Abstract
This study aimed to investigate the prevalence of dyslipidemia and its related factors among urban adults aged 35 to 79 years in Southwestern China. From September 2013 to March 2014, a multi-stage sampling was conducted, and a total of 10,221 people aged 35–79 years living in Chengdu and Chongqing were included. More than 30 investigators were trained in data collection, including questionnaire, anthropometric measurements and blood biomarkers testing. The prevalence of high triglycerides (≥ 2.3 mmol/L), high total cholesterol (≥ 6.2 mmol/L), high low-density lipoprotein cholesterol (≥ 4.1 mmol/L), low high-density lipoprotein cholesterol (< 1.0 mmol/L), and dyslipidemia were 15.7% (95% confidence interval, 15.0–16.4%), 5.4% (4.9–5.8%), 2.5% (2.2–2.8%), 5.7% (5.3–6.2%), and 27.4% (26.5–28.2%), respectively. The prevalence of dyslipidemia was positively correlated with higher education level, monthly income over 2000 CNY, smoking, hypertension, diabetes, overweight and obesity, and central obesity, and negatively correlated with daily physical exercise. The prevalence of dyslipidemia in Southwestern China is lower than the national average level, with high triglycerides being the most common form of dyslipidemia.
Similar content being viewed by others
Introduction
Arteriosclerotic cardiovascular disease (ASCVD) is the leading cause of death in both developed countries1,2 and most developing countries, including China3. The 2007 overall death rate2 from CVD was 251.2 per 100,000 in the United States. Dyslipidemia is one of the most important risk factors for ASCVD4, leading to atherosclerosis5 and increased morbidity and mortality from coronary heart disease6 and ischemic stroke7. With the rapid economic development, the prevalence of dyslipidemia in Chinese adults has been increasing6,8,9,10. Chengdu and Chongqing, the Chengdu-Chongqing economic circle, are representative metropolitans with soaring economic progress of Southwestern China. There has been scarce epidemiological evidence regarding dyslipidemia in Southwestern China. We conducted a community-based cross-sectional survey to assess the burden of dyslipidemia among urban adults in Southwestern China and provide advice on dyslipidemia management.
Results
Demographic and clinical characteristics of the study participants
Among the 10,221 respondents (Table 1), 3474 were men and 6747 were women. The mean age was 55.0 ± 10.7 years, and men had a higher average age. Men had higher prevalence of monthly income over 2000 CNY, smoking, drinking, and daily exercise. The 2 h blood glucose, triglycerides, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) levels were lower in men, and there was no significant difference in fasting blood glucose levels. Men had higher waist circumference (WC), systolic blood pressure (SBP), and diastolic blood pressure (DBP) levels, and lower BMI levels than women. The prevalence of hypertension in men was slightly higher than that in women, and there was no significant difference in the prevalence of diabetes.
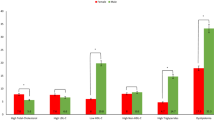
Age-specific prevalence of dyslipidemia
Figure 1 shows the relationships between age, sex, and the prevalence of specific types of dyslipidemia. High TG: In men, compared with those of 35–44 years, it reached the highest in participants of 45–54 years, and then decreased in those of 55–64 and 65–79 years. In women, the prevalence of high TG increased with aging. High TC: In men, there was no significant change with age, while in women, the prevalence of high TC increased with aging. High LDL-C: In men, the prevalence increased with aging, reaching the highest in participants of 55–64 years, and then decreased. In women, the prevalence fluctuated with age. Low HDL-C: In men, the prevalence was highest in participants of 35–44 years and then declined. Among women, there was no significant change. Dyslipidemia: Prevalence decreased with aging in men and increased with aging in women.
Sex- and age-specific mean of lipid levels
Table 2 shows the lipid levels in subgroups stratified by sex and ages. In men, triglycerides levels showed a downward trend with aging, while LDL-C and HDL-C levels showed an upward trend. There was no significant change in TC level across ages. In women, triglycerides, TC, and LDL-C levels showed an upward trend, while HDL-C levels showed no significant trend.
Prevalence of dyslipidemia
Table 3 shows the relationships between different factors and the prevalence of dyslipidemia. The prevalence of high TG, high TC, high LDL-C, low HDL-C, and dyslipidemia were 15.7% (95% confidence interval, 15.0–16.4%), 5.4% (4.9–5.8%), 2.5% (2.2–2.8%), 5.7% (5.3–6.2%), and 27.4% (26.5–28.2%), respectively. The prevalence of dyslipidemia increased with aging, and was higher in men (30.2%) than in women (25.9%). Elevated TG was related to daily exercise, hypertension, diabetes, overweight, and central obesity. TC increased with aging, gender, marital status, education level, smoking status, high blood pressures, diabetes, overweight, and central obesity. Elevated LDL-C was associated with aging and diabetes. Lower HDL-C was associated with gender, education level, income, smoking status, high blood pressures, overweight, and central obesity. Dyslipidemia was associated with aging, sex, education, monthly income, smoking status, daily exercise, hypertension, diabetes, overweight, and central obesity.
Multivariable-adjusted ORs and 95%CI for dyslipidemia
Table 4 shows the results of multivariable logistic regression analysis. High TG was positively correlated with high school education, smoking, hypertension, diabetes, overweight and obesity, central obesity, but negatively correlated with daily physical exercise. Compared with participants of 35–44 years, TG elevation was higher in participants of 45–54 years but lower in those of 65–79 years. For high TC, there was a positive correlation with diabetes, and a negative correlation for women with education levels of high school or above. Compared with participants of 35–44 years, those of 65–79 years had a higher risk of TC elevation. Elevated LDL-C was positively correlated with age and diabetes. Decreased HDL-C was positively correlated with female, high school education, monthly income over 2000 CNY, smoking, overweight and obesity, and central obesity but negatively correlated with aging (35–44 years of age as a reference). Dyslipidemia was positively correlated with high school education, monthly income over 2000 CNY, smoking, hypertension, diabetes, overweight and obesity, central obesity, but negatively correlated with daily physical exercise.
Discussion
This study investigated dyslipidemia and related risk factors in urban adults aged 35–79 years in Chengdu and Chongqing from September 2013 to March 2014, using a multi-stage sampling in Southwestern China. In this study, the prevalence of dyslipidemia was 27.4%, which increased with aging, and was higher in men (30.2%) than in women (25.9%). The higher prevalence in men may be related to the higher income, smoking rate, drinking rate, WC, hypertension, SBP, and DBP levels. The prevalence of dyslipidemia in women was lower than that in men in participants under 55 years of age, whereas the prevalence was higher in women than in men in later life. With the increase of age, TG, TC, and LDL-C levels in women showed an increasing trend. This result was consistent with other studies9,12. This may be related to the changes in estrogen levels in women before and after menopause12. Our results showed that dyslipidemia was unrelated to age and gender. This may be due to the varied age-related changes in the prevalence of dyslipidemia between men and women.
The national chronic kidney disease survey in China13 showed that the prevalence of dyslipidemia in Chinese adults was 34.0%9. The prevalence of dyslipidemia in Southwestern China is lower than Chinese adults. Besides, the prevalence of dyslipidemia (27.4%) and average lipid levels (TG 1.3 mmol/L and TC 4.6 mmol/L) in Southwestern China were lower than that in other regions of China as previously reported. For example, the cities with developed economy, such as Beijing14 (dyslipidemia 35.4%, TG 1.53 mmol/L, TC 5.05 mmol/L), Shanghai12 (dyslipidemia 36.5%), Shenzhen15 (dyslipidemia 34.72%, TG 1.44 mmol/L, TC 4.77 mmol/L), Jilin16 (dyslipidemia 62.1%) and Shandong17 (dyslipidemia 45.8%). The prevalence of dyslipidemia displays obvious economic and regional difference. This may be related to the following reasons: (1) The economically developed regions like Beijing14, Shanghai12 and Guangzhou15 have higher living standards, and their lifestyles and consumptions of Western diet are close to developed countries; (2) The cold climate in the northern region leads to an increased intake of animal fats, a decreased intake of fresh fruits and vegetables, and restriction of outdoor physical activity, thus increasing the risk of obesity and related metabolic abnormalities16,17.
Chengdu is the capital of Sichuan Province, compared with the epidemiological survey of dyslipidemia in Sichuan18 in 2002, the prevalence of dyslipidemia was increased to a certain extent (22.5% vs 27.4%). The lipid levels were also increased. TG and TC levels were 1.14 and 3.76 mmol/L, respectively, in 2002 and 1.3 and 4.6 mmol/L in this study. These increases are consistent with the rapid economic development and lifestyle changes in the Southwestern region. Although the current prevalence of dyslipidemia and lipid levels in the Southwestern urban people aged 35–79 were still lower than that in the other regions in China, the increasing trends indicate that prevention and management of dyslipidemia in Southwestern China should be seriously implemented.
The prevalence of high TG, high TC, low HDL-C, and high LDL-C in people aged 35–79 years in Southwestern China were 15.7%, 5.4%, 5.7%, and 2.5%, respectively, while the prevalence of high TG, high TC, low HDL-C and high LDL-C in Chinese adults9 were 12.2%, 7.5%, 15.3%, and 8.0%, respectively. High TG was the most common dyslipidemia in Southwestern China. The prevalence of high LDL-C was much lower in Southwestern China. Compared to the other lipid parameters, the LDL-C level is most closely related to ASCVD risk19,20. A research21 involving 219,522 Chinese patients with type 2 diabetes showed that, in Chinese adults with type 2 diabetes, the prevalence of CHD and stroke were lowest in Southwest China. Another national survey22 including 480,687 adults aged ≥ 20 years demonstrated that the prevalence of stroke was lowest in Southwestern China. Despite its large population and high GDP, Southwestern China had a lower average number of percutaneous coronary intervention23. In contrast to dyslipidemia, recent studies24,25 showed that the prevalence of hypertension (38.4%) and diabetes (19.5%) in the Southwestern China was higher than the national average (hypertension 32.5%26, diabetes 9.7%27). Therefore, it is reasonable to speculate that the lower prevalence of dyslipidemia and lower LDL-C levels contribute to the lower ASCVD prevalence in Southwestern China. Further studies should be conducted to validate our findings.
This study also analyzed the correlations between dyslipidemia and various factors. In addition to the common risk factors associated with dyslipidemia10,28, such as smoking, hypertension, and diabetes, this study also showed a positive correlation between a high educational level, a monthly income of more than 2000 CNY, and the prevalence of dyslipidemia. This may be due to the better economic and nutritional status of people with higher education and incomes29. Overweight, obesity, and central obesity are correlated with dyslipidemia, suggesting that BMI and waist circumference can be used as screening indicators for dyslipidemia. Weight control is an important prevention and control method30,31. Besides, dyslipidemia was negatively correlated with daily physical exercise, suggesting that strengthening physical exercise is also an important method for the prevention and control of dyslipidemia.
This study has several limitations. In the study design, we did not consider clusters of population sampled with varying probabilities according to their size. We excluded about 24% of participants lacking significant information, such as demographic information, anthropometric measurements, and lipid measurements, which may cause potential selection bias. To minimize the potential selection bias, we calculated the associated Clopper-Pearson 95% confidence intervals for prevalence. Participants enrolled by a multi-stage (district-subdistrict-community) sampling were adults in Chengdu and Chongqing, the most advanced cities in Southwestern China. Five selected districts in this study may not well represent urban areas of Southwestern China or primary sampling frames. A mass of the rural population has been migrating to that both cities due to the government’s urbanization policies, and the study population cannot reflect ethnic diversity in Southwestern China. Thus, the sampling error was underestimated in the study population versus the source population. The prevalence observed likely overestimated the prevalence of dyslipidemia among adults in Southwestern China. Of note, large samples can partially compensate loss of accuracy.
In conclusion, our study provides the latest information regarding dyslipidemia in Southwestern China. The results show that the prevalence of dyslipidemia in Southwestern China was lower than the national average. High TG is the main type of dyslipidemia, and the prevention and control of dyslipidemia is challenging. Dyslipidemia is closely related to smoking, hypertension, diabetes, higher education, higher incomes, obesity, and central obesity. Only by strengthening public health education and intervening in risk factors can we deal with the challenge.
Methods
Study population
From September 2013 to March 2014, a multi-stage (district-subdistrict-community) sampling was conducted in Chengdu and Chongqing. First, Jinjiang district, Longquanyi district, and Chenghua district were randomly sampled from urban areas in Chengdu, and Yubei district and Jiangbei district were randomly sampled from urban areas in Chongqing. Second, a subdistrict was randomly sampled from each district. Finally, a community was randomly s sampled from each subdistrict, and residents in this community who met the inclusion and exclusion criteria were selected. Among the 14,061 eligible participants from five representative urban communities, 13,378 people aged 35–79 years living in Chengdu and Chongqing were enrolled, yielding a response rate of 95.1% (13,378/14,061). The ethics committee of the Second People’s Hospital of Chengdu approved this study protocol (NO 2013015). All participants provided written informed consent.
Inclusion and exclusion criteria
From September 2013 to March 2014, residents aged 35 to 79 years who had lived in selected communities for more than five years were included in the study. People with secondary hypertension, mental illness, malignancy, renal failure requiring dialysis, or refusal to participate were excluded. Due to the lack of demographic information and weight, blood pressure, waist circumference, or body mass index (BMI) data, and lipid measurements, 10,221 participants were included in the final analysis.
Data collection
More than 30 investigators were trained in data collection, including questionnaire, anthropometric measurements and blood biomarkers testing. According to the cardiovascular survey methodology developed by the World Health Organization11, subjects filled out the same field questionnaire, including demographic characteristics; lifestyle, personal and family history of the disease; measurements of height, weight, waist circumference, and blood pressures; fasting glucose, triglycerides (TG) and total cholesterol (TC) levels were also included. BMI was calculated by dividing weight in kilograms by height in meters squared, and subjects were asked to go barefoot and wear only light clothing when measuring height and weight. The researchers measured the minimum circumference between the lower edge of the rib and the iliac spine to get a waist measurement. Thirty minutes before the measurement of blood pressures, the subjects were told not to drink coffee, tea, or alcohol, and not to smoke or exercise. The subjects sat for a five-minute break, then had their blood pressures measured while they sat with a mercury sphygmomanometer. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) recorded the first occurrence of Korotkoff sound (stage I) and the disappearance of Korotkoff sound (stage V), respectively, and averaged blood pressure readings of the two measurements. Fasting venous blood was collected. All blood samples were sent to the Clinical Laboratory Center of Second People's Hospital of Chengdu and Clinical Laboratory Center of the Second Affiliated Hospital of Chongqing Medical University. Total cholesterol, TG, and blood glucose were measured by enzymatic method. All anthropometric measurements and blood biomarkers testing were carried out in accordance with relevant guidelines and regulations.
Index definition
Smoking is defined as having smoked more than 100 cigarettes in a lifetime. Drinking is defined as consuming more than 30 g of alcohol per week for more than a year. Regular physical activity refers to moderate or vigorous activity of 30 min or more on at least 3 days a week8. Hypertension is defined as having a definite medical history, and/or systolic blood pressure greater than or equal to 140 mmHg, and/or diastolic blood pressure greater than or equal to 90 mmHg. Diabetes is defined as having a definite medical history, and/or fasting glucose greater than or equal to 7.0 mmol/L, and/or a 2-h glucose tolerance test greater than or equal to 11.1 mmol/L. According to the guidelines for Prevention and Treatment of Dyslipidemia in Chinese Adults (2016 Revision), dyslipidemia is defined as TC ≥ 6.2 mmol/L, low-density lipoprotein cholesterol (LDL-C) ≥ 4.1 mmol/L, high-density lipoprotein cholesterol (HDL-C) < 1.0 mmol/L, and/or TG ≥ 2.3 mmol/L, and/or self-reported history of dyslipidemia9.
Diagnostic criteria
Dyslipidemia was defined as total cholesterol ≥ 6.2 mmol/L, and/or LDL cholesterol ≥ 4.1 mmol/L, and/or HDL cholesterol < 1.0 mmol /L, and/or TG ≥ 2.3 mmol /L, and/or self-reported history of dyslipidemia, following Chinese Guidelines for Prevention and Treatment of Dyslipidemia in Adults (2016 Revision)9.
Statistical analysis
Absolute number (percentage, %) was used to describe the categorical data, and a Chi-Square test was used to compare the difference between different groups. We calculated 95% confidence intervals for prevalence using Clopper–Pearson method. The data subject to or close to the normal distribution were described by means ± standard deviation, and the difference between different groups was compared by Student’s t-test. The data of skewed distribution were described by the median with the interquartile range, and the comparison between different groups was performed by Wilcoxon rank sum test. Trend analysis was done by Chi-Square trend test or linear regression analysis. Both univariable and multivariable analyses were performed using an unconditional Logistic regression model, and the OR value and its 95% confidence interval were calculated. We used a forward-stepwise selection method (Likelihood Ratio, LR) to specify how independent variables were entered into the multivariable logistic regression model. All statistical analyses were performed with SPSS 23.0 software, and P < 0.05 was considered statistically significant.
References
Murray, C. J. et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 386, 2145–2191 (2015).
Roger, V. L. et al. Heart disease and stroke statisticse2011 update: A report from the American Heart Association. Circulation 123, e18–e209 (2011).
Reiner, Z. et al. ESC/EAS guidelines for the management of dyslipidaemias. Rev. Espanola Cardiol. 64, 1168 (2011).
Yusuf, S., Reddy, S., Ounpuu, S. & Anand, S. Global burden of cardiovascular diseases: part I: General considerations, the epidemiologic transition, risk factors, and impact of ur-banization. Circulation 104, 2746–2753 (2001).
Expert panel on detection, E and treatment of high blood cholesterol in, A, executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III), JAMA 285, 2486–2497 (2001).
Joint Committee for Developing Chinese guidelines on, P and Treatment of Dyslipidemia in, A, Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua xin xue guan bing za zhi. 35, 390–419 (2007).
Pisciotta, L., Bertolini, S. & Pende, A. Lipoproteins, stroke and statins. Curr. Vasc. Pharmacol. 13(2), 202–208 (2015).
Yang, W. et al. Serum lipids and lipoproteins in Chinese men and women. Circulation 125(18), 2212–2221. https://doi.org/10.1161/CIRCULATIONAHA.111.065904 (2012).
Pan, L. et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis 248, 2–9. https://doi.org/10.1016/j.atherosclerosis.2016.02.006 (2016).
Wang, S. et al. Prevalence and associated factors of dyslipidemia in the adult Chinese population. PLoS ONE https://doi.org/10.1371/journal.pone.0017326 (2011).
Rose, G. A. & Blackburn, H. Cardiovascular survey methods. Monogr. Ser. World Health Organ. 56, 1–188 (1968).
Wu, J. Y. et al. Dyslipidemia in Shanghai, China. Prev. Med. 51, 412–415 (2010).
Zhang, L. et al. Prevalence of chronic kidney disease in China: A cross-sectional survey. Lancet 379, 815–822 (2012).
Cai, L., Zhang, L., Liu, A., Li, S. & Wang, P. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J. Atheroscler. Thromb. 19(2), 159–168. https://doi.org/10.5551/jat.10116 (2012).
Yuan, X. et al. 6-Year trends in lipids among adults in Shenzhen, China [published online ahead of print, 2019 Nov 14]. J Public Health (Oxf). fdz113. https://doi.org/10.1093/pubmed/fdz113 (2019).
He, H. et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: A cross-sectional study. Lipids Health Dis. 13:122. Published 2014 Aug 3. https://doi.org/10.1186/1476-511X-13-122 (2014).
Gao, N. et al. Dyslipidemia in rural areas of North China: prevalence, characteristics, and predictive value. Lipids Health Dis. 15(1):154. Published 2016 Sep 13. https://doi.org/10.1186/s12944-016-0328-y (2016).
Deng, Y, Wu, X.P., Gao, Y.L., et al. An epidemiological analysis of dyslipidemia among urban and rural residents in Sichuan Province. China. J. Prev. Contr. Chron. Non-comun. Dis. 14(4). https://doi.org/10.3969/j.issn.1004-6194.2006.04.026 (2006).
Ofori-Asenso, R., Zoungas, S., Tonkin, A. & Liew, D. LDL-cholesterol is the only clinically relevant biomarker for atherosclerotic cardiovascular disease (ASCVD) risk. Clin. Pharmacol. Ther. 104(2), 235–238. https://doi.org/10.1002/cpt.1125 (2018).
Yang, X. et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: The China-PAR project (Prediction for ASCVD Risk in China). Circulation 134(19), 1430–1440. https://doi.org/10.1161/CIRCULATIONAHA.116.022367 (2016).
Lyu, Y. et al. regional differences in the prevalence of coronary heart disease and stroke in patients with type 2 diabetes in China. J. Clin. Endocrinol. Metab. 103(9), 3319–3330. https://doi.org/10.1210/jc.2018-00422 (2018).
Wang, W. et al. Prevalence, incidence, and mortality of stroke in China: Results from a nationwide population-based survey of 480 687 adults. Circulation 135(8), 759–771 (2017).
Lü, S. Z., Song, X. T., Chen, Y. D. Registry of PCI in China (ROPIC) study investigators. [Findings from registry of percutaneous coronary intervention in inland of China]. Zhonghua Xin Xue Guan Bing Za Zhi. 37(1):26–9 (Chinese). (2009).
Huang, X. B. et al. Prevalence, awareness, treatment, and control of hypertension in southwesternern China. Sci. Rep. 9(1), 19098 (2019).
Cao, X. et al. Prevalence and rates of new diagnosis and missed diagnosis of diabetes mellitus among 35–74-year-old residents in urban communities in Southwestern China. Biomed. Environ. Sci. 32(9), 704–709 (2019).
Lewington, S. et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern. Med. 176(4), 524–532 (2016).
Yang, W. et al. Prevalence of diabetes among men and women in China. N Engl J Med. 362(12):1090–101. https://doi.org/10.1056/NEJMoa0908292 (2010).
Toth, P. P., Potter, D. & Ming, E. E. Prevalence of lipid abnormalities in the United States: The National Health and Nutrition Examination Survey 2003e2006. J. Clin. Lipidol. 6, 325–330 (2012).
Sharma, U. et al. Dyslipidemia and associated risk factors in a resettlement colony of Delhi. J. Clin. Lipidol. 7(6), 653–660. https://doi.org/10.1016/j.jacl.2013.06.003 (2013).
Bays, H. E., Chapman, R. H., Grandy, S., SHIELD Investigators' Group. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: Comparison of data from two national surveys [published correction appears in Int J Clin Pract. 2007 Oct;61(10):1777–8]. Int. J. Clin. Pract. 61(5):737–747. https://doi.org/10.1111/j.1742-1241.2007.01336.x (2007)
Nguyen, N. T., Magno, C. P., Lane, K. T., Hinojosa, M. W. & Lane, J. S. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: Findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J. Am. Coll. Surg. 207(6), 928–934. https://doi.org/10.1016/j.jamcollsurg.2008.08.022 (2008).
Acknowledgements
We sincerely thank all the field staff and participants for their contributions.
Author information
Authors and Affiliations
Contributions
C.H. and W.Q.Z. conceived and designed the study, analysed the data and drafted the manuscript. W.W.T. analysed the data and advised on the interpretation of results. Y.L., J.X.L., R.H.X., and X.B.H. participated in the data collection and checking. S.P.Z., and T.D.W., and X.B.H., advised on the interpretation of results and were responsible for the research.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, C., Zhang, WQ., Tang, WW. et al. Prevalence and related factors of dyslipidemia among urban adults aged 35 to 79 years in Southwestern China. Sci Rep 11, 17579 (2021). https://doi.org/10.1038/s41598-021-96864-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96864-w
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.