Abstract
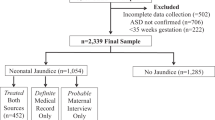
The aim of this study is to examine the clinical characteristics of children suspected to have neurodevelopmental disorders and to present features that could be helpful diagnostic clues at the clinical assessment stage. All children who visited the interdisciplinary clinic for developmental problems from May 2001 to December 2014 were eligible for this study. Medical records of the children were reviewed. A total of 1,877 children were enrolled in this study. Most children were classified into four major diagnostic groups: global developmental delay (GDD), autism spectrum disorder (ASD), developmental language disorder (DLD) and motor delay (MD). GDD was the most common (43.9%), and boys were significantly more predominant than girls in all groups. When evaluating the predictive power of numerous risk factors, the probability of GDD was lower than the probability of ASD among boys, while the probability of GDD increased as independent walking age increased. Compared with GDD and DLD, the probability of GDD was increased when there was neonatal history or when the independent walking age was late. Comparison of ASD and DLD showed that the probability of ASD decreased when a maternal history was present, whereas the probability of ASD increased with male gender. To conclude, the present study revealed the clinical features of children with various neurodevelopmental disorders. These results are expected to be helpful for more effectively flagging children with potential neurodevelopmental disorders in the clinical setting.
Similar content being viewed by others
Introduction
Developmental disabilities caused by dysfunction of the central nervous system, including the brain, are called neurodevelopmental disorders, and children with neurodevelopmental disorders have difficulties in various fields including physical, linguistic, behavior and learning1. According to a previous study conducted in the United States, 5–17% of children suffer from developmental disabilities, and recent trends have shown a gradual increase2. Limitations due to neurodevelopmental disorders might continue throughout life, and individuals with these disorders may require special services, health care and support3. These factors cause enormous social costs to a country as well as economic and psychological burdens for the families of children with developmental disabilities4.
The cause of neurodevelopmental disorders varies, and it is difficult to distinguish between children with neurodevelopmental disorders and typically developing children in early infancy. Even if the neurodevelopmental disorder is caused by nonprogressive factors, the clinical phenotype may change over time as the central nervous system matures5. Therefore, children’s symptoms are different according to their age and severity, and the necessary interventions will vary accordingly. As a result, the diagnosis of a neurodevelopmental disorder can vary greatly depending on the clinician’s perspective, and the treatment or intervention or social support offered may differ according to diagnosis. The time at which an expert is consulted varies widely from newborn to school-aged6. As shown in previous studies7,8, intervention during the period when the brain is developing rapidly can minimize disabilities and reduce the gap in developmental delay; as such, it is important to start precise intervention early. Neurodevelopmental disorders express various features, and the degree of influence by developmental domain varies from case to case. Because of the multi-morbidity feature, attempting to intervene by focusing on only one problem can lead to not only overlooking other accompanying problems but also a problem of inefficient use of limited intervention resources.
To compensate for difficulties in dealing with the complexity of neurodevelopmental disorders, an interdisciplinary clinic named the Developmental Delay Clinic (DDC) has been operating in our hospital. In this clinic, three specialists (a pediatric neurologist, pediatric physiatrist and pediatric psychologist) work together to provide comprehensive diagnoses and intervention plans. The three specialists, depending on area of expertise, each examine children, prescribe necessary tests, share and discuss the results of physical and neurological examinations and various tests and produce a precise diagnosis with a balanced intervention plan for each child. In this study, the authors aimed to identify meaningful factors for diagnosis and to determine if it is possible to distinguish major neurodevelopmental disorders at the clinical assessment stage.
Methods
Children who visited the DDC in our hospital with complaints of any developmental problems from May 2001 to December 2014 were included in this study. The total number of subjects was 1,877. Approval to perform this retrospective study was obtained from our Institutional Review Board (IRB) and research ethics committee (National Health Insurance Medical Center, NHIMC 2015-09-016). The need for informed consent was formally waived by the IRB and research ethics committee. All methods were performed in accordance with relevant guidelines and regulations.
All patients who visited the DDC for the first time had a history taken, and data were gathered according to the prescribed protocol. Data such as birth history, prenatal history, family history and other medical history were collected from a paper questionnaire. Birth history included intrauterine period and birth weight. Prenatal history included fetal distress, problems related to amniotic fluid or placenta, intrauterine growth retardation (IUGR), and fetal movement abnormality. Events such as fetal apnea, meconium aspiration and neonatal seizures were considered in the neonatal history. Postnatal history included infections such as sepsis, infantile spasm, and febrile convulsion. The presence of family history, such as language delay, autism spectrum disorder, and intellectual disability, and maternal history during the pregnancy period, such as anxiety or insomnia, depression, smoking and drinking, were also assessed in the survey.
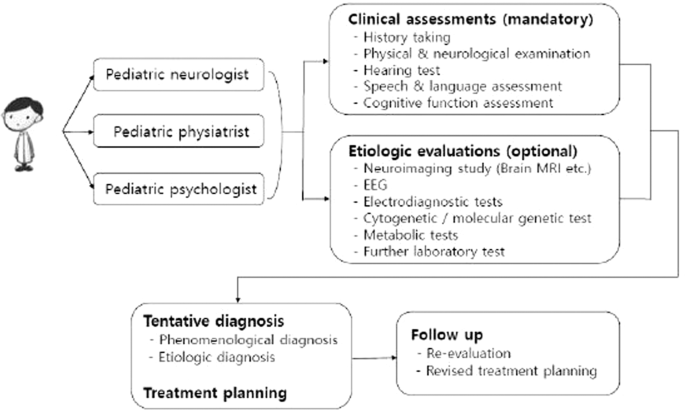
After assessing histories through the questionnaire, the three specialists examined the child and prescribed necessary tests according to protocol. The diagnostic protocol was composed of two categories: required tests applied to all children and selective tests applied to some patients who needed those tests, based on each specialist’s judgment9 (Fig. 1, Supplementary 1).
The diagnosis was determined by discussion among the three specialists in reference to each child’s clinical findings and standardized developmental assessment results. The diagnoses were divided into two categories: either a phenomenological diagnosis based on the child’s current condition or an etiological diagnosis based on the pathophysiology of the condition. All these phenomenological diagnoses were classified into four major groups according to the child’s main features: global developmental delay (GDD), autism spectrum disorder (ASD), developmental language disorder (DLD) and motor delay (MD). The GDD group included diagnoses such as GDD and intellectual disability. GDD refers to children with significant delays in more than two of the following developmental domains: gross motor/fine motor, speech/language, intelligence, social interaction and self-care. In general, children under five years of age who met the requirements were diagnosed with GDD, while older children who could be examined using a reliable and formal intelligence test were diagnosed with intellectual disability10. Diagnoses such as reactive attachment disorder and social communication disorder were included in the ASD group. Those in the ASD group were diagnosed based on diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV)11. However, since it has been updated from DSM-IV to DSM-V, the term ASD is used in this paper to prevent confusion. MD was defined as significant impairment of gross and/or fine-motor function compared with other developmental domains. Cerebral palsy and developmental coordination disorder were included in this group. DLD was defined as significant impairment of speech and language ability compared with other developmental domains. In this context, “significant” meant more than two standard deviations below the average value for the same age10. Etiological diagnoses included chromosomal and genetic anomalies, myopathy, and metabolic disease, among others.
Statistical analysis
SAS ver. 9.2 (SAS Institute, Cary, NC, USA) was used for statistical analysis. The results of the survey were obtained using the Kruskal-Wallis test with Bonferroni correction and logistic regression analysis. The level of significance was set at p < 0.05.
Results
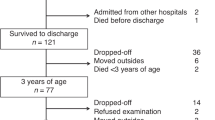
A total of 1,877 children were enrolled in this study. When divided into classes according to major phenomenological diagnosis, GDD accounted for the largest number, with 824 children (43.9%), followed by ASD with 430 (22.9%), DLD with 389 (20.7%) and MD with 72 (3.8%). Only 16 children (0.9%) were finally diagnosed as developing normally after all tests and examinations were given. Boys were more predominant than girls, with 1,316 (70.1%) and 561 (29.9%), respectively (p < 0.05). The age at which children visited the DDC ranged from 2 months to 192 months, and the average age was 50.9 ± 30.0 months. The corrected age was used for preterm children until they reached two years old. Two hundred thirty-four children (12.5%) out of the total could be diagnosed with an etiological diagnosis. Among these, hypoxic ischemic encephalopathy accounted for the largest number, with 58 children (24.8%), followed by chromosomal and/or genetic abnormalities with 53 children (22.6%) and congenital anomalies of the brain with 33 children (14.0%). Among the children who underwent a brain MRI, abnormal findings were mostly found in MD with 27.8%, which was significantly higher than ASD and DLD (p < 0.05) (Table 1).
With respect to preterm birth (gestational age less than 37 weeks), the history of preterm birth was the most prevalent in MD (29.2%), which was significantly higher than that in GDD (12.5%), ASD (10.9%) and DLD (8.7%) (p < 0.05). A history of low birth weight (LBW, birth weight less than 2,500 grams) was most common in MD (44.4%), which was significantly higher than that in ASD (20.9%) and DLD (25.4%) (p < 0.05) but not GDD (32.5%) (p = 0.426). Prenatal histories were most prevalent in MD (5.6%), which was significantly higher than in ASD and DLD (p < 0.05). Neonatal histories were also most prevalent in MD (29.2%), which was significantly higher than in the other three groups (p < 0.05). GDD and MD had a significantly higher prevalence of postnatal history compared with ASD and DLD (p < 0.05), but the difference between GDD and MD was not significant. Among family histories, language delay was the most common across all diagnosis groups, but the prevalence of having a family history did not differ significantly among the groups (p = 0.445). With regard to maternal histories, a maternal history of having anxiety or insomnia was the most common type in GDD, ASD and DLD, but drugs or drinking alcohol were the most common in MD. The percentage of cases with a maternal history did not differ significantly across the groups (p = 0.294) (Table 2).
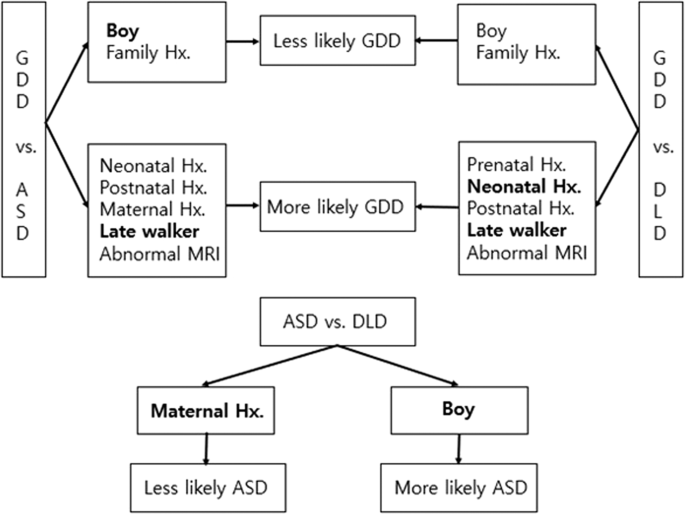
Among the various risk factors mentioned above, logistic regression analysis performed to compare the groups and to determine if certain risk factors contributed to being diagnosed with GDD, ASD and DLD. When comparing GDD with ASD, the risk of having GDD decreased with boys and the presence of family history, while the risk increased with the presence of neonatal, postnatal and maternal history, later independent walking age (a representation of delayed motor milestone) and abnormal findings in the brain MRI. After controlling for confounders, gender and independent walking age showed significant between-group differences. When comparing GDD with DLD, the risk of having GDD was lower in boys and with the presence of a family history, while the risk increased with presence of the prenatal, neonatal and postnatal history, later independent walking age and abnormal findings in the brain MRI. After controlling for confounders, neonatal history and independent walking age showed significant between-group differences. When comparing ASD with DLD, the risk of having ASD was higher in boys, while the risk decreased with the presence of maternal history. The results were the same after controlling for confounders (Table 3, Fig. 2).
When receiver operating characteristic (ROC) curve analysis was performed to confirm the predictive power of these models, the model comparison of GDD vs. ASD and the model comparison of GDD vs. DLD showed good predictive power, while the model comparison of ASD vs. DLD had poor predictive power. Hosmer and Lemeshow’s Goodness-of-Fit Test revealed that all three logistic regression models were fit to predict the risk factors (Table 4).
Discussion
The prevalence of developmental disabilities has risen in recent years with increases in high-risk pregnancies such as aged pregnancy, improved survival of high-risk infants due to medical technology advancement, and improved awareness and diagnosis of developmental disabilities2. The goal of early intervention for children with developmental disabilities is to prevent or minimize delays in all developmental domains, and early intervention allows children to achieve developmental milestones through the provision of enriched environments. Additionally, such interventions help caregivers cope efficiently with their children in daily life12. As seen in this study, the symptoms of children with neurodevelopmental disorders are very diverse, and the timing and symptoms of caregivers’ perception of something wrong in their children also vary. In addition, during the brain development period, one developmental domain affects the development of other domains, thus indicating multi-morbidity features. Proper intervention is important, but intervention is not always necessary. In some cases, it is more important to educate parents and modify the home environment than to use special resources. To effectively use limited resources, it is important to accurately diagnose neurodevelopmental disorders, which represent a multi-morbidity feature.
Among the patients who visited the DDC during the past 14 years, boys outnumbered girls in all diagnostic groups, which is consistent with previous studies2,13. Regarding etiological diagnosis, hypoxic ischemic encephalopathy was the most prevalent, followed by chromosomal and genetic abnormalities and congenital anomalies of the brain. These three factors accounted for 61.5% of the total etiologic causes. This outcome is similar to that of a study conducted by Shevell et al.14 indicating that four causes, i.e., the three causes mentioned above plus poisoning, accounted for 68.9% of total cases with a known etiological basis. There were no children with poisoning in the present study, which could be due to differences in socio-cultural backgrounds. However, more attention to antenatal poisoning might be needed, based on the recent increase in poisoning cases in Korea15.
In cases of preterm birth and LBW, which are known as the strongest risk factors for developmental disabilities16, a history of preterm birth was significantly more common in MD than in GDD, ASD and DLD. In contrast, a history of LBW was not significantly different between MD and GDD. It could be posited that the risk of GDD increased in cases of small for gestational age even in full-term births. Arcangeli et al.17 reported that compared with children of appropriate size for their gestational age, children who had a history of being small for their gestational age or who had fetal growth retardation, even in full-term births, showed lower neurodevelopmental scores. Takeuchi et al.18 reported that being small for gestational age is a risk factor for developmental disabilities, even in full-term babies. These results were consistent with the present study, and more attentive follow-up regarding developmental course is needed for children with a history of being small for gestational age.
Kumar et al.19 reported that the prevalence of neurodevelopmental disorders was higher in groups having family histories of neurodevelopmental disorders, such as epilepsy, GDD, MD, vision or hearing defects, compared with groups without such histories. Among the types of family histories, a history of language delay was seen the most in all diagnostic groups in this study. This finding could be explained by several factors: language delay is often present in various neurodevelopmental disorders, and the recognition and diagnosis of various neurodevelopmental disorders has improved in recent years, but this was not the case before. It may have been diagnosed as language delay13. In addition, it is possible that ASD has been diagnosed as other diseases, such as GDD or language delay, due to negative social perception of the diagnosis in Korea. Several studies have previously revealed that delay in one developmental domain often correlates with delay in other domains. Rechetnikov et al.20 stated that there was a correlation between motor impairment and speech and language disorder. Wang et al.21 reported that motor skill and communication skill were correlated with each other and that the motor skill of a one-and-a-half-year-old could predict the communication skill of a three-year-old. Language delay was predominant among the chief complaints of children who visited the DDC, but their final diagnosis was not limited to DLD. Shevell et al.22 reported that approximately three-quarters of children who were diagnosed with DLD before their fifth birthday showed some limitation of not only language but also communication, motor skill and social function at an early school age. Overall, the physicians would carefully assess all of the developmental domains, even if the chief complaints of parents were language delay, and would also give them a proper intervention plan focusing on the other domains.
This study has a few limitations. First, it is a single-center study, and most of the included children were from a metropolitan area in the Northern Gyeonggi territory. Second, children suspected to have cerebral palsy often visited the outpatient clinic of the rehabilitation department instead of the DDC for their initial evaluation, so the proportion of children with cerebral palsy was low in this study. Third, although the diagnosis may change over time, the study was conducted based on the initial diagnosis. Nevertheless, this study is meaningful in that it is the first study to present a probabilistic model in the clinical evaluation of children with suspected neurodevelopmental disorders. Several papers on the diagnosis of neurodevelopmental disorders that suggest diagnostic steps for GDD and ASD have been published thus far23,24,25,26,27. However, in contrast to the present study, there were no articles suggesting probabilistic models that included comprehensive history taking and clinical diagnosis. Additionally, most previous studies were confined to one diagnosis, such as cerebral palsy or intellectual disabilities, whereas this study represents the many children who visited interdisciplinary clinics for 14 years with various chief complaints about development.
In conclusion, the present study revealed the clinical characteristics of children who have developmental problems. In this study, we present a feature that can aid diagnosis in the stage of clinical evaluation for children with suspected neurodevelopmental disorders. These results are expected to be helpful for more effectively identifying children with potential neurodevelopmental disorders in the clinical setting.
References
Kaufmann, W. E., Capone, G. T., Carter, J. C., Lieberman, D. N. & Disability, G. I. Capute and Accardo’s Neurodevelopmental Disabilities in Infancy and Childhood. (Paul H. Brookes Publishing Company Baltimore, 2008).
Boyle, C. A. et al. Trends in the Prevalence of Developmental Disabilities in US Children, 1997–2008. Pediatrics 127, 1034–1042 (2011).
Boulet, S. L., Boyle, C. A. & Schieve, L. A. Health care use and health and functional impact of developmental disabilities among US children, 1997-2005. Arch. Pediatr. Adolesc. Med. 163, 19–26 (2009).
Anderson, D., Dumont, S., Jacobs, P. & Azzaria, L. The Personal Costs of Caring for a Child with a Disability: A Review of the Literature. Public Health Rep. 122, 3–16 (2007).
Kaplan, B. J., Dewey, D. M., Crawford, S. G. & Wilson, B. N. The Term Comorbidity Is of Questionable Value in Reference to Developmental Disorders: Data and Theory. J. Learn. Disabil. 34, 555–565 (2001).
Yeargin-Allsopp, M., Oakley, G. P., Murphy, C. C. & Sikes, R. K. A multiple-source method for studying the prevalence of developmental disabilities in children: the Metropolitan Atlanta Developmental Disabilities Study. Pediatrics 89, 624–630 (1992).
Morgan, C. et al. Effectiveness of motor interventions in infants with cerebral palsy: a systematic review. Dev. Med. Child Neurol. 58, 900–909 (2016).
Zwaigenbaum, L. et al. Early Intervention for Children With Autism Spectrum Disorder Under 3 Years of Age: Recommendations for Practice and Research. Pediatrics 136, S60–S81 (2015).
Kim, S. W. et al. Diagnosis and Clinical Features in Children Referred to Developmental Delay Clinic. J. Korean Acad. Rehabil. Med. 28, 132–139 (2004).
Shevell, M. I. et al. Practice parameter: evaluation of the child with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and The Practice Committee of the Child Neurology Society. Neurology 60, 367–380 (2003).
Segal, D. L. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). In The Corsini Encyclopedia of Psychology 1–3, https://doi.org/10.1002/9780470479216.corpsy0271 (American Cancer Society, 2010).
Majnemer, A. Benefits of early intervention for children with developmental disabilities. Semin. Pediatr. Neurol. 5, 62–69 (1998).
Baio, J. Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators; Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill. Summ. 63, 1–21 (2014).
Shevell, M. I., Majnemer, A., Rosenbaum, P. & Abrahamowicz, M. Etiologic yield of subspecialists’ evaluation of young children with global developmental delay. J. Pediatr. 136, 593–598 (2000).
Yoon, M. S. The current situation and developmental direction of Korean addiction service delivery system. Ment Health Soc Work 35, 234–266 (2010).
Salas, A. A. et al. Gestational age and birthweight for risk assessment of neurodevelopmental impairment or death in extremely preterm infants. Arch. Dis. Child.-Fetal Neonatal Ed. 101, F494–F501 (2016).
Arcangeli, T., Thilaganathan, B., Hooper, R., Khan, K. S. & Bhide, A. Neurodevelopmental delay in small babies at term: a systematic review. Ultrasound Obstet. Gynecol. 40, 267–275 (2012).
Takeuchi, A. et al. Neurodevelopment in full-term small for gestational age infants: A nationwide Japanese population-based study. Brain Dev. 38, 529–537 (2016).
Kumar, R., Bhave, A., Bhargava, R. & Agarwal, G. G. Prevalence and risk factors for neurological disorders in children aged 6 months to 2 years in northern India. Dev. Med. Child Neurol. 55, 348–356 (2013).
Rechetnikov, R. P. & Maitra, K. Motor impairments in children associated with impairments of speech or language: A meta-analytic review of research literature. Am. J. Occup. Ther. 63, 255–263 (2009).
Wang, M. V., Lekhal, R., Aarø, L. E. & Schjølberg, S. Co-occurring development of early childhood communication and motor skills: results from a population-based longitudinal study. Child Care Health Dev. 40, 77–84 (2014).
Shevell, M. I., Majnemer, A., Webster, R. I., Platt, R. W. & Birnbaum, R. Outcomes at school age of preschool children with developmental language impairment. Pediatr. Neurol. 32, 264–269 (2005).
Moeschler, J. B. & Shevell, M. Clinical genetic evaluation of the child with mental retardation or developmental delays. Pediatrics 117, 2304–2316 (2006).
Moeschler, J. B. & Shevell, M. Comprehensive evaluation of the child with intellectual disability or global developmental delays. Pediatrics 134, e903–e918 (2014).
Bélanger, S. A. & Caron, J. Evaluation of the child with global developmental delay and intellectual disability. Paediatr. Child Health 23, 403–410 (2018).
Charman, T. & Gotham, K. Measurement Issues: Screening and diagnostic instruments for autism spectrum disorders–lessons from research and practise. Child Adolesc. Ment. Health 18, 52–63 (2013).
Charman, T. & Baird, G. Practitioner review: Diagnosis of autism spectrum disorder in 2-and 3-year-old children. J. Child Psychol. Psychiatry 43, 289–305 (2002).
Author information
Authors and Affiliations
Contributions
S.W., H.J. and J.-E. conceived of the presented concept and revised the article. J.K. and H.R. developed the theory, interpreted of data and drafted the article. J.A. collected and analyzed the data and drafted the article. All authors discussed the results and contributed to the final manuscript and had complete access to the study data that support the publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, S.W., Jeon, H.R., Jung, H.J. et al. Clinical Characteristics of Developmentally Delayed Children based on Interdisciplinary Evaluation. Sci Rep 10, 8148 (2020). https://doi.org/10.1038/s41598-020-64875-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64875-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.