Abstract
Although many studies have reported that allergic rhinitis is an independent risk factor highly related to otitis media in children, there is still lack of epidemiological studies on demographics. The objective of this study was to identify if allergic rhinitis was an independent risk factor for otitis media in children aged between 7 and 12 years by using the nationwide survey data representing the local population of South Korea. This is a secondary study based on the ENT examination data (eg. acute otitis media, otitis media with effusion, chronic otitis media). The subjects of this study were 472 children (248 male and 224 female) who completed the Korea National Health and Nutrition Examination Survey 2015. The presence of otitis media was examined by otolaryngologists using tympanometric measurements, audiometric measurements, and otoscopic examination. Allergic rhinitis was diagnosed by Korean-version of International Study of Asthma and Allergies in Childhood, a total serum immunoglobulin E test, an allergen-specific immunoglobulin E test, a blood eosinophil test, an eosinophil cationic protein test, a nasal cytology for eosinophils test, a skin reaction test, and an antigen simultaneous test. Confounding factors included age, gender, the levels of income for households, and household composition. The relationship between allergic rhinitis and otitis media was analyzed by a complex sample logistic regression analysis and the odds ratio and 95% confidence interval were presented. The results of a complex sample design logistic regression revealed that allergic rhinitis in children was significantly associated with otitis media (p < 0.05). Even after adjusting all confounding factors, children with allergic rhinitis had twice significantly higher risk of otitis (OR = 2.04; 95% CI: 1.30–3.18) than children without allergic rhinitis. This epidemiologic study confirmed the independent relationship between pediatric allergic rhinitis and otitis media. In the future, longitudinal study will be needed to verify causality of allergic rhinitis and otitis media.
Similar content being viewed by others
Introduction
Otitis media is an inflammation of the ear that is caused by bacterial infiltration into the tympanic cavity. It is a very common ear illness to young children. Otitis media is low in prevalence in newborns but is most prevalent around the age of 21 and it is Estimated that death rate related to otitis media is especially high under the age of 52. Thus, epidemiological studies on the prevalence of otitis media have mainly reported the results of tests on infants and young children under the age of 23 and there are only a few epidemiological studies which reported the prevalence of school-age children4. Previous epidemiological studies reported that the prevalence of otitis media in children under 14 years old ranged between 3.7 and 8.7%5,6,7,8,9,10. It was revealed that the prevalence of otitis media in developing countries is higher than in developed countries8.
Otitis media is likely to become a chronic disease if it is not proper treatment is in childhood due to frequent recurrences. A previous study reported that five out of 100 young children suffered from recurrent otitis media11. In the United States, the recurrence rate of otitis media in preschool children is steadily increasing12. Otitis media is a major reason for the doctor’s visit in South Korean children as well. As of 2008, otitis media is the sixth most common cause of the doctor’s visit for patients under 10 years old13. Since the childhood health is known to have important effects on the health of adolescents and adulthood, it is required to pay attention to otitis media of children to maintain healthy hearing throughout life.
Although otitis media is not a life-threatening illness, chronic otitis media can adversely affect language development, such as speaking and listening, which can decrease learning performance12,14. In severe cases, it can lead to complications such as hearing loss and degrade the quality of life12,14. Therefore, identifying the risk factors of otitis media and managing them in the early stage are important from the prophylactic point of view.
Previous studies indicated that age, gender, race, genetic factors, low socioeconomic status, breastfeeding, allergic diseases, and chronic sinusitis were associated with otitis media6,7,15,16. Several studies of them reported that allergic rhinitis was a risk factor affecting the occurrence of otitis media17. Kim et al.18 in their case-control study revealed that allergic rhinitis and day nursery were independent risk factors highly associated with young children’s otitis media. Risk factors can be divided into factors that cannot be changed such as genetic factors and family history and factors that can be changed such as environment and lifestyle. The risk and recurrence of otitis media can be reduced by identifying and managing these changeable factors.
Although allergic rhinitis has been reported as an independent risk factor of otitis media, the most of the previous studies targeted only subjects visiting a specific medical facility or were conducted as case-control studies based on a small sample size. Consequently, it is limited to generalize the obtained results to the population of the local community18,19,20. Moreover, studies evaluated the illness of young children under 5 years old identified the history of otitis media using a parental questionnaire12. Consequently, these results pose a possibility to suffer from the bias due to the limited remembrance12. Furthermore, there are only few studies that were adjusted for considering the environmental factors such as the household economy level and day nursery care in addition to the sociodemographic factors. Although environmental, racial, and sociocultural differences are highly associated with the risk factors of otitis media, few epidemiological studies have investigated the risk factors of otitis media in young South Korean children. More epidemiological studies are needed to develop an evidence-based otitis media guideline because the risk factors for an illness can vary by culture and race.
Therefore, it is necessary to conduct an epidemiological study targeting a population in order to identify the risk factors of young children’s otitis media in South Korea. The objective of this study was to identify if allergic rhinitis was an independent risk factor for otitis media in children aged between 7 and 12 years by using the nationwide survey data representing the local population of South Korea.
Methods
Data Source and Participants
The source of this study is Korea National Health and Nutrition Examination Survey (KNHNES) conducted by Korea Centers for Disease Control and Prevention in 2015 with the support of the Ministry of Health and Welfare for the purpose of calculating representative and reliable statistics for the health level and health behavior of South Koreans. KNHANES was approved by the Institutional Review Board of the Korean Center for Disease Control and Prevention (2013-12EXP-03-5C) and carried out compliant with the ethical standards of the Declaration of Helsinki. Source data were provided to the researchers by data management personnel of Korea Center for Disease Control in pseudonymized condition with yet other virtual IDs attached after personal information being deleted. The survey procedures were designed to protect participant privacy by allowing anonymous and voluntary participation. Participants were given identification numbers and guaranteed anonymity. After the survey had been fully explained and all participants had provided written informed consent (both directly and from their parents or legal guardians), participants completed a survey. Authors reported the objective of the study to Korea Centers for Disease Control and Prevention and obtained an official permit to analyze the raw data. KNHANES is based on a rolling sampling design that employs a complex, stratified multistage probability cluster survey of a representative sample of the non-institutionalized population in South Korea (please refer6 for further detail of the sampling methods of the KNHANES). Briefly, KNHANES in 2015 was carried out for 9,773 subjects from 3,840 households and the response rate was 78.3% (n = 7,649).
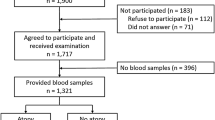
The subjects of this study were 503 children who completed the health survey and otological examination. Among these subjects, 31 children did not respond to the survey on Allergic rhinitis so they were excluded from the study. Consequently, 472 children (248 male and 224 female) were used for further analyses. The flow chart is shown in Fig. 1.
Measurement
Health interview
Trained medical staffs conducted the otological examination at a mobile examination center and the health interview at participants’ homes. For the health interview, the information regarding the highest level of education and economic activities was obtained from face-to-face interviews and the survey on behaviors associated personal health was carried out by using self-administered questionnaires.
Otitis media and allergic rhinitis
The otolaryngological examinations were conducted by following the technical advice provided by The Korean Otologic Society and highly trained 40 otolaryngologists10. Otitis media was diagnosed by the following procedure. As a first step, the swelling, blister formation, redness, perforated eardrum associated with otorrhea, the presence of middle ear effusion, and the color changes in eardrum were checked through direct observation using otoscopy. Afterward, type B or type C middle ear effusion was checked using the tympanometry test. Patients with Down syndrome, palatal facial deformities such as cleft palate, immune disorders, and cochlear implants were excluded from the test. Allergic rhinitis was diagnosed by conducting a total serum immunoglobulin E test, an allergen-specific immunoglobulin E test, a blood eosinophil test, an eosinophil cationic protein test, a nasal cytology for eosinophils test, a skin reaction test, and an antigen simultaneous test. This is a secondary study based on the ENT examination data. Individual diagnostic data (primary data) researched by ENT doctors were provided after being converted into binary data (e.g. otitis media – yes, no) in KNHNES.
Confounding factors
Age, gender, the levels of income for households, and household composition were examined. The levels of income for households were classified into four quartiles. Household composition was classified into two generations households composed of married couples and children, two generations households composed of single parents and children, and three generations households.
Statistical Analysis
The weighted values of KNHANES were calculated so that the subjects of the survey can represent overall Korean population. Detailed explanations on the weighted values are shown in reference10.
The general characteristics of the subjects and the prevalence of otitis media were presented as weighted percentages. Differences in the groups by the prevalence of allergic diseases were confirmed by Rao-Scott Chi-square test. The relationship between allergic rhinitis and otitis media was analyzed by a complex sample logistic regression analysis and the odds ratio and 95% confidence interval were presented. Gender and age were adjusted in the first level of the study model and all confounding factors including household economic level and household composition were adjusted in the second level additionally. IBM SPSS version 24.0 (IBM Inc., Chicago, Illinois) was used for analyses and significance level was 0.05 unless stated otherwise.
Results
The general characteristics of the study subjects
The general characteristics of the study subjects are presented in Table 1. The mean age was 9.6 years (standard error = 0.4) and there were more male subjects (50.5%) than female subjects (49.5%). The fourth quartile household economy level was the most common (33.4%) and the two generations households, which were composed of married couples and children, were dominant (75.3%). The prevalence of allergic rhinitis was 26.5% and the prevalence of otitis media was 26.6%.
The general characteristics of the subjects according to the prevalence of otitis media
The general characteristics of the subjects according to the prevalence of otitis media in young children are shown in Table 2. The results of Rao-Scott Chi-square test showed that the prevalence of otitis media was significantly (p < 0.05) higher in children with allergic rhinitis (37.2%) than in those without any allergic rhinitis (22.7%), which was an only significant variable.
The relationship between allergic rhinitis and otitis media
The relationship between allergic rhinitis and otitis media in young children is shown in Table 3. The results of a complex sample design logistic regression revealed that allergic rhinitis in children was significantly (p < 0.05) associated with otitis media. Even after adjusting all confounding factors (Model 2), children with allergic rhinitis had twice significantly (p < 0.05) higher risk of otitis (OR = 2.04; 95% CI: 1.30–3.18) than children without allergic rhinitis.
Discussion
This epidemiological study examined the relationship between allergic rhinitis and otitis media in children from 7 to 12 years old in South Korea. The results of this study showed that the prevalence of otitis media in children between 7 and 12 years old was 26.6%. Previous studies on the prevalence of otitis media in children were conducted in a small area. Although there was a small variation in the reported prevalence of otitis media in preschool children, previous studies reported high prevalence of otitis media in these children, which agreed with the results of this study: 16.4% for Daegu21, 15.8% for Bucheon22, and 14.5% for Gunsan23. Even though it is difficult to compare directly, the prevalence of this study was higher than the prevalence of otitis media with effusion (10.4%) in children between 6 and 11 years old (2,355 people) in Eastern Anatolia16, the prevalence of otitis media with effusion (8.7%) in 1,800 children registered primary schools in Istanbul24 and the prevalence of otitis media with effusion (10.5%) in 5-year-old preschool children in the UK25.
Particularly, Pyo et al.26 examined the prevalence rate of otitis media in South Korean kindergarten and elementary school students (n = 3,364) and they reported that the prevalence was higher during an in-between season (March; 18.5%) than during a season (6.5%). The results of Pyo et al.26 suggested that the prevalence of otitis media had a seasonal change and it could be affected by the prevalence of seasonal allergic rhinitis25. It will be necessary to conduct a nation-wide time series analysis in order to understand the relationship between the seasonal prevalence of otitis media and allergic rhinitis.
The results of this study showed that, even after adjusting confounding factors, children with allergic rhinitis had twice and significantly higher risk suffering from otitis media than those without allergic rhinitis. Many previous case-control studies consistently reported that allergic rhinitis was significantly associated with otitis media, concurring with the results of this study. For example, a case-control study conducted for children between 4 to 12 years old in Hong Kong indicated that children with allergic rhinitis had a 4.6-fold (OR = 4.64) higher risk of otitis media than children without rhinitis19. Similarly, a case-control study in children under 60 months revealed that allergic rhinitis had a 2.3-fold higher risk of otitis media (OR = 2.32) even after adjusting for confounding factors18. The authors could conclude that there was insufficient evidence that allergic rhinitis directly affected the etiology of otitis media but otitis media in young children could be deteriorated continuously due to respiratory allergies. Similar results were reported in a pediatric epidemiologic study in the United States. The study examined children aged less than 6 years (5,189 people in 1918 and 6,209 people in 1988) participating in the National Health Interview Surveys (NHIS) from 1981 to 1988 and analyzed the risk factors for otitis media to revealed that the increase in allergic rhinitis was significantly related with an increase in otitis media12.
It is known that otitis media may be caused by various factors such as dysfunction of the Eustachian tube, inflammation reaction, and atopy. A recent meta-analysis indicated that allergic rhinitis was identified as a significant risk factor for otitis media with effusion27. Nevertheless, the scientific mechanism to explain the causal relationship between allergic rhinitis and otitis media is still insufficient12. This epidemiological study presents three possible mechanisms to explain the relationship between allergic rhinitis and otitis media in young children.
The first possible mechanism to explain the relationship is “shock organ” hypothesis. The hypothesis speculates that allergic reactions cause mast cells in the mucosa and inflammatory cells in the nose and nasopharynx. They release cytokines and other inflammatory mediators resulting in the occlusion of Eustachian tubes to develop otitis media17,28.
The second hypothesis is the dysfunction of Eustachian tubes as a cause of otitis media. It means that the occlusion of Eustachian tubes disturbs the ventilation in the middle ear cavities to increase the absorption of nitrogen in the middle ear, produce continuous negative pressure, and result in the occurrence of otitis media17. The temporary dysfunction of Eustachian tubes is known to cause the aspiration into the middle ear cavity of nasopharyngeal secretions containing bacteria and viruses. This dysfunction of Eustachian tubes is known to be frequent in young children with allergic rhinitis29,30.
The third hypothesis is the degradation of the immune function. Children have relatively weaker immune functions than adults. Particularly, it is believed that young children with allergic rhinitis are at higher risk of allergic otitis because young children with allergic rhinitis experience the dysfunction of Eustachian tubes more frequently due to the inflammation of lymphoid tissues such as adenoids. Longitudinal studies are needed to understand causality of allergic rhinitis and otitis media in the future.
Since young children with allergic rhinitis are at high risk for otitis media, it is important to prevent the aggravation of allergic rhinitis by managing risks systematically in order to prevent complications (e.g., otitis media). Many countries have prepared an evidence-based guideline for otitis media. The 2004 evidence-based clinical practice guideline published by Agency for Healthcare Research and Quality (AHRQ) recommended doctors to reduce the risk factors of otitis media for children between 2 months and 12 years old in order to prevent the occurrence of otitis media31. Moreover, Ovetchkine and Cohen32 emphasized that the treating the nasal cavity by using antihistamines was helpful to treat otitis media when young children with otitis media accompanies with nasal diseases such as allergic rhinitis or sinusitis. In South Korea, The Korean Otologic Society developed the clinical practice guideline for infant and children with otitis media in 2009 for treating young children based on evidence. The society also published a revised version of The Practice Guideline for Pediatric Otitis Media in 2014 with supplementing the results of evidence-based studies33. The Practice Guideline for Pediatric Otitis Media emphasized the infection factors, genetic factors, socioeconomic factors, and environmental factors as risk factors for pediatric otitis media. However, it is still lacking information regarding related diseases such as allergic rhinitis that can aggravate otitis media. It is necessary to revise the guidelines for the prevention of otitis media, which contains additional evidence for the deterioration factors of otitis media in young children.
The importance of this study was that this study confirmed the relationship between allergic rhinitis and otitis media in young children by using representative epidemiological data of South Korea. The presented study has four main limitations. First, this study only identified the relationship between the prevalence of allergic rhinitis and otitis media. In the future, it is necessary to evaluate the dose-response relationship between the duration of allergic rhinitis and the degree of otitis media. Secondly, subtypes of otitis media were not investigated. It will be necessary to classify otitis media into subtypes (e.g., otitis media with effusion and suppurative otitis media) and identify the relationship between the subtype and allergic rhinitis. Thirdly, it is possible that there are more confounding factors of otitis media in addition to the confounding factors considered in the study. Future studies are required to control more potential confounding factors such as genetic factors, family history factors, and environmental sanitation factors (ex. secondhand smoke exposure, daycare attendance, urban vs rural setting). Fourthly, it is difficult to find a causal relationship in this study because it was a cross-sectional study. A longitudinal study will be needed to verify causality.
Conclusion
This population-based epidemiologic study confirmed the independent relationship between pediatric allergic rhinitis and otitis media. The results of this epidemiologic study ask young children, who are suffering from allergic rhinitis to take regular otologic tests such as eardrum test and hearing test and manage rhinitis for preventing otitis media because they are at high risk for complications of otitis media in the future.
References
Qureishi, A. et al. Update on otitis media–prevention and treatment. Infect Drug Resist 7, 15–24 (2014).
Monasta, L. et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS One 7, e36226 (2012).
Kaspar, A. et al. Prevalence of otitis media and risk-factors for sensorineural hearing loss among infants attending Child Welfare Clinics in the Solomon Islands. Int J Pediatr Otorhinolaryngol 111, 21–25 (2018).
Maharjan, M. et al. Prevalence of otitis media in school going children in Eastern Nepal. Kathmandu Univ Med J (KUMJ) 4, 479–482 (2006).
Tong, M. C. et al. Screening for otitis media with effusion to measure its prevalence in Chinese children in Hong Kong. Ear Nose Throat J 79, 626–629 (2000).
Martines, F. et al. Risk factors for otitis media with effusion: case-control study in Sicilian schoolchildren. Int J Pediatr Otorhinolaryngol 75, 754–759 (2011).
Caffarelli, C. et al. Atopy in children with otitis media with effusion. Clin Exp Allergy 28, 591–596 (1998).
DeAntonio, R. et al. Epidemiology of otitis media in children from developing countries: A systematic review. Int J Pediatr Otorhinolaryngol 85, 65–74 (2016).
Kim, C. S., Jung, H. W. & Yoo, K. Y. Prevalence of otitis media and allied diseases in Korea: results of a nation-wide survey. J Korean Med Sci 8, 34–40 (1993).
Ministry of Health and Welfare, Korea National Health and Nutrition Examination Survey. Seoul, Ministry of Health and Welfare. (2014).
Dowell, S. F. et al. Otitis media―principles of judicious use of antimicrobial agents. J Pediatr 101, 165–171 (1998).
Lanphear, B. P. et al. Increasing prevalence of recurrent otitis media among children in the United States. J Pediatr, 99, e1 (1997).
Song, J. S. & Jung, H. G. Annual Health Insurance Statistical Yearbook 2008. 2009. Seoul, National Health Insurance Corporation.
Bellussi, L. et al. Quality of life and psycho-social development in children with otitis media with effusion. Acta Otorhinolaryngol Ital 25, 359–364 (2005).
Roditi, R. E., Veling, M. & Shin, J. J. Age: An effect modifier of the association between allergic rhinitis and Otitis media with effusion. Laryngoscope 126, 1687–1692 (2016).
Kırıs, M. et al. Prevalence and risk factors of otitis media with effusion in school children in Eastern Anatolia. Int J Pediatr Otorhinolaryngol 76, 1030–1035 (2012).
Yeo, S. G. et al. The role of allergic rhinitis in the development of otitis media with effusion: effect on eustachian tube function. Am J Otolaryngol 28, 148–152 (2007).
Kim, E. J. et al. A study on risk factors of recurrent otitis media. Korean J Pediatr Infect Dis 17, 91–100 (2010).
Pau, B. C. & Ng, D. K. Prevalence of otitis media with effusion in children with allergic rhinitis, a cross sectional study. Int J Pediatr Otorhinolaryngol 84, 156–160 (2016).
Alles, R. et al. The prevalence of atopic disorders in children with chronic otitis media with effusion. Pediatr Allergy Immunol 12, 102–106 (2001).
Kim, J. & Son, Y. Prevalence of otitis media with effusion in kindergarten children in Taegu area. Korean J Otorhinolaryngol-Head Neck Surg 38, 1695–1703 (1995).
Chang, K. H. et al. A prevalence study of otitis media with effusion in kindergarten children in Puchun. Korean J Otolaryngol 40, 374–381 (1997).
Lee, H. J. et al. Prevalence of silent otitis media with effusion in preschool children in Kunsan city. Korean J Fam Med 18, 46–52 (1997).
Gultekin, E. et al. Prevalence and risk factors for persistent otitis media with effusion in primary school children in Istanbul, Turkey. Auris Nasus Larynx 37, 145–149 (2010).
Midgley, E. J. et al. The frequency of otitis media with effusion in British pre‐school children: a guide for treatment. Clin Otolaryngol Allied Sci 25, 485–491 (2000).
Pyo, S. Y. et al. The prevalence of otitis media with effusion among kindergarten and elementary school children in Song buk, Seoul, Korea and risk factors. Korean J Otorhinolaryngol-Head Neck Surg 43, 1158–1165 (2000).
Cheng, X. et al. Allergic rhinitis and allergy are risk factors for otitis media with effusion: A meta-analysis. Allergol Immunopathol (Madr) 45, 25–32 (2017).
Bernstein, J. M. Role of allergy in eustachian tube blockage and otitis media with effusion: a review. Otolaryngol Head Neck Surg 114, 562–568 (1996).
Lazo-Saenz, J. G. et al. Eustachian tube dysfunction in allergic rhinitis. Otolaryngol Head Neck Surg 32, 626–631 (2005).
Martines, F. & Bentivegna, D. Audiological investigation of otitis media in children with atopy. Curr Allergy Asthma Rep 11, 513–520 (2011).
American Academy of Pediatrics. Diagnosis and management of acute otitis media. J Pediatr 113, 1451–1465 (2004).
Ovetchkine, P. & Cohen, R. Shortened course of antibacterial therapy for acute otitis media. Paediatr Drugs 5, 133–140 (2003).
Korean Otological Society, The Practice Guideline for Pediatric Otitis Media in Children. Seoul, Korean Otological Society. (2014).
Author information
Authors and Affiliations
Contributions
H.B. conceived and designed the experiments and analyzed the low data and wrote the paper.
Corresponding author
Ethics declarations
Competing Interests
The author declares no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Byeon, H. The association between allergic rhinitis and otitis media: A national representative sample of in South Korean children. Sci Rep 9, 1610 (2019). https://doi.org/10.1038/s41598-018-38369-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38369-7
This article is cited by
-
Allergy and Otitis Media in Clinical Practice
Current Allergy and Asthma Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.