Abstract
The aim of the study was to evaluate whether pretherapeutic metabolic tumor parameters from 18-fluorodeoxyglucose positron emission tomography (FDG-PET) imaging could predict larynx preservation in laryngeal and hypopharyngeal cancer patients prior to primary chemoradiation. Tumor metabolic parameters [maximum standardized uptake value (SUVmax), metabolic tumor volume (MTV), and total lesion glycolysis (TLG)] were retrospectively assessed in a consecutive cohort of laryngeal and hypopharyngeal cancer patients undergoing primary (chemo-)radiation. Main outcome measures were larynx preservation and survival. The study included 97 patients with a median follow-up of 32 months (IQR 20–54.5). For hypopharyngeal cancer, multivariable analysis showed that patients with a primary tumor’s SUVmax > 9.5 entailed a higher risk of undergoing salvage pharyngolaryngectomy after chemoradiation (HR = 8.64, 95% CI = 1.1–67.3, P = 0.040). In laryngeal cancer, SUVmax did not predict the need for salvage laryngectomy. The only predictor for larynx preservation in laryngeal cancer patients was T-classification at initial diagnosis (HR = 6.67, 95% CI = 0.82–53.9, P = 0.039). In conclusion, SUVmax of primary tumor could be used as a predictor of larynx preservation prior to primary chemoradiation in hypopharyngeal cancer patients. This information may be important for patient counseling, as high SUVmax was correlated with reduced probability of larynx preservation. However, in laryngeal cancer patients, SUVmax does not seem to be predictive of outcome.
Similar content being viewed by others
Introduction
In advanced stage III or IV laryngeal and hypopharyngeal squamous cell carcinoma, organ preservation strategy involves primary chemoradiation as first-line therapy, reserving surgery such as laryngectomy or pharyngolaryngectomy for the salvage setting1,2. Primary upfront laryngectomy or pharyngolaryngectomy followed by adjuvant radiotherapy with or without concomitant chemotherapy, as needed, may be preferred in patients with surgically removable advanced stage carcinomas, as primary chemoradiation with salvage surgery may negatively impact quality of life, functionality and survival3. Therefore, it is crucial to adequately select patients for either of the two strategies. Tumor response to induction chemotherapy has been used in seminal studies as a selection tool2. However, subsequent studies revealed the superiority of concurrent chemoradiation compared to induction chemotherapy followed by radiotherapy for laryngeal preservation, establishing a new standard of care4. Although a few clinical factors, such as gross cartilage infiltration, large tumor volume, and extensive nodal disease are already recognized as unfavorable factors for organ preservation strategy, it would be of interest to provide further tools for clinicians to base their therapeutic decision on5.
18-fluorodeoxyglucose positron emission tomography (FDG-PET) with computed tomography (CT) or magnetic resonance (MR) imaging has become a broadly accepted imaging tool in routine clinical oncology6. Adding FDG-PET to the staging process resulted in higher staging accuracy with improved nodal classification7,8, superior detection of regional or distant metastases, and second primary cancers9,10. In addition, metabolic tumor parameters derived from FDG-PET have been suggested to serve as prognostic markers for the response to chemoradiation11,12. Such metabolic parameters include maximum standardized uptake value (SUVmax), metabolic tumor volume (MTV), and total lesion glycolysis (TLG)13,14.
Tumors with a higher uptake of FDG have a more active tumor metabolism, which negatively correlates with tumor oxygenation through the Warburg effect15,16. Poor tumor oxygenation or tumor hypoxia is moreover associated with resistance to chemoradiation17,18. Consequently, we hypothesized that FDG-PET derived tumor metabolism markers, such as SUVmax, MTV, and TLG, can be used as predictors of response to chemoradiation. The aim of this study was therefore to examine whether different pretherapeutic FDG-PET parameters can predict organ preservation in laryngeal and hypopharyngeal cancer undergoing primary chemoradiation.
Materials and Methods
Study population
After Ethics Review Board approval by the Kantonale Ethikkomission Zürich (protocol number 2016–01799), all patients treated for laryngeal or hypopharyngeal squamous cell carcinoma between June 1st, 2007, and June 1st, 2017, at the Department of Otorhinolaryngology – Head and Neck Surgery of the Zurich University Hospital, Switzerland, were retrospectively assessed. All research was performed in accordance with relevant guidelines and regulations and informed consent of all enrolled patients was obtained. Inclusion criteria were available pre- and posttherapeutic FDG-PET/CT or FDG-PET/MR images and treatment with curative intent. Patients treated with induction chemotherapy, patients that did not complete a course of radiotherapy of at least 60 Gray locally, and patients undergoing primary surgical treatment were excluded.
All patients were staged according to the Union Internationale Contre le Cancer (UICC), TNM staging for head and neck cancer, 7th edition, 201019. After full medical history, physical examination, triple endoscopy with biopsy, and imaging with FDG-PET, all patients were presented and discussed at the local interdisciplinary tumor board. Posttherapeutic FDG-PET/CT or -/MR images were obtained three months after completion of chemoradiation.
Detailed data on age, gender, tumor subsite, and risk factors including smoking, drinking habits, and human papilloma virus (HPV) status were obtained. Immunohistochemical expression of p16 or polymerase chain reaction (PCR) for HPV were used to evaluate HPV status of tumor biopsy samples. Local and regional radiation dose, type and number of cycles of concomitant chemotherapy, time to salvage pharyngolaryngectomy and/or neck dissection, pathological tumor stage, number of nodes dissected, number of positive nodes, and follow-up time were assessed.
The study cohort was then divided into two groups according to tumor site, analyzing laryngeal and hypopharyngeal cancer separately. The primary outcome measure of the study was pharyngo-/laryngectomy-free survival. Secondary outcome measures included local and regional recurrence-free survival, distant metastasis-free survival, disease-specific survival, and overall survival.
FDG-PET/CT or -/MR image acquisition
Patients were injected with a standardized dose of 3.5 MBq of 18-fluorodeoxyglucose (FDG) per kilogram body weight after fasting for at least four hours. All patients had a blood glucose level below 12 mmol/l before imaging. The patients were instructed to remain in lying or recumbent position and silent for 50–60 minutes to minimize muscular FDG uptake in the period between FDG injection and image acquisition. Patients were also kept warm prior to tracer injection and throughout the uptake period to diminish FDG accumulation in brown adipose tissue. All patients received either iodinated or gadolinium-based contrast medium. An integrated Discovery VCT PET/CT system (GE Healthcare, Waukesha, WI), a Discovery PET/CT 690 (GE Healthcare), or a hybrid PET/MRI system (Signa PET/MR, GE Healthcare) was used for image acquisition.
Tumor FDG metabolism
Selected parameters of tumor FDG metabolism were obtained under supervision of a board-certified nuclear physician and radiologist and comprised pre- und posttherapeutic SUVmax, TLG, and MTV of the primary tumor. Moreover, in patients with clinically positive nodal status, SUVmax of the most active metastatic lymph node was measured. SUVmax was calculated automatically using a standard formula [maximum activity in region of interest ÷ (injected dose × body weight)]. MTV was defined as the sum of the volume of voxels with an SUV exceeding a threshold of 42% of the SUVmax. TLG was defined mathematically as MTV × SUVmean. Correct analysis of FDG uptake was ensured through side-by-side reading of the corresponding CT or MR images of the tumor in the axial, coronal, and sagittal plane. Borders of regions of interest (ROI) were set by manual adjustment to exclude adjacent physiologic FDG-avid structures. A written report by a dually board-certified nuclear medicine physician/radiologist was available for pre- and posttherapeutic FDG-PET/CT or -/MR images.
Statistical analysis
For continuous variables, median, interquartile range (IQR), or standard deviation (SD) are given. To compare distribution among samples, the non-parametric Mann Whitney U test was used for two samples. Binary variables were associated in contingency tables using the two-tailed chi-squared test. Main outcome measures of the study were calculated using a multivariable Cox regression model. Results are expressed in hazard ratio (HR) with the 95% confidence interval provided (95% CI). Survival curves were built according to Kaplan-Meier and the log-rank test was used to compare factors. Receiver operating characteristic (ROC) curves were used to determine in which study group pretherapeutic SUVmax was a potential predictor of laryngectomy and to select the best cutoff value for SUVmax to predict high risk of laryngectomy. A P-value lower than 0.05 was considered to indicate statistical significance. Statistical analyses were performed using SPSS® 23.0.0.0 software (IBM®, Armonk, NY, USA).
Meeting presentation
This work was presented at the 2018 Swiss Society for Oto-rhino-laryngology Head and Neck Surgery, Spring Meeting, June 21st, 2018, Basel, Switzerland.
Results
Patient and tumor characteristics
A total of 97 patients with advanced stage III or IV laryngeal or hypopharyngeal cancer were included in this study (Table 1). The median age at diagnosis was 64 years (IQR 56–70). As expected, there was a clear male predominance with 85 (87.6%) male and 12 (12.4%) female patients. Forty patients (41.2%) had squamous cell carcinomas of the larynx and 57 patients (58.8%) of the hypopharynx. Most patients (58.8%) had cT3-cT4 tumors in comparison to 41.2% of patients with cT1-cT2 tumors, including glottic carcinomas. Clinical nodal status was positive in 61 patients (62.9%), of which 40 (41.3%) were staged with cN1-cN2b and 21 (21.6%) with cN2c-cN3 categories.
The median pretherapeutic SUVmax was 10.4 (IQR 7.4–15.7) for the whole cohort, while the median TLG was 34696 (IQR 18160–75166), and median MTV was 6.1 cm3 (IQR 3.6–8.7 cm3). Median follow-up time for all patients was 32 months (IQR 20–54.5).
Treatment characteristics
Patients received either intensity-modulated radiotherapy (IMRT) or volumetric modulated arc therapy (VMAT) with a mean total dose of 70 Gray locally (SD 1.65) and 54 Gray (SD 0.83) regionally. Seventy-four patients (76.3%) received concomitant chemotherapy. 63.5% of chemotherapies were based on cisplatin with a median of five cycles (SD 0.97), while 17.6% consisted of cetuximab with a median of four cycles (SD 1.81). Fourteen patients (18.9%) received both cisplatin and cetuximab, either based on the study protocol of a clinical trial20 or because the therapy was changed to cetuximab due to adverse effects of cisplatin.
Twenty-three patients (23.7%) underwent salvage surgery. Of those, 60.9% had hypopharyngeal cancer and underwent pharyngolaryngectomy and 39.1% had laryngeal cancer with salvage laryngectomy. Median time to pharyngo-/laryngectomy was 13.5 months (IQR 8.8–16.3). Frozen sections were used intraoperatively to assure free margins of the surgical resection specimen and all patients had negative margins upon final pathology (R0).
Neck dissection was performed either on its own or combined with pharyngo-/laryngectomy on 35 patients (36.1%) after a median time of 7 months (IQR 6–14). Eight of these patients (22.8%) had laryngeal cancer in comparison to 27 hypopharyngeal carcinomas (77.2%). Twenty of 35 patients (57.1%) had positive nodal disease (ypN+) with a mean of 2.3 positive lymph nodes (SD 2.59).
Primary Outcome Analysis: Organ Preservation
Various cutoff values for FDG uptake parameters were tested for the different study cohorts. Using receiver operating characteristic (ROC) curves, it was determined that pretherapeutic SUVmax was predictive of laryngectomy for hypopharyngeal cancer patients but not for laryngeal cancer patients (Fig. 1, Panel A–C). For hypopharyngeal cancer patients, the best potential cutoff value for pretherapeutic SUVmax was determined to be 9.5 (Fig. 1, Panel B, sensitivity 92.9%, specificity 37.2%, P = 0.016). Factors possibly predicting organ preservation were analyzed separately between hypopharyngeal (Table 2) and laryngeal cancer patients (Table 3), using a univariable and multivariable Cox regression model.
Receiver operating characteristic (ROC) curve analysis of laryngectomy prediction according to pretherapeutic SUVmax of primary tumor. (A) ROC curve for all patients showing lack of significant correlation (area under the curve (AUC) = 0.595 (95% CI = 0.460–0.730, P = 0.171). (B) ROC in hypopharyngeal cancer patients only. The area under the ROC curve was 0.715 (95% CI = 0.562–0.868, P = 0.016) and 9.5 was determined as best potential cutoff value for comparison. The sensitivity and specificity for SUVmax = 9.5 were 92.9% and 37.2%, respectively. (C) ROC curve in laryngeal cancer patients showing lack of significant correlation (AUC = 0.455 (95% CI = 0.241–0.699, P = 0.686).
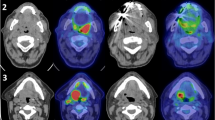
In hypopharyngeal cancer, univariable analysis showed that pretherapeutic SUVmax ≥ 9.5 and T3/4 classification were predictors for salvage pharyngolaryngectomy. In multivariable analysis, the only independent predictor of salvage laryngopharyngectomy was a pretherapeutic SUVmax of the primary tumor ≥ 9.5 (HR = 8.64, 95% CI = 1.1–67.3, P = 0.040). Comparative Kaplan-Meier survival analysis showed a worse laryngectomy-free survival in patients with pretherapeutic SUVmax ≥ 9.5 (Fig. 2A, Log rank test, P = 0.010).
The risk of salvage pharyngolaryngectomy according to pretherapeutic SUVmax of the primary tumor was also evaluated in ordinal fashion. For patients with pretherapeutic SUVmax < 9.5, risk of laryngectomy was low. The risk of laryngectomy increased with a higher pretherapeutic SUVmax in an almost linear manner, as depicted in Fig. 3.
In laryngeal cancer, the only predictor of laryngeal preservation was T-classification (HR = 6.67, CI = 0.82–53.9, P = 0.039) in univariable analysis. Gender, age, N-classification, smoking, alcohol abuse, and metabolic tumor parameters (pretherapeutic SUVmax, MTV, TLG) were not predictors of organ preservation (Table 3, each P > 0.05).
As expected, a low posttherapeutic SUVmax (<3.0) was also predictive of organ preservation in laryngeal and hypopharyngeal cancer (Log-rank test P = 0.001, not shown)
Secondary outcome analysis: survival
The cumulative distant metastasis-free survival at 60 months was 69%. A majority of patients (58.3%) presented with pulmonary metastases. The only factor significantly predictive of distant metastases was nodal stage at diagnosis (Fig. 4, log-rank test, P = 0.004). The cumulative disease-specific survival at 60 months was 61%, with most events occurring within the first three years of follow-up. The cumulative overall survival at 60 months was 49%.
Pretherapeutic SUVmax of the primary tumor was not predictive of regional recurrence-free survival, distant metastasis-free survival, disease-specific survival, and/or overall survival (not shown, log-rank test, each P > 0.05).
Posttherapeutic SUVmax of the primary tumor was predictive of distant metastasis-free survival, disease-specific survival (log-rank test, P = 0.046 and P = 0.021, respectively) but not of regional recurrence-free and overall survival (log-rank test, each P > 0.05).
Discussion
This study evaluates whether pretherapeutic metabolic parameters of laryngeal and hypopharyngeal cancer patients can predict tumor response to chemoradiation. Pretherapeutic SUVmax of the primary tumor was a predictor of laryngeal preservation before chemoradiation in hypopharyngeal cancer but did not seem to be predictive of organ preservation in laryngeal cancer.
The primary goal of our study was to identify pretherapeutically available markers to assist in clinical decision making, choosing between primary chemoradiation and primary surgery followed by adjuvant radiotherapy, as needed.
We also analyzed posttherapeutic metabolic parameters and showed, in accordance with previously published literature21,22, that a high posttherapeutic SUVmax is indicative of poor metabolic response to chemoradiation and predictive of the need for salvage laryngectomy and worse distant metastasis-free and disease-specific survival.
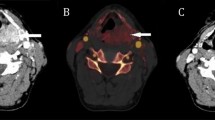
Tumor hypoxia is known to adversely affect tumor response to radiotherapy17, attributed to a decrease of radiation-induced DNA damage under reduced oxygen conditions23. Hypoxic microenvironment within tumors alters cellular metabolism and triggers a myriad of molecular responses including upregulation of hypoxia inducible factors (HIFs)24. HIFs in turn promote transcription activation with upregulation of SNAIL and TWIST signaling pathways, resulting in activation of epithelial to mesenchymal transition (EMT)25,26. Hypoxia and HIFs also induce expression of GLUT1 to provide the cell with sufficient energy through increased glucose uptake, including also FDG27. Our hypothesis was therefore that FDG-PET metabolic parameters, such as SUVmax, could be used as surrogate markers of tumor hypoxia and poor prognosis. This hypothesis could be confirmed in hypopharyngeal (as Fig. 5 shows in an exemplary way) but not in laryngeal cancer. For the latter, T-classification at diagnosis was predictive of laryngeal preservation. Although we do not know the reason for this discrepancy, one factor might be the unassessed confounding effect of cartilage infiltration, which is a known predictor of poor response to chemoradiation, that may, however, be insufficiently addressed by the TNM classification19. Of importance, T-classification should not be underscored in hypopharyngeal cancer patients, as T3/T4 tumors tended towards poorer laryngectomy-free survival. The two cancer entities also differ in their tendency towards nodal metastasis28. Hypopharyngeal carcinomas are generally considered to develop nodal metastases earlier and more frequently compared to laryngeal cancer29,30. Comparing advanced stage hypopharyngeal and laryngeal carcinomas, patients with hypopharyngeal cancer are hence more likely to present with advanced nodal disease while those with cancer of the larynx are more likely to have a larger primary tumor to be categorized as advanced stage (Fig. 6 shows an example of a stage III (cT3 cN0 cM0) laryngeal cancer). This may feature another confounding factor in the analysis of tumor response to radiotherapy, although we did adjust for it in our multivariable analysis.
To the best of our knowledge, our study is the first to show that pretherapeutic SUVmax could help clinicians in decision-making to adequately select hypopharyngeal cancer patients suitable for organ preservation therapy. Nevertheless, previous studies have already suggested the potential of FDG-PET parameters in the prediction of organ preservation. Park et al.14 retrospectively analyzed the prognostic value of hypopharyngeal and laryngeal cancer metabolism in FDG-PET imaging before treatment. They identified MTV as an independent prognostic factor for both locoregional control (HR = 3.141, 95% CI = 1.175–8.399, P = 0.018) and overall survival (HR = 3.758, 95% CI = 1.415–9.982, P = 0.008). However, they did not separate upfront surgery with adjuvant radio(chemo)therapy from primary chemoradiation with salvage surgery, when needed. In their analysis of DeLOS-II trial, a German multicenter randomized phase II trial investigating functional organ preservation in patients with laryngeal and hypopharyngeal cancer receiving induction chemotherapy with or without cetuximab followed by radiotherapy, Wichmann et al.5 proposed a score facilitating decision-making between laryngectomy and organ preservation strategy based on the tumor’s early response to induction chemotherapy. Their score, identifying patients benefitting from larynx preservation strategies and those unsuitable for it, included the number of positive nodes, residual tumor volume, and a ratio of residual SUVmax to SUVmean above 1.51 after induction chemotherapy5.
In our study, SUVmax was the one FDG-PET parameter with the best predictive value regarding organ preservation. Although other studies have recently emphasized on volumetric FDG-PET parameters such as MTV or TLG13,31, SUVmax has the advantage to be a standardized and easily applicable measure with the highest availability32. In clinical practice, it is better reproducible and less subject to variation due to different definitions of the region of interest or due to spill-over of adjacent FDG-avid structures33.
Based on our statistical analysis, we propose an SUVmax cutoff of 9.5 to distinguish between hypopharyngeal tumors with high and low risk of salvage pharyngolaryngectomy. In a previous study on oral cancer, our group already reported an SUVmax cutoff of 9.534. Other studies assessing the association between SUVmax and survival reported cutoff values between 8.0 and 9.0 to identify head and neck carcinomas at risk of shorter disease-free and overall survival35,36,37.
Although organ preservation is of great importance for patients from a psychological, social, and functional point of view, our study shows that hypopharyngeal carcinomas with high SUVmax are at greater risk of treatment failure and should be considered for upfront surgery followed by adjuvant radio(chemo)therapy. With the intensification of nonoperative treatment approaches, an increasing number of patients are experiencing long-term swallowing impairments and functional deficiencies38. These late toxic effects are more common following primary chemoradiation in comparison to upfront surgery with postoperative radiotherapy38,39. Tschiesner et al.40 analyzed the functional outcome in patients with advanced head and neck cancer comparing upfront surgery with primary chemoradiation in a cross-sectional, multi-institutional study. They reported no significant difference between the two groups regarding most aspects of functional outcome. However, body functions, including swallowing and weight maintenance, as well as activities and participations, including social relationships, employment, and economic self-sufficiency, were observed to be more problematic in patients receiving initial chemoradiation. Moreover, Jang et al.41 compared oncological and functional outcomes between initial surgical versus non-surgical treatments for hypopharyngeal cancer in 332 patients. Their data revealed similar oncological outcome and showed even better verbal communication outcomes in advanced-stage hypopharyngeal cancer patients receiving initial chemoradiation. Nevertheless, more patients treated with primary chemoradiation required multiple surgical interventions in the process. This may be explained through a reported failure rate of organ preservation of approximately 46% and also because a significant proportion of survivors with a preserved organ required tracheostomy due to a dysfunctional larynx41,42.
Our study goal was to assess tumor response to chemoradiation according to SUVmax of the primary tumor but not to assess how the larynx reacted to chemoradiation. Our study might therefore overestimate actuarial organ preservation, as patients who formally achieved organ preservation were assessed as such, regardless of the function of their larynx after chemoradiation. Another limitation of our study is its retrospective design. Furthermore, PET scans were acquired on different scanners, albeit the SUVmax is a standardized measure. In addition, the number of patients was relatively low in our study. Differences among groups were, however, sizeable enough to be detected and to avoid beta error43. Lastly, owing to the small size of the study population, a sub-analysis depending on HPV status was not performed. In contrast to oropharyngeal cancer, the percentage of HPV-positive tumors of the hypopharynx or larynx is considerably lower and therefore less confounding. Moreover, there is no evidence that HPV-positive hypopharyngeal or laryngeal cancers have a comparable better prognosis as it is the case for oropharyngeal tumors.
In conclusion, SUVmax of primary tumor could be used as a predictor of laryngeal preservation before chemoradiation in hypopharyngeal cancer. This information may be of great impact in patient counseling, as SUVmax was inversely correlated with the chance of larynx preservation. SUVmax, however, does not seem to be predictive of outcome in laryngeal cancer.
References
Forastiere, A. A. et al. Long-term results of RTOG 91-11. A comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 31, 845–852, https://doi.org/10.1200/JCO.2012.43.6097 (2013).
Wolf, G. T. et al. Induction Chemotherapy plus Radiation Compared with Surgery plus Radiation in Patients with Advanced Laryngeal Cancer. New England Journal of Medicine 324, 1685–1690 (1991).
Grover, S. et al. Total Laryngectomy Versus Larynx Preservation for T4a Larynx Cancer. Patterns of Care and Survival Outcomes. International journal of radiation oncology, biology, physics 92, 594–601, https://doi.org/10.1016/j.ijrobp.2015.03.004 (2015).
Forastiere, A. A. et al. Concurrent Chemotherapy and Radiotherapy for Organ Preservation in Advanced Laryngeal Cancer.
Wichmann, G. et al. Induction chemotherapy followed by radiotherapy for larynx preservation in advanced laryngeal and hypopharyngeal cancer. Outcome prediction after one cycle induction chemotherapy by a score based on clinical evaluation, computed tomography-based volumetry and 18F-FDG-PET/CT. European journal of cancer (Oxford, England: 1990) 72, 144–155, https://doi.org/10.1016/j.ejca.2016.11.013 (2017).
Goerres, G. W., Schmid, D. T., Grätz, K. W., Schulthess, G. K. & Eyrich, G. K. Impact of whole body positron emission tomography on initial staging and therapy in patients with squamous cell carcinoma of the oral cavity. Oral Oncology 39, 547–551, https://doi.org/10.1016/S1368-8375(03)00016-2 (2003).
Rodrigues, R. S. et al. Comparison of whole-body PET/CT, dedicated high-resolution head and neck PET/CT, and contrast-enhanced CT in preoperative staging of clinically M0 squamous cell carcinoma of the head and neck. Journal of nuclear medicine: official publication, Society of Nuclear Medicine 50, 1205–1213, https://doi.org/10.2967/jnumed.109.062075 (2009).
Kyzas, P. A., Evangelou, E., Denaxa-Kyza, D. & Ioannidis, J. P. A. 18F-fluorodeoxyglucose positron emission tomography to evaluate cervical node metastases in patients with head and neck squamous cell carcinoma. A meta-analysis. Journal of the National Cancer Institute 100, 712–720, https://doi.org/10.1093/jnci/djn125 (2008).
Kim, S. Y. et al. Combined 18F-fluorodeoxyglucose-positron emission tomography and computed tomography as a primary screening method for detecting second primary cancers and distant metastases in patients with head and neck cancer. Annals of oncology: official journal of the European Society for. Medical Oncology 18, 1698–1703, https://doi.org/10.1093/annonc/mdm270 (2007).
Lonneux, M. et al. Positron emission tomography with 18Ffluorodeoxyglucose improves staging and patient management in patients with head and neck squamous cell carcinoma. A multicenter prospective study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 28, 1190–1195, https://doi.org/10.1200/JCO.2009.24.6298 (2010).
Halfpenny, W. et al. FDG-PET. A possible prognostic factor in head and neck cancer. British journal of cancer 86, 512–516, https://doi.org/10.1038/sj.bjc.6600114 (2002).
Schrepfer, T. et al. The value of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography for staging of primary extranodal head and neck lymphomas. The Laryngoscope 120, 937–944, https://doi.org/10.1002/lary.20843 (2010).
Pak, K. et al. Prognostic value of metabolic tumor volume and total lesion glycolysis in head and neck cancer. A systematic review and meta-analysis. Journal of nuclear medicine: official publication, Society of Nuclear Medicine 55, 884–890, https://doi.org/10.2967/jnumed.113.133801 (2014).
Park, G. C. et al. Prognostic value of metabolic tumor volume measured by 18F-FDG PET/CT in advanced-stage squamous cell carcinoma of the larynx and hypopharynx. Annals of oncology: official journal of the European Society for Medical Oncology 24, 208–214, https://doi.org/10.1093/annonc/mds247 (2013).
Bredell, M. G. et al. Current relevance of hypoxia in head and neck cancer. Oncotarget 7, 50781–50804 (2016).
Wilson, W. R. & Hay, M. P. Targeting hypoxia in cancer therapy. Nature reviews. Cancer 11, 393–410, https://doi.org/10.1038/nrc3064 (2011).
Brizel, D. M., Sibley, G. S., Prosnitz, L. R., Scher, R. L. & Dewhirst, M. W. Tumor hypoxia adversely affects the prognosis of carcinoma of the head and neck. International Journal of Radiation Oncology*Biology*Physics 38, 285–289, https://doi.org/10.1016/S0360-3016(97)00101-6 (1997).
Nordsmark, M., Overgaard, M. & Overgaard, J. Pretreatment oxygenation predicts radiation response in advanced squamous cell carcinoma of the head and neck. Radiotherapy and Oncology 41, 31–39, https://doi.org/10.1016/S0167-8140(96)01811-7 (1996).
Sobin, L. H., Gospodarowicz, M. K. & Wittekind C. TNM Classification of Malignant Tumours, 7th Edition (Wiley-Blackwell, 2011).
Riesterer, O. A Phase II Study In Patients With Advanced Head And Neck Cancer Of Standard Chemoradiation And Add-On Cetuximab. Available at, https://clinicaltrials.gov/ct2/show/NCT01435252 (2017).
Gupta, T. et al. Diagnostic performance of post-treatment FDG PET or FDG PET/CT imaging in head and neck cancer. A systematic review and meta-analysis. European journal of nuclear medicine and molecular imaging 38, 2083–2095, https://doi.org/10.1007/s00259-011-1893-y (2011).
Cheung, P. K. F., Chin, R. Y. & Eslick, G. D. Detecting Residual/Recurrent Head Neck Squamous Cell Carcinomas Using PET or PET/CT. Systematic Review and Meta-analysis. Otolaryngology–head and neck surgery: official journal of American Academy of Otolaryngology-Head and Neck Surgery 154, 421–432, https://doi.org/10.1177/0194599815621742 (2016).
Kelada, O. J. & Carlson, D. J. Molecular imaging of tumor hypoxia with positron emission tomography. Radiation research 181, 335–349, https://doi.org/10.1667/RR13590.1 (2014).
Joseph, J. P., Harishankar, M. K., Pillai, A. A. & Devi, A. Hypoxia induced EMT. A review on the mechanism of tumor progression and metastasis in OSCC. Oral Oncol 80, 23–32, https://doi.org/10.1016/j.oraloncology.2018.03.004 (2018).
da Silva, S. D. et al. Epithelial-mesenchymal transition (EMT) markers have prognostic impact in multiple primary oral squamous cell carcinoma. Clinical & experimental metastasis 32, 55–63, https://doi.org/10.1007/s10585-014-9690-1 (2015).
Morand, G. B. et al. Preoperative assessment of CD44-mediated depth of invasion as predictor of occult metastases in early oral squamous cell carcinoma. Head & neck 41, 950–958, https://doi.org/10.1002/hed.25532 (2019).
Rupp, N. J. et al. Oxygen supply maps for hypoxic microenvironment visualization in prostate cancer. J Pathol Inform 7, 3, https://doi.org/10.4103/2153-3539.175376 (2015).
Madana, J. et al. Clinical parameters predicting development of pulmonary malignancies in patients treated for head and neck squamous cell carcinoma. Head & neck 38 Suppl 1, E1277–80; https://doi.org/10.1002/hed.24210 (2016).
Magnano, M. et al. Lymphnode metastasis in head and neck squamous cells carcinoma. Multivariate analysis of prognostic variables. Journal of experimental & clinical cancer research: CR 18, 79–83 (1999).
Wycliffe, N. D., Grover, R. S., Kim, P. D. & Simental, A. Hypopharyngeal cancer. Topics in magnetic resonance imaging: TMRI 18, 243–258, https://doi.org/10.1097/RMR.0b013e3181570c3f (2007).
Schwartz, D. L. et al. Metabolic tumor volume as a prognostic imaging-based biomarker for head-and-neck cancer. Pilot results from Radiation Therapy Oncology Group protocol 0522. International journal of radiation oncology, biology, physics 91, 721–729, https://doi.org/10.1016/j.ijrobp.2014.12.023 (2015).
Castelli, J. et al. Overview of the predictive value of quantitative 18 FDG PET in head and neck cancer treated with chemoradiotherapy. Critical reviews in oncology/hematology 108, 40–51, https://doi.org/10.1016/j.critrevonc.2016.10.009 (2016).
Boellaard, R., Krak, N. C., Hoekstra, O. S. & Lammertsma, A. A. Effects of Noise, Image Resolution, and ROI Definition on the Accuracy of Standard Uptake Values: A Simulation Study. Journal of nuclear medicine: official publication, Society of Nuclear Medicine 45, 1519–1527 (2004).
Morand, G. B. et al. Maximum Standardized Uptake Value (SUVmax) of Primary Tumor Predicts Occult Neck Metastasis in Oral Cancer. Scientific reports 8, 11817, https://doi.org/10.1038/s41598-018-30111-7 (2018).
Roh, J.-L. et al. 2-18F-Fluoro-2-deoxy-D-glucose positron emission tomography as guidance for primary treatment in patients with advanced-stage resectable squamous cell carcinoma of the larynx and hypopharynx. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 33, 790–795, https://doi.org/10.1016/j.ejso.2007.01.002 (2007).
Kubicek, G. J. et al. FDG-PET staging and importance of lymph node SUV in head and neck cancer. Head & neck oncology 2, 19, https://doi.org/10.1186/1758-3284-2-19 (2010).
Ishihara, T. et al. 18FFluorodeoxyglucose uptake by positron emission tomography predicts outcomes for oropharyngeal and hypopharyngeal cancer treated with definitive radiotherapy. Nagoya journal of medical science 79, 27–36, https://doi.org/10.18999/nagjms.79.1.27 (2017).
Bentzen, S. M., Rosenthal, D. I., Weymuller, E. A. & Trotti, A. Increasing toxicity in nonoperative head and neck cancer treatment. Investigations and interventions. Int J Radiat Oncol Biol Phys 69, S79–82, https://doi.org/10.1016/j.ijrobp.2007.04.080 (2007).
Morand, G. B. et al. Survival and quality of life in oropharyngeal cancer patients treated with primary chemoradiation after salivary gland transfer. The Journal of laryngology and otology 130, 755–762, https://doi.org/10.1017/S0022215116008100 (2016).
Tschiesner, U., Schuster, L., Strieth, S. & Harréus, U. Functional outcome in patients with advanced head and neck cancer. Surgery and reconstruction with free flaps versus primary radiochemotherapy. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery 269, 629–638, https://doi.org/10.1007/s00405-011-1642-7 (2012).
Jang, J. Y. et al. Comparison of Oncological and Functional Outcomes between Initial Surgical versus Non-Surgical Treatments for Hypopharyngeal Cancer. Annals of surgical oncology 23, 2054–2061, https://doi.org/10.1245/s10434-016-5088-4 (2016).
Lefebvre, J. L. et al. Larynx preservation in pyriform sinus cancer. Preliminary results of a European Organization for Research and Treatment of Cancer phase III trial. EORTC Head and Neck Cancer Cooperative Group. Journal of the National Cancer Institute 88, 890–899 (1996).
Swinscow, T. D. V. & Campbell, M. J. Statistics at square one. 10th ed. (BMJ, London, 2002).
Acknowledgements
J.W. would like to thank his family and his loved ones for their support.
Author information
Authors and Affiliations
Contributions
Basic study idea by G.B.M., G.F.H. and M.W.H. Patients search by J.W. J.W. und M.W.H. extracted the data related to nuclear imaging. J.W. extracted the patients related data, built the figures and wrote the first draft of the manuscript under G.B.M.’s supervision. G.B.M. performed statistical analysis. Manuscript editing and review by M.W.H., N.J.R., A.M.H., M.A.B., and G.F.H. J.W., M.W.H., N.J.R., A.M.H., M.A.B., G.F.H. and G.B.M. have participated substantially to the study and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Werner, J., Hüllner, M.W., Rupp, N.J. et al. Predictive Value of Pretherapeutic Maximum Standardized Uptake Value (Suvmax) In Laryngeal and Hypopharyngeal Cancer. Sci Rep 9, 8972 (2019). https://doi.org/10.1038/s41598-019-45462-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-45462-y
This article is cited by
-
Evaluation of OTL38-Generated Tumor-to-Background Ratio in Intraoperative Molecular Imaging-Guided Lung Cancer Resections
Molecular Imaging and Biology (2023)
-
Prediction of extranodal extension in oropharyngeal cancer patients and carcinoma of unknown primary: value of metabolic tumor imaging with hybrid PET compared with MRI and CT
European Archives of Oto-Rhino-Laryngology (2023)
-
18F-FDG-PET/CT can be used to predict distant metastasis in hypopharyngeal squamous cell carcinoma
Journal of Otolaryngology - Head & Neck Surgery (2022)
-
FDG-PET predicts bone invasion and prognosis in patients with oral squamous cell carcinoma
Scientific Reports (2021)
-
Predictive value of suvmax changes between two sequential post-therapeutic FDG-pet in head and neck squamous cell carcinomas
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.