Abstract
The aim of this study was to investigate whether non-reassuring foetal status (NRFS) affected an infant’s temperament, or if the temperament formed prenatally resulted in an excessive heart rate reaction that was diagnosed as NRFS. We examined the correlation between NRFS and difficulty in holding a baby, and the amount of crying in the one month after birth, which was considered an indicator of the newborn’s temperament. We divided the cases with NRFS into positive NRFS and false positive NRFS. NRFS was associated with bad mood, frequent crying for a long duration, and intense crying. After adjustment for other covariates, NRFS was associated with bad mood (odds ratio, OR = 1.15, 95% confidence interval, CI = 1.00–1.33), and intense crying (1.12, 1.02–1.24). In the multi-variable model, positive and false positive NRFS were not clearly associated with neonatal irritability. When stratified by parity, NRFS and false positive NRFS were likely to be positively associated with neonatal irritability in parous women. The clear association between NRFS and intense crying was observed in parous women (multi-variable adjusted OR = 1.46, 95% CI = 1.16–1.83), but not in nulliparae (1.01, 0.91–1.12) (p for effect modification <0.01). Similarly, increased odds of intense crying associated with false positive NRFS were only found in parous women (multi-variable adjusted OR = 1.40, 95% CI = 1.09–1.81) (p for effect modification = 0.03). There was no association observed between positive NRFS and irritability; therefore, NRFS has no effect on an infant’s temperament.
Similar content being viewed by others
Introduction
Foetal distress during labour is a risk factor for developmental disorders, including autism1,2. It has also been reported that changes in the temperament of babies with diseases related to neuropsychiatric development can be seen in the neonatal and infant stages3. However, there are almost no reports on the association between foetal distress and infant temperament. Irritability is an important element of temperament. It can negatively affect parent-child relationships, which in turn can lead to child abuse. Furthermore, it affects the interactions between the mother and child as well as the child’s mental health.
To the best of our knowledge, only one study has investigated the relationship between postnatal irritability and changes in foetal heart rate during labour that was used to diagnose foetal distress. The study reported a correlation between reduced heart rate during labour and the proportion of crying as an indication of irritability up to day 5 after birth. However, it is unknown whether this reaction was due to hypoxia or acidaemia during labour, or it was simply caused by the predisposition of the neonate4.
Regarding the possibility that an infant’s personality is already formed in infancy, there are reports that heart rate reactivity in infancy is related to postnatal temperamental reactivity, and the characteristics of an infant’s behaviour represent the individual differences in reactivity during infancy5,6. If we presume that an infant’s temperament is already formed before birth, then their heart rate reactivity to the stress of labour may also differ.
Either way, in clinical practice in obstetrics and gynaecology, the well-being of the foetus is evaluated by monitoring the foetal heart rate. When abnormalities in foetal heart rate are observed, which are usually a result of hypoxia and/or acidaemia, the well-being of the foetus cannot be ascertained. However, even if there is an abnormality of the foetal heart rate, and a diagnosis of non-reassuring foetal status (NRFS) is made, normal umbilical cord arterial blood pH and Apgar scores are noted after birth. Therefore, NRFS false positives are thought to be associated with an increase in the number of Caesarean deliveries7,8,9. However, the cause of NRFS false positives is unknown10,11. Furthermore, the term ‘foetal distress’, an inaccurate and non-specific term, does not reflect the reality; therefore, this term is now being replaced with the term non-reassuring foetal status (NRFS)12. In this article, examples that were previously described as foetal distress are called NRFS.
Cases with foetal heart rate abnormalities that satisfied the criteria of an umbilical cord arterial blood pH ≥ 7.2 and an Apgar score ≥7 at 5 minutes were classified as NRFS false positive13,14. We believe that foetuses with these features and false positive NRFS had an overreaction to labour stress. Given that the amount of crying is said to be related to the behavioural characteristics of the newborn15,16, and the difficulty in holding a baby is said to be related to developmental characteristics17, we examined the correlation between NRFS and the difficulty in holding a baby and the amount of crying in the one month after birth that was considered the temperament of the newborn.
The aim of this study was to ascertain if NRFS affected an infant’s temperament, or if the temperament formed prenatally generated an excessive heart rate reaction diagnosed as NRFS.
Methods
Study participants
The Japan Environment and Children’s Study (JECS), an on-going large-scale birth cohort study, enrolled women as early in pregnancy as possible. The protocol of JECS is described elsewhere along with a discussion on its population representativeness18,19.
The JECS protocol was approved by the Japan Ministry of the Environment’s Institutional Review Board on Epidemiological Studies, and the Ethics Committees of all participating institutions. JECS protocol was conducted in accordance with the Helsinki Declaration and other nationally valid regulations, and written informed consent was obtained from each participant.
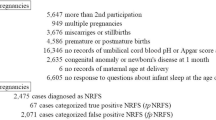
Between 2011–2014, a total of 103,099 pregnancies from fifteen Regional Centres located throughout Japan (Hokkaido, Miyagi, Fukushima, Chiba, Kanagawa, Koshin, Toyama, Aichi, Kyoto, Osaka, Hyogo, Tottori, Kochi, Fukuoka, and South Kyushu/Okinawa) were identified. Of the 103,099 pregnancies, only 97,454 unique mothers were included. Of these, we further excluded 27,129 women due to the following reasons (Supplementary Figure): multiple pregnancies (n = 949); miscarriages or stillbirths or no delivery records (n = 3,709); preterm (<37 weeks of gestation) or post-term (>41 weeks) deliveries (n = 4,586); missing information on maternal age at delivery, umbilical cord blood pH, or Apgar scores at five minutes (n = 16,351); and no responses to the three irritability questions in the maternal questionnaire at one month after delivery (n = 1,534). The remaining 70,325 participants were included in our final analyses.
Non-reassuring foetal status (NRFS)
In the present study, we defined NRFS as that diagnosed by an obstetrician, which was obtained from the medical record transcriptions at birth20. In Japan, when abnormalities in foetal heart rate are observed, obstetricians diagnose the cases using intrapartum management guidelines based on the foetal heart rate pattern classification20. That is, the combination of the various components of the FHR patterns serves to estimate the degree of risk for the foetus, which is then classified into five levels. The five level categories are the same as those used in countries such as the United States21. Those with high risk levels of 3–5 are diagnosed with NRFS. However, in the cohort data, there was no information on the five levels, and only information on the presence or absence of NRFS was available. Of all the infants with NRFS, infants with an umbilical cord blood pH <7.2 and an Apgar score of <7 at 5 minutes after birth were categorised as having positive NRFS, and infants with an umbilical cord arterial blood pH ≥7.2 and an Apgar score ≥7 at 5 minutes were categorised as having false positive NRFS.
Infant irritability
A self-administered questionnaire was distributed to mothers who visited for a health check-up at one month after delivery by research coordinators or via mail. The questionnaire included three questions about a baby’s irritability. The first question was “When you hold your baby, how often do you feel difficulty to hold your baby due to his/her fretting, crying or throwing his/her head back?” with options of “often”, “sometimes”, “seldom”, and “none”, and those who answered “often” were categorised as ‘bad’ mood. The second question was “How often and long does your baby cry?” with options of “quite often and long”, “sometimes and shortly”, and “seldom and hardly”, and those who answered as “quite often and long” were categorised as ‘frequent crying for a long duration’. The third question was “Does your baby cry very hard sometimes no matter what you do to stop him/her?” with options of “yes” and “no”, and those who answered as “yes” were categorised as ‘intense crying’.
Covariates
Maternal characteristics, including maternal age at delivery, smoking habits, alcohol consumption, educational background, household income, parity, and infertility treatment, were collected via self-administered questionnaires and/or medical record during the pregnancy. Also, delivery and birth record transcripts were obtained to gather information about the gestational age at delivery, type of delivery, infant sex, and birth weight. In this study, small for gestational age (SGA) was defined as birth weight <10th percentile of birth weight standards by gestational age, sex, and parity for Japanese neonates22. Postpartum depressive symptoms were assessed using the Edinburgh Postnatal Depression Scale (EPDS) included in the questionnaire at one month after delivery23. According to previous studies, participants with a score of 9 or more were categorised as having depressive symptoms24.
Statistical analyses
Multilevel logistic regression analyses were used to explore the association between NRFS and neonatal irritability, considering that mothers were nested in each Regional Centres, and to estimate the odds ratios (ORs) of neonatal irritability and 95% confidence intervals (CIs), without NRFS as a reference. We initially adjusted for maternal age at delivery, and then further adjusted for educational background (<10, 10–12, 13–16, ≥17 years), household income (<2, 2 to <4, 4 to <6, 6 to 8, 8 to <10, ≥10 million Japanese-yen), smoking habits (never smoked, ex-smokers who quit before pregnancy, smokers during early pregnancy), alcohol consumption (never drank, ex-drinkers who quit before pregnancy, drinkers during early pregnancy), gestational age at birth (37–38, 39–40, and 41 weeks of gestation), SGA (yes, no), infant sex (boys, girls), parity (0, ≥1), infertility treatment (yes, no), type of delivery (vaginal, Caesarean), and postpartum depressive symptoms (yes, no).
When the frequencies of NRFS were affected by certain background factors (except clinical known factors), we performed stratified analyses. Effect modification of the association between NRFS and neonatal irritability according to such factors was evaluated by a likelihood ratio test. This study used the dataset jecs-ag-20160424, which was released in June 2016, and revised in October 2016. Stata version 14 (StataCorp LP, College Station, Texas, USA) was used for all analyses.
Results
The mean maternal age at delivery was 31.2 (standard deviation, SD = 5.1) years in this study population. The baseline characteristics in those with or without NRFS are shown in Table 1. Naturally, the distribution of the type of delivery, gestational age, and SGA differed by the presence or absence of NRFS. Mothers categorised as NRFS tended to be nulliparous and delivered boys. The frequency of NRFS was 3.9%. Among the cases of NRFS, 3.3% were positive NRFS, 83.3% were false positive NRFS and 13.4% did not belong to any of these groups.
Table 2 shows the ORs for NRFS and neonatal irritability. In the maternal age-adjusted model, we observed the association of NRFS with a bad mood, frequent crying for a long duration, and intense crying. After adjustment for other covariates, NRFS was associated with a bad mood (OR = 1.15, 95% CI = 1.00–1.33), and intense crying (1.12, 1.02–1.24), although point estimates of OR were attenuated. In the multi-variable model, positive and false positive NRFS were not clearly associated with neonatal irritability.
When we stratified by parity, NRFS and false positive NRFS were likely to be positively associated with neonatal irritability in parous women (Table 3). The clear association between NRFS and intense crying was observed in parous women (multi-variable adjusted OR = 1.46, 95% CI = 1.16–1.83), but not in nulliparous women (1.01, 0.91–1.12) (p for effect modification <0.01). Similarly, increased odds of intense crying associated with false positive NRFS were only found in parous women (multi-variable adjusted OR = 1.40, 95% CI = 1.09–1.81) (p for effect modification = 0.03). The number of cases of positive NRFS was small; therefore, we did not perform stratified analysis in these cases. Effect modification of the association between NRFS and neonatal irritability was not observed with the sex of the infant (Supplementary Table).
Discussion
Although all cases of NRFS were associated with a bad mood, and intense crying, cases of positive and false positive NRFS were not clearly associated with infant irritability. However, the clear association between false positive NRFS and intense crying was observed in parous women. Therefore, the events during labour did not affect the irritability of the newborns, and, thus, the irritability had formed prenatally.
Some reports have stated that the intrauterine environment affects an infant’s mental development25,26,27,28, while others have stated that it affects the temperament of neonates29. Furthermore, recently there have been reports on the link between the autonomic nervous system reactivity and temperament; people with small fluctuations in their heart rate during the resting phase have excessive circulation reactions–the smaller the fluctuation, the less able they are to control their emotions, and their emotional reactions are greater–and they are less able to withstand significant stress30,31,32.
Factors such as congenital malformations, infections, and cigarette smoking have been linked to false positive NRFS; furthermore, there are reports of a high rate of false positive NRFS even when the foetus’ well-being has been maintained33,34,35. Despite NRFS resulting in emergency Caesarean section deliveries in foetuses with cardiac malformations, many of them do not have acidosis36. Foetal heart rate patterns are mainly produced by the autonomic nervous system and the cardiovascular centre in the brain stem10,11. We believe that the false positive NRFS may be caused by several factors that can affect these systems in the absence of hypoxia and/or acidaemia.
Recently there has been an increasing number of reports about the effect of maternal inflammation and immune activity on the neuropsychiatric development of a child37,38,39. We previously clarified that air pollution exposure during early pregnancy, which results in systemic inflammation, is related to false positive NRFS40. The intrauterine environment affects the foetus, and it may affect the irritability of the newborn; therefore, so we presume that false positive NRFS also incorporate factors related to the infant’s temperament.
One of the limitations of this study was that the cohort data had no information on the NRFS 5-grade classification; only data on the presence or absence of NRFS after diagnosis by an obstetrician was available. Thus, we could not perform analyses for the FHR pattern risk level in this study. However, since obstetricians diagnosed the patients using intrapartum management guidelines based on the foetal heart rate pattern classification, at least the diagnosis of NRFS can be considered accurate. We expect that analyses based on the FHR pattern risk levels will be conducted in the future.
In addition, another limitation of this study is that the information was collected from the mothers via a questionnaire. The infants were not directly examined, which could possibly result in a bias. However, the strength of this study is in its large sample size. Therefore, we believe that a certain trend can be detected; namely, the differences in experiences of the mothers depending on the birth order of the child may have affected the outcome. Therefore, we conducted our investigation after classifying the mothers based on parity41,42,43. An association was found between false positive NRFS and intense crying only in multipara women. With the first child, the mother has little childrearing experience, she is unable to make a comparison, which may have suppressed the distribution spread. Either way, there was no correlation seen between positive NRFS and irritability. Therefore, we believe that NRFS has no effect on an infant’s temperament.
References
Garon, N. et al. Temperament and its association with autism symptoms in a high-risk population. J. Abnorm. Child Psychol. 44, 757–769 (2016).
Gardener, H., Spiegelman, D. & Buka, S. L. Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis. Pediatrics. 128, 344–355 (2011).
Hultman, C. M., Sparén, P. & Cnattingius, S. Perinatal risk factors for infantile autism. Epidemiology. 13, 417–423 (2002).
Woodson, R. H. et al. Fetal mediators of the relationships between increased pregnancy and labour blood pressure and newborn irritability. Early Hum. Dev. 3, 127–139 (1979).
DiPietro, J. A., Ghera, M. M. & Costigan, K. A. Prenatal origins of temperamental reactivity in early infancy. Early Hum. Dev. 84, 569–575 (2008).
DiPietro, J. A., Hodgson, D. M., Costigan, K. A. & Johnson, T. R. Fetal antecedents of infant temperament. Child Dev. 67, 2568–2583 (1996).
Spencer, J. A. Clinical overview of cardiotocography. Br. J. Obstet. Gynaecol. 100, 4–7 (1993).
Devoe, L. Electronic fetal monitoring: does it really lead to better outcomes? Am. J. Obstet. Gynecol. 204, 455–456 (2011).
Neilson, D. R., Freeman, R. K. & Mangan, S. Signal ambiguity resulting in unexpected outcome with external fetal heart rate monitoring. Am. J. Obstet. Gynecol. 198, 717–724 (2008).
Alfirevic, Z., Devane, D. & Gyte, G.M. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst. Rev. CD006066 (2013).
Pinas, A. & Chandraharan, E. Continuous cardiotocography during labour: Analysis, classification and management. Best Pract. Res. Clin. Obstet. Gynaecol. 30, 33–47 (2016).
Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. ACOG Committee Opinion. Number 326, December 2005. Inappropriate use of the terms fetal distress and birth asphyxia. Obstet. Gynecol. 106, 1469–1470 (2005)
Riley, R. J. & Johnson, J. W. Collecting and analyzing cord blood gases. Clin. Obstet. Gynecol. 36, 13–23 (1993).
Casey, B. M., McIntire, D. D. & Leveno, K. J. The continuing value of the Apgar score for the assessment of newborn infants. N. Engl. J. Med. 344, 467–471 (2001).
Kusaka, R., Ohgi, S., Shigemori, K. & Fujimoto, T. Crying and behavioral characteristics in premature infants. J. Jpn. Phys. Ther. Assoc. 11, 15–21 (2008).
Ohgi, S., Gima, H. & Akiyama, T. Neonatal behavioural profile and crying in premature infants at term age. Acta Paediatr. 95, 1375–1380 (2006).
Garon, N. et al. Temperament and its association with autism symptoms in a high-risk population. J. Abnorm. Child Psychol. 44, 757–769 (2016).
Michikawa, T. et al. Baseline profile of participants in the Japan Environment and Children’s Study (JECS). J. Epidemiol. 28, 99–104 (2018).
Kawamoto, T. et al. Rationale and study design of the Japan Environment and Children’s study (JECS). BMC Public Health. 14, 25 (2014).
Okai, T. et al. Perinatology Committee of the Japan Society of Obstetrics and Gynecology. Intrapartum management guidelines based on fetal heart rate pattern classification. J. Obstet. Gynaecol. Res. 36, 925–928 (2010).
Parer, J. T. & Ikeda, T. A framework for standardized management of intrapartum fetal heart rate patterns. Am J Obstet Gynecol. 197, 26.e1–6 (2007).
Itabashi, K., Miura, F., Uehara, R. & Nakamura, Y. New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr. Int. 56, 702–708 (2014).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry. 150, 782–726 (1987).
Yamashita, H. & Yoshida, K. Screening and intervention for depressive mothers of new-born infants. Seishin Shinkeigaku Zasshi. 105, 1129–1135 (2003).
Schlotz, W., Godfrey, K. M. & Phillips, D. I. Prenatal origins of temperament: fetal growth, brain structure, and inhibitory control in adolescence. PLoS One. 9, e96715 (2014).
Schlotz, W. & Phillips, D. I. Fetal origins of mental health: Evidence and mechanisms. Brain Behav. Immun. 23, 905–916 (2009).
Räikkönen, K., Pesonen, A. K., Roseboom, T. J. & Eriksson, J. G. Early determinants of mental health. Best Pract. Res. Clin. Endocrinol. Metab. 26, 599–611 (2012).
O’Donnell, K. J. & Meaney, M. J. Fetal origins of mental health: The developmental origins of health and disease hypothesis. Am. J. Psychiatry. 174, 319–328 (2017).
Knuesel, I. et al. Maternal immune activation and abnormal brain development across CNS disorders. Nat. Rev. Neurol. 10, 643–660 (2014).
Estes, M. L. & McAllister, A. K. Maternal immune activation: Implications for neuropsychiatric disorders. Science 19(353), 772–777 (2016).
Careaga, M., Murai, T. & Bauman, M. D. Maternal immune activation and autism spectrum disorder: From rodents to nonhuman and human primates. Biol. Psychiatry. 81, 391–401 (2017).
Oida, E., Kannagi, T., Moritani, T. & Yamori, Y. Physiological significance of absolute heart rate variability in postural change. Acta Physiol. Scand. 165, 421–422 (1999).
Garite, T. J., Linzey, E. M., Freeman, R. K. & Dorchester, W. Fetal heart rate patterns and fetal distress in fetuses with congenital anomalies. Obstet. Gynecol. 53, 716–720 (1979).
Powell Phillips, W. D. & Towell, M. E. Abnormal fetal heart rate associated with congenital abnormalities. Br. J. Obstet. Gynaecol. 87, 270–274 (1980).
Kaneko, M., Sameshima, H., Ikeda, T., Ikenoue, T. & Minematsu, T. Intrapartum fetal heart rate monitoring in cases of cytomegalovirus infection. Am. J. Obstet. Gynecol. 191, 1257–1262 (2004).
Ueda, K. et al. Intrapartum fetal heart rate monitoring in cases of congenital heart disease. Am. J. Obstet. Gynecol. 201, 64.e1–64.e6 (2009).
Roza, S. J. et al. Intrauterine growth and infant temperamental difficulties: the Generation R Study. J. Am. Acad. Child. Adolesc. Psychiatry. 47, 264–272 (2008).
Katahira, K., Fujimura, T., Matsuda, Y. T., Okanoya, K. & Okada, M. Individual differences in heart rate variability are associated with the avoidance of negative emotional events. Biol. Psychol. 103, 322–331 (2014).
Gillie, B. L., Vasey, M. W. & Thayer, J. F. Heart rate variability predicts control over memory retrieval. Psychol. Sci. 25, 458–465 (2014).
Morokuma, S., Michikawa, T., Yamazaki, S., Nitta, H. & Kato, K. Association between exposure to air pollution during pregnancy and false positives in fetal heart rate monitoring. Sci. Rep. 7, 12421 (2017).
Stoolmiller, M. Implications of the restricted range of family environments for estimates of heritability and nonshared environment in behavior-genetic adoption studies. Psychol. Bull. 125, 392–409 (1999).
Jenkins, J. M., Rasbash, J. & O’Connor, T. G. The role of the shared family context in differential parenting. Dev. Psychol. 39, 99–113 (2003).
Bornstein, M. H. et al. Infant temperament stability by age, gender, birth order, term status, and socioeconomic status. Child. Dev. 86, 844–863 (2015).
Acknowledgements
We would like to express our gratitude to all the participants in this study and all the individuals involved in data collection. We would also like to thank the following members of the JECS (principal investigator, Toshihiro Kawamoto) as of 2017: Hirohisa Saito (National Center for Child Health and Development, Tokyo, Japan), Reiko Kishi (Hokkaido University, Sapporo, Japan), Nobuo Yaegashi (Tohoku University, Sendai, Japan), Koichi Hashimoto (Fukushima Medical University, Fukushima, Japan), Chisato Mori (Chiba University, Chiba, Japan), Shuichi Ito (Yokohama City University, Yokohama, Japan), Zentaro Yamagata (University of Yamanashi, Chuo, Japan), Hidekuni Inadera (University of Toyama, Toyama, Japan), Michihiro Kamijima (Nagoya City University, Nagoya, Japan), Takeo Nakayama (Kyoto University, Kyoto, Japan), Hiroyasu Iso (Osaka University, Suita, Japan), Masayuki Shima (Hyogo College of Medicine, Nishinomiya, Japan), Yasuaki Hirooka (Tottori University, Yonago, Japan), Narufumi Suganuma (Kochi University, Nankoku, Japan), Koichi Kusuhara (University of Occupational and Environmental Health, Kitakyushu, Japan), and Takahiko Katoh (Kumamoto University, Kumamoto, Japan). We also thank Kevin Y. Urayama for his valuable comments and edit, as well as James R. Valera for his editorial support. NM and SM initiated the study concept and designed the analysis protocol; NM analysed the data; NM and CN wrote the paper and have primary responsibility for the final content. K.K., M.S., E.S., M.T., A.S., T.K., S.O., K.K. contributed critical revisions to the manuscript and read and approved the final manuscript. The Japan Environment and Children’s Study was funded by the Ministry of the Environment, Japan. The findings and conclusions of this article are solely the responsibility of the authors and do not represent the official views of the above government.
Author information
Authors and Affiliations
Contributions
Study concept and design: S.M. Statistical analyses: T.M. Drafting of the manuscript: S.M. and T.M. and have primary responsibility for the final content. K.K., M.S., E.S., M.T., A.S., T.K., S.O., K.K. contributed critical revisions to the manuscript and read and approved the final manuscript. Critical revision of the manuscript for important intellectual content: all authors. Manuscript review: all authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Morokuma, S., Michikawa, T., Kato, K. et al. Non-reassuring foetal status and neonatal irritability in the Japan Environment and Children’s Study: A cohort study. Sci Rep 8, 15853 (2018). https://doi.org/10.1038/s41598-018-34231-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-34231-y
Keywords
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.