Abstract
In the present study, we aimed to evaluate the prevalence of dyslipidemia in students from different ethnic groups in Xinjiang. It is an observational, cross-sectional study. The sample of 7096 students aged 21–25 years was randomly selected from the clinic of Xinjiang Medical University. Baseline data, serum concentration of total cholesterol (TC), triglyceride (TG), low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C) and fasting plasma glucose (FPG) were reported. The prevalence of changes in lipid profile according to Body mass index (BMI) in three ethnic groups was calculated. Compared with Han and Uygur students, TC, LDL-C, TG and FPG levels were lower in kazakh sutdents, while HDL-C level was lower in Uygur students. The prevalence of high TC change was higher in Uygur students, and high LDL-C change was higher in Han students. The prevalence of low HDL-C change was higher in Uygur students, and high TG change was lower in Kazakh students. The prevalence of high TC, LDL-C, TG and low HDL-C changes was observed in normal weight, overweight and obesity groups according to the nutritional status by BMI among students of each ethnic group. The present study demonstrated the prevalence of dyslipidemia in students from different ethnic groups, and enriched the limited data on the early prevention and treatment of dyslipidemia and cardiovascular diseases in Xinjiang medical students crowd.
Similar content being viewed by others
Introduction
Atherosclerosis is as a result of pathological accumulation of plaque in the arterial vessels and leads to cardiovascular disease, the main cause of death in the worldwide1. It is well known that atherosclerotic process begins early in childhood and dyslipidemia plays a vital role in the progression of the disease2. Dyslipidemia is a family of lipoprotein metabolism disorders manifested by elevated total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), and reduced high density lipoprotein cholesterol (HDL-C) concentrations in the blood3. Increased lipid levels result in vessel wall reations, including endothelial dysfunction, smooth muscle cells proliferation, lipid accumulation, foam cell formation, and, finally, necrosis and plaque development4,5. Like other well-known risk factors such as diabetes, hypertention, obesity and smoking, dyslipidemia is also associated with the development of atherosclerotic disease6,7,8. Studies revealed that early onset of dyslipidemia is associated with the development of early atherosclerotic coronary and peripheral artery disease and increased incidence of cardiovascular disease in adulthood9,10.
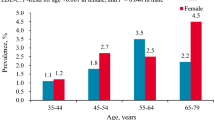
Recently, dyslipidemia is increasingly prevalent in all age groups, and the incidence tends to be younger11. In the last decade, Diseases caused by high total cholesterol (TC) increased global morbidity and mortality by 26.9% and 28.0%, respectively12,13. Bogalusa Heart Study reported that more than 70% of children with adverse lipid profiles are prone to dyslipidemia in adult life14. A study conducted on individuals from two regions of Argentina, aged 7–14 years old, revealed the prevalence of high TG was 28.8% and 3.5% and low HDL was 30% and 5.5%15. Another study on the Korean students aged 10–18 years old, indicated that the morbidity of dyslipidemia in girls and boys was 21.7% and 25.2%, respectively16. Greek school-aged boys were found to have higher mean of TC (5.8 mg/dL) and TG (10.8 mg/dL), and lower mean of HDL-C (−16.9 mg/dL)17. Identification and prevention of dyslipidemia at the young age is an important strategy to reduce present and future health risks.
Epidemiologic surveys of cardiovascular disease (CVD) precursors in children have showed that differences in lipid and lipoprotein levels among cultures and ethnic groups occur early in childhood18,19. Further, we assumed that college students are not as disrupted by environmental factors as adults, and genetic factors may be considered as the main influencing factors of dyslipidemia. In the present study, we aimed to establish the prevalence of dyslipidemia in college students from different ethnic groups and to evaluate its association with the nutritional status.
Methods
This is an observational, cross-sectional study, and the sample was obtained from students who were seen at the clinic of the Xinjiang Medical University from September 2018 to December 2018, consisting of Han, Uygur, and Kazakh students aged between 21 and 25, of both genders. Trained research interviewers administered standardized questionnaire through in-person interviews. Data collection involved demographic information, dietary habit, physical activity, and medical historty. Anthropometric measures (e.g. height, weight, and blood pressure) were performed according to a standard protocol. Blood samples were obtained from an antecubital vein into vacutainer tubes containing EDTA in the morning after an overnight fasting period. All the collected samples were transported on dry ice at prearranged intervals to Xinjiang coronary artery disease VIP laboratory. The concentration of serum total cholesterol, triglyceride, low density lipoprotein (LDL), high density lipoprotein (HDL) and fasting glucose were measured by the Clinical Laboratory Department of the First Affiliated Hospital of Xinjiang Medical University with the biochemical analyzer (Dimension AR/AVL Clinical Chemistry System, Newark, NJ, USA). Each participant was informed and signed a written consent. The survey protocol abided the ethical guidelines of the 1975 declaration of Helsinki20,21.
The 2016 Chinese Guideline for the Management of Dyslipidemia in Adults (Chinese guideline) was used to classify the serum TC, LDL-C, HDL-C, and TG levels22. These classifications defined by Chinese guideline were the same with the criteria in the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report (NCEP-ATP III)23. High TC was defined as TC ≥ 6.22 mmol/L. High LDL-C was defined as LDL-C ≥ 4.14 mmol/L. Low HDL-C was defined as HDL-C ≤ 1.04 mmol/L, and high TG was defined as TG ≥ 2.26 mmol/L. Body mass index (BMI, kg/m2) was calculated from the height and weight measurements. Based on the Criteria of Weight for Adults released by the Ministry of Health of China (WS/T 428–2013), individuals were categorized into three groups: 18.5 kg/m2 ≤BMI< 24.0 kg/m2 (normal weight), 24.0 kg/m2 ≤BMI < 28.0 kg/m2 (over weight), and BMI ≥ 28.0 kg/m2 (obesity)21.
Exclusion criteria included (1) no blood samples available; (2) missing data on lipid concentrations; (3) ethnic groups other than Han, Uygur and Kazakh; (4) known familial hypercholesterolemia; (5) use of cholesterol-lowering medications; (6) age younger than 21 years and older than 25 years. A total of 7096 students were finally enrolled in the present study.
Statistical analysis
The analysis was performed using SPSS 22 software. The continuous variables were presented as mean and standard deviation and the categorical variables as absolute frequency. The distribution of variables was assessed using the Kolgomorov-Sminorv test. The comparisons of the continuous variables with normal distribution were performed with the unpaired Student’s t-test, and for more than two independent groups, one way variance analysis (ANOVA) was used. Following the the ANOVA with statistically significant results, post hoc Tukey comparisons were performed, and all p-values were adjusted. For the comparisons of categorical variables, the chi-square test or Fisher’s exact test was used. For the study of the association, multiple linear regression were performed. P value < 0.05 was considered statistically significant.
Ethics approval and consent to participate
The study was approved by the Ethical Review Board of The First Affiliated Hospital of Xinjiang Medical University. Written informed consent was obtained from all enrolled patients.
Results
Baseline characteristics and the mean values of lipid profile of the population enrolled according to ethnic groups were listed in Table 1. A total of 7096 students from three ethnic groups with a mean age of 21.26 ± 1.64 years were participated in this project, and 2451(34.5%) of them were male. Compared with Han and Kazakh students, the average height and weight of Uygur students were lower. BMI values were higher in Han students than other two groups, while blood pressure was lower in Uygur students than others. TC, LDL-C, TG and FPG levels were lower in Kazakh students than other two groups, and HDL-C levels were lower in Uygur students than Han and Kazakh students (all P < 0.05, Table 1).
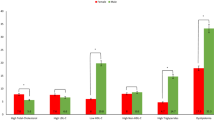
Regarding the prevalence of lipid profile changes, according to different ethnic groups, it was observed the prevalence of high TC change was higher in Uygur students, but the difference was not statistically significant (P = 0.8, Table 2). The prevalence of high LDL-C change was significantly higher in Han students (P = 0.003, Table 2), and the prevalence of low HDL-C change was significantly higher in Uygur students (P < 0.001, Table 2). Meanwhile, the prevalence of high TG change was significantly lower in Kazakh students (P < 0.001, Table 2).
The prevalence of changes in lipid profile according to the nutritional status by BMI in three ethnic groups was listed in Tables 3–5. In Han students, It was observed that the prevalence of high TC, LDL-C and low HDL-C change was higher in obese students, while prevalence of high TG change was higher in normal weight students, but the differences were not statistically significant. (Table 3). In Uygur students, the higher prevalence of high TC, LDL-C and low HDL-C change was observed in overweight students, and high TG change in normal weight students, but the differences were not statistically significant (Table 4). However, in Kazakh students, the higher prevalence of low HDL-C change was mainly concentrated in obese students (P < 0.001, Table 5). The prevalence of high TC change was higher in normal weight students, while the prevalence of high LDL-C and high TG change were higher in obese students, but there were also not statistically significant differences (Table 5).
For all the varabiles, multiple linear regression analysis, according to different ethnic groups, was performed to estimate the risk factors of BMI. The results revealed that, in Han students (R2 = 0.310), Age (β = −0.036, P = 0.013), Sex (β = −0.066, P < 0.001), HDL-C (β = −0.242, P < 0.001), LDL-C (β = 0.174, P = 0.018), TG (β = 0.138, P < 0.001), FPG (β = 0.031, P = 0.038), SBP (β = 0.127, P < 0.001) and DBP (β = 0.098, P < 0.001) were the independent risk factors of BMI (Table 6). In Uygur students (R2 = 0.269), Sex (β = −0.092, P < 0.001), TC (β = −0.328, P = 0.004), LDL-C (β = 0.466, P < 0.001), TG (β = 0.159, P < 0.001), SBP (β = 0.099, P < 0.001) and DBP (β = 0.119, P < 0.001) were the independent risk factors of BMI (Table 7). In Kazakh students (R2 = 0.230), only Sex (β = −0.145, P < 0.001), TG (β = 0.117, P = 0.012) and DBP (β = 0.148, P = 0.011) were the independent risk factors of BMI (Table 8).
Discussion
It is well known that lipid disorders in children and adolescents are associated with increased risks of cardiovascular and cerebrovascular disease in adults24. Hence, for improving cardiovascular health in adulthood, dyslipidemia in children and adolescents should be screened early25. Studies reported that lipid metabolism disorders, such as high LDL-C and low HDL-C, in children could be used as the main predictors of future atherosclerosis26. A study on Spanish children showed that the reduced mortality from ischemic cardiac disease in children may be associated with elevated HDL-C levels compared with other developed countries27. Therefore, dyslipidemia in adolescents or children should be taken attention.
Previous studies on lipidomics reported that there are differences between races in lipid levels. The Bogalusa Heart Study reported that the black children had higher mean levels of TC, LDL-C and HDL-C than white children did28. The NHANES III data showed that, compared with non-Hispanic white and Mexican Americans’, the TC, LDL-C, and HDL-C levels were higher in non-Hispanic black children and adolescents29,30. Xinjiang locates in the northwest of China, where the main ethnic groups are Han, Uygur and Kazakh. Since the geographical location, living environment and ethnic categories of Xinjiang province are different from other parts of China, the life styles of the people are also quite different. As the most Kazakh people lead nomadic lives, the consumption of beef, mutton and dairy products is much higher than others. Uygur people are mainly based on agriculture, the levels of pasta and meat consumption are higher than Han people. Furthermore, Xinjiang is defined as the area of high incidence of cardiovascular diseases in China31.
In present study, we analyzed serum concentrations of TC, LDL-C, HDL-C, and TG in students from Han, Uygur and Kazakh ethnic groups, and evaluated the association of overweight and obesity with these variables. Our study showed that although there were significant differences in LDL-C, HDL-C and TG among the three groups, the difference was not significant in TC. For LDL-C levels, Kazakh students had obviously lower values than other two groups, while Uygur students had apparently high HDL-C lowering values. Han students had the highest values of TG among the three groups. Besides of the ethnic factor, the main reason of these differences may be life style, Uygurs and kazakhs consume more pasta, meat and dairy products than Han do, which are higher in saturated and trans fats. This may suggest that, in Xinjiang, the prevalence of dyslipidemia among these ethnic groups has been different since adolescence even childhood. Nevertheless, We have found that although the differences in mean values between the three groups are small, the statistical analysis is still significant even after adjustment for multiple comparisons. This is probably an effect of the large sample size.
Obesity is not only a disease itself, but also a risk factor for other diseases. It is an increasingly serious global problem32. In the Europe, 30–40% of children between the ages of 6 and 10 are overweight (including overweight and obesity)24, and up to 43% of American children and adolescents with overweight/obesity diagnosed as dyslipidemia25. Similarly, obesity persists into adulthood, and is positively correlated with a lot of diseases, including hypertension, diabetes, dyslipidemia, insulin resistance (IR), and atherosclerosis33,34. Obesity rates are still rising rapidly in many parts of the world, and if current trends continue, they will reach 18% of men and more than 21% of women globally by 2025, placing a heavy burden on individuals, societies and health care systems35. Consequently, unless prevented or treated promptly, this risk factor is maintained throughout early adulthood, suggesting the need for early preventive intervention.
When analyzing lipid profile of each ethnic group students according to the nutritional status by BMI, in Han students, the prevalence of high TC, LDL-C, low HDL-C was concentrated in the obese group and high TG in the normal weight group. In Uygur students, the overweight group had the higher prevalence of high TC, LDL-C, and low HDL-C than other groups did, while the normal weight group had the highest prevalence of high TG. In Kazakh students, the prevalence of high LDL-C, TG and low HDL-C was observed in the obese group, and high TC was in the normal weight group. This may indicate a high incidence of dyslipidemia in Kazakh populations, even if they are not overweight or obese. Besides of the ethnic difference and life styles, genetic factors that mediate the levels of lipid proteins may play a role in the synthesis of serum lipid.
The main strength of the study was a large cohort of healthy students from different ethnic groups. We compared the blood lipid levels of medical students from three different ethnic groups and laid the foundation for preliminarily evaluating the distribution of abnormal blood lipid in these ethnic groups. In addition, the cohort of overweight/obese students was collected during the same period, which provided information on the effect of obesity on lipid concentration, thus clarifying the health-related effects of obesity on human metabolism in early childhood. Therefore, our results support the development of early prevention strategies for cardiovascular disease in this region. The limitation of this study is its observational, cross-sectional sample population, and our sample is from students at Xinjiang Medical University. Although these students come from all parts of Xinjiang, they could not represent the young population of Xinjiang. Further researches could utilize the results suggested in this article to study the associated risk factors and intervention of overweight and obesity in a representative sample of the adult population.
In conclusion, this study demonstrated the prevalence of dyslipidemia in different ethnic group students. The continuous relation between cardiovascular disease risk factors and dyslipidemia were documented. This study enriched the limited data on the early prevention and treatment of dyslipidemia and cardiovascular diseases in Xinjiang medical students crowd.
Data availability
The data will not be shared, since part of the data is being reused by another study.
References
Tabas, I., García, C. G. & Owens, G. K. Recent insights into the cellular biology of atherosclerosis. Cell Biol 209, 13–22 (2015).
McGill, H. C. et al. Origin of atherosclerosis in childhood and adolescence. Am. J. Clin. Nutr 72, 1307S–1315S (2000).
Perk, J. et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Atherosclerosis 223, 1–68 (2012).
Nomikos, T. et al. Hierarchical modelling of blood lipids’ profile and 10-year (2002-2012) all cause mortality and incidence of cardiovascular disease: the ATTICA study. Lipids Health Dis 14, 108 (2015).
Kavey, R. E. W. et al. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation 107, 1562–6 (2003).
Bayer, O. et al. Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity (Silver Spring) 19, 1069–76 (2011).
Joshi, S. M. et al. Tracking of cardiovascular risk factors from childhood to young adulthood-the Pune Children’s Study. Int. J. Cardiol 175, 176–8 (2014).
Lauer, R. M., Lee, J. & Clarke, W. R. Factors affecting the relationship between childhood and adult cholesterol levels: the Muscatine Study. Pediatrics 82, 309–18 (1988).
De, W. J. A., Middelkoop, B. & Verkerk, P. H. Tracking of thinness and overweight in children of Dutch, Turkish, Moroccan and South Asian descent from 3 through 15 years of age: a historical cohort study. Int J Obes (Lond) 42, 1230–1238 (2018).
Schmidt, M. D. et al. Predictive associations between alternative measures of childhood adiposity and adult cardio-metabolic health. Int J Obes (Lond) 35, 38–45 (2011).
Dowla, S. et al. Dyslipidemia is associated with pediatric nonalcoholic fatty liver disease. J Clin Lipidol 12, 981–987 (2018).
GBD 2015 Risk Factors Collaborators, Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659-1724 (2016).
Moon, S. et al. Association between serum selenium level and the prevalence of diabetes mellitus in U.S. population. J Trace Elem Med Biol 52, 83–88 (2019).
Nicklas, T. A., von, D. S. P. & Berenson, G. S. Tracking of serum lipids and lipoproteins from childhood to dyslipidemia in adults: the Bogalusa Heart Study. Int J Sports Med null, S39–43 (2002).
Hirschler, V. et al. Dyslipidemia without obesity in indigenous Argentinean children living at high altitude. Pediatr 161, 646–51 (2012).
Kim, C. J., Park, J. & Kang, S. W. Health-promoting lifestyles and cardio-metabolic risk factors among international students in South Korea. Collegian 22, 215–23 (2015).
Pan, W. H. et al. Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: implications for definitions of overweight and obesity for Asians. Am. J. Clin. Nutr 79, 31–9 (2004).
Deurenberg, P., Deurenberg, Y. M. & Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev 3, 141–6 (2002).
Wulan, S. N., Westerterp, K. R. & Plasqui, G. Ethnic differences in body composition and the associated metabolic profile: a comparative study between Asians and Caucasians. Maturitas 65, 315–9 (2010).
Pan, S. et al. Appropriate body mass index and waist circumference cutoffs for categorization of overweight and central adiposity among Uighur adults in Xinjiang. PLoS One 8, e80185 (2013).
Ma, J. Y. et al. Association between urinary polycyclic aromatic hydrocarbon metabolites and dyslipidemias in the Chinese general population: A cross-sectional study. Environ Pollut 245, 89–97 (2019).
Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol 15, 1–29 (2018).
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285, 2486–97 (2001).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
Suomela, E. et al. Childhood predictors of adult fatty liver. The Cardiovascular Risk in Young Finns Study. Hepatol 65, 784–790 (2016).
Sekine, M. et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health Dev 28, 163–70 (2002).
Golley, R. K. et al. Australasian nutrition research for prevention and management of child obesity: innovation and progress in the last decade. Pediatr Obes 9, e132–6 (2014).
Li, S. et al. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am. J. Epidemiol null, S142–9 (2012).
Kim, H., Hu, E. A. & Rebholz, C. M. Ultra-processed food intake and mortality in the USA: results from the Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994). Public Health Nutr null, 1–9 (2019).
Malandrino, N. et al. Cognitive Function in Individuals with Normal Weight Obesity: Results from the Third National Health and Nutrition Examination Survey (NHANES III). J. Alzheimers Dis 65, 125–135 (2018).
Yang, W. et al. Comparison Between Metabolic Syndrome and the Framingham Risk Score as Predictors of Cardiovascular Diseases Among Kazakhs in Xinjiang. Sci Rep 8, 16474 (2018).
Peters, S. A. E. & Muntner, P. W. M. Sex Differences in the Prevalence of, and Trends in, Cardiovascular Risk Factors, Treatment, and Control in the United States, 2001 to 2016. Circulation 139, 1025–1035 (2019).
Nooyens, A. C. J. et al. Adolescent skinfold thickness is a better predictor of high body fatness in adults than is body mass index: the Amsterdam Growth and Health Longitudinal Study. Am. J. Clin. Nutr 85, 1533–9 (2007).
Currie, C. et al. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med 66, 1429–36 (2008).
Rosário, R. et al. The impact of an intervention taught by trained teachers on childhood overweight. Int J Environ Res Public Health 9, 1355–67 (2012).
Acknowledgements
We thank all students for participating in this study. We are also grateful to the clinic of the Xinjiang Medical University. This work was supported financially by The science and technology support project Xinjiang Uygur Autonomous Region (2017E0269).
Author information
Authors and Affiliations
Contributions
J.A., Y.W. and Z.F. conceived and designed the experiments, and wrote the draft of the manuscript; F.L. and B.C. collected data and undertook the statistical analyses; J.A., Y.W., D.A., F.L. and B.C. performed laboratory experiments; Y.M., Y.Y., X.M. and X.L. gave critical comments on the draft and contributed to the manuscript writing; J.A., Y.W. and D.A. reviewed clinical assessments in this study and supervised this study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abuzhalihan, J., Wang, YT., Adi, D. et al. Prevalence of Dyslipidemia in Students from Han, Uygur, and Kazakh Ethnic Groups in a Medical University in Xinjiang, China. Sci Rep 9, 19475 (2019). https://doi.org/10.1038/s41598-019-55480-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-55480-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.