Abstract
People living in rural China are more frequently exposed to some specific risk factors which made stillbirth rate higher than urban areas. National Free Preconception Health Examination Project was launched to investigate these risk factors and collected a representative sample of 248501 participants from 31 provinces in China from 2010 to 2013. Parental risk factors were ascertained twice before and during pregnancy respectively by questionnaires. Stillbirth or live birth were recorded by trained physicians. In the analysis, nested case-control study was conducted, and propensity score matching method was used to adjust the confounding. Multi-level logistic regression was used to fit for multi-level sampling. The overall stillbirth rate was 0.35% in rural China, it was higher in North (0.42%) and West (0.64%) areas. Maternal exposure to pesticide (OR (95%CI 1.06, 3.39)), hypertension (OR = 1.58 (95%CI 1.07, 2.34)), lack of appetite for vegetables (OR = 1.99 (95%CI 1.00, 3.93)), stress (compared with no pressure, OR of a little pressure was 1.34(95% CI 1.02, 1.76)); paternal exposure to smoking (OR = 1.22 (95% CI 1.02, 1.46)), organic solvents (OR = 1.64 (95% CI 1.01, 2.69)) were found independent risk factors of stillbirth. Folacin intake 3 months before pregnancy (OR = 0.72 (95%) CI 0.59, 0.89), folacin intake 1-2 months before pregnancy (OR = 0.71 (95% CI 0.55, 0.92)), folacin intake after pregnancy (OR = 0.81 (95% CI 0.65, 1.02) for) were protect factors of stillbirth. Maternal pesticide exposure, lack of vegetables, stress, paternal smoking and exposure to organic solvents were risk factors of stillbirth. Folic acid intake was protective factor of stillbirth, no matter when the intake began.
Similar content being viewed by others
Introduction
Women and children’s health is a priority of public health in China now. The stillbirth rate in China has declined by 4–6% from 2000 to 2015, but the newborn survival has lagged behind maternal and under-five survival the rate, the stillbirth rate declined more slowly than other adverse maternal and infant outcomes1. To end preventable stillbirths, the Every Newborn Action Plan, a global multi-partner movement set a target for national stillbirth rates of 12 or fewer stillbirths per 1000 births in all countries by 2030 in 2014. Disparities within countries should also be addresses2,3. As an agricultural country, 43.9% of Chinese total population live in rural areas4. Compared with city women, women in rural China do face inequalities in health services and access to health education and promotion, and are generally more exposed to risk factors such as pesticide, unhealthy diet, and inadequate folate intake due to limited resources available, economical underdevelopment, and substandard education level5,6,7,8,9. Besides, the living and environmental condition are also worse in rural areas10.
Access to health services, parental health-related behaviors such as smoking, drinking, physical activities and folacin intake are established to be risk factors of many adverse pregnancy outcomes11,12,13,14,15. No national perspective investigation about the epidemic of these risk factors and their relationship with stillbirth in rural China was conducted before.
To get a better understanding of maternal and newborn health of rural China, and identify current risk factors so as to improve maternal and newborn health, the government launched the “National Free Preconception Health Examination Project” in rural China from January 2010. Our study was based on the data on couples enrolled during 2010–12, which is the first set of the project data16,17.
Study Design
Participants
A two-stage stratified cluster sampling method was used for the recruitment of participants aged 21∼49, planning to deliver a baby within 6 months from 220 counties of 31 provinces, 86% of the target population was covered18. For all 31 provinces, counties were selected in the same proportion based on the population size and numbers of counties in each province17. All eligible couples living in these selected counties have access to this project, and 86% of target population were covered18,19.
A standardized questionnaire about the general information before the pregnancy including parental basic characteristics, childbearing history, living habit, and other exposing status before and during pregnancy were collected at the time of enrollment to the project by the local health workers20. Then they were followed up by telephone interview every 2–3 months to determine the conception status. Women who became pregnant within 6 months were closely followed up, and another standardized family heath file about health exposures during the pregnancy and medical examination data was recorded. Pregnancy outcomes were collected according to hospital health record within 6 weeks after delivery or 2 weeks within other pregnancy outcome by doctors. For those participants of whom no relevant hospital health record can be found, telephone follow-up was conducted. All records are uploaded in a web-based electronic data collection system16,17,20.
By December 2012, 248501 families achieved the whole follow-up of this project, and their pregnancy outcomes were recorded by doctors. Pregnancy outcomes including birth defects and multiple gestations were excluded from the analysis considering the undiagnosed genetic conditions.
Definition and Assessment on variables
Stillbirth was defined as fetal death on or after 20 weeks of gestation in this study. Maternal BMI in adults was categorized into four groups: <18.5, 18.5–23.9; between 24.0–27.9, ≥28.0 kg/m21. Advanced maternal age was defined as first pregnancy on or after the age of 35. Past medical history of hypertension or systolic blood pressure >140 or diastolic blood pressure >90 were considered as high blood pressure. Parental education levels were classified into illiteracy, primary school, junior middle school, senior middle school, undergraduate, postgraduate and above according to the current education system. Parental occupation was classified into farmer, physical worker, service industry laborer, businessman, house worker, office clerk, and others.
We divided the participants geographically according to the Qinling-Huaihe line, and Heihe-Tengchong line. Qinling-Huaihe line bisects China into north and south regions, culture, climate, living habits are all different between north and south, which affect people’s health situation22. Heihe-Tengchong line divides China from Heihe in Heilongjiang province to Tengchong in Yunnan province into east and west. The east is more economically developed with higher civilization degree than west, and it takes up 96% of total Chinese population even though it only covers 36% areas of China. The economic imbalance between east and west resulted the huge differences in health resources23.
Environmental exposure as pesticide and new decoration were classified into two groups, no and yes, social pressure was classified to five levels, with 1 the lowest and 5 the highest. Folacin intake duration was classified into more than 3 months before pregnancy, 1–2 months before pregnancy, after pregnancy, and no. And whether they take folacin regularly was also asked.
Statistical analysis
To control multiple confounding between the cases and controls and address severe imbalance between numbers of case and control which may cause high misclassification of interested outcome by logistic regression24, nested case-control study was conducted, and propensity score matching method was used to find 8 controls for each case. Logistic regression was used to calculate the propensity score, confounding factors as area22,23, breeding history25,26, education level27,28, occupation29, age group30 were adjusted in this procedure. Parental age, education level, occupation were closed related and can’t be put into the logistic regression together, we select maternal age, education level27,28, and paternal occupation as the dependent variables, as they were commonly used in the scoring of family social economic status, and were reported to be more closed related with the family utilization of health resources and family health status31. Wald χ2 was used for the model’s overall significance test, Hosmer-Lemeshow was used for the goodness test. After propensity score matching, cases and selected controls were used for further risk factors analysis.
T-test and McNemar test were conducted respectively for continuous data and categorical data in the univariate analysis. Due to differences in climate, culture and economics between different provinces, the subjects may share some homogeneity within a province and heterogeneity between provinces, individually independence required by traditional logistic regression was not matched. As a result, multi-level logistic regression was used to compare the exposures between case and control group. Province was set as the first level and individuals as the second level. Due to collinearity between some exposures between parents, models were built separately for maternal exposures and paternal exposures. Risk factors which were statistically significant in univariate analysis or were proven to be confounders in previous studies were included in the models. GLM procedure in SAS was used to build the model, parameters as Tolerance (TOL) and Variance Inflation Factor (VIF) were used to detect the collinearity between variables32. Intra-Class Correlation Coefficient (ICC) was used to test the independence and heterogeneity within level.
All data were expressed as mean ± SD or count (percentages), as appropriate. All statistical procedures were analyzed by SAS 9.4.
Results
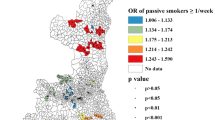
The overall stillbirth rate was 0.35% in rural China, it was higher in north (0.42%) and west (0.64%) than in South (0.32%) and east (0.34%).
Before the propensity score matching, parental education level, occupation, age group, height, weight, were all significantly different between stillbirth group and live birth group (Table 1). Maternal illiteracy group had a stillbirth rate of 0.60%, while mothers with education level equal or higher than postgraduate had a stillbirth rate of 0.64%, both significantly higher than the average rate. Parental advanced age group also had higher stillbirth rate, 0.54% for paternal advanced age and 0.77% for maternal advanced age. Beside, stillbirth group had average lower parental height.
By propensity score matching, 8 controls were found for each case. Breeding history, living region, maternal education level, maternal age, paternal occupation were taken into consideration in the matching process. The logistic regression used to calculate the propensity score was statistically significant, withχ2Wald = 127.04, P < 0.0001, and the Hosmer-Lemeshow test showed that the goodness of fit of the model is good, withχ2HL = 3.56, P = 0.8946. After the propensity score matching, basic characteristics were all equally distributed between the two groups (Table 2). Following analysis were conducted with the two groups of 811 cases and 6488 controls.
As to parental health behaviors before pregnancy, Mc-Nemar test result showed that maternal passive smoking (P = 0.0443, OR = 1.56 (95%CI 1.01, 2.41)), lack of vegetables (P = 0.0165, OR = 2.25 (95%CI 1.16, 4.39)), exposed to pesticide before pregnancy (P = 0.0047, OR = 2.24 (1.26, 3.97)), hypertension (P = 0.006, OR = 1.73 (95%CI 1.17, 2.56)) were related with stillbirth. Paternal smoking (P = 0.0025, OR = 1.28 (95%CI 1.09, 1.50)), and paternal exposed to new decoration before pregnancy (P = 0.0287, OR = 1.71 (1.05, 2.77)) were related with stillbirth. While maternal smoking (P = 0.3042, OR = 1.65(95% CI 0.63, 4.31)), paternal lack of vegetables (P = 0.4584, OR = 0.36 (95%CI 0.60, 3.08)), paternal passive smoking (P = 0.0978, OR = 1.36 (95%CI 0.95, 1.96)) were not found statistically significantly related with stillbirth in our study (Table 3).
Parental exposed to working or life stress was associated with stillbirth, but the relationship was not linear. Economic stress and got ready for pregnancy were not statistically significant related with stillbirth (Table 3).
We found that folacin intake was a protective factor of stillbirth in our study (P = 0.0016), the OR was similar for those who take folacin at least 3 months before pregnancy (OR = 0.70 (95%CI 0.58, 0.85)) or 1–2 months before pregnancy (OR = 0.71 (95%CI 0.56, 0.90)*), and slightly higher in those who take folacin after getting pregnant (OR = 0.78 (95%CI 0.63, 0.96)). And as long as the mothers take folacin, it’s not significantly different between those who take regularly and who not (P = 0.2213) (Table 3).
To illustrate the relationship between vegetables consumption and stillbirth, we stratified the data by folacin intake. For both who take folacin and who don’t, lack of vegetables seemed to be a risk factor, with OR of 3.60(95% CI 1.04, 12.38) and 2.04(95% CI 0.94, 4.43) respectively (Table 4).
Multi-level logistic model of risk factors of maternal and paternal were analyzed independently. TOL of variables in both models were all greater than 0.1, and VIF were all less than 10, so that we assume no collinearity among variables in the two models respectively. Overall tests of the two models were statistically significant, with both P < 0.001. Tests of Random parameter was also significant, with P = 0.03045 < 0.05, which mean that multi-level models should be used.
Multi-level logistic regression showed that maternal exposure to pesticide (OR (95%CI 1.06, 3.39)), maternal hypertension (OR = 1.58 (95%CI 1.07, 2.34)), lack or loss of appetite for vegetables (OR = 1.99 (95%CI 1.00, 3.93)), maternal pressure (compared with no pressure, OR of a little pressure was 1.34 (95% CI 1.02, 1.76)), paternal smoking (OR = 1.22 (95% CI 1.02, 1.46)), paternal exposing to Organic solvents (OR = 1.64 (95% CI 1.01, 2.69)) were independent risk factors of stillbirth. Folacin intake 3 months before pregnancy (OR = 0.72 (95% CI 0.59, 0.89)), folacin intake 1-2 months before pregnancy (OR = 0.71 (95% CI 0.55, 0.92)), folacin intake after pregnancy (OR = 0.81 (95% CI 0.65, 1.02) for) were protect factors of stillbirth compared with no folacin intake (Table 5).
Discussion
We found that stillbirth rate was much higher in the west, almost twice of the average rate. Due to low economic development level and sparse population, the maternal and child healthcare services provided in western areas were not as good as east. Some researches showed that the management rate, physical examination rate at early pregnancy, the visiting rate after delivery were all lower in western areas33. How to implement effective maternal and child health management for western areas are of vital important now.
Maternal exposure to pesticide was identified as an independent risk factor of stillbirth, which is consistent with previous studies34,35,36. Pesticide exposure are more common with farmers with lower education level. Due to limited health literacy, they know little about the harm of pesticide and protection methods. To protect people from the harm of pesticide, regular health education on how to apply pesticide safely should be provided, and specialized teams should be organized to help with the pesticide spraying37,38.
Maternal high blood pressure before pregnancy was also associated with stillbirth. According to previous studies, 4–7% of stillbirth happened due to high blood pressure during pregnancy, and high blood pressure before pregnancy which was not ideally control was an important cause of high blood pressure during pregnancy39,40,41,42. Reinforce the management of maternal blood pressure, and provide adequate treatment for those with high blood pressure before pregnancy are very important to reduce the stillbirth rate.
Folacin intake was proved to be protective factor of stillbirth, regardless of when the woman started the intake. And for those who rarely or don’t eat vegetables, the protective effect was larger. Previous studies showed that the rate of folacin intake among women in rural China is rising these years, which is a good phenomenon. It is important for basic public health services departments to increase the rate of folacin intake in a standardized way18.
Stress in daily life or work is also a risk factor of stillbirth, which may be a bigger problem for women in business. But it is worthwhile to notice that the stillbirth rate showed no statistically significance between those who got ready for this baby and those who not.
For paternal risk factors, paternal smoking, paternal drinking, and paternal exposed to new house decoration were all associated with stillbirth after adjustment of paternal age. In rural China, male smoking and drinking are still severe public health problems that need to be addressed43,44. New decorated house may be associated with higher dosage level of formaldehyde or organic solvent, which were reported to be risk factors of stillbirth45.
Limitations of our studies include that many of risk factors collected by our study were binary data, which made the analysis of dose-response relationship impossible, the exposing status such as smoking, drinking or pesticide were self-reported, which may not be very accurate. Also, the participants were not randomly selected, which may also cause some bias of our study.
Ethical approval
The study was approved by the institutional research review board at the National Health and Family Planning Commission and National Research Institute for Family Planning. Informed consents were obtained from all participants or their legal representatives. All research was performed in accordance with relevant guidelines.
Data Availability
The data generated cannot be made publicly available according to the Chinese law of personal data protection and also our project data management rules. However, data inquires or further suggestions for analyses can be made to the corresponding author.
References
Chen, D., Cui, S., Liu, C., Qi, H. & Zhong, N. Stillbirth in China. The Lancet 387, 1995–1996, https://doi.org/10.1016/S0140-6736(16)30461-5 (2016).
Blencowe, H. et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. The Lancet. Global health 4, e98–e108, https://doi.org/10.1016/s2214-109x(15)00275-2 (2016).
WHO. Every Newborn Action Plan consultation 2014, http://www.who.int/maternal_child_adolescent/topics/newborn/enap_consultation/en/.
China, N. B. O. S. O. (China Statistical Press, 2016).
Liu, X., Gao, W. & Yan, H. Measuring and decomposing the inequality of maternal health services utilization in Western Rural China. BMC Health Services Research 14, 102–102, https://doi.org/10.1186/1472-6963-14-102 (2014).
Li, Q. et al. Distribution, source, and risk of organochlorine pesticides (OCPs) and polychlorinated biphenyls (PCBs) in urban and rural soils around the Yellow and Bohai Seas, China. Environmental pollution (Barking, Essex: 1987) 239, 233–241, https://doi.org/10.1016/j.envpol.2018.03.055 (2018).
Qin, W. et al. Estimating benefit equity of government health subsidy in healthcare Services in Shandong Province, China: a cross-sectional study. International journal for equity in health 17, 61, https://doi.org/10.1186/s12939-018-0775-3 (2018).
Li, Y. N., Nong, D. X., Wei, B., Feng, Q. M. & Luo, H. Y. The impact of predisposing, enabling, and need factors in utilization of health services among rural residents in Guangxi, China. BMC Health Serv Res 16, 592, https://doi.org/10.1186/s12913-016-1825-4 (2016).
Qian, Y. et al. An economy-ralated equity analysis of health service utilization by women in economically underdeveloped regions of western China. International journal for equity in health 16, 186, https://doi.org/10.1186/s12939-017-0667-y (2017).
Nan, W., Banghong, Z. & Haifen, Y. A Research on Impacting Factor of Rural Environment and Environment Protection Awareness of Famers. Energy Procedia 5, 2623–2628, https://doi.org/10.1016/j.egypro.2011.03.341 (2011).
Roncati, L., Piscioli, F. & Pusiol, T. The endocrine disruptors among the environmental risk factors for stillbirth. The Science of the total environment 563–564, 1086–1087, https://doi.org/10.1016/j.scitotenv.2016.04.214 (2016).
Oldereid, N. B. et al. The effect of paternal factors on perinatal and paediatric outcomes: a systematic review and meta-analysis. Human reproduction update 24, 320–389, https://doi.org/10.1093/humupd/dmy005 (2018).
Hossain, M. S., Kypri, K., Rahman, B. & Milton, A. H. Smokeless tobacco consumption and stillbirth: Population-based case-control study in rural Bangladesh. Drug and alcohol review 37, 414–420, https://doi.org/10.1111/dar.12566 (2018).
Morales-Suarez-Varela, M., Nohr, E. A., Olsen, J. & Bech, B. H. Potential combined effects of maternal smoking and coffee intake on foetal death within the Danish National Birth Cohort. European journal of public health 28, 315–320, https://doi.org/10.1093/eurpub/ckx222 (2018).
Tshibumbu, D. D. & Blitz, J. Modifiable antenatal risk factors for stillbirth amongst pregnant women in the Omusati region, Namibia. African journal of primary health care & family medicine 8, e1–6, https://doi.org/10.4102/phcfm.v8i1.1054 (2016).
Zhou, Q. et al. A new perspective on universal preconception care in China. Acta obstetricia et gynecologica Scandinavica 95, 377–381, https://doi.org/10.1111/aogs.12865 (2016).
Zhang, S., Wang, Q. & Shen, H. Design of the national free proception health examination project in China. Zhonghua yi xue za zhi 95, 162–165 (2015).
Chen, J. et al. Investigation on folic acid supplementation status among Chinese women in the first trimester of pregnancy. Zhonghua yi xue za zhi 96, 1215–1219, https://doi.org/10.3760/cma.j.issn.0376-2491.2016.15.016 (2016).
Zhou, Q. et al. A new perspective on universal preconception care in China. Acta Obstetricia et Gynecologica Scandinavica 95, 377–381, https://doi.org/10.1111/aogs.12865 (2016).
Liu, J. et al. Seroepidemiology of hepatitis B virus infection in 2 million men aged 21–49 years in rural China: a population-based, cross-sectional study. The Lancet Infectious Diseases 16, 80–86, https://doi.org/10.1016/S1473-3099(15)00218-2 (2016).
Chen, C. & Lu, F. C. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomedical and environmental sciences: BES 17(Suppl), 1–36 (2004).
Hongyan, L., Ya, L. & Shengjin, W. Comparative Analysis of Health Status with Elderly People between South and North China–A Case Control Study of Zhuhai,Changchun and Siping. Population Journal 38, 77–87 (2016).
Yong, B. et al. Analysis of Health Status and Service Demand and Utilization in Community Dweller in City of East and West. 中国卫生经济, 42–44 (2001).
Guoju, L. Survey of Classification with Imbalanced Data. Modern Computer, 30–33, 50, https://doi.org/10.3969/j.issn.1007-1423.2016.04.007 (2016).
Maghsoudlou, S. et al. Consanguineous marriage, prepregnancy maternal characteristics and stillbirth risk: a population-based case-control study. Acta obstetricia et gynecologica Scandinavica 94, 1095–1101, https://doi.org/10.1111/aogs.12699 (2015).
Lamont, K., Scott, N. W., Jones, G. T. & Bhattacharya, S. Risk of recurrent stillbirth: systematic review and meta-analysis. Bmj 350, h3080, https://doi.org/10.1136/bmj.h3080 (2015).
Aminu, M. et al. Causes of and factors associated with stillbirth in low- and middle-income countries: a systematic literature review. BJOG: an international journal of obstetrics and gynaecology 121(Suppl 4), 141–153, https://doi.org/10.1111/1471-0528.12995 (2014).
Auger, N., Delezire, P., Harper, S. & Platt, R. W. Maternal education and stillbirth: estimating gestational-age-specific and cause-specific associations. Epidemiology 23, 247–254, https://doi.org/10.1097/EDE.0b013e31824587bc (2012).
Savitz, D. A., Olshan, A. F. & Gallagher, K. Maternal occupation and pregnancy outcome. Epidemiology 7, 269–274 (1996).
Lean, S. C., Derricott, H., Jones, R. L. & Heazell, A. E. P. Advanced maternal age and adverse pregnancy outcomes: A systematic review and meta-analysis. PloS one 12, e0186287, https://doi.org/10.1371/journal.pone.0186287 (2017).
Green, L. W. Manual for scoring socioeconomic status for research on health behavior. Public health reports (Washington, D.C. 1896) 85, 815–827 (1970).
Yudong, Z., Rong, L., Yanling, L., Feng, X. & Yang, Z. Colinearity analysis of multiple logistic regression. Chinese health statistics 17, 259–261, https://doi.org/10.3969/j.issn.1002-3674.2000.05.001 (2000).
Zhen, J., Lirong, J., Zhifeng, W. & Zhenling, S. Study on current situation of maternal health care coverage in rural area of central and western China. Maternal & Child Health Care of China 28, 5101–5105, https://doi.org/10.7620/zgfybj.j.issn.1001-4411.2013.28.01 (2013).
Liqin, W., Aihua, W. & Xinghui, C. U. I. Pesticide exposure Intensity of exposure Women pesticide users Reproductive health. Chinese JOURNAL OF Social Medicine 33, 160–161,165, https://doi.org/10.3969/j.issn.1673-5625.2016.02.019 (2016).
Shao-mei, Y. et al. Relationship between pesticide exposure and adverse pregnancy outcomes among famers: a meta-analysis. Chinese Journal of Industrial Hygiene and Occupational Diseases 30, 859–862, https://doi.org/10.3760/cma.j.issn.1001-9391.2012.11.016 (2012).
Wolff, M. S. et al. Prenatal pesticide and PCB exposures and birth outcomes. Pediatric research 61, 243–250, https://doi.org/10.1203/pdr.0b013e31802d77f0 (2007).
Xiaowen, C., Qing, F. & Jie, Z. The application of pesticide in China and its effect on Health. Soft Science of Health 26, 560–562, https://doi.org/10.3969/j.issn.1003-2800.2012.06.022 (2012).
Yan Yongjian, F. A. N. Z. & Jihu, Y. Survey on Using Pesticides in Shandong Province. Journal Of Labour Medicine 17, 178–180, https://doi.org/10.3969/j.issn.1006-3617.2000.03.017 (2000).
Ampt, A. J., Ford, J. B., Taylor, L. K. & Roberts, C. L. Are pregnancy outcomes associated with risk factor reporting in routinely collected perinatal data? New South Wales public health bulletin 24, 65–69, https://doi.org/10.1071/nb12116 (2013).
Flenady, V. et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet (London, England) 377, 1331–1340, https://doi.org/10.1016/s0140-6736(10)62233-7 (2011).
Warland, J., McCutcheon, H. & Baghurst, P. Maternal blood pressure in pregnancy and stillbirth: a case-control study of third-trimester stillbirth. American journal of perinatology 25, 311–317, https://doi.org/10.1055/s-2008-1075031 (2008).
Yao, R., Ananth, C. V., Park, B. Y., Pereira, L. & Plante, L. A. Obesity and the risk of stillbirth: a population-based cohort study. American journal of obstetrics and gynecology 210, 457.e451–459, https://doi.org/10.1016/j.ajog.2014.01.044 (2014).
Lin, W. & Sloan, F. Risk perceptions and smoking decisions of adult Chinese men. J Health Econ 39, 60–73, https://doi.org/10.1016/j.jhealeco.2014.11.006 (2015).
Yang, X. et al. Assessment of successful smoking cessation by psychological factors using the Bayesian network approach. Psychology, health & medicine 21, 652–661, https://doi.org/10.1080/13548506.2015.1073337 (2016).
Chengqiu, W. Study on Reproductive and Embryonic Developmental Toxicity and Mechanism of Formaldehyde and Benzene in Decorated House Indoor Air, Central South University (2010).
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (grant number 81673184). We sincerely appreciate all participants for your support and cooperation. We also would like to thank all the project staff for your hard working.
Author information
Authors and Affiliations
Contributions
Study design, statistical analysis and paper writing: Yimin Qu. and Yu JIANG; Administrative, technical, or material support:, Shi Chen, Hui Pan, Huijuan Zhu, Chengsheng Yan, Shikun Zhang.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qu, Y., Chen, S., Pan, H. et al. Risk factors of stillbirth in rural China: A national cohort study. Sci Rep 9, 365 (2019). https://doi.org/10.1038/s41598-018-35931-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-35931-1
This article is cited by
-
Utilization of preconception care and its impacts on health behavior changes among expectant couples in Shanghai, China
BMC Pregnancy and Childbirth (2021)
-
Preconception ambient temperature and preterm birth: a time-series study in rural Henan, China
Environmental Science and Pollution Research (2021)
-
Impact of free maternal health care policy on maternal health care utilization and perinatal mortality in Ghana: protocol design for historical cohort study
Reproductive Health (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.