Abstract
Locally applied vancomycin is increasingly being used in primary hip and knee arthroplasty to reduce the risk of infection. Despite encouraging initial results, considerable debate remains on the basis of the data currently available. In particular, it has been unclear up to now whether local vancomycin is suitable to further reduce the risk of infection even if the rate of infection is already low (< 1%). In this monocentric retrospective cohort study, all primary total hip and knee arthroplasties performed between 2013 and 2018 were included. After a change in procedure at the hospital, 1 g vancomycin powder was applied intraarticularly before wound closure. The remaining perioperative procedure was constant over the investigation period. The follow-up was one year. The presence of an infection according to the currently valid MSIS criteria was defined as the endpoint. In patients with TKA two infections (0.3%) were observed under vancomycin prophylaxis in contrast to 44 infections (1.3%) in the control group (p = 0.033). In patients with THA two infections (0.5%) were observed under vancomycin prophylaxis and 48 infections (1.1%) in the control group without local vancomycin but this difference was statistically not significant. No wound complications requiring revision were observed as a result of the vancomycin. On the basis of the results of this study, intraarticular application of vancomycin powder in total hip and knee arthroplasty may be considered. Prospective randomized studies have to confirm this promising results prior a common recommendation.
Level of Evidence III Retrospective cohort study.
Similar content being viewed by others
Introduction
Infections after endoprosthetic hip or knee replacement, in spite of all perioperative improvements, are observed with an incidence of 1–2%1,2,3,4. Despite the apparently low risk, efforts to further reduce the risk are sensible in light of the consequences for the patients concerned, with the potential for several follow-up operations and the often limited functional outcome.
In spinal surgery, the reduction in the rate of infection through locally applied vancomycin was established more than 10 years ago and has been well documented by meta-analyses and animal experiments5,6,7,8. The positive effect is set against minor complications caused in 0.3% of cases, mostly culture-negative seroma formation9, so that it is even used successfully in children10.
Otte et al. were able to show that intrawound vancomycin powder lowers the infection rate after knee and hip arthroplasty from 1.6 to 0.5%, compared with a control group11. In a subgroup analysis, the effect in revision operations was even greater, with a reduction of the infection rate from 3.9 to 0%. Patel et al. showed a reduction in the infection rate through vancomycin of 2.7–0.3% and determined a number needed to treat (NNT) of 47.512. Systemic side effects were not observed. The local application of vancomycin was assessed to be safe and cost-effective.
Dial et al. observed a similar effect in primary hip arthroplasty, with a lowering of the infection rate from 5.5% without vancomycin to 0.7% with intrawound vancomycin powder13. However, sterile wound complications were seen in 4.4% of the cases treated with vancomycin, compared with 0% in the control group. Hanada et al. had sterile wound complications in as many as 11.8% of cases after vancomycin, compared with 4.3% in the control group14. This paper failed to show a statistically significant advantage of the intraoperative administration of vancomycin, so that the authors did not recommend its use.
In a current meta-analysis, pooled data were used to demonstrate a significant reduction of the infection rate through locally applied vancomycin, with an odds ratio of 0.4415.
Also, in the implant-retaining treatment of early infection by irrigation, debridement and exchange of all modular components, it was shown that a combination of povidone-iodine and vancomycin increases the success rate of this procedure16.
In the studies that demonstrated a positive effect, however, the infection rate was between 1.6 and 5.5%, and was thus higher than the incidence of less than 1% described for many centers with optimized perioperative prophylaxis17,18,19,20,21. It is unclear whether locally applied vancomycin can also lower the risk of infection in an optimized setting with an already low infection rate.
Up to now, there has been a lack of monocentric studies with sufficiently high case numbers to demonstrate the efficacy of vancomycin when there is already a low infection rate of less than 1%. This requires considerably higher case numbers than those published to date, with constant perioperative management. Therefore, the hypothesis of the present study is that locally applied vancomycin can also further reduce an already low risk of infection.
Methods
This is a monocentric retrospective cohort study that is designed to investigate the effect of a change in the orthopaedic department’s practice, i.e., the intraoperative administration of 1 g intraarticular vancomycin powder in total hip and knee arthroplasty. It was not used selectively, so that an inclusion bias due to restricted use in specific indications could be excluded. The study was approved by the ethics committee of the University Hospital Jena (2019–1395). Resulting from the retrospective and anonymized study design, an informed consent was not necessary according to the ethics committee approval. All methods were carried out in accordance with the relevant guidelines and regulations based on the approval.
All primary total knee and hip arthroplasties performed between 2013 and 2018 due to primary or secondary osteoarthritis were included. Cases of postinfectious osteoarthritis as well as revision surgery were excluded, in order to prevent falsification through a potentially already existing infection or contamination.
The follow-up time was defined to one year for all patients. This was done to avoid higher infection rates in patients with a longer follow up resulting from bacteremia unrelated to the operation. The presence of an infection was defined as the endpoint. This was determined on the basis of the medical files of patients returning for follow-up examinations or readmissions within one year after operation at our hospital for any cause.
Except for the intraarticular application of vancomycin, the perioperative regimen was constant for the whole study period and did not differ between the two study groups.
All patients were washed with antiseptic (Stellisept, Hartmann, Heidenheim, Germany) one day before the operation. No preoperative instructions for bathing or at home cleansing process was used. This skin was not shaved, and hair was trimmed immediately prior to the operation only in the event of interfering hair growth (3M Surgical Clipper, Saint Paul, USA). Cutasept (Hartmann, Heidenheim, Germany), was used for disinfection. All total hip arthroplasties (THA) were covered with an iodine-impregnated incision drape (Ioban, 3M, Saint Paul, USA). In case of a known iodine allergy a drape without iodine was used. Total knee arthroplasties (TKA) were covered without a drape. Single shot antibiotic prophylaxis was applied 30 min prior to skin incision (2 g cefazolin). In case of an allergy, clindamycin was administered. If the operation lasted longer than 2 h, the antibiotic prophylaxis was repeated once.
Patients were included via a database search for procedures 5-820 (THA) and 5-822 (TKA) performed between 2013 and 2018. Surgery documentation revealed whether or not intraarticular vancomycin powder (1 g) was administered. A further database search identified all patients who were readmitted for any reason after prosthesis implantation. The records were screened for the presence of an implant associated infection. The diagnosis was confirmed according to the available microbiological laboratory findings and surgery reports on the basis of current MSIS criteria (Table 1)22.
In addition, noninfectious wound problems were recorded. Such a wound revision was recorded as a potential complication of vancomycin powder usage.
All infected cases were treated according to the latest guidelines of the Infectious Diseases Society of America (IDSA)23,24. The IDSA is a medical association of health care professionals who specialize in infectious diseases and recommend diagnosis and treatment algorithms based on the actual evidence.
Statistics
The group comparison was conducted with regard to the primary endpoint of infection using the chi-squared test, while all other demographic comparisons were tested for differences using the t-test. All statistical tests were conducted at a significance level of 0.05. A post-hoc power analysis was performed.
Results
Over 5 years, 8,945 joints were included in the study. Intraarticular vancomycin powder was used in 1,082 joints (432 THA, 650 TKA) and was not used in 7,863 joints (4,392 THA, 3,471 TKA). In no case was an aseptic wound revision performed related to the application of vancomycin powder.
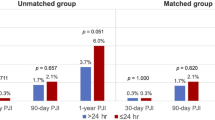
Regarding all total joint arthroplasties, four infections (0.4%) in the vancomycin group were observed in contrast to 92 infections in the control group without local vancomycin application (1.1%). This difference was statistically significant (p = 0.017, Table 2). Nine patients received a bilateral simultaneous procedure (4 THA and 5 TKA), all of them were in the control group without vancomycin and none of them was infected.
In patients with TKA two infections (0.3%) were observed under vancomycin prophylaxis in contrast to 44 infections (1.3%) in the control group (p = 0.033, Table 3). In patients with THA two infections (0.5%) were observed under vancomycin prophylaxis and 48 infections (1.1%) in the control group without local vancomycin but this difference was statistically not significant (p = 0.216, Table 4). Based on the numbers the statistical power of the Chi2 test was calculated to be higher than 99% for every test.
Staph. epidermidis and staph. aureus were the most common bacteria in both groups (Table 5). Patients’ body mass index and ASA scores did not differ between the groups (Table 6).
Discussion
The main result of the present study is that intraarticular vancomycin powder lowers the infection rate after total knee arthroplasty and possibly after total hip arthroplasty. At the same time, no local wound complications requiring revision were observed.
Both results contradict the data of Hanada et al., who observed local aseptic complications due to vancomycin powder without a reduction of the infection rate14. The infection rates of 7.6% (control group) and 4.5% (vancomycin group) described in this study are far higher than the 1–2% reported in the literature for primary arthroplasty. In addition, the number of cases is insufficient to exclude an effect of vancomycin, particularly since the infection rate in the vancomycin group is nominally lower than that in the control group.
The present study could be explained by the predominantly intraarticular application of vancomycin. The powder was placed in the joint before capsule closure and, after capsule closure, the powder adhering to the container was tapped into the subcutaneous tissue. Therefore, a high concentration of vancomycin was not to be expected in the immediate vicinity of the skin.
This is in line with a review of the use of vancomycin powder on the spine, which likewise did not detect an elevated rate of aseptic wound complications9.
An effect of vancomycin powder on wear in the sense of a potentially conceivable third-body wear was ruled out in vitro, so that long-term sequelae are improbable25.
Investigations after spinal operations on large patient populations show a concentration-dependent shift in the microbial spectrum in the case of an infection after application of intrawound vancomycin powder. Gram-negative bacteria were dominant in patients in whom 1 g vancomycin powder was used, whereas gram-positive bacteria were dominant in those in whom 2 g powder was used24. Even if the mechanism is unclear, a selective pressure of locally applied vancomycin cannot be ruled out.
The minimal inhibitory concentration of vancomycin on methicillin-resistant Staphylococcus aureus (MRSA), Staphylococcus epidermidis, Haemophilus influenzae, Pseudomonas aeruginosa, Burkholderia cepacia, and Escherichia coli was determined to be 1.6 µg/ml, so that 5 µg/ml were enough to kill all bacteria within one day after exposure in vitro26. This is supported by the guidelines of the infectious disease society of America, that recommend serum vancomycin concentrations > 10 µg/ml to avoid the development of resistance and 15–20 µg/ml for a sufficient treatment27. In vivo, 2 g of intrawound vancomycin powder resulted in wound concentrations of 207 µg/ml one day after operation26, so that therapeutic concentrations are to be expected even under unfavorable conditions. At the same time, a maximum serum concentration of less than 5 µg/ml is achieved 12 h after the operation, so that systemic side effects are unlikely28.
Vancomycin does not show any penetration of biofilm, so that it may only be used in prevention of infection or in combination with antibiotics that act against biofilm.
The main limitation of the present study is its retrospective study design, which, even if all potential influencing factors remain constant, cannot exclude unknown confounders. In addition, not all patients were systematically followed up with regard to the endpoint. Those patients who returned to follow-up or were readmitted at their own wish were evaluated according to the MSIS criteria on the basis of the available data. Therefore, it cannot be excluded that infected patients that regretted treatment in our hospital were not included in the analysis. However, it would appear plausible that the rate of such patients does not differ between the groups, so that the group differences and thus the conclusions remain unchanged.
The main advantage of the study, despite its monocentric design, is the high number of cases included in a short period of time, which potentially decreases the chance of confounding variables. In contrast to multicentric studies or investigations with a long inclusion period, this meant that influencing factors relevant to periprosthetic joint infection (preoperative antiseptic washing, use of drapes, clipping, type of single-shot prophylaxis and of antiseptic for washing, dressing, etc.) could be kept constant, so that the use of intraarticular vancomycin remains as the only variable.
Until data concerning the effect of vancomycin on cartilage are available, its use in unicompartmental knee arthroplasty or hemiarthroplasty of the hip must be viewed critically. None of the infected cases in the vancomycin group in our study showed resistance against vancomycin. Nevertheless it is worrying to use vancomycin as an antibiotic of last resort for infection prophylaxis. Local application of vancomycin in joints is not approved and therefore off-label. The patients should therefore sign an informed consent prior to operation.
On the basis of the results of the present study, intraarticular application of vancomycin powder in total hip and knee arthroplasty may be considered. Prospective randomized studies have to confirm this promising results prior a common recommendation.
References
Lindeque, B., Hartman, Z., Noshchenko, A. & Cruse, M. Infection after primary total hip arthroplasty. Orthopedics 37, 257–265 (2014).
Almustafa, M. A. et al. Risk factors for surgical site infection following lower limb arthroplasty: A retrospective cohort analysis of 3932 lower limb arthroplasty procedures in a high volume arthroplasty unit. J Arthroplasty 33, 1861–1867 (2018).
Saku, S. A., Madanat, R. & Mäkinen, T. J. Reasons and risk factors for ninety day re-admission following primary total knee arthroplasty in a high-volume centre. Int. Orthop. 42, 95–99 (2018).
Kurtz, S. M. et al. Are we winning or losing the battle with periprosthetic joint infection: Trends in periprosthetic joint infection and mortality risk for the medicare population. J. Arthroplasty. 33, 3238–3245 (2018).
Bakhsheshian, J., Dahdaleh, N. S., Lam, S. K., Savage, J. W. & Smith, Z. A. The use of vancomycin powder in modern spine surgery: Systematic review and meta-analysis of the clinical evidence. World Neurosurg. 83, 816–823 (2015).
Kang, D. G., Holekamp, T. F., Wagner, S. C. & Lehman, R. A. Intrasite vancomycin powder for the prevention of surgical site infection in spine surgery: A systematic literature review. Spine J. 15, 762–770 (2015).
Zebala, L. P. et al. Intrawound vancomycin powder eradicates surgical wound contamination: An in vivo rabbit study. J. Bone Joint Surg. Am. 96, 46–51 (2014).
Pahys, J. M. et al. Methods to decrease postoperative infections following posterior cervical spine surgery. J. Bone Joint Surg. Am. 95, 549–554 (2013).
Ghobrial, G. M., Cadotte, D. W., Williams, K., Fehlings, M. G. & Harrop, J. S. Complications from the use of intrawound vancomycin in lumbar spinal surgery: A systematic review. Neurosurg. Focus 39, E11 (2015).
Thompson, G. H., Poe-Kochert, C., Hardesty, C. K., Son-Hing, J. & Mistovich, R. J. Does vancomycin powder decrease surgical site infections in growing spine surgery? A preliminary study. J. Bone Joint Surg. Am. 100, 466–471 (2018).
Otte, J. E., Politi, J. R., Chambers, B. & Smith, C. A. Intrawound vancomycin powder reduces early prosthetic joint infections in revision hip and knee arthroplasty. Surg. Technol. Int. 30, 284–289 (2017).
Patel, N. N., Guild, G. N. & Kumar, A. R. Intrawound vancomycin in primary hip and knee arthroplasty: A safe and cost-effective means to decrease early periprosthetic joint infection. Arthroplast. Today 4, 479–483 (2018).
Dial, B. L., Lampley, A. J., Green, C. L. & Hallows, R. Intrawound vancomycin powder in primary total hip arthroplasty increases rate of sterile wound complications. Hip Pelvis. 30, 37–44 (2018).
Hanada, M. et al. Intrawound vancomycin powder increases post-operative wound complications and does not decrease periprosthetic joint infection in primary total and unicompartmental knee arthroplasties. Knee Surg Sports Traumatol. Arthrosc. https://doi.org/10.1007/s00167-019-05498-z (2019).
Heckmann, N. D. et al. Systematic review and meta-analysis of intrawound vancomycin in total hip and total knee arthroplasty: A call for a prospective randomized trial. J. Arthroplasty https://doi.org/10.1016/j.arth.2019.03.071 (2019).
Riesgo, A. M. et al. Vancomycin povidone-iodine protocol improves survivorship of periprosthetic joint infection treated with irrigation and debridement. J. Arthroplasty 33, 847–850 (2018).
Lee, Q. J., Mak, W. P. & Wong, Y. C. Risk factors for periprosthetic joint infection in total knee arthroplasty. J. Orthop. Surg. (Hong Kong) 23, 282–286 (2015).
Katz, J. N. et al. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am 83-A, 1622–1629 (2001).
Hijas-Gómez, A. I. et al. Surgical site infection incidence and risk factors in knee arthroplasty: A 9-year prospective cohort study at a university teaching hospital in Spain. Am. J. Infect. Control 46, 1335–1340 (2018).
Lamplot, J. D., Luther, G., Mawdsley, E. L., Luu, H. H. & Manning, D. Modified protocol decreases surgical site infections after total knee arthroplasty. J. Knee Surg. 28, 395–403 (2015).
Bullock, M. W. et al. A bundle protocol to reduce the incidence of periprosthetic joint infections after total joint arthroplasty: A single-center experience. J. Arthroplasty 32, 1067–1073 (2017).
Shohat, N. et al. Hip and knee section, what is the definition of a Periprosthetic Joint Infection (PJI) of the knee and the hip? Can the same criteria be used for both joints?: proceedings of international consensus on orthopedic infections. J. Arthroplasty 34, S325–S327 (2019).
Osmon, D. R. et al. Diagnosis and management of prosthetic joint infection: Clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect Dis. 56, e1–e25 (2013).
Anemüller, R. et al. Hip and knee section, treatment, antimicrobials: Proceedings of international consensus on orthopedic infections. J. Arthroplasty 34, S463–S475 (2019).
Qadir, R. et al. Establishing a role for vancomycin powder application for prosthetic joint infection prevention-results of a wear simulation study. J. Arthroplasty 29, 1449–1456 (2014).
Xie, L., Zhu, J., Luo, S., Xie, Y. & Pu, D. Do dose-dependent microbial changes occur during spine surgery as a result of applying intrawound vancomycin powder? A systematic literature review. Asian Spine J. 12, 162–170 (2018).
Rybak, M. J. et al. Vancomycin therapeutic guidelines: A summary of consensus recommendations from the infectious diseases Society of America, the American Society of Health-System Pharmacists, and the Society of Infectious Diseases Pharmacists. Clin. Infect. Dis. 49, 325–327 (2009).
Johnson, J. D. et al. Serum and wound vancomycin levels after intrawound administration in primary total joint arthroplasty. J. Arthroplasty 32, 924–928 (2017).
Acknowledgements
Open access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
G.M. wrote the main manuscript text; B.J. gathered the data of all patients; G.M., S.B. and E.R. operated most of the patients and reviewed every suspicious case for fulfilling MSIS criteria; S.B. and J.K. performed the statistics and critically reviewed and improved the text.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matziolis, G., Brodt, S., Böhle, S. et al. Intraarticular vancomycin powder is effective in preventing infections following total hip and knee arthroplasty. Sci Rep 10, 13053 (2020). https://doi.org/10.1038/s41598-020-69958-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-69958-0
This article is cited by
-
Prophylactic use of vancomycin powder on postoperative infection after total joint arthroplasty
BMC Musculoskeletal Disorders (2024)
-
Effects of different doses of vancomycin powder in total knee and hip arthroplasty on the periprosthetic joint infection rate: a systematic review and meta-analysis
Journal of Orthopaedic Surgery and Research (2022)
-
Topical vancomycin powder does not affect patella cartilage degeneration in primary total knee arthroplasty and conversion rate for secondary patella resurfacing
Archives of Orthopaedic and Trauma Surgery (2022)
-
Vancomycin-soaked femoral head allograft in opening wedge high tibia osteotomy enables earlier postoperative recovery and reduces infection rates compared to allogenic bone chips
Knee Surgery, Sports Traumatology, Arthroscopy (2022)
-
The bactericidal effect of vancomycin is not altered by tranexamic acid, adrenalin, dexamethasone, or lidocaine in vitro
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.