Abstract
Post-endoscopic submucosal dissection bleeding (PEB) is one of the important complications after endoscopic submucosal dissection (ESD), but still difficult to predict. The present study aimed to identify significant risk factors for PEB according to onset time. Between November 2008 and January 2016, a total of 1864 lesions resected via ESD were analyzed. PEB was classified as either early or late according to onset time (within or after 24 hours post-ESD, respectively). During second-look endoscopy, the artificial ulcer bed was subjected to Forrest classification. A high risk of stigma was defined as active spurting bleeding, oozing bleeding, and a non-bleeding visible vessel in the ulcer. The endoscopic factors and medications associated with PEB were analyzed. PEB occurred in 77 lesions (4.1%): early only in 46 (2.4%), late only in 22 (1.1%), and early and late in 9 (0.4%). Among 55 early PEB events, 25 were asymptomatic and diagnosed during second-look endoscopy. Age ≤65 years, resection size ≥30 mm, procedure time ≥20 min, lower third of the stomach, erosion, and clopidogrel use were significantly associated with early PEB. If the number of risk factors were ≤1, the risk of early PEB was 0.6%. For late PEB, the mid to upper third of the stomach, undifferentiated carcinoma, erosion, high risk of stigma during second-look endoscopy, history of early PEB, and clopidogrel use were significant risk factors. If risk factors were absent, the risk of late PEB was 0.1%. For patients at high risk of early PEB, selective second-look endoscopy might be a useful. For patients at high risk of late PEB, careful monitoring of bleeding should be considered.
Similar content being viewed by others
Introduction
Endoscopic resection for early gastric cancer (EGC) and adenoma is a well-established treatment modality. The Japanese Gastric Cancer Association recommends endoscopic resection as a first-line treatment for differentiated mucosal cancer lesions ≤20 mm in size without ulceration1. Endoscopic submucosal dissection (ESD) for EGC and gastric adenoma has shown a higher en-bloc resection rate and a lower local recurrence rate than conventional endoscopic mucosal resection using an electrosurgical snare2. However, the longer procedure time and higher complication rate associated with ESD such as iatrogenic perforation and bleeding are obstacles to the widespread use of ESD2. Iatrogenic perforation and long procedure time can be overcome with greater surgical experience and endoscopic instruments. However, post-ESD bleeding (PEB) occurs in 4.5–5.7% of patients3.
Intraoperative bleeding during mucosal incision and submucosal dissection is generally not considered a complication until a patient requires a blood transfusion or emergent surgical/radiological intervention. However, delayed PEB detected several hours to days after ESD may result in serious cardiovascular complications. Consensus is lacking on the optimal management of artificial gastric ulcers after ESD such as use of anti-secretory agents (which drugs, optimal doses, and optimal treatment duration) and routine use of second-look endoscopy. Although studies showed that 33–74% of PEB cases occur within 24 hours of ESD4,5,6, several studies of the routine use of second-look endoscopy after ESD showed no advantage for the prevention of PEB6,7,8,9. However, those studies enrolled relatively a small number of cases and excluded patients taking antiplatelet or antithrombotic medications.
Because unmeasurable factors such as surgical experience, technical factors, and undiagnosed comorbid conditions may be related to PEB, the reported risk factors of PEB are inconsistent3. Here we aimed to analyze factors associated with PEB (early within 24 hours and late 24 hours post-ESD) for gastric epithelial neoplasms (EGC and adenoma).
Materials and Methods
Patients
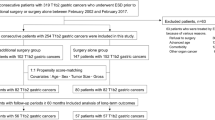
Between November 2008 and January 2016, the medical records of patients who underwent ESD at Pusan National University Yangsan Hospital (PNUYH) in the Republic of Korea were reviewed retrospectively. During the study period, a total of 1942 gastric tumors were resected via ESD. Cases of benign submucosal tumor (n = 29), lymphoma (n = 2), neuroendocrine tumor (n = 4), iatrogenic perforation during ESD (n = 8), and no evidence of tumor after ESD (n = 35) were excluded. Finally, a total of 1864 gastric epithelial tumors were enrolled and analyzed (Fig. 1). Written informed consent, including procedure and complications was obtained from all patients before ESD. The present study was approved by the ethics committee of the institutional review board of Pusan National University (L-2018-145).
Procedure
A standard single-channel endoscope (GIF-H260, GIF-H260Z, or GIF-HQ290; Olympus Optical, Tokyo, Japan) or a two-channel endoscope (GIF-2TQ260M; Olympus Optical) was used at the surgeons’ discretion. During ESD, after creating a marking of 1–2 mm outside the lesion, a submucosal injection of a solution containing a mixture of normal saline, epinephrine, and indigo carmine was made before the incision or submucosal dissection. A circumferential mucosal incision outside the marking was performed using an electrosurgical generator (ERBEVIO 300D, Endocut I mode, effect 3, duration 2; Erbe Co, Tubingen, Germany). During the submucosal dissection, a coagulation current (Swift coagulation 60 W, ERBE VIO 300D; Erbe Co) was used. After lesion removal, preventive coagulation (Soft coagulation 60 W, ERBE VIO 300D, Erbe Co) was performed of all visible vessels (Fig. 2).
Steps of endoscopic submucosal dissection (ESD). (A) diagnostic endoscopy showed a depressed mucosal lesion with central depression and reddish color change at the antrum. (B) artificial ulcer just after ESD. (C) adherent clot on the artificial ulcer base during second-look endoscopy the day after ESD. (D) post-coagulation state during second-look. (E) Artificial ulcer bed without bleeding or clots the day after second-look endoscopy. (F) artificial ulcer scar after 8 weeks proton pump inhibitor treatment.
Before the ESD procedure, an intravenous bolus injection of a proton pump inhibitor (pantoprazole 40 mg every 12 hours for 48 hours) was started. We usually recommend discharge 48 hours after ESD when there was no evidence of gastrointestinal bleeding and a regular oral dose of a proton pump inhibitor was started for 8 weeks. When a patient was using an antiplatelet medication (low-dose aspirin or clopidogrel) or antithrombotic medication (warfarin), we consulted the cardiovascular department for guidance on medication management. All patients taking antiplatelet and antithrombotic drugs were asked to stop the medication for 7 days before ESD. For patients using dual antiplatelet or antithrombotic medications, clopidogrel or warfarin was stopped without interruption of the low-dose aspirin. For patients with a high thromboembolic risk, bridging therapy using heparin was performed. All antiplatelet or antithrombotic drugs were restarted 1–2 days post-ESD.
H. pylori diagnosis was performed simultaneously with endoscopic forceps biopsy and rapid urease test at least 2 weeks holding PPI at the 2–6 month follow up endoscopic examination. When both or one of the tests were positive, H. pylori eradication treatment was performed.
Definition
Second-look endoscopy was performed in all patients the day after ESD. The high risk of stigma during second-look endoscopy was subjected to Forrest classification (Fig. 3)10. During second-look endoscopy, high risk of stigma was defined as spurting blood (Forrest type Ia), oozing blood (Forrest type Ib), and non-bleeding visible vessels (Forrest type IIa). Preventive coagulation was performed for all patients at high risk of stigma on the ulcer bed. We removed adherent clots (Forrest type IIb) and reclassified them according to whether or not there was high risk of stigma. A PEB was defined as clinical evidence of bleeding in the artificial ulcer lesions such as overt hematemesis, melena, spurting or oozing bleeding from the artificial ulcer bed, and the presence of fresh blood or clots in the stomach during endoscopic examination. During second-look endoscopy, oozing blood on the artificial ulcer bed without evidence of blood or clots in the stomach was classified as high risk of stigma rather than PEB. PEB detected during or before the second-look endoscopy within 24 hours was classified as early PEB, whereas that detected after 24 hours was classified as late PEB.
Lesion location was classified as the lower third, middle third, or upper third of the stomach11. Each lesion’s maximal diameter was measured via pathologic examination of each resected specimen. Lesion color was compared to the background mucosa. Nodularity was defined as an irregularly raised or nodular mucosal surface. Submucosal fibrosis was recorded after confirming the presence of fibrosis during submucosal dissection. The extent of atrophic gastritis was measured by the endoscopic Kimura–Takemoto classification system: mild (normal to closed type 2), moderate (closed type 3 to open type 1), and severe (open type 2 to open type 3)12. The procedure time was calculated from the marking of the lesion to the completion of preventive coagulation of the artificial ulcer bed after lesion removal. Low risk of post-ESD bleeding was defined as the incidence of bleeding being less than 1% according to the number of significant risk factors after multivariate analysis13.
The resected specimens were stretched, pinned, and fixed in formalin. Fixed specimens were then sectioned at 2 mm intervals. En-bloc resection was defined as a resection in a single piece of the lesion. Complete resection was defined as the absence of tumor cells at the margins of an en-bloc resected specimen.
Statistical analyses
Univariate analysis was performed using the chi-square test or Fisher’s exact test for categorical variables or Student’s t-test for continuous variables. The variables with values of p < 0.05 on univariate analysis were included in the multivariate analysis using multiple logistic regression models. Values of p < 0.05 were considered statistically significant. Calculations were performed using the Statistical Package for the Social Sciences (SPSS) version 21.0 for Windows (IBM Corp., Armonk, NY, USA).
Ethical standard
Written informed consent, including procedure and complications was obtained from all patients before ESD.. The study including the use of patient data was approved by the ethics committee of the Institutional Review Board.
Results
Figure 1 shows a summary of the final events of PEB. Definite PEB after ESD occurred in 77 lesions (4.1%). Among them, early PEB or late PEB occurred in 55 (2.9%) and 31 patients (1.6%), respectively. In 9 cases (0.4%), early and late PEB occurred in the same lesion. All cases of PEB were successfully treated by endoscopic hemostasis.
The patients’ clinicopathologic characteristics are summarized in Table 1. The mean patient age was 68.3 ± 9.3 years. The mean lesion and resection sizes were 12.6 ± 8.1 mm and 30.2 ± 9.3 mm, respectively. The mean procedure time was 24.9 ± 17.4 min. The most common lesion location was the lower third of the stomach (65.2%). The en-bloc and complete resection rates were 98.4% and 95.4%, respectively. Among the resected lesions, 64.5% were adenoma and 35.5% were adenocarcinoma. Low-dose aspirin, clopidogrel, and warfarin medications were found in 11.4%, 3.8%, and 0.4% of lesions, respectively.
Risk factor analyses associated with early PEB are shown in Tables 2 and 3. On univariate analysis, age ≤65 years, lesion size ≥20 mm, resection size ≥30 mm, procedure time ≥20 min, location in lower third of the stomach, erosion, and clopidogrel use were significant. On multivariate analysis, age ≤65 years (odds ratio [OR], 3.375; 95% confidence interval [CI], 1.919–5.935; p < 0.001), resection size ≥30 mm (OR, 2.027; 95% CI, 1.021–4.026; p = 0.044), procedure time ≥20 min (OR, 2.453; 95% CI, 1.185–5.078; p = 0.016), lower third of the stomach (OR, 2.845; 95% CI, 1.381–5.860; p = 0.005), erosion (OR, 1.870; 95% CI, 1.056–3.313; p = 0.032), and clopidogrel use (OR, 4.041; 95% CI, 1.587–10.286; p = 0.003) were significant. The symptoms at the time of PEB diagnosis are shown in Fig. 4A. Common symptoms for early PEB were asymptomatic (n = 25), followed by hematemesis (n = 15) and melena (n = 12). Asymptomatic patients were diagnosed during routine second-look endoscopy.
Tables 4 and 5 show the risk factor analysis associated with late PEB. A total of 31 events (1.6%) occurred. On univariate analysis, age ≤65 years, procedure time ≥20 min, mid to upper third of the stomach, undifferentiated carcinoma, erosion, submucosal invasion, high risk of stigma during second-look endoscopy, history of early delayed bleeding, and the use of aspirin, clopidogrel, and warfarin were significant. After multivariate analysis, mid to upper third of the stomach (OR, 4.664; 95% CI, 1.990–10.929; p < 0.001), undifferentiated carcinoma (OR, 4.878; 95% CI, 1.112–21.394; p = 0.036), erosion (OR, 2.819; 95% CI, 1.259–6.310; p = 0.012), high risk of stigma during second-look endoscopy (OR, 4.215; 95% CI, 1.272–13.971, p = 0.019), history of early PEB (OR, 3.899; 95% CI, 1.009–15.064; p = 0.048), and clopidogrel use (OR, 4.257; 95% CI, 1.364–13.288; p = 0.013) were significant. The symptoms at the time of late PEB diagnosis are shown in Fig. 4B. Common symptoms were hematemesis (n = 17) and melena (n = 10).
According the number of risk factors, the incidence rate of PEB is shown in Fig. 5. The incidence of early PEB was less than 1% if the number risk factor was ≤1. The incidence of late PEB was than 1% if risk factors were absent.
Incidence of post-ESD bleeding according to the number of risk factors. A. early post-ESD bleeding, the risk factors of early post-ESD bleeding include age ≤65 years, resection size ≥30 mm, procedure time ≥20 min, lower third of stomach, erosion, and clopidogrel use. B. late-post ESD bleeding, the risk factors of late post-ESD bleeding include the mid to upper third of the stomach, undifferentiated carcinoma, erosion, high risk of stigma during second-look endoscopy, history of early post-ESD bleeding, and clopidogrel use. ESD; endoscopic submucosal dissection.
Discussion
The present study results show a PEB rate of 4.1%. The reported incidence of ESD-related bleeding varies. The reported intra-procedural and PEB rates were 11.9–45.1% and 5.1%, respectively3,14,15. Bleeding is inevitable during mucosal incision and submucosal dissection using an electrosurgical knife. Intra-procedural bleeding, manageable by an endoscopic maneuver, should not be considered a complication. A delayed diagnosis of PEB in artificial ulcers after ESD may be accompanied by cardiovascular compromise due to late symptom onset. Among cases of PEB, 33–74% reportedly occur within 24 hours after ESD4,5,6. In the present study, early PEB occurred in 55 patients. In addition, 25 patients were asymptomatic before active bleeding was noted on routine second-look endoscopy. In cases of acute gastrointestinal bleeding, hemoglobin levels do not fall immediately because of a proportionate reduction in plasma and red blood cell volumes. Therefore, hemoglobin levels may be normal or only minimally decreased at the initial presentation of severe artificial ulcer bleeding. Diagnosing or detecting PEB before the onset of cardiovascular compromise is important, especially for older patients and those at risk of cardiovascular morbidity. Recent prospective studies on the efficacy of the routine use of second-look endoscopy showed no advantage for the prevention of PEB6,7,8,9. However, those studies had several limitations such as differing definitions of PEB, the exclusion of patients who took antiplatelet/antithrombotic medications, and small sample sizes. Therefore, patients at high risk of PEB might have been excluded from those studies. In the present study, we included patients who took antiplatelet/antithrombotic medications (low-dose aspirin, clopidogrel, and warfarin) and analyzed the risk factors associated with early and late PEB.
In the present study, the analysis of risk factors associated with PEB was performed according to early or late onset. Early PEB was associated with age ≤65 years, resection size ≥30 mm, procedure time ≥20 min, location in the lower third of the stomach, erosion, and clopidogrel use. The reason why younger patients are at higher risk of PEB is unclear. Mucosal and submucosal vascular prominence may differ among age groups. For older patients, the vascular plexus may decrease proportionate to age and atrophic mucosal changes14. In South Korea, both endoscopic and histological atrophy increased proportionate to age16. Longer procedure time and larger resection size may be associated with a more difficult ESD procedure. A difficult ESD procedure may be associated with lesion location, lesion size, anatomical factors, surgical experience, or poor patient cooperation. Damage to vessels beneath the submucosa or proper muscle may occur more frequently during a difficult ESD procedure. Surface erosion of the gastric epithelial tumors is associated with endoscopic findings of higher-grade dysplasia or EGC17. Surface erosion may be associated with active inflammation or previous repeated endoscopic forceps biopsy. An active inflammatory lesion may be associated with the existence of more vessels in the submucosal layer5.
The PEB tendency differed according to lesion location. In the lower third of the stomach, early PEB occurred more frequently. However, late PEB was more frequently associated with the mid to upper third of the stomach. At the earlier time after ESD, antral contractility and bile or digestive enzyme reflux from the duodenum might be associated with bleeding events. A previous study reported that the preventive coagulation of visible vessels at the artificial ulcer bed just after tumor excision was important in preventing PEB18. Intraoperative bleeding occurs less frequently in the antrum than in the mid to upper part of the stomach. Therefore, preventive coagulation might be insufficient during and just after ESD. The submucosal arteries in the mid to upper part of the stomach are more stubby and thicker than those in the antrum18. During the ESD procedure, intraoperative bleeding occurs more frequently than in the antrum because of submucosal artery damage. The gastric wall and submucosa thickness differ between anatomical locations. The body wall and submucosa are thinner than the antrum19. Endoscopic handling is more difficult in the mid to upper third of the stomach than in the antrum. Preventive coagulation at the ulcer bed for exposed or bleeding vessels might be insufficient during the ESD procedure. Undifferentiated carcinoma was a risk factor for late PEB. Undifferentiated carcinoma occurs more frequently in the mid to upper part of the stomach than in the antrum20.
In the present study, clopidogrel use was an important risk factor for early and late PEB. We asked our patients to stop taking clopidogrel 7 days before ESD and to restart it 1–2 days after ESD. Clopidogrel is a potent antiplatelet inhibitor that decreases ulcer-induced gastric epithelial cell proliferation and inhibits angiogenesis in gastric ulcer healing21,22. Thus, clopidogrel might inhibit the healing process of artificial ulcers and increase the patient’s risk of PEB.
In the present study, routine second-look endoscopy was performed in all patients the day after ESD. We subjected the artificial ulcer bed to Forrest classification, which is used for risk classification of peptic ulcer re-bleeding. For patients at high risk of stigma ulcer, additive preventive endoscopic hemostasis was performed. The high risk of stigma and early PEB lesions were risk factors for late PEB despite additive hemostasis. Previous studies have reported that patients who underwent second-look endoscopy showed higher bleeding rates than patients in non-second look endoscopic groups6,7. Another study reported that routine prophylactic hemostasis during second-look endoscopy may be ineffective for preventing PEB23. The reason for this is unclear. However, incomplete hemostasis for the exposed vessel or active bleeding spots might be one possible reason. In addition, additive coagulation for patients at low risk of bleeding ulcer (such as oozing bleeding or pigmentation) may aggravate tissue and vessel damage beneath the submucosa.
In the present study, the incidence rate of PEB according to the number of risk factors was calculated. The results of present study highlighted that patients with early PEB with ≥2 risk factors had a PEB rate of more than 1.2% within 24 hours of ESD. The incidence rate increased in line with increasing risk factor numbers. Therefore, these patients may be candidates for second-look endoscopy. Patients with late PEB with ≥1 risk factor, the risk of late PEB was more than 1.1% and the increasing incidence of bleeding was associated with increasing risk factor numbers. These patients should be recommended for careful monitoring after discharge.
The present study has several limitations. First, selection bias may be present because of a retrospective analysis of medical chart review. Therefore, we cannot generalize the present study results. Second, in the present study, we could only evaluate low-dose aspirin, clopidogrel, and warfarin from the retrospective medical chart review. Direct-acting anticoagulants (DOAC) could not be confirmed in this study. Several other antiplatelet medications, antithrombotic medications, and other unchecked medications might be associated with bleeding events. Third, although 7 dialysis patients and 8 atrial fibrillation patients were included, the patients’ comorbid diseases associated with bleeding tendency could not be evaluated from the retrospective chart review. Fourth, the effect of second-look endoscopy could not be evaluated because all patients underwent second-look endoscopy.
In summary, age ≤65, resection size ≥30 mm, procedure time ≥20 min, location in the lower third of the stomach, erosion, and clopidogrel use were associated with early PEB. Routine second-look endoscopy for all patients might not be beneficial. However, the incidence of early PEB is increased according the number of risk factors. Therefore, patients with ≥2 risk factors may be considered for second-look endoscopy. Location in the mid to upper third of the stomach, undifferentiated carcinoma, erosion, clopidogrel use, high risk of stigma, and history of early PEB were associated with late PEB. After patients with these risk factors are discharged, careful monitoring should be considered.
References
Japanese Gastric Cancer, A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20, 1–19 (2017).
Lian, J., Chen, S., Zhang, Y. & Qiu, F. A meta-analysis of endoscopic submucosal dissection and EMR for early gastric cancer. Gastrointest Endosc 76, 763–770 (2012).
Libanio, D., Costa, M. N., Pimentel-Nunes, P. & Dinis-Ribeiro, M. Risk factors for bleeding after gastric endoscopic submucosal dissection: a systematic review and meta-analysis. Gastrointest Endosc 84, 572–586 (2016).
Goto, O. et al. A multicenter survey of the management after gastric endoscopic submucosal dissection related to postoperative bleeding. Dig Dis Sci 57, 435–439 (2012).
Choi, C. W. et al. Clinical outcomes of second-look endoscopy after gastric endoscopic submucosal dissection: predictive factors with high risks of bleeding. Surg Endosc 28, 2213–2220 (2014).
Mochizuki, S. et al. Scheduled second-look endoscopy is not recommended after endoscopic submucosal dissection for gastric neoplasms (the SAFE trial): a multicentre prospective randomised controlled non-inferiority trial. Gut 64, 397–405 (2015).
Ryu, H. Y. et al. Second-look endoscopy is not associated with better clinical outcomes after gastric endoscopic submucosal dissection: a prospective, randomized, clinical trial analyzed on an as-treated basis. Gastrointest Endosc 78, 285–294 (2013).
Kim, J. S. et al. The need for second-look endoscopy to prevent delayed bleeding after endoscopic submucosal dissection for gastric neoplasms: a prospective randomized trial. Gut Liver 8, 480–486 (2014).
Jee, S. R. et al. Clinical impact of second-look endoscopy after endoscopic submucosal dissection of gastric neoplasm: a multicenter prospective randomized-controlled trial. Eur J Gastroenterol Hepatol 28, 546–552 (2016).
Gralnek, I. M. et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47, a1–46 (2015).
Japanese Gastric Cancer, A. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14, 101–112 (2011).
Mihara, M. et al. The role of endoscopic findings for the diagnosis of Helicobacter pylori infection: evaluation in a country with high prevalence of atrophic gastritis. Helicobacter 4, 40–48 (1999).
Chan, F. K. L. et al. Management of patients on antithrombotic agents undergoing emergency and elective endoscopy: joint Asian Pacific Association of Gastroenterology (APAGE) and Asian Pacific Society for Digestive Endoscopy (APSDE) practice guidelines. Gut 67, 405–417 (2018).
Jeon, S. W. et al. Predictors of immediate bleeding during endoscopic submucosal dissection in gastric lesions. Surg Endosc 23, 1974–1979 (2009).
Park, S. E. et al. Risk factors and correlations of immediate, early delayed, and late delayed bleeding associated with endoscopic resection for gastric neoplasms. Surg Endosc 30, 625–632 (2016).
Eshmuratov, A. et al. The correlation of endoscopic and histological diagnosis of gastric atrophy. Dig Dis Sci 55, 1364–1375 (2010).
Choi, C. W. et al. Endoscopic submucosal dissection as a treatment for gastric adenomatous polyps: predictive factors for early gastric cancer. Scand J Gastroenterol 47, 1218–1225 (2012).
Takizawa, K. et al. Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection–an analysis of risk factors. Endoscopy 40, 179–183 (2008).
Park, S. et al. Stretching Causes Extensive Changes of Gastric Submucosa: Is It Acceptable to Define 500 microm as the Safe Margin? Gut Liver 2, 199–204 (2008).
Lauren, P. The Two Histological Main Types of Gastric Carcinoma: Diffuse and So-Called Intestinal-Type Carcinoma. An Attempt at a Histo-Clinical Classification. Acta Pathol Microbiol Scand 64, 31–49 (1965).
Luo, J. C. et al. Clopidogrel delays gastric ulcer healing in rats. Eur J Pharmacol 695, 112–119 (2012).
Luo, J. C. et al. Clopidogrel inhibits angiogenesis of gastric ulcer healing via downregulation of vascular endothelial growth factor receptor 2. J Formos Med Assoc 115, 764–772 (2016).
Kim, D. S. et al. Usefulness of the Forrest Classification to Predict Artificial Ulcer Rebleeding during Second-Look Endoscopy after Endoscopic Submucosal Dissection. Clin Endosc 49, 273–281 (2016).
Acknowledgements
Hyeong Seok Nam and Cheol Woong Choi share first authorship.
Author information
Authors and Affiliations
Contributions
H.S. Nam and C.W. Choi wrote the main manuscript text. S.J. Kim, H.W. Kim, D.H. Kang, S.B. Park and D.G. Ryu collected the data. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nam, H.S., Choi, C.W., Kim, S.J. et al. Risk factors for delayed bleeding by onset time after endoscopic submucosal dissection for gastric neoplasm. Sci Rep 9, 2674 (2019). https://doi.org/10.1038/s41598-019-39381-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39381-1
This article is cited by
-
Usefulness of the combined orthodontic rubber band and clip method for gastric endoscopic submucosal dissection
BMC Gastroenterology (2022)
-
External validation of the BEST-J score and a new risk prediction model for ESD delayed bleeding in patients with early gastric cancer
BMC Gastroenterology (2022)
-
Carbazochrome sodium sulfonate is not effective for prevention of post-gastric endoscopic submucosal dissection bleeding: A retrospective study
Surgical Endoscopy (2022)
-
Validation of the BEST-J score, a prediction model for bleeding after endoscopic submucosal dissection for early gastric cancer: a multicenter retrospective observational study
Surgical Endoscopy (2022)
-
Influence of hospital volume on bleeding after endoscopic submucosal dissection for early gastric cancer in Japan: a multicenter propensity score-matched analysis
Surgical Endoscopy (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.