Abstract
Essential tremor (ET) is a major cause of disability and is not effectively managed in half of the patients. We investigated whether mechanical vibration could reduce tremor in ET by selectively recruiting afferent pathways. We used piezoelectric actuators to deliver vibratory stimuli to the hand and forearm during long trials (4 min), while we monitored the tremor using inertial sensors. We analyzed the effect of four stimulation strategies, including different constant and variable vibration frequencies, in 18 ET patients. Although there was not a clear homogeneous response to vibration across patients and strategies, in most cases (50–72%) mechanical vibration was associated with an increase in the amplitude of their tremor. In contrast, the tremor was reduced in 5–22% of the patients, depending on the strategy. However, these results are hard to interpret given the intrinsic variability of the tremor: during equally long trials without vibration, the tremor changed significantly in 67% of the patients (increased in 45%; decreased in 22%). We conclude that mechanical vibration of the limb does not have a systematic effect on tremor in ET. Moreover, the observed intrinsic variability of the tremor should be taken into account when designing future experiments to assess tremor in ET and how it responds to any intervention.
Similar content being viewed by others
Introduction
Essential tremor (ET) is one of the most prevalent movement disorders in adults1, affecting approximately 5% of people over age 652. ET manifests as a bilateral, largely symmetric postural or kinetic tremor involving the hands and forearms, and is often accompanied by head tremor3. There are different phenotypes of ET patients4,5, but their pathological differences are not fully understood. Importantly, even though as many as 75% of ET patients report significant disability6,7, tremor is only effectively managed in 50% of all patients8,9. Therefore, there is an important need to develop new treatments for ET.
Tremor in ET is thought to originate because of the projection of pathological oscillations in cerebello-thalamo-cortical pathways to the motoneurons innervating the affected muscles10, although its exact mechanisms remain elusive. Some studies point at neurodegeneration in the cerebellum11,12,13,14 although this notion has been challenged by a different group15. A classic hypothesis proposes that the inferior olive is the ultimate cause of tremor in ET, due to abnormal oscillations in the olivo-cerebellar pathways that are transmitted to thalamo-cortical circuits16. The involvement of the inferior olive is put forward due to its rhythmic properties, which mediate the production of tremor in harmaline models of ET17. However, the harmaline model is quite debated18. Harmaline model is based on the administration of harmaline and harmine (tremorigenic β-carbolines) to experimental animals with the aim to induce postural and kinetic tremor by interference with the inferior olive, climbing fibers, and the deep cerebellar nuclei19.
Mechanoreceptors, including Pacinian and Meissner corpuscles, are sensitive to vibratory stimuli. In anesthetized or decerebrated animals, Pacinian corpuscles respond to high frequency stimuli (60–600 Hz), whereas Meissner corpuscles respond to lower frequency stimuli (10–300 Hz)20,21. Sensory responses from both types of receptors are projected to the ipsilateral cuneate nucleus22, the main brainstem recipient of sensory input from the upper limbs23 through afferent thick myelinated fibers. The cuneate nucleus has important projections to the thalamus and the inferior olive22,24, and therefore may provide a pathway to modulate the circuits that mediate tremor in ET. For example, direct stimulation of the cuneate nucleus has inhibitory effects on cerebellar activity in decerebrated cats24.
Tremor in ET is primarily managed with drugs or using deep brain stimulation, a technique that requires neurosurgery8. Non-invasive wearable devices that stimulate or exert forces on the affected limb are an appealing alternative25,26. Examples of these devices span robotic exoskeletons27,28, functional electrical stimulation systems29, or devices that aim at recruiting afferent pathways30,31,32. Sensory electrical stimulation (with the intensity range between sensory and motor threshold) reduced postural tremor in ET patients even five minutes post-stimulation. Although the underlying mechanism is unknown, the authors proposed that feedback signal through the afferent pathway might have affected the cerebrum as the source of tremor31,32. Although many of them showed clear improvements during standard clinical tasks in convenience samples of patients, none of them –to the best of our knowledge– has gone beyond laboratory trials. Moreover, none has tried to deliver selective vibration to stimulate the afferent vibratory fibres to generate a physiological sensory input without the drawback of provoking the pain observed in electric stimulation.
Here we investigated whether afferent stimuli delivered through mechanical vibration of the hand and forearm could attenuate the tremor in ET. Our hypothesis was that vibration would recruit Pacinian corpuscles and thus modulate the abnormal activity in tremor-related pathways, which would in turn reduce the tremor. However, our data do not support this hypothesis. We found that across a proof of concept study with a sample of 18 patients the response to vibration was largely heterogeneous, with the tremor being reduced, increased or unaffected depending on the patient and the stimulation strategy. Moreover, a patient-specific analysis revealed that there was not a systematic trend in the response to stimulation, and we could not find any relationship between patient response, tremor characteristics or clinical features. Critically, we also found that during our relatively long continuous recordings (4 min), tremor amplitude was very non-stationary even during the no stimulation condition. We propose that future interventions should be evaluated during several-minute long trials due to the largely non-stationary characteristics of the tremor.
Results
Protocol and apparatus
We designed and built a platform to stimulate mechanically the afferent pathways of a patient and assess the effects in the ongoing tremor. Vibratory stimuli were applied using piezoelectric actuators attached to the tremor-dominant hand and forearm. The stimulators were located on the fingertips, the palm of the hand and the anterior side of the forearm, the areas with the highest density of Pacinian corpuscles33,34 (Fig. 1a). We measured the ongoing wrist tremor using inertial measurement units (IMUs), which we strapped to the hand dorsum and the distal part of the forearm of the patient (Fig. 1b). In our task, patients rested their most affected arm on a support, keeping the forearm outstretched against gravity, with the fingers slightly outstretched and the hand parallel to the ground (Fig. 1c). Prior to the beginning of the experiments, we verified that patients were able to perceive the vibratory stimuli.
Experimental setup, task and protocol design. (a) Placement of the piezoelectric actuators used to apply vibratory stimuli (fingertips, hand and forearms; palmar view). (b) Placement of the IMUs used to record the ongoing tremor (dorsal view). (c) Apparatus used to perform the postural task: patients rested the distal part of their arms on a horizontal elastic band in the arm support. (d) Schematic of the experimental protocol. In the top row, each rectangle is one of the five stimulation strategies; the expanded panel shows how each trial was divided in four 60-s epochs.
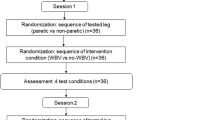
All ET patients (n = 18; see details in Supplementary Table 1 and Methods) performed this postural task five times, each time under a different stimulation strategy (Fig. 2d). These five trials lasted 4 min each, and were interleaved with 10 min rest periods. This design ensured that the stimulation response was independent across trials, and minimized fatigue accumulation. The five stimulation strategies were: (1) No stimulation (“NoStim”): no stimulation was applied, we just recorded the ongoing tremor as a control measurement to characterize it; (2) Stimulation at 50 Hz (“50 Hz”): vibration was delivered at 50 Hz, a frequency that minimally recruits Pacinian corpuscles34; (3) Stimulation at 250 Hz (“250 Hz”): vibration was delivered at 250 Hz, a frequency that should maximally recruit Pacinian corpuscles34; (4) Increasing stimulation frequency (“IncreasingFreq”): we delivered vibratory stimuli with increasing frequency, from 50 to 450 in 50 Hz steps (each frequency was delivered for 13.33 s), to test the influence of stimulation frequency on the tremor; and (5) Random stimulation frequency (“RandomFreq”): we applied the same frequencies than in the previous strategy, but in random order. For strategies 2–5, each 4-min trial comprised a 1-min baseline epoch (Pre-stim), followed by a 2-min stimulation epoch (Stim which we divided in two 1-min epochs, Stim1 and Stim2, for the analysis), and a 1-min epoch to assess eventual lasting effects (Post-stim; see inset in Fig. 1d).
Example recordings during all stimulation strategies for one patient (P4). (a) Wrist tremor (3 s of data) during each of the four epochs (Pre-stim, Stim1, Stim2, Post-stim; each shown in a different column) for all the stimulation strategies (each shown in a different row); the fifth column represents the corresponding power spectral densities (data band-pass filtered between 3–12 Hz). (b) Tremor amplitude during each of the five strategies for the same patient. Each trace represents the time-varying RMS of the tremor amplitude computed in 1-s long windows. Same color code as in a.
Responses to mechanical vibration
Figure 2 shows example recordings during all five stimulation strategies for one patient (Supplementary Figs 1, 2 show data for two other patients). As shown in the top row of Fig. 2a, tremor amplitude varied over time even in the NoStim condition. Moreover, the pre-stimulation amplitude (left most column in Fig. 2a) differed greatly across trials, highlighting the intrinsic variability of the tremor. In contrast, there were no clear differences in tremor frequency within or across stimulation strategies, as reported for other peripheral interventions on tremor27,35,36 (right most column in Fig. 2a; see data for all patients in Supplementary Figs 3, 4). Figure 2b shows our preliminary processing for data analysis: we estimated the tremor amplitude in non-overlapping 1-s long windows for each of the 1-min long epochs (Pre-stim, Stim1, Stim2, Post-stim). These example data, suggests that the tremor amplitude exhibited complex changes over time, both in the absence of stimulation and in association with the different stimulation strategies.
When comparing tremor characteristics (NoStim trials) across patients, we observed not only differences in the amplitude of their tremor, but also in its time-varying dynamics (Fig. 3a; notice that Y axis in panels a-e are logarithmic). Normalizing the data for each patient with respect to its amplitude during the first 1-min epoch (Epoch 1 in the figure) helps characterize this large inter-patient variability: the SD is as large as 1.17 times over the mean (lightest trace in Fig. 3f). Therefore, tremor amplitude was considerably variable over long periods without stimulation. In fact, tremor amplitude was significantly different across all 1-min epochs when no stimulation was applied —including both all four epochs in the NoStim trials and the Pre-stim epochs in the stimulation trials (Kruskal-Wallis test, P~0 for all comparisons; see Methods).
Changes in tremor amplitude for each patient, in response to each stimulation strategy. (a–e) Median tremor amplitude (RMS) for each strategy (indicated on top) during each 1-min epoch. Each color represents one patient. (f) Data pooled over all patients after normalizing the tremor amplitude with respect to the Pre-stim amplitude for the corresponding strategy. Error bars: mean ± SD.
The changes in tremor amplitude were largely variable across patients for each of the four stimulation strategies (Fig. 3b–e). These large, complex changes happened even when we stimulated at 50 Hz, the frequency that should have had the least influence on the tremor based on the frequency-dependent response of Pacinian corpuscles34 (Fig. 3b). This finding is perhaps less surprising given how intrinsically variable the tremor was (Fig. 3a). As for the NoStim trials, normalizing each trial with respect to its Pre-stim amplitude revealed large SDs in the response to all stimulation strategies (Fig. 3f and Supplementary Fig. 5), therefore, all group trends in these data must be interpreted with caution. Because of this heterogeneous response to stimulation, we have not included the results for the Post-stim epochs.
After observing these large inter-patient differences, we sought to understand each patient’s response to stimulation with a finer grain analysis. Figure 4 shows detailed comparisons between the PreStim and Stim conditions (the two 1-min Stim1 and Stim2 epochs combined) for each stimulation strategy for three patients. Overall, the effect of each stimulation strategy differed greatly across them. For example, during stimulation at 250 Hz: for patient P4, tremor amplitude increased greatly (Fig. 4g); for patient P9, tremor amplitude decreased greatly (Fig. 4i); and for patient P15, tremor amplitude barely changed (Fig. 4j).
Effect of the different stimulation strategies on the tremor of three representative patients (P4, P9 and P15). Each panel compares the Pre-stim epoch (blue) with its correspondent two minutes Stim epoch (Stim1 + Stim2; in red). Each histogram is the distribution of tremor amplitude in 1 s bins for the corresponding stimulation condition. Top errorbars: mean ± SD; * denotes that the Pre-Stim and Stim epochs are significantly different (P < 0.01, Mann-Whitney U test).
Figure 5 summarizes this analysis for all 18 patients. Overall, all stimulation strategies predominantly increased the amplitude of the tremor, indicated as the dominant portion of red squares in the subject-specific responses to stimulation (Fig. 5b). However, there were also a few patients for whom the tremor was reduced or unaffected (Fig. 5a). This same varied response was observed during the NoStim trials, as expected from Fig. 3. Besides, even for the six patients whose tremor remained unchanged during the NoStim trial, the changes in tremor amplitude during the stimulation trials were very heterogeneous, resulting in tremor that was mostly increased (46%; data pooled across all stimulation strategies), but also decreased (17%) or unaffected (37%).
Summary of the changes in tremor amplitude during the different stimulation strategies. (a) Change in tremor amplitude during each Stim epoch with respect to the corresponding Pre-stim epoch for each patient, during each trial type. (b) Percentage of patients for which the tremor decreased, increased or remained unaltered.
As the global tendency was that for the tremor to increase when the stimulation was applied, we tried to identify a global effect by assessing the Stim/PreStim ratio (RT) response under the different stimulation strategies. This ratio was calculated using the rms value of tremor during epoch 1 (PreStim) and epochs 2 and 3 (Stim), following Eq. (1). Subject specific responses are represented in Fig. 6a.
Stim/PreStim ratio response to stimulation strategies. Panel a. shows the individual response of each subject under every stimulation strategy. Columns represent each subject behavior; a different marker is used to identify each stimulation strategy. Markers under 100% line (grey dashed line) mean that the subjects decreased his/her tremor, while markers over the 100% line mean an increase in subjects tremor. Panel b. represents subjects behavior grouped by stimulation strategies. No significant differences were found between No Stim condition and the other stimulation strategies (paired samples t-test, P > 0.01). Notice that both panels use logarithmic scales in the Y axis.
After grouping subjects responses according to the stimulation strategy, we tried to find a global effect of the different stimulation strategies. The analysis of these groups revealed that no significant differences exist between tremor response under stimulation strategies and the No Stim condition (P > 0.01; paired-samples t-test; see Fig. 6b).
Relationship between stimulation response and patient characteristics
We sought to understand whether the complex changes in tremor amplitude during each stimulation strategy depended on relevant clinical features of the patients (age, disease duration, tremor severity and gender). We tried to find linear relationships between these features and the evolution of tremor under the different stimulation strategies. However, the two only significant relationships (P < 0.01) that we found were between the evolution of the tremor and tremor severity when the NoStim strategy and the IncreasingFreq strategy were applied (Supplementary Fig. 8, panels c and i). These limited significant fits together with the high intrinsic variability of the tremor (Fig. 3f), suggest that clinical characteristics do not have a clear effect on our results.
When relating the changes in tremor amplitude during stimulation to tremor characteristics (frequency and amplitude), the only statistically significant relationship in the group data was that the lower the tremor frequency, the more its amplitude increased during the IncreasingFreq (P = 0.007) and RandomFreq stimulation trials (P = 0.015) (Fig. 7a,b). When examining the relationship between tremor amplitude and stimulation frequency during these trials for each patient separately, we found a statistically significant association in 44% of the patients in the IncreasingFreq trials (P < 0.01; detailed results in Supplementary Table 4, see examples of statistically significant models in Fig. 7c–e). However, this relationship did not hold during the RandomFreq trials (no significant associations for any patient). Given that we applied the same set of stimulation frequencies during the IncreasingFreq and RandomFreq trials (but in a different order), we conclude that the effect of mechanical vibration on the tremor is not strongly frequency-dependent.
Understanding the relationship between tremor characteristics and the changes in tremor amplitude during stimulation. (a) There was a significant relationship between tremor frequency and how tremor amplitude changed during the IncreasingFreq and RandomFreq trials. (b) For some patients, there was also a significant relationship between tremor amplitude and the frequency of the vibratory stimuli. *Denotes that the models were statistically significant (P < 0.01).
Discussion
We studied the effect of mechanical vibration of the forearm and the hand on tremor in ET. Our goal was to selectively recruit the Pacinian corpuscles to disrupt the tremor-related activity in the brain and attenuate the tremor. To that end, we designed a protocol in which we delivered vibratory stimuli with different characteristics (frequency) and studied their impact on the tremor. Overall, although in the majority of individual analysis the result seems to be that mechanical vibration is paralleled by an increase in tremor amplitude, the inter-patient response was too large variable to draw meaningful conclusions. In fact, the assessment of the effect of the stimulation strategies across patients with Stim/PreStim ratio resulted in no significant differences between basal condition and vibratory conditions, i.e. mechanical vibration does not produce a clear and consistent effect in ET patients tremor. Critically, we also observed that during our relatively long recordings without stimulation (NoStim trials), there were very large changes in the amplitude of the tremor. This casts a shadow on how to interpret the stimulation results. Moreover, it suggests that previous studies, which are mostly based on shorter trials, should be interpreted with caution, and that these intrinsic fluctuations need to be considered when designing future experimental protocols to validate tremor suppression approaches.
Relation to previous studies
No previous study, to our knowledge, had investigated the effect of mechanical vibration on tremor in ET. However, a few groups have used sensory (i.e., below the motor threshold) electrical stimulation to try to reduce tremor in ET. Heo et al.30 showed that electrical stimulation of the main arm and wrist muscles at 100 Hz reduced the amplitude of the tremor in ET. Even though their group results were statistically significant, their data also seem largely variable across patients and trials given how broad their data distributions are (their Fig. 2). Dosen et al.31 used a similar approach, although their sample of patients only included two ET patients and tremor suppression was only effective in one of them. The same group recently used surface and intramuscular stimulation, also delivered at 100 Hz, to recruit Ia afferent fibres (among other pathways) and reduce the tremor of four ET patients32. Interestingly, intramuscular stimulation, which likely recruits less tactile receptors than surface stimulation because it is delivered within the muscle, was most effective at attenuating the tremor. Therefore, mechanical vibration seems to affect the tremor in a fundamentally different manner than afferent electrical stimulation, because the trend in our data was for the tremor to remain unaffected compared with basal condition. This is a proof of concept study and further studies with larger samples of patients are needed to confirm if this trend is relevant. However, previous studies investigating novel tremor suppression strategies found a significant reduction with a sample size of 15 to 20 subjects27,28,30,31,32,37.
Two studies have investigated vibration therapy in Parkinson’s disease38,39 (PD), the second most prevalent cause of tremor40. Both studies were based on whole body vibration and reported a reduction in tremor amplitude of 25% and ~50%, respectively. The apparent discrepancy between these results and ours could be interpreted as there being a difference in the response to mechanical vibration between tremor in ET and PD. However, the differences in protocol could account for this discrepancy. In this way, whole-body vibration stimulation approaches38,39 hampers the interpretation of the results due to the complex mechanical interactions between body parts. We overcame this challenge, by only targeting arm tremor and using a support to standardize the task and minimize inter-individual variability.
On the intrinsic variability of the tremor
We observed clear fluctuations over time in the amplitude of the tremor without stimulation. These fluctuations may be caused, at least in part, by subjective factors such as anxiety, distraction or surprise3 –as also mentioned by Dideriksen et al.32. However, they also suggest that there may be a quite large intrinsic variability in tremor in ET32.
This observation is important because most studies that test novel approaches for tremor suppression used shorter trials. For example, trial duration in Heo et al.30 was 15 s. Although in the study presented by Dosen et al.31, the authors used 120 s, they were composed by 1 s epochs without stimulation followed by 3 s with stimulation. Only Dideriksen et al.32 used longer trials of 150 s, which they divided in 30 s epochs with and without stimulation. Traditionally, several groups including ours tried to account for tremor variability by splitting trials in epochs without and with stimulation that were compared to each other27,31,32,35, but this reasonable approach might not be ideal if few-minute long trials are not used. A concern about using long trials in the case of ET is that holding a posture or performing a movement for long periods of time will lead to significant muscle fatigue, and is not very representative of most activities of daily living41.
Relationship with the neural mechanisms of essential tremor
The cuneate nucleus receives input from Pacinian corpuscles. Studies in anesthetized or de-cerebrated animals showed that Pacinian neurons respond maximally to stimulation frequencies in the 50–400 Hz range20,21,22. These data motivated our experimental design: we chose the 250 Hz stimulation strategy as the one that should lead to the maximal effect, and the 50 Hz stimulation strategy as the one that should cause little or no effect22. We also used two strategies in which we delivered stimuli with increasing or random frequency (in 13.3 s blocks) to exclude any potential adaptation to the stimulation34. The stimulation frequencies in these two strategies were the same, to compare the robustness of the response. Unfortunately, our results do not let us support or reject the hypothesis that selective recruitment of Pacinian corpuscles may lead to a reduction of tremor in ET. However, they do suggest that mechanical vibration of the limb is not effective at attenuating the tremor.
The main limitation of this study is that we cannot be certain that mechanical vibration of the limb selectively and/or exclusively recruited Pacinian corpuscles. For example, mechanical vibration of the muscle-tendon complex at frequencies similar to the ones we employed recruits muscle spindles in both animals42,43 and humans44,45. Perhaps the most dramatic evidence of this is that many “sensory illusions” can be triggered by vibrating the tendons46. Therefore, our mechanical stimulation may have recruited afferent pathways other than mechanoreceptors. Another neural mechanism to consider are the persistent inward currents (PICs) that “amplify” motoneuron output47, and that have an important influence on motor control under certain conditions–e.g., by modifying the gain in the spinal cord48. Tendon vibration during voluntary contractions is known to cause PICs in humans49, and thus we could have potentially elicited them during our protocol. Overall, the potential implication of these and other neural mechanisms makes it hard to interpret the data under the light of our hypothesis.
Finally, most previous studies on the integration of sensory input by the cuneate nucleus have been done in de-cerebrated or anesthetized animals, primarily cats. Given the potentially important role of descending cortical input on cuneate activity50, it is perhaps not surprising if the influence of mechanoreceptors is not what would be expected based on those studies. A second potential confound to test our hypothesis is that the neuroanatomy of the primate cuneate nucleus seems to differ from that of the cat51. Therefore, additional neurophysiological studies are needed to better understand the neural pathways involved in the generation of ET and how to target them for new interventions.
Summary
We developed a system to reduce tremor in ET by applying vibratory stimuli to the forearm and the hand. We observed that mechanical vibration was paralleled by largely heterogeneous changes in the tremor across patients, although the dominant trend was for the tremor amplitude to increase when individual analyses were performed. However, we were not able to identify a clear and consistent effect of the stimulation strategies compared with the basal condition. These varied changes could not be explained based on the vibration frequency or the characteristics of the patients. Critically, during our relatively long trials, the intrinsic variability of the tremor, even without stimulation, was larger than we had expected based on previous studies. This observation further hampers the interpretation of our data, but also suggests that new experimental protocols should take into consideration the intrinsic variability of the tremor.
Methods
Patients
Essential tremor (ET) patients were recruited from neurology clinics of the University Hospital 12 de Octubre (Madrid, Spain) after being examined by an expert neurologist in movement disorders. We included patients with age ≥ 18 years that had been diagnosed as having ET according to the diagnostic criteria for ET52. Exclusion criteria were having a pacemaker or deep brain stimulator implanted, or having previous history of epilepsy, head trauma or stroke. For patients taking tremor-management drugs, the medication was kept stable at least since two weeks before the experiments. The local ethical committee at Hospital 12 de Octubre gave approval to the experimental protocol, and warranted its compliance with the Declaration of Helsinki. Trial and protocol were publicly registered in ANZCRT on 14/05/2018; Trial id: ACTRN12618000819224.
A total of 18 patients were eligible and gave written informed consent to participate (six female, twelve male; average age 75.8 ± 7.9 years, mean ± SD; range, 59–88). Average disease duration was 13.6 ± 11.2 years (range 1–40 years). Tremor severity ranged from mild to severe, with a mean score of 2.1 ± 0.9 (range, 1–4) according to the Fahn-Tolosa-Marin tremor rating scale. Five patients were classified as having mild tremor (27.8%), seven patients as having moderate tremor (38.9%), and six patients as having severe tremor (33.3%). A non-exhaustive summary of clinical features is shown in Supplementary Table 1.
The sample size in this study is similar to several publications investigating approaches to suppress tremor in ET patients. Most of these checked their proposed approach with groups of 15 to 20 patients27,28,30,31,32,37.
Apparatus
We designed and built a device that delivered vibratory stimuli with different frequencies to the forearm and the hand, at the same time that we recorded the movement of the wrist. Vibratory stimuli were delivered using piezoelectric actuators (model QP-10W, for the fingertips; PPA-4011 for the hand; PPA-1022 for the forearm; all from Mide Technology, US), which were controlled at 5 kHz through piezoelectric haptic drivers (DRV8662, Texas Instruments, US) via a data acquisition card (DAQ) (NI USB 6003, National Instrument, US) connected to a consumer laptop. The amplitude of the mechanical vibration was left constant during the experiment, and set to the maximum (this corresponded to the following voltage levels: 50 V for PPA-1022, 75 V for QP-10W and PPA-4011). Wrist movement was monitored at 100 Hz using inertial sensors (TechMCS, Technaid, SP).
Experimental protocol
We performed the experiments in the arm most affected by tremor, which was identified by a neurologist at the beginning of the experimental session. During the experiments, patients were comfortably seated in front of a desk. Piezoelectric actuators were located over the fingertips, the hand and the forearm, the areas where Pacinian corpuscle density is higher33 (Fig. 1a). To measure wrist movement, we strapped inertial sensors to the dorsal side of the hand and forearm (Fig. 1b). We elicited hand tremor by asking patients to perform a standard postural task. The proximal arm rested on a purposely-built support (note that the support did not constrain hand or forearm movements to minimize muscle fatigue and inter-subject variability, e.g., such as observed during kinetic task53. During the trials, patients were instructed to hold the arm, forearm and hand outstretched against gravity, to trigger their tremor.
The experimental protocol consisted of five 4 min trials in which we applied different stimulation strategies (Fig. 1d). These trials were interleaved with 10 min long resting periods. The experimental session lasted for ~90 minutes.
-
1.
No stimulation (“NoStim”): a control measurement in which we recorded the tremor during 240 seconds.
-
2.
Stimulation at 50 Hz (“50 Hz”): vibration was delivered at 50 Hz, a frequency which should minimally recruit Pacinian corpuscles34.
-
3.
Stimulation at 250 Hz (“250 Hz”) stimulation: vibration was delivered at 250 Hz, a frequency which should maximally recruit Pacinian corpuscles34.
-
4.
Increasing stimulation frequency (“IncreasingFreq”): vibration was delivered in 50 Hz steps (increasingly, from 50 Hz to 450 Hz); each frequency was applied during 13.33 s. This trial was designed to test the frequency-dependency of the stimulation.
-
5.
Random stimulation frequency (“RandomFreq”): vibration was delivered at the same frequencies as during the IncreasingFreq trials, but their order was randomized; each frequency was again applied during 13.33 seconds. This trial was designed to check any potential adaptation to the stimulation from the frequency-dependent effects.
Trials 2 to 5 were divided into four 60 s epochs: during the first epoch (Pre-stim) we assessed the patient’s basal tremor; during epochs 2 and 3 (Stim1 and Stim2), we applied vibratory stimuli as defined by the corresponding strategy (50 Hz, 250 Hz, IncreasingFreq, RandomFreq); during the last epoch (Post-stim), we assessed the tremor to detect potential after-effects.
Data analysis
Wrist flexion-extension was calculated as the difference between the forearm and hand angular velocities54. The resulting movement was band-passed filter, to keep only the fundamental tremor-related component of movement (10th order Butterworth, fc = 3–12 Hz). We then computed the root-mean-squared value (RMS) of the filtered data in 1 s non-overlapping windows to characterize the time-varying amplitude of the tremor.
We first assessed whether the tremor characteristics were stable during the epochs without stimulation (the whole NoStim trial and the four PreStim epochs of the stimulation trials) using a Kruskal-Wallis test (n = 60), as the data did not conform normality (one-sample Kolmogorov Smironov test; P~0 for all epochs).
To study the changes in tremor amplitude associated with the different stimulation strategies, we compared the corresponding Pre-stim and Stim epochs (concatenated Stim1 and Stim2 epochs) for each patient separately using a Mann-Whitney U test (n = 60 and n = 120, respectively). Detailed results are presented in Supplementary Table 2.
Due to the high variability of the tremor across all epochs without stimulation, we created a combined baseline that characterized the basal tremor for each patient. This combined baseline comprised all eight 60 s epochs without stimulation, excluding the Post-Stim epochs (the whole NoStim trial and the four Pre-stim epochs). We repeated the previous analysis comparing the Stim epoch for each stimulation strategy to the combined baseline rather than to the corresponding baseline, using a Mann-Whitney U test (n = 60 and n = 480, respectively). The detailed results, which are not dramatically different from the original method, are presented in Supplementary Figs 6 and 7.
To find the global effect of the stimulation strategies in tremor behaviour, we calculated the Stim/PreStim ratio of each trial. After checking the normality of the data under each stimulation strategy (Kolmogorov-Smirnov test, P > 0.01) and homoscedasticity of the data (Levene test, P > 0.01), we compared the distribution of NoStim ratios with the responses under the other stimulation strategies using paired-samples t-tests (N = 18). Detailed results are presented in Supplementary Table 5.
Throughout the paper, results are reported as mean ± SD. The confidence threshold was set to P < 0.01.
Ethical committee
The local ethical committee at Hospital 12 de Octubre gave approval to the experimental protocol, and warranted its compliance with the Declaration of Helsinki. Written (signed) informed consent was obtained from all enrolees. Trial and protocol were publicly registered in ANZCRT on 14/05/2018; Trial id: ACTRN12618000819224.
References
Benito-León, J. Essential tremor: One of the most common neurodegenerative diseases? Neuroepidemiology 36, 77–78 (2011).
Louis, E. D. Essential tremor. Lancet Neurol. 4, 100–110 (2005).
Deuschl, G. et al. Consensus statement of the Movement Disorder Society on tremor. Mov. Disord. 13, 2–23 (1998).
Hopfner, F. et al. Early- and late-onset essential tremor patients represent clinically distinct subgroups. Mov. Disord. 31, 1560–1566 (2016).
Louis, E. D. The evolving definition of essential tremor: What are we dealing with? Park. Relat. Disord., https://doi.org/10.1016/j.parkreldis.2017.07.004 (2017).
Busenbark, K. L., Nash, J., Nash, S., Hubble, J. P. & Koller, W. C. Is essential tremor benign? Neurology 41, 1982–1983 (1991).
Louis, E. D. et al. Correlates of functional disability in essential tremor. Mov. Disord. 16, 914–20 (2001).
Deuschl, G., Raethjen, J., Hellriegel, H. & Elble, R. Treatment of patients with essential tremor. The Lancet Neurology 10, 148–161 (2011).
Benito-León, J. & Louis, E. D. Clinical update: diagnosis and treatment of essential tremor. Lancet 369, 1152–4 (2007).
Helmich, R. C., Toni, I., Deuschl, G. & Bloem, B. R. The Pathophysiology of Essential Tremor and Parkinson’s Tremor. Curr. Neurol. Neurosci. Rep. 13, 378 (2013).
Louis, E. D. et al. Neuropathological changes in essential tremor: 33 cases compared with 21 controls. Brain 130, 3297–307 (2007).
Bonuccelli, U. Essential tremor is a neurodegenerative disease. J. Neural Transm. 119, 1383–1387 (2012).
Louis, E. D. et al. Cerebellar Pathology in Familial vs. Sporadic Essential Tremor. Cerebellum 16, 786–791 (2017).
Louis, E. D. Re-thinking the biology of essential tremor: From models to morphology. Park. Relat. Disord. 20, S88–S93 (2014).
Rajput, A. H., Robinson, C. A., Rajput, M. L., Robinson, S. L. & Rajput, A. Essential tremor is not dependent upon cerebellar Purkinje cell loss. Parkinsonism Relat. Disord. 18, 626–8 (2012).
Deuschl, G. & Elble, R. J. The pathophysiology of essential tremor. Neurology 54, S14–20 (2000).
Louis, E. D., Jiang, W., Gerbin, M., Mullaney, M. M. & Zheng, W. Relationship between blood harmane and harmine concentrations in familial essential tremor, sporadic essential tremor and controls. Neurotoxicology 31, 674–9 (2010).
Louis, E. D. & Lenka, A. The Olivary Hypothesis of Essential Tremor: Time to Lay this Model to Rest? Tremor Other Hyperkinet. Mov. (N. Y). 7, 473 (2017).
Handforth, A. Harmaline tremor: underlying mechanisms in a potential animal model of essential tremor. Tremor Other Hyperkinet. Mov. (N. Y)., https://doi.org/10.7916/D8TD9W2P (2012).
Talbot, W. H., Darian-Smith, I., Kornhuber, H. H. & Mountcastle, V. B. The sense of flutter-vibration: comparison of the human capacity with response patterns of mechanoreceptive afferents from the monkey hand. J. Neurophysiol. 31, 301–34 (1968).
Mountcastle, V. B., LaMotte, R. H. & Carli, G. Detection thresholds for stimuli in humans and monkeys: comparison with threshold events in mechanoreceptive afferent nerve fibers innervating the monkey hand. J. Neurophysiol. 35, 122–136 (1972).
Douglas, P. R., Ferrington, D. G. & Rowe, M. Coding of information about tactile stimuli by neurones of the cuneate nucleus. J. Physiol. 285, 493–513 (1978).
Gilman, S. Joint position sense and vibration sense: anatomical organisation and assessment. J. Neurol. Neurosurg. Psychiatry 73, 473–7 (2002).
Geborek, P., Jörntell, H. & Bengtsson, F. Stimulation within the cuneate nucleus suppresses synaptic activation of climbing fibers. Front. Neural Circuits 6, 120 (2012).
Rocon, E., Gallego, J. Á., Belda-Lois, J. M., Benito-León, J. & Luis Pons, J. Biomechanical loading as an alternative treatment for tremor: a review of two approaches. Tremor and other hyperkinetic movements 2, 1–13 (2012).
Fasano, A. & Deuschl, G. Therapeutic advances in tremor. Movement Disorders 30, 1557–1565 (2015).
Rocon, E. et al. Design and Validation of a Rehabilitation Robotic Exoskeleton for Tremor Assessment and Suppression. IEEE Trans. Neural Syst. Rehabil. Eng. 15, 367–378 (2007).
Taheri, B., Case, D. & Richer, E. Adaptive suppression of severe pathological tremor by torque estimation method. IEEE/ASME Trans. Mechatronics 20, 717–727 (2015).
Prochazka, A., Elek, J. & Javidan, M. Attenuation of pathological tremors by functional electrical stimulation I: Method. Ann. Biomed. Eng. 20, 205–224 (1992).
Heo, J. H. et al. Sensory electrical stimulation for suppression of postural tremor in patients with essential tremor. Biomed. Mater. Eng. 26, S803–S809 (2015).
Dosen, S. et al. Online Tremor Suppression Using Electromyography and Low-Level Electrical Stimulation. IEEE Trans. Neural Syst. Rehabil. Eng. 23, 385–395 (2015).
Dideriksen, J. L. et al. Electrical stimulation of afferent pathways for the suppression of pathological tremor. Front. Neurosci. 11, 178 (2017).
Bruce Goldstein, E. Sensation and perception. (Schreiber, Linda, 2010).
Roudaut, Y. et al. Touch sense: functional organization and molecular determinants of mechanosensitive receptors. Channels (Austin, Tex.) 6, 234–245 (2012).
Gallego, J. Á., Rocon, E., Belda-Lois, J. M. & Pons, J. L. A neuroprosthesis for tremor management through the control of muscle co-contraction. J. Neuroeng. Rehabil. 10, 1–13 (2013).
Jung, J.-Y., Heo, W., Yang, H. & Park, H. A Neural Network-Based Gait Phase Classification Method Using Sensors Equipped on Lower Limb Exoskeleton Robots. Sensors (Basel). 15, 27738–27759 (2015).
Prochazka, A., Elek, J. & Javidan, M. Attenuation of pathological tremors by functional electrical stimulation. I: Method. Ann. Biomed. Eng. 20, 205–224 (1992).
Haas, C. T., Turbanski, S., Kessler, K. & Schmidtbleicher, D. The effects of random whole-body-vibration on motor symptoms in Parkinson’s disease. NeuroRehabilitation 21, 29–36 (2006).
King, L. K., Almeida, Q. J. & Ahonen, H. Short-term effects of vibration therapy on motor impairments in Parkinson’s disease. NeuroRehabilitation 25, 297–306 (2009).
Wenning, G. K. et al. Prevalence of movement disorders in men and women aged 50–89 years (Bruneck Study cohort): a population-based study. Lancet Neurol. 4, 815–820 (2005).
Heldman, D. A. et al. Essential tremor quantification during activities of daily living. Parkinsonism Relat. Disord. 17, 537–42 (2011).
Granit, R. & Henatshch, H. D. Gamma control of dynamic properties of muscle spindles. J. Neurophysiol. 19, 356–66 (1956).
Bianconi, R. & Van Der Meulen, J. P. The response to vibration of the end organs of mammalian muscle spindles. J. Neurophysiol. 26, 177–90 (1963).
Burke, D., Hagbarth, K. E., Löfstedt, L. & Wallin, B. G. The responses of human muscle spindle endings to vibration of non-contracting muscles. J. Physiol. 261, 673–693 (1976).
Seizova-Cajic, T., Smith, J. L., Taylor, J. L. & Gandevia, S. C. Proprioceptive Movement Illusions Due to Prolonged Stimulation: Reversals and Aftereffects. PLoS One 2, e1037 (2007).
Goodwin, G. M., McCloskey, D. I. & Matthews, P. B. Proprioceptive illusions induced by muscle vibration: contribution by muscle spindles to perception? Science 175, 1382–4 (1972).
Heckman, C. J., Gorassini, M. A. & Bennett, D. J. Persistent inward currents in motoneuron dendrites: Implications for motor output. Muscle Nerve 31, 135–156 (2005).
Wei, K. et al. Serotonin affects movement gain control in the spinal cord. J. Neurosci. 34, 12690–700 (2014).
Gorassini, M., Yang, J. F., Siu, M. & Bennett, D. J. Intrinsic Activation of Human Motoneurons: Possible Contribution to Motor Unit Excitation. J. Neurophysiol. 87, 1850–1858 (2002).
Andersen, P., Eccles, J. C. & Schmidt, R. F. Presynaptic inhibitory actions: Presynaptic inhibition in the cuneate nucleus. Nature 194, 741–743 (1962).
Suresh, A. K. et al. Methodological considerations for a chronic neural interface with the cuneate nucleus of macaques. J. Neurophysiol. 118, 3271–3281 (2017).
Bain, P. et al. Criteria for the diagnosis of essential tremor. Neurology 54, S7 (2000).
Serrano, J. I. et al. Identification of activities of daily living in tremorous patients using inertial sensors. Expert Syst. Appl. 83, 40–48 (2017).
Rocon de Lima, E., Andrade, A. O., Pons, J. L., Kyberd, P. & Nasuto, S. J. Empirical mode decomposition: A novel technique for the study of tremor time series. Med. Biol. Eng. Comput. 44, 569–582 (2006).
Acknowledgements
This work was funded by the projects ESSENTIAL (DPI2015-72638-EXP) and NeuroMOD (DPI2015-68664-C4-1-R), financed by the Spanish Ministry of Economy, Industry and Competitiveness, and by RoboCity2030-DIH-CM, Madrid Robotics Digital Innovation Hub, S2018/NMT-4331, funded by “Programas de Actividades I+D en la Comunidad de Madrid” and cofunded by Structural Funds of the EU. Julio S. Lora-Millan was in receipt of a Training Program for Academic Staff fellowship (FPU16/01313) by the Ministry of Science, Innovation and Universities of the Government of Spain. Juan A. Gallego received funding from the EU Commission (FP7-PEOPLE-2013-IOF-627384) and from the Community of Madrid (Atracción de Talento Grant 2017-T2/TIC-5263).
Author information
Authors and Affiliations
Contributions
Mr. Lora-Millán (J.S.L.M.): (1) implemented the experimental setup; (2) performed the experiments; (3) analyzed the data; (4) prepared the figures; and (5) wrote the manuscript. Mr. López-Blanco (R.L.B.): (1) recruited the patients; (2) performed the experiments; and (3) revised the manuscript. Dr. Gallego (J.A.G.): (1) assisted in data analysis; and (2) wrote the manuscript. Dr. Méndez-Guerrero (A.M.G.): (1) recruited patients; and (2) revised the manuscript. Dr. González de la Aleja (J.G.A.): (1) conceived and designed the research project; (2) assisted in data analysis; and; (3) wrote the manuscript. Dr. Rocon (E.R.): (1) conceived and designed the research project; (2) secured funding; (3) assisted in data analysis, and; (4) wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lora-Millán, J.S., López-Blanco, R., Gallego, J.Á. et al. Mechanical vibration does not systematically reduce the tremor in essential tremor patients. Sci Rep 9, 16476 (2019). https://doi.org/10.1038/s41598-019-52988-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-52988-8
This article is cited by
-
4D printing of soft orthoses for tremor suppression
Bio-Design and Manufacturing (2022)
-
Peripheral electrical stimulation to reduce pathological tremor: a review
Journal of NeuroEngineering and Rehabilitation (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.