Abstract
Although the prognostic factors of interstitial pneumonia (IP) patients have been reported, IP has poor prognosis. Hospitalized patients with IP have severely impaired pulmonary diffusion capacity and prominent desaturation. We hypothesized that determining oxygen saturation recovery (SpO2 recovery index) after the 6-minute walk test (6MWT) can provide additional prognostic information regarding rehospitalization for respiratory-related events. We evaluated 73 IP patients at our hospital for demographic characteristics, pulmonary function tests and 6MWT. The Kaplan–Meier method was used to estimate rehospitalisation for respiratory-related events using SpO2 recovery index. Cox regression analysis revealed a relationship between SpO2 recovery index and rehospitalisation. The optimum cutoff value of SpO2 recovery index was 4% (sensitivity, 71.4%; specificity, 79.2%). SpO2 recovery index was most closely related to pulmonary diffusion capacity (r = 0.684, P < 0.001). In a multivariable model, it was the strongest independent predictor of rehospitalisation for respiratory-related events (hazard ratio, 0.3; 95% confidence interval, 0.10–0.90; P = 0.032). In this study, we estimated pulmonary diffusion capacity using SpO2 recovery index values obtained from 6MWT. A SpO2 recovery index of <4% can be useful in predicting rehospitalisation for respiratory-related events.
Similar content being viewed by others
Introduction
Central pathophysiological features of interstitial pneumonia (IP) include impaired degradation of pulmonary diffusion capacity due to pulmonary interstitium and capillary bed disorders, ventilation perfusion ratio mismatch, and worsening gas exchange with exercise1. Dyspnea during exercise reduces exercise tolerance, ability to perform daily activities, and health-related quality of life2. Although prognostic factors for IP have been reported, IP has poor prognosis3,4,5,6,7,8, including reduced pulmonary diffusion capacity and hypoxemia are poor prognostic factors in patients with IP3,4. Also, measuring partial oxygen pressure (PaO2) during exercise predicts survival in patients with IP5. Moreover, desaturation during the 6-minute walk test (6MWT) is a prognostic factor for patients with IP in stable conditions6. Exercise-induced hypoxemia (EIH) of patients with IP is related to the pulmonary diffusion function, which is also one of the prognostic factors6,7,8.
A simple test to evaluate desaturation is used clinically in 6MWT9,10. Heart rate recovery (HRR) obtained from 6MWT has drawn attention as a prognostic factor in patients with IP and in those with chronic obstructive pulmonary disease and heart failure11,12. Heart rate recovery 1 (HRR1), obtained by subtracting heart rate (HR) after 1-min walk, from the rate at 6MWT end, showed the strongest significance for mortality13,14. Considering the physiologic response after exercise as a prognostic indicator is essential. Hospitalized patients with IP have severely impaired pulmonary diffusion capacity and prominent desaturation; changes in HR after exercise and desaturation evaluation are important. Studies on the relationship between mortality and clinical indicators during and after exercise included stable IP outpatients13,14. To our knowledge, no study has evaluated hospitalized IP-patient mortality. HR during and HRR after exercise and all-cause mortality are reported, but readmission/mortality predictive factors have not been considered, restricting acute IP exacerbation and respiratory failure15,16,17. During rehabilitation of hospitalised patients with IP with an unstable respiratory state, pulmonary diffusion capacity should be considered. Determining the breathing pattern, exercise oxygen saturation, post-exercise oxygen saturation recovery and HR changes is crucial because rehospitalisation for acute IP exacerbation and respiratory failure accounts for a majority of the deaths in this disease; therefore, the results of such evaluations constitute useful information for risk management. Therefore, we examined whether oxygen saturation after 6MWT in hospitalized patients with IP reflected pulmonary diffusion capacity. Oxygen saturation recovery after 6MWT was hypothesized to provide additional prognostic information regarding rehospitalization for respiratory-related events in these patients.
Materials and Methods
Ethical approval
The study protocol was approved by the ethics committee of Shinshu University (No. 3732) and conducted according to the Declaration of Helsinki (latest version). Written informed consent was obtained from all participants after detailed explanation of the study protocol.
Patient selection
Patients with IP who were hospitalized at Shinshu University Hospital in Japan during January 2015-July 2018 were selected. IP was diagnosed based on the American Thoracic Society/Infectious Diseases Society of America guidelines18.
Patients with underlying gait disturbance due to cerebral infarction/collagen vascular disease/occupational exposure/high-flow oxygen and those with recognized cognitive decline (23 points > Mini-Mental State Examination)19 were excluded.
Procedure
This study is a cohort study. Demographic characteristics (age, gender, body mass index; BMI), diagnosis (idiopayhic pulmonary fibrosis, acute interstitial pneumonia, combined pulmonary fibrosis and emphysema), treatment (prednisolone, supplemental O2 flow), pulmonary function tests, 6MWT and laboratory data on admission (krebs von den lungen-6, PaO2/FIO2 ratio) were collected upon hospital discharge. 6MWT was performed upon hospital discharge and indicators were collected. Pulmonary function tests, including spirometry and pulmonary diffusion capacity for carbon monoxide (DLco), and changes in nitrogen levels (ΔN2) were measured as previously described20. Forced vital capacity (FVC) and DLco were assessed according to the American Thoracic Society/European Respiratory Society (ATS/ERS) criteria; their results were reported as predicted value percentages21,22,23. Pulmonary function tests using CHESTAC-8900 (CHEST, Tokyo, Japan) were conducted. Pulmonary hypertension (PH) was diagnosed based on the estimated pulmonary artery systolic pressure calculated using the simple Bernoulli equation [estimated pulmonary artery systolic pressure = 4 × (3 tricuspid regurgitation velocity)2 + estimated right atrial pressure] with reference to trans tricuspid pressure gradient determined using echocardiography24.
6MWT
Walking path and criteria for terminating measurement was set by the ATS guidelines25. 6MWT protocol was designed to accurately assess oxygen desaturation and to provide a clinically useful oxygen titration. All patients’ baseline HR and saturation of percutaneous oxygen (SpO2) using pulse oximetry (Pulsox-M, Teijin Ltd, Tokyo, Japan) were measured. For patient safety, the test was discontinued on noting unbearable chest pain/shortness of breath/new arrhythmia development. To accurately assess SpO2, the respiratory therapist confirmed an acceptable pulse oximeter signal and pulsing of oximeter bar indicating synchrony between HR before beginning all tests. Patients walked on a level surface with gentle vocal encouragement using set phrases every 1 min. SpO2 and HR were continuously measured during 6MWT, and in all patients modified Borg scale at 6MWT end and distance were measured. Change in SpO2 (ΔSpO2) was the difference between a subject’s resting SpO2 and the lowest SpO2 during 6MWT (resting – lowest SpO2). SpO2 recovery index was the difference between a subject’s SpO2 at 6MWT end (<6 min if the test was terminated for a low SpO2) and 1 min into recovery and dividing by the resting SpO2: [(SpO2 1 min into recovery after 6MWT − lowest SpO2)/resting SpO2] × 100.
End point
Subjects were followed-up with after 12 months; any major respiratory-related events requiring hospitalization were recorded.
Statistical analysis
The subjects were classified into two groups: not-rehospitalization (event free) and rehospitalization due to respiratory-related events groups. Categorical and continuous data were compared using the χ2 and Mann-Whitney U tests, respectively. Correlations between quantitative variables of the lowest SpO2, ΔSpO2, SpO2 at 1 min after 6MWT, distance, SpO2 recovery index, and %DLco in the entire population were evaluated using the bivariate Pearson test. Rehospitalization SpO2 recovery index validity was determined considering rehospitalization and SpO2 recovery index as objective and explanatory variables, respectively. The receiver operating characteristic (ROC) curve and area under the ROC curve (AUC) were determined. An optimal cutoff point maximizing sensitivity and specificity for SpO2 recovery index was determined from sensitivity and specificity curve intersection26.
The product-limit method was used to derive rehospitalization for respiratory-related events; Kaplan-Meier curves were used to display rehospitalization for the study sample stratified by SpO2 recovery index. For multivariable analysis of rehospitalization due to respiratory-related events to develop the most parsimonious model, candidate variables included those with a P < 0.05 on bivariate analysis. Cox regression analysis examined the relationship between SpO2 recovery index and rehospitalization; adjusting for demographic characteristics; PH diagnosis and complication; treatment; and physiologic, 6MWT, and laboratory data. Overfitting was avoided by reducing potential confounding factors including SpO2 recovery index to a single composite characteristic by applying a propensity score.
Analyses were performed using SPSS 24.0 software (IBM Japan, Tokyo, Japan). Descriptive statistics [mean ± standard deviation (SD)] were used. All tests assumed unequal variances; P < 0.05 indicated statistical significance.
Results
Follow-up on rehospitalization
No patient was lost to follow-up during the subsequent 12 months. Fourteen respiratory-related events (10 IP acute exacerbations and 4 respiratory failures) occurred during the tracking period (event rate = 19.2%).
Participant characteristics
Table 1 shows clinical characteristics of participants in the two groups. There were no between-group significant differences in age, gender percentage, BMI, diagnosis, prednisolone use, forced expiratory volume (FEV1.0), ΔN2, resting SpO2, ΔSpO2, modified Borg scale at 6MWT end, and clinical laboratory data.
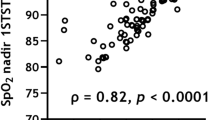
Correlation analysis
Lowest SpO2, ΔSpO2, SpO2 1 min after 6MWT, distance, and SpO2 recovery index significantly correlated with %DLco with moderate correlation coefficients. SpO2 recovery index obtained from 6MWT had the highest correlation coefficient (r = 0.684, P < 0.001; Fig. 1) including other evaluations.
ROC curves and related rehospitalization analysis
Figure 2 shows the ROC curve of SpO2 recovery index to deduce rehospitalization of respiratory-related events. AUC showing the usefulness of SpO2 recovery index usefulness was significantly higher at 0.75 (standard error = 0.07; P = 0.005). The optimum cutoff value of SpO2 recovery index was 4% (sensitivity = 71.4%; specificity = 79.2%). The positive likelihood ratio of in the cutoff of SpO2 recovery index was 3.43.
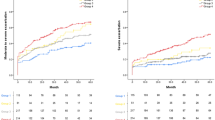
Kaplan-Meier curves
Figure 3 shows Kaplan-Meier analyses of rehospitalization for the study sample stratified by SpO2 recovery index (≥4% vs <4%). In time-to-event survival analysis, SpO2 recovery index was significantly associated with respiratory-related events for patients with IP (P < 0.001).
Multivariate Cox regression analysis
Table 2 shows a Cox proportional hazard model. In multivariable analyses using the propensity score, SpO2 recovery index [hazard ratio (HzR) = 0.3; 95% confidence interval (CI) = 0.10–0.90; P = 0.032] and HHR1 (HzR = 0.91; 95% CI = 0.82–0.99; P = 0.045) were significantly associated with respiratory-related events. Among them, SpO2 recovery index was the most associated with respiratory-related events.
Discussion
To the best of our knowledge, this is the first study to reveal a relationship between SpO2 recovery index values obtained from 6MWT and pulmonary diffusion capacities in patients with IP. It is also the first exploration of the predictors of rehospitalization predictors due to acute IP exacerbation and respiratory failure. SpO2 recovery index from 6MWT for IP inpatients was most strongly associated with pulmonary diffusion capacity and was a strong predictor for rehospitalization due to acute IP exacerbation and respiratory failure. When the 4% cutoff generated from ROC curves was used as a reference for SpO2 recovery index value for rehospitalization, the risk of rehospitalization during the follow-up period decreased by 0.3-fold with every 1% increase in SpO2 recovery index. Multivariate Cox regression analysis identified HRR1 obtained from 6MWT as a rehospitalization predictor for respiratory-related events, supporting previous studies on mortality. However, in this study, SpO2 recovery index was as a stronger predictor than HRR1.
Patients with IP with EIH have a poor prognosis, indicating the importance of evaluating EIH5,27. In clinical, radiological and physiological scoring systems for predicting prognosis in patients with IP, PaO2 during cardiopulmonary exercise testing is a significant survival rate predictor and the strongest prognosis predictor5. A recent American Thoracic Society consensus statement suggested a 4% decrease in saturation during exercise as an adverse prognostic sign in idiopathic pulmonary fibrosis (IPF)1. Many of these studies focused on desaturation/PaO2 during cardiopulmonary exercise testing. However, registry data suggest that cardiopulmonary exercise tests are rarely used to assess prognostic predictions in IPF patients28, possibly relating to the expense and limited availability of this diagnostic modality. 6MWT is a simple, convenient, inexpensive test requiring minimal medical personnel and can be performed in an office setting29. In this study, clinical data derived from 6MWT were analyzed. SpO2 recovery index from 6MWT was significantly associated with the gas exchange index %DLco, suggesting the estimation of pulmonary diffusion capacity levels using SpO2 recovery index after 6MWT without performing detailed pulmonary function tests (difficult to conduct due to insufficient facilities and environmental problems). These results may help in risk management during exercise therapy and determining oxygen levels during home oxygen therapy introduction.
For rehospitalization predictors, causes of deaths in patients with IP were not specifically identified in previous studies. HR changes during exercise and HRR after exercise, demonstrated in many previous studies, may reflect cardiac function and are presumed to be outcomes, a large part of which is accounted for by mortality attributable to cardiac disease as a complex. Previous studies included large patient numbers with high right ventricular systolic pressure (RSVP), using cardiac medication14, and who suffered PH after the study/had PH-related mortality13. To explain HR changes during and HRR changes after exercise as mortality predictors, Heindl30 noted abnormal sympathetic activation in patients with chronic respiratory failure, including some with pulmonary fibrosis. Most deaths occur from the progression of lung fibrosis rather than from commonly occurring comorbidities15,16,17. Frequent hospitalization for respiratory problems are common and associated with death15,16,17. Identifying rehospitalization predictors due to respiratory-related events (respiratory failure and acute IP exacerbation) was necessary. Unlike previous studies, our study limited the reasons for rehospitalization to IP exacerbation and respiratory-related events, including respiratory failure. Respiratory system function had a greater impact on the analysis and may justify why SpO2 recovery index after 6MWT, which is more relevant to the pulmonary diffusion capacity than HHR1, was a rehospitalization predictor for respiratory-related events. SpO2 recovery index was a useful index with clinical applicability regardless of whether the resting SpO2 level was high/low because it was adjusted with resting SpO2 for compensating oxygen consumption effect.
These results allow for a novel means of predicting respiratory-related events, such as acute IP exacerbation and respiratory failure and all-cause mortality, including that due to cardiac diseases. Evaluating SpO2 recovery index after 6MWT predicts rehospitalization due to acute IP exacerbation and respiratory failure, aiding in clinical practice.
Limitations of this study are that independent variables used in the multivariate analysis were limited because of the small sample size and the short, 1-year follow-up period, which can be addressed by subject accumulation and longer follow-up. This study excluded patients with immeasurable 6MWT, such as those using a high-flow-rate oxygenator and with a history of bone and joint diseases. Therefore, this method is not applicable to all patients in clinical practice and should be used for prognosis prediction after appropriate patient selection. SpO2 recovery is useful in predicting rehospitalization due to respiratory-related events. However, there is no clear intervention for minimizing rehospitalization due to respiratory-related events risk, and improvement of exercise tolerance and lower leg muscle strength by rehabilitation may be important, other than pulmonary diffusion capacity due to drugs.
Conclusion
SpO2 recovery index after 6MWT in hospitalized patients with IP was most closely related to pulmonary diffusion capacity and the strongest independent rehospitalization predictor due to respiratory-related events. In clinical practice, pulmonary diffusion capacity can be estimated using SpO2 recovery indices obtained from 6MWT in appropriately selected patients and may help during exercise therapy. It was also useful in predicting rehospitalization due to respiratory-related events.
References
American Thoracic Society. idiopathic pulmonary fibrosis: diagnosis and treatment: international consensus statement: American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med. 161, 646–664 (2006).
Swigris, J. J., Kuschner, W. G., Jacobs, S. S., Wilson, S. R. & Gould, M. K. Health-related quality of life in patients with idiopathic pulmonary fibrosis: a systematic review. Thorax. 60, 588–594 (2005).
Hamada, K. et al. Significance of pulmonary arterial pressure and diffusion capacity of lung as prognosticator in patients with idiopathic pulmonary fibrosis. Chest. 131, 650–656 (2007).
Flaherty, K. R. et al. Ideopathic pulmonary fibrosis. Prognostic value of changes in physiology and six minute-walk test. Am J Repir Crit Care Med. 174, 803–809 (2006).
King, T. E. Jr., Tooze, J. A., Schwarz, M. I., Brown, K. R. & Cherniack, R. M. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med. 164, 1171–1181 (2001).
Lama, V. N. et al. Prognostic Value of Desaturation during a 6-Minute Walk Test in Idiopathic Interstitial Pneumonia. Am J Respir Crit Care Med. 168, 1084–1090 (2003).
Lamberto, C. et al. Membrane and capillary blood components of diffusion capacity of the lung for carbon monoxide in pulmonary sarcoidosis. Chest. 125, 2061–2068 (2004).
Lebecque, P., Lapierre, J. G., Lamarre, A. & Coates, A. L. Diffusion capacity and oxgen desaturation effects on exercise in patients with cystic fibrosis. Chest. 91, 693–697 (1987).
Solway, S., Brooks, D., Lacasse, Y. & Thomas, S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 119, 256–270 (2001).
Steele, B. Timed walk tests of exercise capacity in chronic cardiopulmonary illness. J Cardiopulm Rehabil. 16, 25–33 (1996).
Cahalin, L. P. et al. Heart rate recovery after the 6 min walk test rather than distance ambulated is a powerfulprognostic indicator in heart failure with reduced and preserved ejection fraction: a comparison with cardiopulmonary exercise testing. European Journal of Heart Failure. 15, 519–527 (2013).
Lacasse, M. et al. Post-exercise heart rate recovery and mortality in chronic obstructive pulmonary disease. Respir Med. 99, 877–886 (2005).
Swigris, J. J. et al. Heart rate recovery after six-minute walk test predicts pulmonary hypertension in patients with idiopathic pulmonary fibrosis. Respirology. 16, 439–445 (2011).
Swigris, J. J. et al. Heart Rate Recovery After 6-Min Walk Test Predicts Survival in Patients With Idiopathic Pulmonary Fibrosis. Chest. 136, 841–848 (2009).
Martinez, F. J. et al. The clinical course of patients with idiopathic pulmonary fibrosis. Ann Intern Med. 142, 963–967 (2005).
King, T. E. Jr. et al. Effect of interferon gamma-1b on survival in patients with idiopathic pulmonary fibrosis (INSPIRE): a multicentre, randomised, placebo-controlled trial. Lancet. 374, 222–228 (2009).
Brown, A. et al. Outcomes after hospitalization in idiopathic pulmonary fibrosis: a cohort study. Chest. 147, 173–179 (2015).
American Thoracic Society/European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. Am J Respir Crit Care Med. 165, 277–304 (2002).
Avin, K. G. et al. Management of falls in community-dwelling older adults: clinical guidance statement from the Academy of Geriatric Physical Therapy of the American Physical Therapy Association. Physical therapy. 95, 815–834 (2015).
Gay, S. E. et al. Idiopathic pulmonary fibrosis: predicting response to therapy and survival. Am J Respir Crit Care Med. 157, 1063–1072 (1998).
Macintyre, N. et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 26, 720–735 (2005).
Miller, M. R. et al. Standardisation of spirometry. Eur Respir J. 26, 319–338 (2005).
Pellegrino, R. et al. Interpretative strategies for lung function tests. Eur Respir J. 26, 948–968 (2005).
Guidelines for Treatment of Pulmonary Hypertension. Japan Circulation Society. 1–69 (2012).
ATS Statement: Guidelines for the Six-Minute Walk Test. Am J Repir Crit Care Med. 166, 111–117 (2002).
Hosmer, D. & Lemeshow, S. Applied logistic regression. New York: John Wiley and Sons (2000).
Miki, K. et al. Impairments and prognostic factors for survival in patients with idiopathic pulmonary fibrosis. Respir Med. 97, 482–490 (2003).
Mapel, D. W., Samet, J. M. & Coultas, D. B. Corticosteroids and the treatment of idiopathic pulmonary fibrosis: past, present, and future. Chest. 110, 1058–1067 (1996).
Poulain, M. et al. 6-Minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest. 123, 1401–1407 (2003).
Heindl, S. et al. Marked sympathetic activation in patients with chronic respiratory failure. Am J Respir Crit Care Med. 164, 597–601 (2001).
Acknowledgements
The authors would like to thank Enago for the English language review.
Author information
Authors and Affiliations
Contributions
Yasunari sakai designed the study, and wrote the initial draft of the manuscript. Yasunari sakai contributed to analysis and interpretation of data, and assisted in the preparation of the manuscript. Mr. Yamamoto, Mrs. Hoshina, and Mr. Kawachi contributed to the data collection. Mr. Yamamoto contributed to the statistical analysis. Mr. Yamamoto, Mrs. Hoshina, Mr. Kawachi, Mr. Ichiyama and Mr. Hanaoka have contributed to data collection and interpretation, and critically reviewed the manuscript. All authors approved the final version of the manuscript, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakai, Y., Yamamoto, S., Hoshina, M. et al. Using SpO2 Recovery Index after a 6-Minute Walk Test to Predict Respiratory-Related Events in Hospitalized Patients with Interstitial Pneumonia. Sci Rep 9, 15226 (2019). https://doi.org/10.1038/s41598-019-51818-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51818-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.