Abstract
Genetic polymorphism of drug metabolizing enzymes and transporters may influence drug response. The frequency varies substantially between ethnicities thus having implications on appropriate selection and dosage of various drugs in different populations. The distribution of genetic polymorphisms in healthy Pakistanis has so far not been described. In this study, 155 healthy adults (98 females) were included from all districts of Karachi. DNA was extracted from saliva and genotyped for relevant SNVs in CYP1A1, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A4 and CYP3A5 as well as ALDH3A1, GSTA1, ABCB1 and ABCC2. About 64% of the participants were born to parents who were unrelated to each other. There was generally a higher prevalence (p < 0.05) of variant alleles of CYP450 1A2, 2B6, 2C19, 3A5, ALDH3A1, GSTM1 as well as ABCB1 and ABCC2 in this study cohort than in other ethnicities reported in the HapMap database. In contrast, the prevalence of variant alleles was lower in GSTA1. Therefore, in the Pakistani population sample from Karachi a significantly different prevalence of variant drug metabolizing enzymes and ABC transporters was observed as compared to other ethnicities, which could have putative clinical consequences on drug efficacy and safety.
Similar content being viewed by others
Introduction
The concept of choosing the right medicine for right person is not new. However, pharmacogenomic research has enabled us to predict an adverse outcome of administering a medication that would formerly have been judged to be generally safe and effective1. Due the initiative of the Clinical Pharmacogenetics Implementation Network and others2, many drugs in the USA are now dispensed with FDA advised pharmacogenetic warning labels. A detailed list of pharmacogenetic markers is available online at the FDA website (www.fda.gov/Drugs/ScienceResearch/ucm572698.htm). Drug regulatory agencies like the European EMA are following the lead. However, such data stems mainly from the West, which may not be applicable to other parts of the world.
Genetic variability of drug metabolizing enzymes and drug transporters has been associated with interindividual differences in pharmacokinetics and pharmacodynamics. Such differences may result in variation in drug efficacy, safety and treatment outcomes in a number of frequently prescribed drugs3. A notable example is that of pharmacogenetic peculiarities of Ashkenazi Jewish population who are reported to have important therapeutic implications, such as VKORC1 gene polymorphism necessitating warfarin dose adjustment4. Hence, interindividual genetic differences within but also between various ethnic groups are considered to be an important contributory factor to the variability of drug responses5. In this study, we characterized single nucleotide variants (SNVs) of select phase I enzymes (CYPs and ALDHs), phase II enzymes (GSTs, UGTs, TPMPTs and NATs) and transporters involved in drug metabolism in a population of 155 Karachiites in Pakistan, because no such studies are reported for this population. Further, we compared the variant allele frequency with allele frequencies reported for major ethnic groups in HapMap database and reported the differences between our population and each of those representative groups in HapMap.
It is estimated that 75–80% of prescribed drugs are metabolized by oxidizing phase I cytochrome P450 enzymes such as CYP3A4 and 5, CYP2D6, CYP2C19 or CYP2C9, with CYP3A4/5 metabolizing more than half of currently prescribed drugs6. In addition, phase II enzymes catalyze the conjugation of xenobiotic metabolites with various hydrophilic molecules to render them less toxic and more polar, thus favouring their excretion from the body. Such reactions are catalyzed by different enzyme groups, such as GSTs (glutathione S-transferases), UGTs (UDP-glucuronosyl transferases), TPMTs (thiopurine S-methyl transferases), NATs (N-acetyl transferases)7. GSTs also support detoxification reactions8 and play an important role in preventing oxidative stress9.
Additionally, ALDHs (aldehyde dehydrogenases) are phase I xenobiotic metabolizing enzymes which have diverse functions, such as neutralization of toxic aldehydes during lipid peroxidation10, coenzyme Q synthesis11, prevention of tobacco smoke-induced respiratory epithelial cytotoxicity12, metabolism of cyclophosphamide8 and ethanol13 among other functions. Thus, altered ALDH function could predispose individuals to numerous medical conditions such as atherosclerosis, dementia, infertility, cancers. This becomes further complicated if the biological role shows a gene-dose effect, as we previously reported for ALDH3A18.
ATP binding cassette (ABC) transporters are a group of membrane transporters, which transport many xenobiotics, including drugs, in and out of various cells. In fact, some of them were called multi-drug resistance proteins because of this role. Of notable interest are ABCB1 and ABCC2 transporters. Their substrates include many drugs, including anticancer drugs, HIV protease inhibitors, antibiotics, beta blockers, statins, anticonvulsants, opiates14.
As outlined above, ethnic differences exist in the prevalence of genetic variants of the enzymes and transporters15. Hence, genetic characterization of patients may prove valuable in predicting therapeutic outcomes16,17,18. We reported previously19 that significant differences exist in the frequencies of polymorphic genes involved in metabolism and cellular transport of breast cancer chemotherapy among breast cancer patients from Karachi, as compared to some ethnic groups reported in HapMap database (https://www.ncbi.nlm.nih.gov/snp). However, that study was limited because of the small sample size used and the absence of data from a healthy population.
To the best of our knowledge, there is no comprehensive study on this topic involving South Asia and adjoining regions. Hence, we designed this study to explore the genotype profiles among healthy adults from different ethnicities living in Karachi, allowing us to compare them with those reported for other major ethnic groups in the HapMap database.
Results
Table 1 shows the baseline characteristics of the study population. A total of 155 healthy Pakistani adults (98 females and 57 males) with a median age of 19 years (range: 18–70 years) were included in this study. Participants were from all districts of Karachi and belonged to various major ethnic groups within Pakistan. Ethnicity was classified according to their mother tongue, including Balochi, Gujrati, Pashtun, Punjabi, Seraiki, Sindhi, and other minor groups. As expected, the local Urdu-speaking community with heterogeneous Indian ancestry, collectively described as Muhajir (Arabic/Urdu; immigrants) featured most in our population. Since consanguineous marriages are common in Pakistan20, we sought information regarding this fact. Most individuals declared that their parents were not related to each other. Some of the participants, labelled as ‘mixed lineage’ had grandparents from different ethnicities.
Table 2 shows the frequency distribution of SNVs and genotypes. Genotypes were in Hardy-Weinberg equilibrium. Some of the samples could not be genotyped completely, apparently due to low DNA quantity or quality. Haplotype and diplotype analyses were carried out where applicable. Table 2 shows that in our population the percent frequency of wild type genotype was as follows:
-
(a)
Phase I enzymes: CYP1A1 42% (heterozygous 46%; homozygous variant 12%), CYP2B6 20% (heterozygous 54%; homozygous variant 26%), CYP2C9 71% (heterozygous 26%), CYP2C19 27% (heterozygous 48%; homozygous variant 25%), CYP2D6 extensive metabolizers 74% (25% intermediate metabolizers, 1% poor metabolizers), CYP3A4 98% (heterozygous 2%), CYP3A5 1% (heterozygous 38%, homozygous variant 61%), ALDH3A1 8% (heterozygous 50%, homozygous variant 42%).
-
(b)
Phase II enzymes: GSTA1 49% (heterozygous 41%, homozygous variant 10%), GSTM1 null 59%.
-
(c)
ABC Transporters: ABCB1 wildtype haplotype 10%, ABCC2 wildtype haplotype 50%
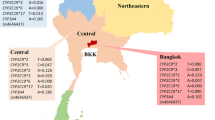
Table 3 and Fig. 1 show variant allele frequencies. This study compared Pakistani population with major global ethnic groups (African of Yoruba Nigerian ancestry, Caucasian of Northern and Western European ancestry, Chinese of Han ancestry) as well as a subset from the neighbouring area of India (Gujrati Indians in Houston, Texas), all taken from the HapMap database. Variant allele frequencies were compared using Chi-square or Fischer exact tests. The results show that as compared to ethnicities in the HapMap database there were significant differences in prevalence of variant alleles of (a) ALDH3A1, (b) CYP1A1*2A, CYP2B6*4, CYP2B6*6, CYP2C19*2, CYP3A5*3, (c) GSTA1, and (d) ABCB1 2677G > T/A and ABCC2 1249G > A in our population. GSTM1 null genotype was found higher than in other reported ethnicities. CYP2D6*3 was absent in our study sample. All other SNVs showed intermediate or similar prevalence of variant alleles as compared to other ethnicities.
Variant allele frequencies (percent) of drug metabolizing enzymes and ABC transporters in healthy Pakistanis as compared to the HapMap Database (http://www.ncbi.nlm.nih.gov/SNP/). KHI, Karachi Pakistan (current study); CHIN, Chinese of Han ancestry; CAUC, Caucasians of Northern and Western European ancestry; AFR, African of Yoruba Nigerian ancestry; GUJ, Gujrati Indian ancestry living in Houston, Texas, USA. Green highlighted row shows current study sample and yellow shaded areas show significant difference from KHI samples computed through chi-square or Fisher exact test. The missing values indicate absence of data in HapMap database for that particular SNV.
Discussion
This study is the first comprehensive pharmacogenetic report from Pakistan. Previously we had shown that SNV prevalence of a select group of Phase-I as well as Phase-II drug metabolizing enzymes and ABC transporters in a breast cancer population sample had significant differences as compared to various ethnicities in HapMap database19. In this study also we identified several important differences between allele and genotype frequencies compared to other populations. Interestingly, the differences were similar to those reported previously for breast cancer population19, suggesting that real differences might exist. It is important to understand the implications of such differences in this population as compared to others as a first step to precision medicine globally. For example, an altered gene function can lead to unfavourable therapeutic outcome(s) in acute care or chronic management of various disorders. A few recent examples where gene variant necessitate adjusted dosing of a drug include that of clopidogrel in case of CYP2C19 SNVs21, warfarin in case of CYP2C9 or VKORC1 SNVs22 and tamoxifen in case of CYP2D6 SNVs23.
This study has many advantages. Pakistan is a populous multi-ethnic country with more than 200 million inhabitants. We included people from various major ethnic groups including Urdu-speaking, Balochi, Gujrati, Pashtun, Punjabi, Seraiki and Sindhi. The presence of a substantial proportion of Urdu-speaking population enabled us to extend the relevance of our results to neighbouring India which has a population over 1300 million. Overall their relevance could be extended to approximately 20–25% of the World’s population, which is historically underrepresented in pharmacogenomic studies. Hence, these results provide an important window to a largely unstudied population. Despite this, there are some limitations of our study. Approximately one third of our study population represented an inbred cohort due to consanguineous marriages, a widespread practice in this region. Further, our study cohort did not have substantial numbers of other Pakistani ethnic groups, like Baloch, Pashtun, Punjabi and Sindhi for sub-group analysis and robust conclusions regarding these ethnic groups. Hence, we recommend replicating the study to target these groups across the country and region.
The following section discusses in depth the implications of various significant observations in our study sample, comparing it with other ethnicities documented in the HapMap database, including African, Caucasian, Chinese and Gujrati. For further research and analysis, a web-based detailed account regarding substrates, inducers and inhibitors of various drug metabolizing enzymes, and updated clinical application of pharmacogenetics (CPIC guidelines) can be found at https://www.pharmgkb.org/, http://bioinformatics.charite.de/transformer/. and https://cpicpgx.org/guidelines/.
CYP1A1
Cytochrome P450 1A1 metabolizes xenobiotics such as polycyclic aromatic hydrocarbons (PAHs) found in tobacco smoke, atmospheric pollutants and industrial waste and generates carcinogens from several substrates24. Hence, CYP1A1 is considered a link between environment-gene interaction in the etiology of various cancers such as head and neck cancers among smokers25. Our sample shows a higher prevalence of variant alleles (58% of diplotypes carried at least one variant allele) as compared to Caucasians and could potentially confer an elevated disease risk although this would need further validation. The difference in prevalence of SNVs could also have an impact on therapeutic outcome of drugs that may be favourable such as in case of antineoplastic docetaxel26, or first-line antiepileptics27, but unfavourable for antiemetic granisetron28.
CYP2B6
Our results show a significantly higher prevalence of variant alleles CYP2B6*4 (48%) and CYP2B6*6 (36%) genotypes as compared to other ethnicities reported in HapMap database. Both alleles are associated with lower CYP2B6 activity leading to pharmacogenetic implications with many drugs including the antidepressant bupropion29, antiretroviral efavirenz30, anti-tuberculosis rifamycins and ethionamide31, among others. Pakistan has a high prevalence of tuberculosis, whereas HIV prevalence is on the rise especially in high-risk groups like sex workers and intravenous drug addicts32. Hence, compromised CYP2B6 function in the population could lead to elevated risk of side effects and drug-drug interactions. Further research is needed to evaluate the situation in this respect.
CYP2C9
This enzyme metabolizes many drugs, such as warfarin33, phenytoin34 and non-steroidal anti-inflammatory drugs diclofenac and ibuprofen35. Our results show an intermediate prevalence of CYP2C9*2 genotype in KHI (6.8%) as compared to Caucasian (10.4%) and African (0%) populations in HapMap database. However, the CYP2C9*3 genotype is more frequent (9.93%) than in those population groups. Haplotype analysis suggests that approximately 30% population has some degree of compromised function of CYP2C9. The potential effects of this observation should be explored, especially for warfarin and phenytoin due to their narrow therapeutic index.
CYP2C19
While CYP2C19*2 leads to complete loss-of-function, CYP2C19*17 is associated with gain-of-function. Several widely used drugs such as the antiplatelet clopidogrel36, antifungal voriconazole37, and the antidepressant citalopram38 are metabolized by CYP2C19. Because of problems in efficacy and pharmacokinetics, the USFDA and other such agencies include pharmacogenetic information in some drug labels to optimize the use of drugs, such as clopidogrel. Our data shows that only 27% of the Pakistani population had normal phenotype (CYP2C19*1/*1). Thus, further studies are required to elucidate the pharmacogenetics in this population, especially regarding drugs used in acute emergencies, such as clopidogrel in acute coronary syndrome.
CYP2D6
This highly polymorphic enzyme is involved in the metabolism of more than 20% of drugs. Notable examples include the antidepressant paroxetine38, SERM tamoxifen39, antipsychotic clozapine40, adrenoceptor antagonists metoprolol and carvedilol among others41. Our data shows that the minor allele frequency was approximately 30%, whereas, 26% population had genotypes associated with some degree of functional loss.
ALDH3A1
Aldehyde dehydrogenases are phase-1 metabolizing enzymes which exist as different isoenzymes. Our focus was ALDH3A1 which is involved in a broad spectrum of physiological activities, including the protection of oral and respiratory tract mucosa from damage caused by cigarette smoke12, food and air pollutants42, and ionizing radiation43. Additionally, it is involved in preventing ultraviolet light induced corneal damage44, detoxification of 4-HNE (4-hydroxynonenal; a by-product of lipid peroxidation)9, generation of NO from organic nitrates36, metabolism of oxazophorines like cyclophosphamide8, and synthesis of Coenzyme Q11. Thus, ALDH3A1 takes part in drug metabolism and reduction of oxidative stress. We had previously shown that the prevalence of ALDH3A1 (985C > G) variant allele shows significant differences among various ethnicities in HapMap database and was much more prevalent (62.5%) in Pakistani breast cancer patients with 40% homozygous for variant allele19. In this study, we have shown that it is similarly prevalent in the healthy population (67% variant allele; 42% homozygous variant genotype). So far however, there is lack of concrete evidence that non-functional ALDH3A1 is associated with increased disease risk.
GSTA1
Glutathione S-transferase A1 is the most abundant form of GSTs in human liver, kidney, adrenal gland and testis, where they appear to scavenge electrophiles and reduce oxidative stress45. It also appears to regulate other functions. For example, a recent in vitro study suggested that GSTA1 may facilitate nicotine-induced lung cancer metastasis46. Another study suggested its role in metabolism of anticancer drug busulfan47. We had previously reported that loss of GSTA1 is a major determinant of neutropenia among breast cancer patients receiving standard dose FAC (5-fluorouracil, doxorubicin, cyclophosphamide) chemotherapy8. Our current results also show that prevalence of variant allele is lower (30.5%) in the Pakistani population as compared to others in HapMap database (range: 58.4–89.5%) though in absolute terms it is still high.
GSTM1
Glutathione S-transferase M1 is another GST believed to eliminate oxidative intermediates in the alimentary tract as posed by dietary toxins. The role of GSTM1 null genotype as a susceptibility factor for various carcinoma is conflicting, although a large meta-analysis comprising 198 studies revealed an association of lung cancer to GSTM1 null genotype48. Other studies have suggested that GSTM1 null genotype is associated with pathogenesis of chronic obstructive pulmonary disease49, or increased likelihood of toxicity of cyclophosphamide50 and oxaliplatin51. Our results show a high prevalence of putative “at risk” null genotype (59%). A recent study from Pakistan observed elevated levels of carcinogenic 1-hydroxypyrene in GSTM1 null carriers52, making further molecular epidemiological studies necessary in the Pakistani population.
ABCB1
The ATP-binding cassette transporter B1, also called MDR1 (multi-drug resistance protein 1) or P-gp (permeability glycoprotein), is a membrane transporter located at many interfaces in the body53. It actively transports various xenobiotics and toxins across the cell membranes and has been implicated in antineoplastic drug resistance54. Certain drugs, such as amiodarone, clarithromycin, omeprazole, and calcium channel blockers, can inhibit this protein leading to drug-drug interactions55. Our results show a prevalence of 54–65% variant alleles of ABCB1 (1236C > T, 2677G > T/A, 3435C > T; rs1128503, rs2032582, rs1045642 respectively). These frequencies are not significantly different from most populations except African.
ABCC2
ATP-binding cassette transporter C2, also called MRP2 (multidrug resistance-associated protein 2) or CMOAT (Canalicular Multispecific Organic Anion Transporter), is an active efflux transporter identified at apical or biliary canalicular surfaces of hepatocytes and in the kidney. There is mounting evidence that by promoting efflux in target cells this protein is involved in the resistance to several drugs, such as antiepileptics56, antiretroviral drugs57, antineoplastic drugs58, and statins among others59. Conversely, its decreased function may lead to increased drug toxicity. Our data (Tables 2 and 3) suggests that a substantial proportion of the population has diplotypes with some degree of functional deficit where the prevalence of variant alleles ranges from 15–37%. Thus, the effects of this finding should be explored in terms of drug efficacy and toxicity.
In conclusion, this study showed that in our sample compared with other ethnic populations, there was a generally higher prevalence (p < 0.05) of variant alleles of ALDH3A1, CYP1A1*2A, CYP2B6*4, CYP2B6*6, CYP2C19*2, CYP3A5*3, ABCB1 2677G > T/A and ABCC2 1249G > A. Further, GSTM1 null genotype also had higher frequency. There is a lower prevalence of variant alleles of GSTA1, and ABCC2 3972C > T as compared to other ethnicities. As mentioned above, these results are not significantly different from our previously reported Pakistani female breast cancer patients19, thus suggesting real differences between our sample and other ethnicities in HapMap database, namely African, Caucasian, and Chinese. Hence, further research in other population cohorts within the country and the region would be beneficial for a more complete understanding of the pharmacogenetic landscape in a region which is underrepresented in genetic studies. This is an important step forward in achieving widespread and cost-effective implementation of personalized medicine in the community60.
Methods
The study was conducted at Jinnah Medical and Dental College (JMDC), Karachi, Pakistan from July 2013 to December 2015 after approval by The Ethics Committee of Jinnah Medical & Dental College, in accordance with relevant guidelines. The study cohort included students and employees of JMDC who were invited to be volunteers and gave written informed consent.
Saliva was the source of genomic DNA. The saliva samples were collected and stored in Oragene® DNA collection kits (DNA Genotek Inc. Canada) according to manufacturer’s recommendations. DNA was extracted through the proprietary extraction kit provided with collection kits. The extracted DNA was air-shipped to the Institute of Experimental and Clinical Pharmacology, Christian-Albrechts University, Kiel, Germany for genotyping.
For primers and experimental method details, see Supplementary Tables 1 and 2. Briefly, genotyping was performed by restriction fragment length polymorphism (RFLP) for CYP1A1 SNVs rs1048943 (g.3798C > T, *2A and *2B), rs1799814 (g.2454A > G, *2B) and rs4646903 (g.2452C > A, *4); for CYP2B6 SNVs rs2279343 (c785A > G, *4), rs3211371 (c.1459C > T, *5) and rs3745274 (c.516G > T, *6); for CYP2C9 SNVs rs1799853 (430C > T, *2) and rs1057910 (1075A > C, *3); for CYP2C19*2 SNV rs4244285 (681G > A); for CYP2D6 SNVs rs5030655 (g.1707delT, *6), rs3892097 (g.1846C> T, *4), rs35742686 (g.2549delA, *3), rs5030656 (g.2615-g.2617delAAG, *9 and rs1065852 (g.100C > T), *10); and for CYP3A5 SNV rs776746 (g.6986G > A, *3). The CYP2D6 deletion (*5) and gene duplication could not be determined in the DNA retrieved from saliva specimen. All homozygous variant genotypes detected through RFLP were repeated to ensure accuracy.
A PSQ HS 96 (Qiagen, Hilden, Germany) was used for pyrosequencing (PSQ) SNVs for GSTA1 −69C > T and −52G > A (rs3957357 and rs3957356 respectively; representing GSTA1*A and GSTA1*B haplotype); for ALDH3A1 (985C > G; rs2228100), and for CYP3A4 (15389C > T; rs35599367. Novel PSQ methods were established for CYP2C19*17, ABCB1 SNVs (rs1128503, g.1236C > T; rs2032582 g.2677G > T/A; rs1045642 g.3435C > T), and for ABCC2 (rs717620 −g.24C > T, rs2273697 g.1249G > A, rs3740066 g.3972C > T). For all the PCR reactions, a GeneAmp PCR 9700 Thermocycler (Applied Biosystems, Darmstadt, Germany) was used.
The data was analysed using SPSS® version 19.0 software (IBM, Ehningen, Germany). The results were entered as frequencies, and percentage and 95% confidence interval (proportions) was calculated. All genotype frequencies were tested and found to be within Hardy-Weinberg equilibrium. Allele frequency data was compared through χ2 or Fisher’s Exact test where applicable. A p-value < 0.05 was considered significant.
Data Availability
The authors undertake that materials, data and associated protocols would be made available to readers.
References
Böhm, R. & Cascorbi, I. Pharmacogenetics and Predictive Testing of Drug Hypersensitivity Reactions. Front. Pharmacol. 7, 396. eCollection, https://doi.org/10.3389/fphar.2016.00396 (2016).
Luzum, J. A. et al. The Pharmacogenomics Research Network Translational Pharmacogenetics Program: Outcomes and Metrics of Pharmacogenetic Implementations Across Diverse Healthcare Systems. Clin. Pharmacol. Ther. 102, 502–510 (2017).
Relling, M. V. & Evans, W. E. Pharmacogenomics in the clinic. Nature. 526, 343–350 (2015).
Yang, Y., Peter, I. & Scott, S. A. Pharmacogenetics in Jewish populations. Drug Metabol. Drug Interact. 29, 221–233 (2014).
McGraw, J. & Waller, D. Cytochrome P450 variations in different ethnic populations. Expert Opin. Drug Metab. Toxicol. 8, 371–382 (2012).
Preissner, S. C. et al. Polymorphic cytochrome P450 enzymes (CYPs) and their role in personalized therapy. PLoS One. 8, e82562, https://doi.org/10.1371/journal.pone.0082562 (2013).
Jancova, P., Anzenbacher, P. & Anzenbacherova, E. Phase II drug metabolizing enzymes. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 154, 103–116 (2010).
Afsar, N. A. et al. Relationship of drug metabolizing enzyme genotype to plasma levels as well as myelotoxicity of cyclophosphamide in breast cancer patients. Eur. J. Clin. Pharmacol. 68, 389–395 (2012).
Suvakov, S. et al. Glutathione S-transferase A1, M1, P1 and T1 null or low-activity genotypes are associated with enhanced oxidative damage among haemodialysis patients. Nephrol. Dial. Transplant. 28, 202–212 (2013).
Black, W. et al. Molecular mechanisms of ALDH3A1-mediated cellular protection against 4-hydroxy-2-nonenal. Free Radic. Biol. Med. 52, 1937–1944 (2012).
Stefely, J. A. et al. Mitochondrial protein functions elucidated by multi-omic mass spectrometry profiling. Nat. Biotechnol. 34, 1191–1197 (2016).
Jang, J. H. et al. Aldehyde dehydrogenase 3A1 protects airway epithelial cells from cigarette smoke-induced DNA damage and cytotoxicity. Free Radic. Biol. Med. 68, 80–86 (2014).
Matsumoto, A., Thompson, D. C., Chen, Y., Kitagawa, K. & Vasiliou, V. Roles of defective ALDH2 polymorphism on liver protection and cancer development. Environ. Health Prev. Med. 21, 395–402 (2016).
Cascorbi, I. Role of pharmacogenetics of ATP-binding cassette transporters in the pharmacokinetics of drugs. Pharmacol. Ther. 112, 457–473 (2006).
Shah, R. R. & Gaedigk, A. Precision medicine: does ethnicity information complement genotype-based prescribing decisions? Ther. Adv. Drug Saf. 9, 45–62 (2018).
Garte, S. et al. Metabolic gene polymorphism frequencies in control populations. Cancer Epidemiol. Biomarkers Prev. 10, 1239–1248 (2001).
Ingelman-Sundberg, M. Pharmacogenetics: an opportunity for a safer and more efficient pharmacotherapy. J. Intern. Med. 250, 186–200 (2001).
Schaeffeler, E. et al. Frequency of C3435T polymorphism of MDR1 gene in African people. Lancet. 358, 383–384 (2001).
Afsar, N. A. et al. Genotype Frequencies of selected Drug Metabolizing Enzymes and ABC Drug Transporters among Breast Cancer Patients on FAC Chemotherapy. Basic Clin. Pharmacol. Toxicol. 107, 570–576 (2010).
Hussain, R. & Bittles, A. H. The prevalence and demographic characteristics of consanguineous marriages in Pakistan. J. Biosoc. Sci. 30, 261–275 (1998).
Scott, S. A. et al. Clinical Pharmacogenetics Implementation Consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin. Pharmacol. Ther. 94, 317–323 (2013).
Johnson, J. A. et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for Pharmacogenetics-Guided Warfarin Dosing: 2017 Update. Clin. Pharmacol. Ther. 102, 397–404 (2017).
Goetz, M. P. et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and Tamoxifen Therapy. Clin. Pharmacol. Ther. 103, 770–777 (2018).
Rendic, S. & Guengerich, F. P. Contributions of Human Enzymes in Carcinogen Metabolism. Chem. Res. Toxicol. 25, 1316–1383 (2012).
Liu, L. et al. Functional CYP1A1 genetic variants, alone and in combination with smoking, contribute to development of head and neck cancers. Eur. J. Cancer. 49, 2143–2151 (2013).
Dong, N. et al. Pharmacogenetic assessment of clinical outcome in patients with metastatic breast cancer treated with docetaxel plus capecitabine. J. Cancer Res. Clin. Oncol. 138, 1197–1203 (2012).
Grover, S. et al. Genetic polymorphisms in sex hormone metabolizing genes and drug response in women with epilepsy. Pharmacogenomics. 11, 1525–1534 (2010).
Bustos, M. L., Zhao, Y., Chen, H., Caritis, S. N. & Venkataramanan, R. Polymorphisms in CYP1A1 and CYP3A5 Genes Contribute to the Variability in Granisetron Clearance and Exposure in Pregnant Women with Nausea and Vomiting. Pharmacotherapy. 36, 1238–1244 (2016).
Benowitz, N. L., Zhu, A. Z., Tyndale, R. F., Dempsey, D. & Jacob, P. 3rd. Influence of CYP2B6 genetic variants on plasma and urine concentrations of bupropion and metabolites at steady state. Pharmacogenet. Genomics. 23, 135–141 (2013).
Soeria-Atmadja, S. et al. Genetic variants in CYP2B6 and CYP2A6 explain interindividual variation in efavirenz plasma concentrations of HIV-infected children with diverse ethnic origin. PLoS One. 12, e0181316, https://doi.org/10.1371/journal.pone.0181316 (2017).
Shimokawa, Y. et al. Inhibitory Potential of Twenty Five Anti-tuberculosis Drugs on CYP Activities in Human Liver Microsomes. Biol. Pharm. Bull. 38, 1425–1429 (2015).
Mishra, S. et al. Sexual behaviour, structural vulnerabilities and HIV prevalence among female sex workers in Pakistan. Sex Transm. Infect. 89, Sii34–42 (2013).
Liu, R., Li, X., Zhang, W. & Zhou, H. H. Comparison of Nine Statistical Model Based Warfarin Pharmacogenetic Dosing Algorithms Using the Racially Diverse International Warfarin Pharmacogenetic Consortium Cohort Database. PLoS One. 10, e0135784, https://doi.org/10.1371/journal.pone.0135784 (2015).
Caudle, K. E. et al. Clinical Pharmacogenetics Implementation Consortium. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. Clin. Pharmacol. Ther. 96, 542–548 (2014).
Krasniqi, V., Dimovski, A., Domjanović, I. K., Bilić, I. & Božina, N. How polymorphisms of the cytochrome P450 genes affect ibuprofen and diclofenac metabolism and toxicity. Arh. Hig. Rada. Toksikol. 67, 1–8 (2016).
Bergmeijer, T. O. et al. ICPC Investigators. Genome-wide and candidate gene approaches of clopidogrel efficacy using pharmacodynamic and clinical end points-Rationale and design of the International Clopidogrel Pharmacogenomics Consortium (ICPC). Am. Heart J. 198, 152–159 (2018).
Lin, X. B. et al. Population pharmacokinetics of voriconazole and CYP2C19 polymorphisms for optimizing dosing regimens in renal transplant recipients. Br. J. Clin. Pharmacol. 84, 1587–1597 (2018).
Hicks, J. K. et al. Clinical Pharmacogenetics Implementation Consortium. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Selective Serotonin Reuptake Inhibitors. Clin. Pharmacol. Ther. 98, 127–134 (2015).
Khan, B. A. et al. Cytochrome P450 Genetic Variation Associated with Tamoxifen Biotransformation in American Indian and Alaska Native People. Clin. Transl. Sci. 11, 312–321 (2018).
Dean, L. Clozapine Therapy and CYP2D6, CYP1A2, and CYP3A4 Genotypes. In Medical Genetics Summaries (ed. Pratt, V., McLeod, H., Rubinstein, W., Dean, L. & Malheiro, A.), http://www.ncbi.nlm.nih.gov/books/NBK367795/ (2012).
Luzum, J. A. et al. CYP2D6 Genetic Variation and Beta-Blocker Maintenance Dose in Patients with Heart Failure. Pharm. Res. 34, 1615–1625 (2017).
Giebułtowicz, J. et al. Salivary aldehyde dehydrogenase - temporal and population variability, correlations with drinking and smoking habits and activity towards aldehydes contained in food. Acta Biochim. Pol. 57, 361–368 (2010).
Saiki, J. P. et al. Aldehyde dehydrogenase 3A1 activation prevents radiation-induced xerostomia by protecting salivary stem cells from toxic aldehydes. Proc. Natl. Acad. Sci. USA 115, 6279–6284 (2018).
Chen, Y., Thompson, D. C., Koppaka, V., Jester, J. V. & Vasiliou, V. Ocular aldehyde dehydrogenases: protection against ultraviolet damage and maintenance of transparency for vision. Prog. Retin. Eye Res. 33, 28–39 (2013).
Ma, X. et al. Expression of glutathione S-transferase A1, a phase II drug-metabolizing enzyme in acute hepatic injury on mice. Exp. Ther. Med. 14, 3798–3804 (2017).
Wang, W. et al. Glutathione S-transferase A1 mediates nicotine-induced lung cancer cell metastasis by promoting epithelial-mesenchymal transition. Exp. Ther. Med. 14, 1783–1788 (2017).
Ansari, M. et al. GSTA1 diplotypes affect busulfan clearance and toxicity in children undergoing allogeneic hematopoietic stem cell transplantation, a multicenter study. Oncotarget. 8, 90852–90867 (2017).
Liu, C. et al. Genetic polymorphisms and lung cancer risk: Evidence from meta-analyses and genome-wide association studies. Lung Cancer. 113, 18–29 (2017).
Cao, T., Xu, N., Wang, Z. & Liu, H. Effects of Glutathione S-Transferase Gene Polymorphisms and Antioxidant Capacity per Unit Albumin on the Pathogenesis of Chronic Obstructive Pulmonary Disease. Oxid. Med. Cell Longev. 2017, 6232397, https://doi.org/10.1155/2017/6232397 (2017).
Audemard-Verger, A. et al. Glutathione S Transferases Polymorphisms Are Independent Prognostic Factors in Lupus Nephritis Treated with Cyclophosphamide. PLoS One. 11, e0151696, https://doi.org/10.1371/journal.pone.0151696 (2016).
Gataa, I., Emile, G., Loriot, M. A., Goldwasser, F. & Alexandre, J. Association between high antitumor activity of oxaliplatin and cyclophosphamide and constitutional GSTM1 homozygous deletion in an advanced ovarian cancer patient. Chemotherapy. 59, 290–293 (2013).
Abdur Rehman, M. Y., Kamal, A., Taqi, M. M. & Malik, R. N. Tracing biomarker of PAH-exposure and susceptibility factor (GSTM-polymorphism) among cancer patients in Pakistan. Chemosphere. 178, 384–390 (2017).
Thiebaut, F. et al. Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc. Natl. Acad. Sci. USA 84, 7735–7738 (1987).
Sui, H., Fan, Z. Z. & Li, Q. Signal transduction pathways and transcriptional mechanisms of ABCB1/Pgp-mediated multiple drug resistance in human cancer cells. J. Int. Med. Res. 40, 426–435 (2012).
Balayssac, D., Authier, N., Cayre, A. & Coudore, F. Does inhibition of P-glycoprotein lead to drug-drug interactions? Toxicol. Lett. 156, 319–329 (2005).
Qian, L. et al. The ABCC2 c.-24C > T polymorphism increases the risk of resistance to antiepileptic drugs: A meta-analysis. J. Clin. Neurosci. 37, 6–14 (2017).
da Rocha, I. M. et al. Polymorphisms associated with renal adverse effects of antiretroviral therapy in a Southern Brazilian HIV cohort. Pharmacogenet. Genomics. 25, 541–547 (2015).
Vinette, V., Placet, M., Arguin, G. & Gendron, F. P. Multidrug Resistance-Associated Protein 2 Expression Is Upregulated by Adenosine 5′-Triphosphate in Colorectal Cancer Cells and Enhances Their Survival to Chemotherapeutic Drugs. PLoS One. 10, e0136080, https://doi.org/10.1371/journal.pone.0136080 (2015).
Becker, M. L. et al. Genetic variation in the ABCC2 gene is associated with dose decreases or switches to other cholesterol-lowering drugs during simvastatin and atorvastatin therapy. Pharmacogenomics J. 13, 251–256 (2013).
Levy, K. D. et al. Prerequisites to implementing a pharmacogenomics program in a large health-care system. Clin. Pharmacol. Ther. 96, 307–309 (2014).
Acknowledgements
We dedicate this study to Mr. Abdul Sattar Edhi (circa. 1926 – 8 July 2016), who was a renowned humanitarian, social worker, ascetic, philanthropist and founder of Edhi Foundation. We are thankful to all the participating students, faculty, staff and administration of Jinnah Medical and Dental College, Karachi, Pakistan for their help and support. The skilful technical assistance of Britta Schwarten, Kiel University, is gratefully acknowledged. This study was supported through a generous research grant (No. 314140202132, Year 2012) by Alfaisal University, Riyadh, Saudi Arabia. We also thank Dr. Peter, M.B. Cahusac, Associate Professor of Pharmacology and Biostatistics, Alfaisal University, Riyadh, for his kind support in reviewing the article for English language.
Author information
Authors and Affiliations
Contributions
N.A.A. contributed in design of the study, experimental work, collection and analysis of data, acquisition of financial support, writing the manuscript, and administration and management of the project. H.B. contributed in experimental work. A.N.W. contributed in experimental design and work, analysis of data. M.K.N. contributed in study design and collection of data. H.R.A. contributed in study design, collection and analysis of data, and writing the manuscript. I.C. contributed in experimental design, analysis of data, writing the manuscript and overall supervision of the project at the participating institution. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Afsar, N.A., Bruckmueller, H., Werk, A.N. et al. Implications of genetic variation of common Drug Metabolizing Enzymes and ABC Transporters among the Pakistani Population. Sci Rep 9, 7323 (2019). https://doi.org/10.1038/s41598-019-43736-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43736-z
This article is cited by
-
Study on the Effect of Three CYP2C9 Variants on Drug–Drug Interaction Related to Six Drugs In Vitro by LC–MS/MS Method
Chromatographia (2022)
-
Functional phenotyping of the CYP2D6 probe drug codeine in the horse
BMC Veterinary Research (2021)
-
Meta-analysis of probability estimates of worldwide variation of CYP2D6 and CYP2C19
Translational Psychiatry (2021)
-
Pharmacogenetics of tamoxifen therapy in Asian populations: from genetic polymorphism to clinical outcomes
European Journal of Clinical Pharmacology (2021)
-
Elevated exposure to polycyclic aromatic hydrocarbons (PAHs) may trigger cancers in Pakistan: an environmental, occupational, and genetic perspective
Environmental Science and Pollution Research (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.