Abstract
An effective specific immunotherapy should contain elements to generate specific recognition (T-cell peptides) and to modulate the immunological response towards a Th1/Treg pattern by enhancing dendritic cells (DCs). We propose a novel sublingual immunotherapy for peach allergy, using systems, that combine Prup3-T-cell peptides with mannose dendrons (D1ManPrup3 and D4ManPrup3). Peach anaphylactic mice were treated 1, 2 and 5 nM concentrations. Tolerance was assessed one/five weeks after finishing treatment by determining in vivo/in vitro parameters after challenge with Prup3. Only mice receiving D1ManPrup3 at 2 nM were protected from anaphylaxis (no temperature changes, decrease in Prup3-sIgE and -sIgG1 antibody levels, and secreting cells) compared to PBS-treated mice. Moreover, an increase of Treg-cells and regulatory cytokines (IL-10+/IFN-γ+) in CD4+-T-cells and DCs were found. These changes were maintained at least five weeks after stopping treatment. D1ManPrup3 is an effective new approach of immunotherapy inducing protection from anaphylaxis which persists after finishing treatment.
Similar content being viewed by others
Introduction
The increasing prevalence of food allergy (FA) in developed countries, represents a heavy burden for health systems, affecting around 8% of children and 5% of adults1. FA is often induced by fruits, especially members of the Rosaceae family, such as peach and apple. The major allergens from this family are non-specific lipid transfer proteins (nsLTP), considered panallergens. Reactions present a complex clinical pattern, and a wide range of cross-reactivity to food derived from multiple sources, known as LTP syndrome2.
Avoidance of the causal food is the first-line approach for managing FA. However, accidental ingestion is often inevitable due to the ubiquity of panallergens and hidden sources3, strongly limiting quality of life, which has been described in one study of children as worse than for chronic diseases like diabetes4. Therefore, there is a clear need for safe and effective treatment.
One such approach is allergen specific immunotherapy (AIT). Clinical AIT studies have been performed for peanut, milk, hazelnut and kiwi5, however there is a risk of anaphylactic side effects during treatment with natural allergens6. For LTP allergy, sublingual immunotherapy (SLIT) with the major peach allergen, Prup3, produces clinically beneficial effects for mild, moderate, and even severe reactions7,8,9,10. Studies of the immunological events associated with the tolerant response induced by SLIT have found increases of allergen-specific IgG4 (sIgG4) and decreases of allergen-specific IgE (sIgE) and effector T cells (Th2 and Th9). These changes are orchestrated by dendritic cell (DCs) that modulate the response towards a Th1 pattern, and the generation of FoxP3+ regulatory T cells (Treg), which develop their suppressive activity mainly by the induction of IL-10+ Treg cells9,10,11.
Nevertheless, AIT does not fully reduce the risk of severe reactions5. The international consensus consortium on AIT has suggested approaches to improve the efficacy of AIT, such as allergen-derived peptides12 that lack the capacity to cross-link IgE or activate effector cells, making them safer, as demonstrated for house dust mites (HDM), grass13 and bee venom allergies14. However, recent trials, including a phase III trial with cat peptide AIT and a phase IIb trial with HDM peptide AIT, did not achieve their clinical end-points13 showing the need for further improvements.
One approach under study is combining the T-cell peptide with a system to induce appropriate antigen presentation by DCs. We have previously demonstrated that SLIT with a system combining Prup3 T-cell peptides and an oligodeoxyribonucleotide sequence with CpG motifs, intended to act as an adjuvant through TLR9 interaction, induces a specific Th1/Treg response producing protection from anaphylaxis15. Similar results were obtained by Srivastava et al., combining CpG coated nanoparticles with peanut extract16.
Targeting DCs can be further fine-tuned by altering the properties of the nanostructure, i.e. size/carbohydrate composition, to facilitate antigen uptake and presentation by DCs17. For example, glycosystems attaching of mannose to nanocarriers have been shown to improve uptake efficiency by targeting a DC C-type lectin receptor, affecting immunomodulation18,19.
In this study, we propose the use of glycodendropeptides (GDPs) to improve SLIT for treating FA. These GDPs include a Prup3 peptide, either monovalent (D1ManPrup3) or tetravalent (D4ManPrup3), bound to a mannose dendron structure. Results show that the monovalent molecule, D1ManPrup3 leads to protection upon allergen exposure, with no signs of anaphylaxis. Protection was maintained for at least five weeks after treatment and was associated with a reduced Th2 response (IgE and IgG1) and increased Th1/Treg (IFN-γ and IL-10).
Results
Synthesis of GDP nanostructures conjugated with Prup3 T-cell epitope
Synthesis of D1ManPrup3 and D4ManPrup3 (Fig. 1) was achieved using the strategy described in the Supplementary Material (See Fig. S1). We have previously prepared GDPs with different peptide epitopes20 using a similar approach. The glycodendritic platform contains a glycodendron moiety at one site and either 1 or 4 copies of a maleimide group at the other site. The glyco-maleimide dendrons can be used as common intermediates to be conjugated with any type of peptidic epitopes, highlighting the potential versatility of this approach. Here, GDPs D1ManPrup3 (6) and D4ManPrup3 (7) were prepared in good yields of high purity as demonstrated by HPLC and mass spectrometry (see Supplementary Material).
Analysis of the in vivo response to Prup3 after receiving SLIT with DnManPrup3
The SLIT with DnManPrup3 was safe and no mice showed any adverse effect during the treatment. The in vivo response was analyzed by change in body temperature before and after challenge with intraperitoneal Prup3 (Fig. 2B) either one or five weeks after SLIT, with no change indicating tolerance. All GDP treated animals showed a smaller drop in temperature than PBS treated, at both one and five weeks. Mice treated with 2 nM or 5 nM of either D1ManPrup3 or D4ManPrup3 showed little or no reduction in temperature upon challenge, similar to the non-sensitized mice, at one week after finishing SLIT, although a few of the D4ManPrup3 treated mice showed some decrease, as described below. 5 w after finishing, this lack of decrease after challenge was maintained for mice treated with D1ManPrup3 at 2 nM and D4ManPrup3 at 5 nM. The non-sensitized control group showed no change in temperature after challenge at any time point. The analysis of the response in group 17, treated with Prup3, indicated a similar decrease in the body temperature compared to the PBS treated group and that tolerance was only achieved in two out of ten mice (20%).
(A) Experimental procedures. Seven sensitization procedures were performed with Prup3 + LPS. SLIT started at week 6 for 8 weeks and mice were challenged with Prup3 at week 14 or 18. (B) In vivo evaluation of anaphylaxis after SLIT with D1ManPrup3 or D4ManPrup3. Dots show decreases in body temperature 30–40 min after challenge with Prup3, 1 week (black dots) or 5 weeks after ending the SLIT.
Nine mice (90%) treated with SLIT D1ManPrup3 at 2 nM and 5 nM and D4ManPrup3 at 2 nM maintained their body temperature without systemic symptoms, much higher than for mice treated with SLIT D1ManPrup3 at 1 nM (2 mice, 20%) and D4ManPrup3 at 1 nM (0 mice) and 5 nM (5 mice, 50%). Moreover, after 5 weeks without treatment, only the group treated with SLIT D1ManPrup3 at 2 nM contained a high percentage of mice (90%) showing no changes in body temperature.
Analysis of the humoral response to Prup3 after receiving SLIT with DnManPrup3
Assessment of serum specific antibody levels (Table 1) showed a decrease in Prup3-sIgE and sIgG1 in GDP treated mice compared to those treated with PBS, with the exception of those treated with D4ManPrup3 at 2 nM/5 nM for IgE and D4ManPrup3 5 nM for IgG1. Decreases were also observed for the number of Prup3-sIgE and -sIgG1-secreting cells as determined by ELISpot. We also compared antibody levels between those observed 5 w after finishing treatment and 1 w. This revealed a significant increase of Prup3-sIgE in those treated with D1ManPrup3 and D4ManPrup3 at 5 nM (p = 0.001 for both groups), showing similar levels compared to the PBS-treated group at 5 w. Regarding secreting cell numbers, an increase was observed for mice treated with D1ManPrup3 at 1 nM. No changes were observed in Prup3-sIgE and sIgG1 in Prup3 treated mice compared to those treated with PBS although significant decrease of Prup3-sIgE and -sIgG1-secreting cells (p = 0.017 and p = 0.0016, respectively) were found.
Analysis of the cellular response to Prup3 after receiving SLIT
There was a significant decrease in CD4+ T splenocyte proliferation to Prup3 in GDP-treated mice compared to the PBS-treated group, with the exception of D1ManPrup3 5 nM at 1 w (Fig. 3A).
Evaluation of the cellular response to Prup3 after SLIT with D1ManPrup3 or D4ManPrup3. (A) Mean and S.D. Prup3-specific CD4+T-splenocytes proliferation index. Statistically significant differences (p < 0.05) compared to PBS-treated represented as *. (B) Median and interquartile ranges for CD11c+ (Left) and CD4+-cell percentages (Right) producing intracellular IL-4/IFN-γ. Significant differences (p < 0.05) compared to PBS treated group represented as *.
We evaluated the intracellular production of IL-4 and IFN-γ in DCs from lymph nodes and splenocytes after Prup3 stimulation (Fig. 3B). In DCs, a decrease in IL-4-producing CD11c+-cells was observed for all mice treated with D1ManPrup3 at all concentrations at both 1 w and 5 w post treatment, and with D4ManPrup3 at 2 nM, compared to the PBS-treated group. In contrast, an increase of IFN-γ-producing CD11c+-cells only occurred in animals treated with at 1 and 2 nM of D1ManPrup3 at 1 w, and 2 nM of D4ManPrup3 at 1 w. An increase was also observed for 2 and 5 nM of D1ManPrup3 at 5 w (Fig. 3B left).
In CD4+ cells, a significant decrease in IL-4-producing cells was observed in mice treated with either GDP at 2 and 5 nM compared to PBS-treated group, at both 1 w and 5 w. Moreover, an increase in IFN-γ-producing CD4+-cells was observed in mice treated with D1ManPrup3 at 2 and 5 nM at 1 w, and for 2 nM at 1 w; and with D4ManPrup3 at 2 nM at 1 w, and 5 nM at 5 w (Fig. 3B, right).
Analysis of the regulatory response to Prup3 after receiving SLIT
We further analyzed the influence of SLIT on the cellular regulatory response by analyzing changes in regulatory DCs (CD11c+CD103+) and CD4+ splenocytes (CD4+CD25+FoxP3+) (Fig. 4). No significant differences for regulatory DCs were found compared to PBS-treated mice, for any condition except for mice treated with D4ManPrup3 at 5 nM and after 5 w (Fig. 4A left). A significant increase in Tregs was observed for mice treated with D1ManPrup3 at 2 or 5 nM, and D4ManPrup3 at 2 nM at 1 w (Fig. 4B left). These increases disappeared at 5 w in mice treated with D1ManPrup3 at 5 nM. Interestingly, in mice treated with D4ManPrup3 at 5 nM a significant increase of both regulatory DCs and Tregs appeared at 5 w only.
Evaluation of the regulatory response during SLIT with D1ManPrup3 or D4ManPrup3. (A) Median and interquartile ranges for percentages of CD11c+CD103+ cells (Left) and cells producing intracellular IL-10 (Right). (B) Median and interquartile ranges for percentages of regulatory CD4+CD25+FoxP3+ cells (Left) and cells producing intracellular IL-10 (Right). Significant differences (p < 0.05) are represented as * when compared to PBS treated group.
The analysis of IL10-producing cells showed a significant increase in mice treated with D1ManPrup3 at 2 and 5 nM and with D4ManPrup3 at 2 nM in both DCs and CD4 cells at 1 w. These increases were maintained in CD4 cells but not in DCs for D1ManPrup3; in the case of mice treated with D4ManPrup3 the increase disappeared in both DCs and CD4 cells (Fig. 4 right).
Discussion
Food allergy is becoming an important health problem for children and adults1,21. Current treatments, such as AIT show promise, but in many cases, such as LTP syndrome, better treatments are required2.
One potential factor for the current lack of AIT efficacy may be related to allergen concentration. However, given that complete proteins from the allergenic extracts are used in conventional AIT, higher concentrations might increase allergic reactions. Moreover, despite efforts towards standardization, large-scale production of vaccines using natural protein extracts can lead to differences between batches. Therefore, there is much interest in the development of new immunotherapy approaches, including modified food allergens or peptides. The use of longer contiguous overlapping peptides for cat allergy22 although promising in initial trials, did not achieve the clinical end points at phase II, with no differences compared to placebo13. It may be the case that this type of treatment requires the immunological system to be boosted by adding an adjuvant. To this end, adjuvants that interact with toll like receptors (TLRs), specifically with TLR9, have been used to shift the Th2 immune response towards a Th1/Treg balance in allergic rhinitis23 as well as FA24. Our group recently showed that the use of this ligand with a dendrimeric structure containing Prup3-T cell peptides induced protection from anaphylaxis in experimental models15. Similar results have also been found for peanut extract16.
In addition to TLRs, C-type lectin receptors represent another potential target on antigen presenting cells that can improve the uptake and presentation of different compounds modulating the immunological response, as has been demonstrated using gold nanoparticles and glycodendrimers17,19. In allergic diseases, mannan-conjugated allergoids have been shown to increase allergen uptake and induce splenic Foxp3+Treg cell production25. For this we designed a new synthetic strategy which confers an important advantage in that it uses glycodendritic platforms that can be functionalized easily using a thiol-ene reaction by a terminal cysteine present at one end of the peptide epitope. Here, we have put these elements together to create a novel SLIT approach for peach allergy, in which one or four Prup3 T-cell peptides are combined with mannose dendrons.
The results suggest that the optimal quantity of SLIT using D1ManPrup3 or D4ManPrup3 would be 2 nM, as this led to the most tolerant response, as measured by no changes in body temperature upon challenge, a decrease of Prup3-specific IgE and -IgG1 level and secreting cells as well as Prup3 specific-splenocyte CD4 proliferation and IL-4 production accompanied by an increase in IFN-γ and IL-10-producing splenocytes and Tregs. Compared to previous results from our group where CpG was used as adjuvant, the percentage of cases with tolerant responses was a little bit higher: 90% with D1ManPrup3 vs 80% with D1Prup3 + CpG, with similar results at in vitro levels15.
We also assessed the effect of SLIT with these GDPs on DCs since, as has been reported, AIT efficacy may directly correlate with the capability of SLIT to modulate DCs13. After treatment with D1ManPrup3 at 2 nM, we observed a significant decrease of IL-4, in parallel with an increase of IFN-γ and IL-10-producing DCs. This suggests that SLIT is modulating DCs to produce the specific signalling molecules needed to induce Tregs and thus supress the Th2 response26. It has been reported that changes in CD103+CD11c+DCs during AIT are related to the induction of antigen-specific Foxp3+Treg cells27, however although we observed increases in FoxP3+Tregs, no significant change in CD103+CD11c+DCs was found. This discrepancy could be due to the fact that CD103+CD11c+DCs from different lymph nodes were analyzed together, making it difficult to find population-specific changes. Further studies should be performed to identify whether only a subset of DCs, i.e. from the submandibular27 or mesenteric lymph nodes28, are modified by our system.
One of the main aims of SLIT as a FA treatment is to induce sustained unresponsiveness that persists after finishing treatment. However, to date only a handful of studies have addressed this aspect, and only for oral immunotherapy29,30. In animal models the protective effects induced by oral immunotherapy with egg white or ovomucoid were lost after 2 weeks31. Here, we found that only D1ManPrup3 at 2 nM induced the maintenance of tolerance five weeks after stopping SLIT, with 90% of the mice in this group not showing anaphylactic symptoms. Moreover, this was underlined by similar immunological changes to those obtained one week after finishing treatment. Importantly in our model, this sustained unresponsiveness was achieved without continued exposure to the allergen, which has previously been proposed by others as a requirement to maintain the unresponsive state29.
Regarding D4ManPrup3 at 2 nM, although beneficial effects were observed 1 week after treatment, these disappeared after 5 weeks, indicating a desensitization effect rather than sustained unresponsiveness. Previous work from our group investigating SLIT using dendrimeric structures with CpG as an adjuvant found that the tetrameric structure afforded no protection at all15. It may be that D4ManPrup3 is more effective in this current study due to the presence of mannose rather than CpG. The lesser effects of D4ManPrup3, compared to D1ManPrup3, could be due to the size of the nanostructure or differences in presentation, which may affect DC uptake and the induction of the immunosuppressive Th1/Treg responses32. Moreover although further studies are necessary, we have observed that these tetrameric compounds, both with CpG15 and with mannose (data not shown) have the capacity to cross-link at least two sIgE on the basophil surface, which is associated with an allergic or Th2 response.
One interesting finding is that D1ManPrup3 only induced a long-term beneficial effect when administered at 2 nM. This long term effect obtained with D1ManPrup3 at 2 nM was associated with the induction of FoxP3+Treg cells and IL-10 production, both of which are thought to be essential in tolerance induction33,34. Higher concentrations of 5 nM, induced a protective effect initially, however this disappeared after 5 weeks. This dose-dependent effect has been observed in 2 trials of intranasal AIT for rhinitis and rhinoconjunctivitis35,36 and in a study of AIT in a murine model of shrimp allergy33. This lower effect may be explained by the results of previous studies showing that a high concentration of antigen exposure is related with a Th2 polarization and a lack of FoxP3+Treg induction37,38
In conclusion, we have shown that SLIT with a monomeric GDP of Prup3, D1ManPrup3, induces protection, as defined by an absence of anaphylaxis symptoms, against the allergen, Prup3. This tolerance was associated with a decreased Th2 response (IgE, IgG1 and IL-4) and an increased Th1/Treg pattern (IFN-γ and IL-10). Moreover, the long-term sustained unresponsiveness persisted for at least five weeks after treatment and without the need to maintain regular contact with the allergen. Thus, D1ManPrup3 represents a promising new specific immunotherapy approach that does not require additional adjuvants and moreover, the molecular design and chemical route for access to the composition make it highly versatile and potentially adaptable to other types of allergens for which the chemical structure of the antigenic determinants are known.
Methods
Synthesis of GDPs including Prup3-epitope
The synthesis and characterization of GDPs (Fig. 1) is described in detail in the Supplementary Material (Figs S1–S5). Selected peptide includes the essential residues to induce immunological responses in human PBMCs, including T and B epitopes39.
Sensitization and Immunotherapy procedures
The experimental procedures in animals were approved by the Animal Experimentation Ethics Committee of BIONAND, Malaga, Spain, (REF26072017) according to international standards of animal welfare and confirming that all experiments were performed in accordance with relevant guidelines and regulations. SLIT efficacy was assessed using a previously established murine model of peach allergy15. BALB/c mice (female, 4–5 weeks: Janvier Lab, Saint-Berthevin Cedex, France) were used, divided into 17 different groups (N = 10 per group) (Table 2). The protocols for sensitization, immunotherapy and challenge were as described15,40.
Sensitization
Mice from groups 3–17 were anaesthetized and treated with 20 µg of natural Prup3 (Bial Laboratory, Zamudio, Spain) (optimal concentration after previous studies) and 20 ng of LPS (InvivoGen, San Diego, CA) in a final volume of 12 µl applied intranasally. This approach was chosen based on our previous experience by which only in combination with LPS, Prup3-specific anaphylaxis can be generated after nasal sensitisation40 since the respiratory tract has also been suggested in food sensitization41,42. The administration schedule was three consecutive days plus once a week for four weeks. The same schedule and volume were followed with PBS in mice of group 1 (Table 2).
Immunotherapy
At week 6, after sensitization, mice from groups 5–16 were treated sublingually with 10 µl of D1ManPrup3 or D4ManPrup3 (1, 2 or 5 nM/dose), weekly for eight weeks. For mice of group 3 and 4 we followed the same schedule but with 10 µl of PBS and for group 17 with Prup3 at 10 µg/mL (Table 2).
In vivo assessment of tolerant response
The immunotherapy efficacy was assessed by determining the inhibition of the appearance of systemic anaphylaxis after challenge with Prup3 in one intraperitoneal dose (100 µg). This was evaluated by measuring change in body temperature with a rectal probe, and by assessing physical and behavioural symptoms (according to a scoring system) at weeks 14 and 18, 30–40 min (Fig. 2A). The most characteristic symptoms were inactivity, isolation from other animals, difficulty breathing and convulsions.
For further studies, blood from mice were obtained from the retro-orbital plexus on day 0 (basal) and at either week 14 or 18 after challenge, and sera were stored at −20 °C. After challenge and in vivo evaluation, mice were sacrificed by cervical dislocation and the spleen and lymph nodes were removed aseptically and teased to prepare a single-cell suspension for cellular analysis.
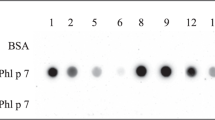
Prup3-sIgE and -sIgG1 levels and secreting cells determination
The levels of Prup3-specific IgE and IgG1 were measured by ELISA as described (Rodriguez, Mascaraque, et al., 2017). The results are expressed as optical density.
The number of antibody-secreting cells was measured using an ELISpot assay as previously described40. The results are expressed as number of Ig secreting cells.
Evaluation of the cellular response
Proliferative response of CD4 and CD8 spleen cells after immunotherapy was assessed by flow cytometry as described15,40. Results were expressed as proliferation index (PI) for CD4+ or CD8+ measured as the ratio: %CD4+CFSEdim or %CD8+CFSEdim in stimulated sample/%CD4+CFSEdim or %CD8+CFSEdim in non-stimulated sample and considered positive when the ratio was higher than 2.
The cytokine pattern was evaluated in spleen cells by determining intracellular cytokines using BD Cytofix/CytoPerm Fixation/Permeabilization solution kit (BD™ Biosciences) and staining with specific fluorochrome-conjugated mAbs, anti-IFNγ-APCCy7, ant-iIL-4-PE-Cy7A and anti-IL-10-PE (BD Pharmingen). Regulatory cells were defined as CD3+CD4+CD25+FoxP3+ using anti-CD25 and FoxP3 (BD Pharmingen). Results are expressed as percentages.
Studies of dendritic cells and cytokine production
Dendritic cells were purified from axillary, cervical, inguinal and mesenteric lymph nodes by positive selection using CD11c microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany). The CD11c+ fraction was incubated in the absence (negative control) or presence of Prup3 at 25 µg/mL at 37 °C and 5% of CO2.
In order to assess dendritic cells regulatory responses, after 48 hours of the culture, the cells were stained with specific fluorochrome-conjugated mAbs, anti-CD11c-APC and anti-CD103-FITC and phenotyped as described above. For intracellular cytokine detection, cells were fixed, stained and phenotyped, using anti-IFNγ-APCCy7, anti-IL-4-PE-Cy7A and anti-IL-10-PE (BD Pharmingen). Results are expressed as percentages.
Statistical analysis
Data are presented as individual data values or mean and standard deviation (S.D.). For unrelated samples comparisons Mann-Whitney U, Kruskal-Wallis or χ2-test were used. Related samples were compared using the Wilcoxon signed-rank test. P-values lower than 0.05 were considered statistically significant.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
17 April 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Sicherer, S. H. & Sampson, H. A. Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. The Journal of allergy and clinical immunology 133, 291–307; quiz 308, https://doi.org/10.1016/j.jaci.2013.11.020 (2014).
Fernandez-Rivas, M. Fruit and vegetable allergy. Chemical immunology and allergy 101, 162–170, https://doi.org/10.1159/000375469 (2015).
Sampson, H. A. Food-induced anaphylaxis. Novartis Foundation symposium 257, 161–171; discussion 171–166, 207–110, 276–185 (2004).
Flokstra-de Blok, B. M. et al. Health-related quality of life of food allergic patients: comparison with the general population and other diseases. Allergy 65, 238–244, https://doi.org/10.1111/j.1398-9995.2009.02121.x (2010).
Chen, M. & Land, M. The current state of food allergy therapeutics. Human vaccines & immunotherapeutics 13, 2434–2442, https://doi.org/10.1080/21645515.2017.1359363 (2017).
Wai, C. Y. Y., Leung, N. Y. H., Leung, P. S. C. & Chu, K. H. Immunotherapy of Food Allergy: a Comprehensive Review. Clinical reviews in allergy & immunology, https://doi.org/10.1007/s12016-017-8647-y (2017).
Lucendo, A. J., Arias, A. & Tenias, J. M. Relation between eosinophilic esophagitis and oral immunotherapy for food allergy: a systematic review with meta-analysis. Annals of allergy, asthma & immunology: official publication of the American College of Allergy, Asthma, & Immunology 113, 624–629, https://doi.org/10.1016/j.anai.2014.08.004 (2014).
Garcia, B. E. et al. Sublingual immunotherapy in peach allergy: monitoring molecular sensitizations and reactivity to apple fruit and Platanus pollen. Journal of investigational allergology & clinical immunology 20, 514–520 (2010).
Gomez, F. et al. The clinical and immunological effects of Prup3 sublingual immunotherapy on peach and peanut allergy in patients with systemic reactions. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology 47, 339–350, https://doi.org/10.1111/cea.12901 (2017).
Palomares, F. et al. Immunological Changes Induced in Peach Allergy Patients with Systemic Reactions by Prup3 Sublingual Immunotherapy. Molecular nutrition & food research, https://doi.org/10.1002/mnfr.201700669 (2017).
Shamji, M. H. et al. Biomarkers for monitoring clinical efficacy of allergen immunotherapy for allergic rhinoconjunctivitis and allergic asthma: an EAACI Position Paper. Allergy 72, 1156–1173, https://doi.org/10.1111/all.13138 (2017).
Jutel, M. et al. International Consensus on Allergen Immunotherapy II: Mechanisms, standardization, and pharmacoeconomics. The Journal of allergy and clinical immunology 137, 358–368, https://doi.org/10.1016/j.jaci.2015.12.1300 (2016).
Berings, M. et al. Advances and highlights in allergen immunotherapy: On the way to sustained clinical and immunologic tolerance. J Allergy Clin Immunol 140, 1250–1267, https://doi.org/10.1016/j.jaci.2017.08.025 (2017).
Larche, M. T cell epitope-based allergy vaccines. Current topics in microbiology and immunology 352, 107–119, https://doi.org/10.1007/82_2011_131 (2011).
Rodriguez, M. J. et al. Prup3-Epitope-based sublingual immunotherapy in a murine model for the treatment of peach allergy. Molecular nutrition & food research 61, https://doi.org/10.1002/mnfr.201700110 (2017).
Srivastava, K. D. et al. Investigation of peanut oral immunotherapy with CpG/peanut nanoparticles in a murine model of peanut allergy. The Journal of allergy and clinical immunology 138, 536–543 e534, https://doi.org/10.1016/j.jaci.2016.01.047 (2016).
Le Guevel, X. et al. Multivalent Glycosylation of Fluorescent Gold Nanoclusters Promotes Increased Human Dendritic Cell Targeting via Multiple EndocyticPathways. ACS applied materials & interfaces 7, 20945–20956, https://doi.org/10.1021/acsami.5b06541 (2015).
Ribeiro-Viana, R. et al. BODIPY-labeled DC-SIGN-targeting glycodendrons efficiently internalize and route to lysosomes in human dendritic cells. Biomacromolecules 13, 3209–3219, https://doi.org/10.1021/bm300998c (2012).
Mascaraque, A. et al. stimulate dendritic cell maturation and T cell proliferation: a potential influenza A virus immunotherapy. MedChemComm 6, 1755–1760, https://doi.org/10.1039/C5MD00133A (2015).
Kowalczyk, W., Mascaraque, A., Sánchez-Navarro, M., Rojo, J. & Andreu, D. Convergent Synthesis of Glycodendropeptides by Click Chemistry Approaches. Eur. J. Org. Chem 24, 4565–4573 (2012).
Umasunthar, T. et al. Incidence of fatal food anaphylaxis in people with food allergy: a systematic review and meta-analysis. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology 43, 1333–1341, https://doi.org/10.1111/cea.12211 (2013).
Patel, D. et al. Fel d 1-derived peptide antigen desensitization shows a persistent treatment effect 1 year after the start of dosing: a randomized, placebo-controlled study. J Allergy Clin Immunol 131(103-109), e101–107, https://doi.org/10.1016/j.jaci.2012.07.028 (2013).
Kulis, M., Gorentla, B., Burks, A. W. & Zhong, X. P. Type B CpG oligodeoxynucleotides induce Th1 responses to peanut antigens: modulation of sensitization and utility in a truncated immunotherapy regimen in mice. Molecular nutrition & food research 57, 906–915, https://doi.org/10.1002/mnfr.201200410 (2013).
Lehfeldt, H., Tietze, C. & Gorstein, F. Ovarian pregnancy and the intrauterine device. American journal of obstetrics and gynecology 108, 1005–1009 (1970).
Schulke, S. & Vieths, S. Dendritic cell targeting with C-type lectins for improvement of allergen immunotherapy. The Journal of allergy and clinical immunology 138, 568–570, https://doi.org/10.1016/j.jaci.2016.06.006 (2016).
Kapsenberg, M. L. Dendritic-cell control of pathogen-driven T-cell polarization. Nat Rev Immunol 3, 984–993, https://doi.org/10.1038/nri1246 (2003).
Tanaka, Y. et al. Oral CD103(−)CD11b(+) classical dendritic cells present sublingual antigen and induce Foxp3(+) regulatory T cells in draining lymph nodes. Mucosal immunology 10, 79–90, https://doi.org/10.1038/mi.2016.46 (2017).
Coombes, J. L. et al. A functionally specialized population of mucosal CD103+ DCs induces Foxp3+ regulatory T cells via a TGF-beta and retinoic acid-dependent mechanism. J Exp Med 204, 1757–1764, https://doi.org/10.1084/jem.20070590 (2007).
Vickery, B. P. et al. Sustained unresponsiveness to peanut in subjects who have completed peanut oral immunotherapy. The Journal of allergy and clinical immunology 133, 468–475, https://doi.org/10.1016/j.jaci.2013.11.007 (2014).
Varshney, P. et al. A randomized controlled study of peanut oral immunotherapy: clinical desensitization and modulation of the allergic response. The Journal of allergy and clinical immunology 127, 654–660, https://doi.org/10.1016/j.jaci.2010.12.1111 (2011).
Leonard, S. A., Martos, G., Wang, W., Nowak-Wegrzyn, A. & Berin, M. C. Oral immunotherapy induces local protective mechanisms in the gastrointestinal mucosa. J Allergy Clin Immunol 129, 1579–1587 e1571, https://doi.org/10.1016/j.jaci.2012.04.009 (2012).
Inoue, K. et al. Effects of multi-walled carbon nanotubes on a murine allergic airway inflammation model. Toxicology and applied pharmacology 237, 306–316, https://doi.org/10.1016/j.taap.2009.04.003 (2009).
Leung, N. Y. H. et al. Low-Dose Allergen-Specific Immunotherapy Induces Tolerance in a Murine Model of Shrimp Allergy. International archives of allergy and immunology 174, 86–96, https://doi.org/10.1159/000479694 (2017).
Dioszeghy, V. et al. Differences in phenotype, homing properties and suppressive activities of regulatory T cells induced by epicutaneous, oral or sublingual immunotherapy in mice sensitized to peanut. Cellular & molecular immunology, https://doi.org/10.1038/cmi.2016.14 (2016).
Pocobelli, D., Del Bono, A., Venuti, L., Falagiani, P. & Venuti, A. Nasal immunotherapy at constant dosage: a double-blind, placebo-controlled study in grass-allergic rhinoconjunctivitis. J Investig Allergol Clin Immunol 11, 79–88 (2001).
Marcucci, F. et al. Low-dose local nasal immunotherapy in children with perennial allergic rhinitis due to Dermatophagoides. Allergy 57, 23–28 (2002).
Hashiguchi, M., Hachimura, S., Ametani, A. & Kaminogawa, S. Th2 polarization enhanced by oral administration of higher doses of antigen. Cytotechnology 33, 237–245, https://doi.org/10.1023/A:1008102304740 (2000).
Kretschmer, K. et al. Inducing and expanding regulatory T cell populations by foreign antigen. Nature immunology 6, 1219–1227, https://doi.org/10.1038/ni1265 (2005).
Tordesillas, L. et al. T-cell epitopes of the major peach allergen, Prup3: Identification and differential T-cell response of peach-allergic and non-allergic subjects. Molecular immunology 46, 722–728, https://doi.org/10.1016/j.molimm.2008.10.018 (2009).
Rodriguez, M. J. et al. LPS promotes Th2 dependent sensitisation leading to anaphylaxis in a Prup3 mouse model. Scientific reports 7, 40449, https://doi.org/10.1038/srep40449 (2017).
Lack, G. et al. Factors associated with the development of peanut allergy in childhood. The New England journal of medicine 348, 977–985, https://doi.org/10.1056/NEJMoa013536 (2003).
Tordesillas, L. et al. Skin exposure promotes a Th2-dependent sensitization to peanut allergens. The Journal of clinical investigation 124, 4965–4975, https://doi.org/10.1172/JCI75660 (2014).
Acknowledgements
The authors would like to thank Mrs Reyes Molina from the animal facility service at the Andalusian Centre for Nanomedicine & Biotechnology (BIONAND), Malaga, Spain. Mrs Ana Molina for the immunological analysis in IBIMA laboratories, Malaga, Spain and David Andreu from the Department of Experimental and Health Sciences, Universitat Pompeu Fabra of Barcelona for the synthesis of Prup3 T-cell peptide. The study was funded by the Institute of Health “Carlos III” of the Ministry of Economy and Competitiveness: PI12/02481, PI15/00559 and PI18/00288, RETICS ARADyAL (RD16/0006/0001, /0003, /0011) and Sara Borrell Program (CD14/00242). Andalusian Regional Ministry of Economy and Knowledge: CTS-7433), Nicolas Monardes Program (C-0044-2012 SAS2013) and the Spanish Ministry of Economy and Competitiveness (CTQ2014-52328-P, CTQ2017-86265-P and AGL2014-52395-C2-2) and a FPI grant (JRS). Grants were cofunded by the European Regional Development Fund (ERDF).
Author information
Authors and Affiliations
Contributions
C.M., J.R. and A.D.P. conceived and designed the study and were involved in analysis and interpretation and manuscript production. M.J.R., A.M. and J.R.S. performed the experiments, data analysis and drafted the article. M.J.T. helped write and revise the article. F.G. was involved in conducting the experiments and data analysis; J.R.P. was involved in data analysis and final manuscript revision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rodriguez, M.J., Ramos-Soriano, J., Perkins, J.R. et al. Glycosylated nanostructures in sublingual immunotherapy induce long-lasting tolerance in LTP allergy mouse model. Sci Rep 9, 4043 (2019). https://doi.org/10.1038/s41598-019-40114-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-40114-7
This article is cited by
-
C-Type Lectin Receptor Mediated Modulation of T2 Immune Responses to Allergens
Current Allergy and Asthma Reports (2023)
-
Nanomaterials for antigen-specific immune tolerance therapy
Drug Delivery and Translational Research (2023)
-
Transcriptome Analysis of Reciprocal Hybrids Between Crassostrea gigas and C. angulata Reveals the Potential Mechanisms Underlying Thermo-Resistant Heterosis
Marine Biotechnology (2023)
-
Transcriptional changes in dendritic cells underlying allergen specific induced tolerance in a mouse model
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.