBS and whole blood was compared. The results of the meta-analysis of 7 studies showed no difference in the detection of malaria parasites between the two blood samples for PCR analysis. As the results of the meta-analysis were heterogeneous, one-by-one or subgroup analysis was required to determine the sources of heterogeneity among the included studies. One by one interpretation of the included studies was performed. The study by Proux et al. showed that PCR using DNA extracted from DBS had a greater two-fold performance for detecting malarial parasites than PCR using DNA extracted from whole blood16. Although the study of Proux et al. indicated that DBS had greater sensitivity for detecting malaria parasites, the experiments were performed in different laboratories with different reagents, thermocyclers, and technicians16; therefore, the higher performance of PCR using DNA extracted from DBS than PCR using DNA extracted from whole blood requires further investigation. A study by Strom et al. has demonstrated the lower performance of PCR using DNA extracted from DBS than PCR using DNA extracted from whole blood12.
The subgroup analysis of this study demonstrated that PCR using DNA extracted from DBS provided a lower performance in detecting P. vivax than PCR using DNA extracted from whole blood, and no difference in performance for detecting P. falciparum or mixed infections was observed. Although no difference was demonstrated between the comparative performance of PCR using DNA extracted from DBS and PCR using DNA extracted from whole blood for detecting P. falciparum when using the results of the five included studies, the study by Strom et al. has demonstrated a lower performance of PCR using DNA extracted from DBS and suggested that the concentration of DNA in DBS was lower than that in whole blood, and PCR using DNA extracted from DBS missed 46.1% of P. falciparum infections12. For the performance of PCR in detecting P. vivax malaria, the result of the meta-analysis of four studies demonstrated that PCR had a lower efficiency using DNA extracted from DBS than PCR using DNA extracted from whole blood. In addition, no heterogeneity was observed among the four included studies, and therefore, the results of this analysis can be interpreted reliably. Among the four included studies, the study by Canier et al. has demonstrated that PCR using DBS missed 27% of malarial parasites, mostly P. vivax (84%)9. In addition, a study by Ataei et al. demonstrated that PCR using DBS missed only 10.3% of P. vivax infections14. Furthermore, a study by Zainabadi et al. indicated that PCR using DBS missed 10% of P. vivax infections and 25% of mixed infections21.
A previous study indicated that the lower performance of PCR using DBS compared to using whole blood might be attributable to the DNA extraction methods, the type of filter paper, amplification factors, and sample storage15,17,22. Only two included studies, namely those by Al-Harthi et al. and Taylor et al., used the same DNA extraction method for both DBS and whole blood15,20. The study by Al-Harthi et al. demonstrated that the DNA extracted using a commercial kit provided a higher quality of DNA than the conventional methanol fixation method15. Despite the use of the same DNA extraction method (QIAamp DNA blood mini kit), the sensitivity of PCR was lower for DBS (57.6%) than for whole blood (67%)15. The study by Taylor et al. used Chelex 100 (Sigma) for DNA extraction for both DBS and whole blood. However, they performed real-time PCR, which displayed higher sensitivity for malaria detection from DBS (74%) than from whole blood (69%)20. This study used different PCR conditions for the two sample types, including differences in the number of PCR cycles and cycle threshold to overcome the high background fluorescence of the filter paper20.
A study has demonstrated that DBS contained lower quantities of malarial DNA for amplification resulting in lower detection even after PCR, whereas whole blood samples contain robust quantities of malarial DNA for more successful DNA amplification regardless of the PCR method12,16. Therefore, the lower efficiency of PCR using DNA extracted from DBS for detecting P. vivax might be due to the low quantity and quality of DNA. Other factors that might contribute to the low performance of PCR using DNA extracted from DBS include, but not limited to, an extremely low level of parasitemia16, high temperature12, and humidity17,23, which might negatively influence the overall quality of DBS samples during storage. Relative to this, exploring and defining optimal storage protocols and conditions for DBS samples for improved recovery of malarial DNA using molecular methods seem beneficial. Despite the lower efficiency of PCR using DNA extracted from DBS, it allowed the detection of malarial parasites in several samples that were negative on microscopic examination. Moreover, DBS offers many advantages including the use of finger-prick sampling, long-term storage at room temperature, easy sample transport, and simple and rapid protocols for diagnostic purposes.
This study had some limitations. First, a small number of studies comparing PCR using whole blood with that using DBS were included in the analysis. Second, the included studies vary in the protocol of DNA extraction methods and PCR protocols and, therefore, might be the source of heterogeneity across the included studies. Third, as the results of the meta-analysis were heterogeneous, the comparative performance of PCR using DNA extracted from DBS compared with PCR using DNA extracted from whole blood must be interpreted carefully. In conclusion, the comparative performance of PCR using DNA extracted from DBS and PCR using DNA extracted from whole blood was significantly different in detecting P. vivax. Therefore, detecting P. vivax in endemic areas should be interpreted with care with PCR in cases where PCR using DNA extracted from DBS potentially gives a negative result. Further studies are required to improve the use of DBS for molecular methods possibly by defining the optimal storage protocols and conditions to protect the integrity of the low quantities of DNA. This will enhance the detection of P. vivax and other malarial parasites, which will be helpful in conducting studies and performing routine surveillance of malaria, especially with renewed efforts toward the eradication of the disease.
References
Mathison, B. A. & Pritt, B. S. Update on malaria diagnostics and test utilization. J. Clin. Microbiol. 55, 2009–2017. https://doi.org/10.1128/JCM.02562-16 (2017).
Moody, A. Rapid diagnostic tests for malaria parasites. Clin. Microbiol. Rev. 15, 66–78. https://doi.org/10.1128/cmr.15.1.66-78.2002 (2002).
Kotepui, M., Kotepui, K. U., De Jesus Milanez, G. & Masangkay, F. R. Summary of discordant results between rapid diagnosis tests, microscopy, and polymerase chain reaction for detecting Plasmodium mixed infection: A systematic review and meta-analysis. Sci. Rep. 10, 12765. https://doi.org/10.1038/s41598-020-69647-y (2020).
Humar, A., Ohrt, C., Harrington, M. A., Pillai, D. & Kain, K. C. Parasight F test compared with the polymerase chain reaction and microscopy for the diagnosis of Plasmodium falciparum malaria in travelers. Am. J. Trop. Med. Hyg. 56, 44–48. https://doi.org/10.4269/ajtmh.1997.56.44 (1997).
Berzosa, P. et al. Comparison of three diagnostic methods (microscopy, RDT, and PCR) for the detection of malaria parasites in representative samples from Equatorial Guinea. Malar. J. 17, 333. https://doi.org/10.1186/s12936-018-2481-4 (2018).
Agaba, B. B. et al. Systematic review of the status of pfhrp2 and pfhrp3 gene deletion, approaches and methods used for its estimation and reporting in Plasmodium falciparum populations in Africa: Review of published studies 2010–2019. Malar. J. 18, 355. https://doi.org/10.1186/s12936-019-2987-4 (2019).
Snounou, G. et al. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol. Biochem. Parasitol. 61, 315–320. https://doi.org/10.1016/0166-6851(93)90077-b (1993).
Rubio, J. M. et al. Semi-nested, multiplex polymerase chain reaction for detection of human malaria parasites and evidence of Plasmodium vivax infection in Equatorial Guinea. Am. J. Trop. Med. Hyg. 60, 183–187. https://doi.org/10.4269/ajtmh.1999.60.183 (1999).
Canier, L. et al. Malaria PCR detection in Cambodian low-transmission settings: Dried blood spots versus venous blood samples. Am. J. Trop. Med. Hyg. 92, 573–577. https://doi.org/10.4269/ajtmh.14-0614 (2015).
Mal, E. R. A research agenda for malaria eradication: Diagnoses and diagnostics. PLoS Med. 8, e1000396. https://doi.org/10.1371/journal.pmed.1000396 (2011).
Zimmerman, P. A. & Howes, R. E. Malaria diagnosis for malaria elimination. Curr. Opin. Infect. Dis. 28, 446–454. https://doi.org/10.1097/QCO.0000000000000191 (2015).
Strom, G. E., Moyo, S., Fataki, M., Langeland, N. & Blomberg, B. PCR targeting Plasmodium mitochondrial genome of DNA extracted from dried blood on filter paper compared to whole blood. Malar. J. 13, 137. https://doi.org/10.1186/1475-2875-13-137 (2014).
Canier, L. et al. An innovative tool for moving malaria PCR detection of parasite reservoir into the field. Malar. J. 12, 405. https://doi.org/10.1186/1475-2875-12-405 (2013).
Ataei, S., Nateghpour, M., Hajjaran, H., Edrissian, G. H. & Foroushani, A. R. High specificity of semi-nested multiplex PCR using dried blood spots on DNA banking card in comparison with frozen liquid blood for detection of Plasmodium falciparum and Plasmodium vivax. J. Clin. Lab. Anal. 25, 185–190. https://doi.org/10.1002/jcla.20454 (2011).
Al-Harthi, S. A. & Jamjoom, M. B. PCR assay in malaria diagnosis using filter paper samples from Jazan region Saudi Arabia. J. Egypt Soc. Parasitol. 38, 693–706 (2008).
Proux, S. et al. Considerations on the use of nucleic acid-based amplification for malaria parasite detection. Malar. J. https://doi.org/10.1186/1475-2875-10-323 (2011).
Farnert, A. et al. Sampling and storage of blood and the detection of malaria parasites by polymerase chain reaction. Trans. R. Soc. Trop. Med. Hyg. 93, 50–53. https://doi.org/10.1016/s0035-9203(99)90177-3 (1999).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6, e1000097. https://doi.org/10.1371/journal.pmed.1000097 (2009).
GA Wells, B. S., D O'Connell, J Peterson, V Welch, M Losos, P Tugwell. (Canada).
Taylor, B. J. et al. Real-time PCR detection of Plasmodium directly from whole blood and filter paper samples. Malar. J. https://doi.org/10.1186/1475-2875-10-244 (2011).
Zainabadi, K. et al. A novel method for extracting nucleic acids from dried blood spots for ultrasensitive detection of low-density Plasmodium falciparum and Plasmodium vivax infections. Malar. J. 16, 11. https://doi.org/10.1186/s12936-017-2025-3 (2017).
Brown, A. E., Kain, K. C., Pipithkul, J. & Webster, H. K. Demonstration by the polymerase chain reaction of mixed Plasmodium falciparum and P. vivax infections undetected by conventional microscopy. Trans. R. Soc. Trop. Med. Hyg. 86, 609–612. https://doi.org/10.1016/0035-9203(92)90147-5 (1992).
Färnert, A. et al. Sampling and storage of blood and the detection of malaria parasites by polymerase chain reaction. Trans. R. Soc. Trop. Med. Hyg. 93, 50–53. https://doi.org/10.1016/S0035-9203(99)90177-3 (1999).
Acknowledgements
The authors would like to thank Walailak University for supporting the funding for this study, the New Strategic Research (P2P) project.
Author information
Authors and Affiliations
Contributions
A.M., M.K. participated in the study design, data analysis, and writing of the paper. F.R.M., K.U.K., and G.D.M. participated in the writing of the paper. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahittikorn, A., Masangkay, F.R., Kotepui, K.U. et al. Comparative performance of PCR using DNA extracted from dried blood spots and whole blood samples for malaria diagnosis: a meta-analysis. Sci Rep 11, 4845 (2021). https://doi.org/10.1038/s41598-021-83977-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-83977-5
This article is cited by
-
Tenfold difference in DNA recovery rate: systematic comparison of whole blood vs. dried blood spot sample collection for malaria molecular surveillance
Malaria Journal (2022)
-
RNA purification-free detection of SARS-CoV-2 using reverse transcription loop-mediated isothermal amplification (RT-LAMP)
Tropical Medicine and Health (2022)
-
Feasibility of community at-home dried blood spot collection combined with pooled reverse transcription PCR as a viable and convenient method for malaria epidemiology studies
Malaria Journal (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.