Abstract
Mitochondrial pathology has been implicated in the pathogenesis of psychotic disorders. A few studies have proposed reduced leukocyte mitochondrial DNA (mtDNA) copy number in schizophrenia and bipolar disorder type I, compared to healthy controls. However, it is unknown if mtDNA copy number alteration is driven by psychosis, comorbidity or treatment. Whole blood mtDNA copy number was determined in 594 psychosis patients and corrected for platelet to leukocyte count ratio (mtDNAcnres). The dependence of mtDNAcnres on clinical profile, metabolic comorbidity and antipsychotic drug exposure was assessed. mtDNAcnres was reduced with age (β = −0.210, p < 0.001), use of clozapine (β = −0.110,p = 0.012) and risperidone (β = −0.109,p = 0.014), dependent on prescribed dosage (p = 0.006 and p = 0.026, respectively), and the proportion of life on treatment (p = 0.006). Clozapine (p = 0.0005) and risperidone (p = 0.0126) had a reducing effect on the mtDNA copy number also in stem cell-derived human neurons in vitro at therapeutic plasma levels. For patients not on these drugs, psychosis severity had an effect (β = −0.129, p = 0.017), similar to age (β = −0.159, p = 0.003) and LDL (β = −0.119, p = 0.029) on whole blood mtDNAcnres. Further research is required to determine if mtDNAcnres reflects any psychosis-intrinsic mitochondrial changes.
Similar content being viewed by others
Introduction
Psychosis is a common trait in schizophrenia (SZ), schizoaffective disorder, delusional disorder and bipolar disorder (BD)1, displayed as a range of symptoms reflecting dissociation from reality. Psychosis and the underlying psychiatric diagnoses have shown a robust association with somatic conditions linked to aging such as cardiovascular disease (CVD)2, inflammation3, and obesity4. These somatic conditions may be caused by chronic oxidative stress5,6 or exposure to drug toxicity7, leading to cellular ageing8,9 which recently has been found increased in psychotic disorders10,11.
The mitochondrion is the organelle for ATP production which contains multiple copies of mitochondrial DNA (mtDNA), in blood present in leukocytes and platelets. Ongoing oxidative chain reactions within its compartments make mitochondria a significant source of intracellular reactive oxygen and nitrogen species (ROS/RNS)12. The molecular machinery and DNA of the mitochondria are thus at risk from the deleterious effects of oxidative stress resulting in mitochondrial dysfunction13.
Mitochondrial dysfunction and ROS/RNS are implicated in the induction of apoptosis through caspase activation14,15, inflammasome recruitment16 and the activation of downstream cytokines and inflammatory mediators17. In the central nervous system, mitochondrial dysfunction could through these processes lead to neurodegeneration, the precursor to cognitive decline and dementia. Mitochondrial dysfunction has been implicated in various somatic and neuro-degenerative disorders18,19. Additionally, evidence of mitochondrial dysfunction in BD and SZ has been reported in magnetic resonance spectroscopy studies of small patient groups of BD and SZ20,21. Mitochondrial structural abnormalities have been reported in patients with BD22 and SZ23,24 and both diseases are associated with mtDNA mutations and polymorphisms25,26,27,28,29,30,31,32,33,34. Hyper-oxidative states and chronic inflammation resulting from mitochondrial dysfunction may be involved in the progression of SZ6. Alterations in mtDNA copy number have been studied as a sensitive index of cellular oxidative stress, mitochondrial dysfunction, the aging process35,36,37,38, and have been associated with a range of factors such as age, gender, smoking and alcohol intake39,40,41,42. In addition to this, a few studies have reported alterations in leukocyte or whole blood mtDNA copy number in patients of psychotic disorders10,11,42,43,44. Li et al., reported lower whole blood mtDNA copy number in antipsychotic drug treatment naïve SZ patients compared to healthy controls, and lower mtDNA copy number in patients being linked to better treatment response10. Chang et al. showed that leukocyte mtDNA copy number reduction and increased oxidative damage was present in euthymic patients with BD type I (BD-I) compared to healthy controls and De Sousa et al. showed that specifically BD-I patients had reduced leukocyte mtDNA copy number compared to BD type II (BD-II) patients and healthy controls43,44. Conversely, Cai et al. and Tyrka et al. showed that childhood adversity as well as depression and anxiety disorders were associated with higher saliva or whole blood mtDNA copy number11,45.
Psychosis is common in both BD-I and SZ46,47. There are several lines of evidence, for shared disease etiology in SZ and BD, from pharmacology, pathology, family segregation and genetic studies48,49,50,51,52,53. Interestingly, amongst the shared endophenotypes of BD-I and SZ are dysregulation of energy metabolism and mitochondrial dysfunction20,54,55. Conversely, patients of bona-fide mitochondrial disorders experience psychotic symptoms and have been misdiagnosed as BD or SZ. This provides more explicit support for the link between mitochondrial dysfunction and psychosis-like symptoms56,57,58,59.
Anti-psychotic drugs60, especially clozapine, are known to increase the risk for obesity and metabolic syndrome (MetS)7,61,62. MetS consists of a group of factors, including abdominal obesity, hyperglycemia, dyslipidemia, and hypertension that lead to diabetes and CVD, overrepresented in schizophrenia spectrum of disorders (SSD)4 and BD63. An in vitro study suggested that clozapine causes MetS-like effects at the cellular level by inducing mitochondrial alterations, inflammation and insulin resistance in insulin responsive cells64. Intriguingly, while mtDNA copy number reduction have been attributed to MetS65, mtDNA alterations caused by antipsychotic drug treatment of patients has to our knowledge not been investigated much in clinical cohorts even if some antipsychotic drugs are known to impair mitochondrial function in various transformed cell lines in vitro and in rodent brain in vivo64. Mitochondria exist in both platelets and leukocytes, and may vary in count and size between subpopulations of leukocytes66,67,68. Platelets skew the mtDNA copy number as on average they have 1.6 molecules of mtDNA with no accompanying nuclear DNA, whereas leukocytes have between 5–30 copies of mtDNA and a nuclear genome66,67,68. Recent specifications for the refinement of mtDNA copy number assessment in whole blood, through correction for leukocyte and thrombocyte count67,68, are yet to be adopted by investigators of mtDNAcn in psychosis cohorts68,69,70.
Here, we investigated whole blood mtDNA copy number when corrected for platelet and leukocyte counts, in relation to clinical characteristics in a cohort of psychosis patients, the vast majority of whom were diagnosed with SSD or BD type I. Additionally, the effects of antipsychotic drugs on mtDNA copy number were investigated by using human neurons in vitro. In the present study we aimed to determine if mtDNA copy number was associated to (i) severity of psychotic illness, (ii) exposure to specific antipsychotic drugs, and (iii) degree of metabolic comorbidity in psychosis patients. Based on the aforementioned reports, we hypothesized that the mtDNA copy number would be (i) decreased in those with more severe psychosis, (ii) reduced in those taking antipsychotics with reported mitochondrial toxicity, and (iii) reduced with metabolic comorbidity.
Materials and Methods
Psychosis patient group
Patients receiving routine clinical treatment from several specialist psychosis clinics were recruited to the Swedish Study of Metabolic Risks in Psychosis (SMRP)71,72. The diagnostic and statistical manual of mental disorders, 4th Ed. (DSM-IV) was used to make clinical diagnoses of psychiatric disorders1. The evaluation of the severity of mental illness was reported by the clinician according to the clinical global impression-severity scale (CGI-S)73, duration of illness, type of current treatment and duration of all treatment received. Medical records were used for the confirmation of medication and dosage. Most patients were treated with anti-psychotics from the onset of syndrome (Supplementary Fig. S1A and B). A self-reported questionnaire in the clinic, under the supervision of a nurse, was used to evaluate somatic health, smoking status and alcohol consumption. Waist circumference and body mass index were measured. The presence of psychiatric disorders in first degree relatives was reported. After an overnight fast, venous blood was collected. Whole blood and serum samples were saved at −80 °C until laboratory analysis. Consecutively recruited patients, n = 614, diagnosed with psychosis were included for the present investigation. The patient characteristics analyzed in this study are presented in Table 1. All participants provided informed consent in writing and ethical approval for the study was received from the Stockholm Regional Ethics Review Board. All methods were performed conforming to applicable guidelines and regulations designated by Karolinska Institutet and the Stockholm Regional Ethics Review Board.
Whole blood mtDNA copy number, adjusted for platelet to leukocyte count ratio, of the patients were investigated for association with gender, age, CGI-S score, smoker status, alcohol consumption, and psychiatric diagnosis together with antipsychotic drug treatment, presence of mood stabilizer, and with variables associated with the metabolic profile of patient including waist circumference, presence of high blood pressure, fasting blood levels of high-density-lipoprotein (HDL), low-density-lipoprotein (LDL), insulin sensitivity marker (HOMA-IR): homeostatic model of assessment for insulin resistance74, glucose levels, and presence of metabolic syndrome (MetS). Gender, smoking status, presence of antipsychotic and mood stabilizing drugs, presence of high blood pressure and MetS were dichotomous variables while all others were continuous variables. Non-smokers were designated as those who have not smoked at all and all others were considered smokers. MetS and high blood pressure were defined according to International Diabetes Federation (IDF) criteria(61).
Measurement inflammation and metabolic markers in the psychosis patients
Serum lipid profiles (HDL and LDL), plasma glucose, insulin levels and blood cell counts, were determined according to standard GLP protocols. Analyses were performed at the clinical laboratory of the Karolinska University Hospital.
Whole blood DNA extraction and mitochondrial DNA copy number (mtDNA)
DNA was extracted from venous blood using a standard phenol-chloroform method (Lindblom and Holmlund)75 followed by desalting using Illustra NAP-5 columns (GE Healthcare, Buckinghamshire, UK) and was quantified spectrophotometrically with the NanoDrop ND-1000 spectrophotometer (NanoDrop Technologies, Wilmington, DE, USA).
The copy number of mitochondrial DNA per nuclear genome (i.e. per cell) was determined using real-time quantitative PCR (qPCR) according to Rooney JP76 and Venegas V77 protocol. The relative amount of mitochondrial gene tRNA-Leu(UUR), to the nuclear single-copy gene β2-microglobulin (B2M) (mtDNA copy number) was determined using a standard curve. In brief, each DNA sample (4.0 ng) was assessed for tRNA-Leu(UUR) and B2M in triplicate within the same 384-well plate, amplified by using Power SYBR Green in 10 µl total reaction volume. The reaction was performed on QuantStudio 7 Flex (Applied Biosystems; Life Technologies; Thermo Fisher Scientific, Waltham, MA, USA) with the following conditions: 95 °C for 15 min, followed by 40 repeats of 95 °C for 15 s and 60 °C for 1 min, followed by a dissociation stage to monitor amplification specificity. The same standard curve of control genomic human DNA (Applied Biosystems) ranging from 10 ng to 0.016 ng, was run on each plate for both genes and was used to determine the quantity of each gene for each sample. This allowed controlling for differences in the efficiencies between that of mtDNA and B2M. The gene quantities were then used to determine the M/S ratio for each sample. DNA samples with a Ct standard deviation of ≥0.3 between triplicates or a Ct value outside the standard curve were omitted from the analyses. Samples were analyzed in 12 consecutive plates. R2 coefficients of the standard curves were above 0.99 for each primer set and 384-plate. The inter-plate coefficient of variation (CV) of M/S ratio was 8.3% calculated as a mean from three inter-plate control samples run in the 12, 384-well plates. The mean intra-plate CV of M/S ratio of the three control samples in triplicates was 4.6%. Primer binding regions were selected for low deletional <3%78 or mutational (SNPs) exposure 2.2%79. No known psychiatry related SNPs are present in the primer binding mtDNA regions (Online Mendelian Inheritance in Man, OMIM®80 and www.mitomap.org)79. The probability of random somatic mutations to occur at the primer binding regions is calculated to be 0.24%. For a subset of the patients an alternative amplicon in the D-loop region of the mitochondrial genome was targeted for the quantification of mtDNA to confirm the sensitivity of the assay. This D-loop amplicon was selected based on Bai and Wong78 and was carefully designed from mtDNA sequences that do not contain reported mutations or polymorphisms occurring in more than 1.6% of the population (http://www.genpat.uu.se/mtDB/Polysites)79,81. The D-loop region has been used for mtDNA content analysis in similar investigations for mtDNA copy number quantification11,42. mtDNAcn measurements targeting the D-loop and tRNA-Leu(UUR) were compared and found to be highly correlated, n = 55, r = 0.996, p = 1.62E-58.
The primer sequences were (written 5′ → 3′): mtDNA [tRNA-Leu(UUR)] Fw: CAC CCA AGA ACA GGG TTT GT; mtDNA Rv: TGG CCA TGG GTA TGT TGT TA; B2M Fw: TGC TGT CTC CAT GTT TGA TGT ATC T; B2M Rv: TCT CTG CTC CCC ACC TCT AAG T. Alternative primer binding region in D-loop of mitochondrial genome (written 5′ → 3′): D-loop Fw: CAT CTG GTT CCT ACT TCA GGG; D-loop Rv:TGA GTG GTT AAT AGG GTG ATA GA.
The mtDNA copy number measurement success rate was 97% (594/614 samples). mtDNA copy number was corrected for platelet and leukocyte count as these variables are known to affect MS ratio. Platelets have mitochondria and accompanying mtDNA but no nuclei and hence lack a nuclear genome, which results in an overestimation of mtDNA68. Whole blood derived mtDNA are associated with leukocyte count as reported by several groups and thus a correction for the platelet and leukocyte have been suggested as a refinement to the mtDNA copy number measurement68,69,70.
Generation of human neurons in vitro and drug treatment
The long-term neuroepithelial stem cell (NESC) line I3.2, derived from human embryonic stem cells and previously described82 was used for the generation of human neurons in vitro. For maintenance, NESC were cultured on poly-l-Ornithine (PLO, Sigma-Aldrich, Irvine, UK) and laminin (Sigma-Aldrich, Irvine,UK) coated wells, in DMEM/F12 (Gibco) media supplemented with N2 and B27 supplements (Life Technologies; Carlsbad, CA, USA) in the presence of the growth factors EGF and FGF2-basic as previously described82. To induce differentiation, EGF and FGF2-basic were removed from the media (Supplementary Fig. 2A and B). Briefly, NESC were seeded on PLO/laminin at the density of around 75000–150000 cells per well, in a 48-well plate, and cultured for 7 days in DMEM/F12 media supplemented with N2 (1:100) and B27 (1:100) supplements. After one week of differentiation, media was changed to DMEM/F12 supplemented with N2 (1:100) with the addition of glial cell-derived neurotrophic factor (GDNF) 20 ng/ml, brain-derived neurotrophic factor (BDNF) 20 ng/ml, ascorbic acid 10 mM, dibutyryl adenosine 3′,5′-cyclic monophosphate sodium salt (dcAMP) 25 mM. Drug treatments started after 2 weeks of in vitro differentiation, when NESCs had a clear neuronal morphology. Differentiated neurons were characterized through immunohistochemistry stains for neuronal marker TUBB3.
For drug treatments, neurons were treated in plain DMEM/F12 media supplemented with only N2 (1:100), with the addition of either the vehicle or different concentrations of the drugs for one week before they were processed for DNA extraction. Clozapine and risperidone were dissolved in 1 M HCl before added to cell culture medium in the concentrations of 0.075 μM, 0.75 μM and 0.025 μM, 0.25 μM respectively. The vehicle used was plain DMEM/F12 media acidified by 0.0025 μM HCl, pH neutralized by CO2 buffer. The concentrations were selected to simulate clinical target concentrations in plasma and diluted by 10-fold to simulate concentration in the cerebrospinal fluid and brain interstitial fluid83,84,85. At the end of treatment, cells were lysed and DNA extraction was performed using the Quick-DNA™ Miniprep Plus Kit (Zymo Research Corp, Irvine, CA, USA). Subsequently mtDNA copy number determination was performed as described above. Experiments were run in 3 biological replicates.
Statistical analyses
The effect of platelet and leukocyte counts on mtDNA copy number (mtDNAcn) was assessed by regressing mtDNAcn on age, platelet count and leukocyte count as follows: mtDNAcn = b0 + b1 (age) + b2 (leukocyte count) + b3 (platelet count). Thereafter, mtDNAcn was corrected for platelet and leukocyte counts by regressing mtDNAcn on the platelet to leukocyte count ratio (platelet count/leukocyte count), as outlined in Hurtado-Roca, et al.68, generating normally distributed unstandardized residuals. The unstandardized residual variable, hereafter designated as mtDNAcnres, was treated as the dependent variable in the following regression analyses.
We evaluated the significance of psychiatric diagnosis on mtDNAcnres using an analysis of covariance (ANCOVA) adjusting for covariates suggested to influence mtDNAcnres, i.e. age, gender, smoking, alcohol intake and psychosis severity10,39,40,41,42,86,87. Non-parametric Mann Whitney U test, was used to assess difference in mtDNAcnres between patients with MetS and those without MetS.
To study putative predictors of mtDNAcnres, regression modelling was performed as previously described72,88. In brief, an iterative method of regression modelling was initiated with no variables in the model, adding each variable to be tested with an entry requirement of p < 0.05 and a loss of significance at p > 0.10. Regression residuals were ensured to be normally distributed. Errors due to multiple testing were corrected for using the bonferroni method. Four multiple linear regression models were built to evaluate the effects of i) age, gender, psychosis severity (CGI-S), alcohol intake and smoking ii) drug treatment and iii) metabolic factors on mtDNAcnres. Model 1 was as follows: mtDNAcnres = b0 + b1 (age) + b2 (gender) + b3 (CGI) + b4 (smoking) + b5 (alcohol) + b6 (psychiatric diagnosis). The second model looking at the effect of antipsychotic drugs and mood stabilizers on mtDNAcnres was as follows: mtDNAcnres = b0 + b1 (age) + b2 (gender) + b3 (psychiatric diagnosis) + b4 (mood stabilizer) + bn (drug), where (drug) represents the patient’s treatment [yes/no] with any of n = 11 different antipsychotics. The mood stabilizer variable represents the presence of any mood stabilizer [yes/no] as more detailed information was not available. The numbers of patients on each drug and on any mood stabilizer are listed in Table 1. The mtDNAcnres of patients using a drug significant in model 2 were, for confirmation, compared to that of the all other patients using Mann-Whitney U test. The effect of clozapine and risperidone treatment on mtDNAcnres was further investigated by calculating Spearman’s correlation coefficient, ρ, between the prescribed daily drug dose and the mtDNAcnres. To compare the effects of CGI-S with antipsychotic drug treatment effects we imported the significant variables from the model 1 and 2 to a third regression model. The equation of model 3 was as follows: mtDNAcnres = b0 + b1 (proportion of life on antipsychotic treatment) + b2 (CGI) + b3 (age). This model was separately run on patients who were treated with clozapine or risperidone (model 3a, n = 139) and patients who were not on risperidone and clozapine (model 3b, n = 348). The fourth model (metabolic profile) which analyzed the effect of metabolic factors was adjusted for significant predictors of mtDNAcnres obtained from model 3. Model 4a was mtDNAcnres = b0 + b1 (age) + b2 (proportion of life on antipsychotic treatment) + b3 (gender) + b4 (waist) + b5 (LDL) + b6 (HDL) + b7 (glucose) + b8 (Log10HOMA-IR) + b9 (high BP); and model 4b was mtDNAcnres = b0 + b1 (age) + b2 (CGI) + b3 (gender) + b4 (waist) + b5 (LDL) + b6 (HDL) + b7 (glucose) + b8 (Log10HOMA-IR) + b9 (high BP). Model 4a was run on patients who were treated with clozapine and risperidone (n = 123) and model 4b was run on patients who were not on risperidone and clozapine (n = 324). A sensitivity analysis of the Models 1, 2, 3 and 4 was performed in the patients with a diagnosis of schizophrenia. Output model indices and lack of multi-collinearity between input variables were confirmed using standard multiple linear regression (the enter method), including all input variables. Analyses were performed using IBM Statistical Package for the Social Sciences version 23, (IBM Corporation, USA). Power calculations were performed using http://biomath.info/power/ttest.htm.
Results
As previously reported we found that whole blood mtDNAcn was significantly influenced by platelet and leukocyte counts (βplatelets = 0.119, p = 0.005, and βleukocytes = −0.298, p < 0.001). A regression of whole blood mtDNAcn on the platelet to leukocyte count ratio (platelet/leukocyte) was performed to generate normally distributed unstandardized residuals (mtDNAcnres) which were used in the following analyses as a dependent variable (Supplementary Fig. S3).
The clinical characteristics of the psychosis patients are shown in Tables 1 and 2. The psychiatric diagnoses within the psychosis patient cohort were SZ, schizoaffective disorder, delusional disorder, psychosis unspecified, BD and other disorders with psychotic features. The effect of diagnosis on mtDNAcnres was evaluated using an analysis of covariance (ANCOVA) correcting for covariates suggested to influence mtDNAcnres, i.e. age, gender, smoking and alcohol intake. No significant difference in mtDNAcnres was observed between the six diagnosis groups (p = 0.212). Nonetheless, in subsequent regression analyses (Models 1, 2, 3 and 4) of the psychosis patients, adjustment was made for psychiatric diagnosis, in addition to age and gender, to exclude detectable confounding. Moreover, a sensitivity analysis in only those with a SZ diagnosis (n = 306) replicated the findings in Models 1–4 of the full psychosis cohort (Supplementary Table S1).
Clinical Profile (Model 1): mtDNA copy number was associated with psychosis severity (CGI-S)
Association between mtDNAcnres and severity of psychotic illness, the latter indicated by the clinician-rated CGI-S score, was assessed. A multiple linear regression model including the predictors: age, gender, CGI, smoking, alcohol, psychiatric diagnosis, returned the variables age and CGI as significant predictors of mtDNAcnres (adjusted R2 = 0.038, F = 10.7, p < 0.001, n = 497). Increasing age and psychosis severity (CGI-S) were associated with a decreased mtDNAcnres (age: βstandardized = −0.142, t = −3.20, p < 0.001; CGI: βstandardized = −0.128, t = −2.90, p = 0.004) (Table 3). A linear relationship between mtDNAcnres and CGI-S was observed (Spearman’s correlation coefficient ρ = −0.152, p = 0.0006, n = 507, Fig. 1a), and between mtDNAcnres and age (Spearman’s ρ = −0.188, p < 0.001).
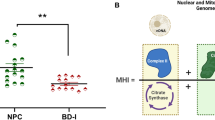
(a) mtDNAcnres was negatively correlated with Clinical Global Impression - Severity (CGI-S) score (Spearman’s ρ = −0.152, p = 0.0006, n = 507). (b) mtDNAcnres correlated with the prescribed daily dose of clozapine (Spearman’s ρ = −0.351, p = 0.006, n = 61). (c) mtDNAcnres correlated with the prescribed daily dose of risperidone (Spearman’s ρ = −0.233 p = 0.026, n = 91). (d) Clozapine treatment, at 0.075 μM there was a 16% reduction in mtDNA copy number compared to vehicle treated cells (p = 0.0005), and at 0.75 μM there was a 25% reduction in mtDNA compared to vehicle treated cells (p = 0.0004). Risperidone treatment, at 0.025 μM there was no change in mtDNA copy number compared to vehicle treated cells, whereas at 0.25 μM there was a 14% reduction in mtDNA copy number compared to vehicle treated cells (p = 0.0126). Error bars indicate standard error. R.Q.: relative quantification (mtDNA copy number). *p < 0.05; ***p < 0.001.
Treatments (Model 2): Clozapine and risperidone treatments were associated with decreased mtDNA copy number
The effect of antipsychotics on mtDNAcnres was assessed using multiple linear regression modelling including the variables age, gender, psychiatric diagnosis, presence of any mood stabilizer [yes/no] and the different antipsychotic drugs [yes/no]. Age, clozapine and risperidone were significant predictors of mtDNAcnres (adjusted R2 = 0.064, F = 9.61, p < 0.001, n = 504). Age, clozapine and risperidone were associated with decreased mtDNAcnres (age: βstandardized = −0.210, t = −4.74, p < 0.001, clozapine: βstandardized = −0.110, t = −2.52, p = 0.012, risperidone: βstandardized = −0.109, t = −2.48, p = 0.014) (Table 3). To confirm the difference in mtDNAcnres for clozapine and risperidone treatment groups compared to patients not on these treatments non-parametric Mann-Whitney U tests were performed. Both the clozapine and risperidone patient groups showed a significantly reduced level of mtDNAcnres (clozapine: p = 0.022 and risperidone: p = 0.005). Furthermore, clozapine and risperidone daily oral treatment doses correlated with mtDNAcnres (clozapine: Spearman’s ρ = −0.351, p = 0.006; risperidone: Spearman’s ρ = −0.233, p = 0.026, Fig. 1b,c). As expected, there was no correlation for any of the other antipsychotic drugs with mtDNAcnres corrected for age (Spearman’s |ρ| < 0.074, p > 0.085).
Psychosis severity and proportion of life on antipsychotic treatment (Model 3): The effect of clozapine and risperidone treatment duration superseded the effect of psychosis severity on mtDNA copy number
Since there was an association for clozapine and risperidone treatment to mtDNAcnres, we assessed the effect of proportion of life on antipsychotic treatment, compared to the effect of psychosis severity (CGI-S) and age detected in model 1. First, proportion of life on treatment correlated with CGI-S to a similar extent for both groups of patients (those on clozapine or risperidone: Spearman’s ρ = 0.258, p = 0.002, n = 140; those patients not on clozapine or risperidone: ρ = 0.234, p < 0.001, n = 349; Supplementary Fig. 4A and B), with relatively small effect sizes in both subgroups (β = 0.248 and 0.251 respectively). Second, we compared the effect on mtDNAcnres by psychosis severity (CGI-S), age and the proportion of life on treatment. For those patients on clozapine and risperidone the model (3a) explained 4.7% of the variance in mtDNAcnres (adjusted R2 = 0.047, F = 7.70, p = 0.006, n = 136, with proportion of life on treatment being the single predictor (βstandardized = −0.232, t = −2.78, p = 0.006, n = 136). However, for the patients who were not on risperidone or clozapine, the model (3b) explained 4.2% of the variance, age and CGI-S were the only significant predictors: adjusted R2 = 0.042, F = 8.46, p < 0.001, n = 340; age: βstandardized = −0.159, t = −2.97, p = 0.003 and CGI-S: βstandardized = −0.129, t = −2.41, p = 0.017 (Table 3); thus the proportion of life on treatment did not additionally explain variance in mtDNAcnres.
The association of mtDNA with metabolic profile (Model 4)
mtDNAcnres was tested for association with the metabolic profile of patients as described by the variables waist circumference, fasting blood levels of LDL, HDL, glucose, log10HOMA-IR and presence of high BP. The multiple linear regression model to identify potential metabolic predictors of mtDNAcnres was corrected for the variables detected to influence mtDNAcnres in models 3a and 3b. Therefore, modelling for those on clozapine or risperidone was adjusted for the proportion of life on treatment (model 4a) whereas the model for the patients not on clozapine or risperidone included age and CGI-S (model 4b). Model 4a (adjusted R2 = 0.039, F = 5.93, p = 0.016), returned proportion of life on treatment as a significant predictor of mtDNAcnres variance (βstandardized = −0.215, t = −2.44, p = 0.016), where metabolic variables did not explain any variance of mtDNAcnres. Model 4b (adjusted R2 = 0.055, F = 7.13, p < 0.001), returned the significant variables age (βstandardized = −0.173, t = −3.17, p = 0.002) and CGI-S (βstandardized = −0.113, t = −2.07, p = 0.040) and LDL (βstandardized = −0.119, t = −2.19, p = 0.029) (Table 3). There was no association between presence of MetS and mtDNAcnres (Mann-Whitney U test: p = 0.130).
Antipsychotic drug effects on mtDNA copy number in human neurons in vitro
To assess the effect of clozapine and risperidone on neurons, human neurons generated in vitro from NESCs were exposed for 7 days to clozapine (0.075 μM and 0.75 μM) or risperidone (0.025 μM and 0.25 μM). For clozapine treatment, at 0.075 μM, there was a 16% reduction in mtDNA copy number compared to vehicle treated cells (p = 0.0005), and at 0.75 μM, the corresponding reduction was 25% (p = 0.0004) (Fig. 1d). For risperidone treatment, at 0.025 μM there was no change in mtDNA copy number compared to vehicle treated cells, but at 0.25 μM, there was a 14% reduction in mtDNA copy number compared to vehicle treated cells (p = 0.0126) (Fig. 1d). Thus, risperidone was found to have a reducing effect on mtDNA copy number at a concentration simulating the clinical target level in plasma but not at the concentration simulating CSF or brain interstitial target level. Clozapine was found to be associated with reduced mtDNA copy number at both doses, in a dose dependent manner. Higher doses of anti-psychotic drugs (clozapine, 75 μM and risperidone, 25 μM) were associated with massive neuronal cell death (data not shown).
Discussion
From a neuroanatomical point of view, a much reviewed discrepancy between SZ and healthy controls are aberrations in dendritic spine morphology. These have been observed in the cortical layers of SZ patients with concomitant increases in the molecular signatures of mitochondrial dysfunction89,90. Interestingly, compelling evidence exists to explain the link between mitochondrial dysfunction and aberrations in dendritic spine morphology as mitochondria play salient roles in dendritic spine architecture and neuronal processes which affect crucial cortical circuitry91,92. Mitochondrial dysfunction and oxidative stress in both brain and leukocytes are overrepresented in not only SZ but also BD type I23,26,44,93. There is a link between mitochondrial dysfunction and psychosis-like symptoms53,94, and mitochondrial dysfunction is reported to be intrinsic to the complex etiology of SZ89. Oxidative stress induced in dysfunctional mitochondria can cause deletions of mtDNA, and influence mitochondrial biogenesis36. A few studies have utilized mtDNA copy number analysis to investigate mitochondrial dysfunction and reported reduced whole blood or leukocyte mtDNA copy number in SZ and BD type I compared to healthy controls10,43,44.
Similarly, the present study was performed to further explore whole blood mtDNA copy number, adjusted for platelet to leukocyte count ratio, in psychosis by focusing on effects of disease severity, antipsychotic drug treatment and metabolic comorbidity. The main findings of this study were that (i) mtDNA copy number was reduced with increasing psychosis severity, and (ii) the antipsychotic drugs clozapine and risperidone decreased mtDNA copy number in patient blood with similar effects on human neurons in vitro in a dose dependent manner. While this has not previously been reported, clozapine, risperidone and other antipsychotic drugs are known to be toxic to mitochondria in various transformed cell lines (neuroblastoma, adipocytes, myoblasts, hepatocytes, lymphoblasts and monocytes) in vitro64,89 and in rodent brain95. Accordingly, we found reduced whole blood mtDNA copy number in psychosis patients treated with clozapine and risperidone compared to psychosis patients treated with or without other antipsychotics. We also showed an inverse correlation between prescribed oral drug dosage and mtDNA copy number. The proportion of life on antipsychotic treatment was a significant predictor of mtDNA copy number variance only in the subset of patients who were treated with clozapine and risperidone.
For patients not on clozapine or risperidone, decreasing mtDNA copy number was associated with increasing age and psychosis severity measured by the CGI-S (n = 348). Existing literature from studies of healthy individuals and non-psychotic post mortem studies support our finding that mtDNA copy number is reduced with advancing age96,97,98. Where psychotic features are of concern, conclusions along a similar grain were made by Li et al.10, who reported reduced whole blood mtDNA copy number in first-episode drug-naïve SZ patients (n = 137) compared to healthy controls and a trend for reduced mtDNA copy number to be associated with positive symptoms in SZ patients (p = 0.07). Two other studies which considered BD patients found reduced leukocyte mtDNA copy number in euthymic BD-I patients compared to BD-II and healthy controls43,44.
The findings linking psychosis with mtDNA copy number are bolstered by previous human post mortem studies where the number of mitochondria per tissue volume was found to be significantly decreased in oligodendrocytes of prefrontal cortex and caudate nucleus of SZ patients23. Mitochondrial density in the neuropils were significantly reduced in the caudate nucleus and putamen of SZ subjects compared to controls93,99. Moreover, psychotic positive symptoms, such as hallucinations, have been reported in subjects with mitochondrial disease94, and a high degree of mitochondrial myopathy encephalopathy lactic acidosis and stroke-like (MELAS) episodes have been reported in SZ and BD31.
To explore if the effects of clozapine and risperidone on mtDNA copy number in blood cells could also be detected in human neurons, we treated NESC-derived human neurons with clozapine and risperidone. We found that the effect was dose dependent at drug concentrations corresponding to target CSF levels during therapy84,100. Clozapine had a stronger effect than risperidone on mtDNA copy number at drug levels which simulate CSF or brain interstitial target levels. At clinical target plasma concentrations, there was a significant decrease (estimated at 15–25% reduction) in mtDNA copy number in the neurons exposed to any of the two drugs. These findings are supported by several studies that have shown that antipsychotics (clozapine, risperidone, haloperidol, olanzapine, quetiapine, chlorpromazine, and thiothixene) can inhibit the mitochondrial respiratory chain and cause further damage to mitochondria through oxidative stress95,101,102, however, the effect on mtDNA copy number was not previously studied. We detected an effect by only clozapine and risperidone but had a statistical power corresponding to 80% to detect an effect similar to that of risperidone for those drugs with a sample size of above 40 (that is haloperidol, olanzapine, zuclopenthixol, aripiprazole, perphenazine, risperidone and ziprasidone). Thus, we did not confirm a previously reported mitochondrial effect for haloperidol and olanzapine. An important limitation of this study is that while the total length of antipsychotic drug treatment was known, the specific antipsychotic drug names were available only for the antipsychotic drug treatment at sampling, and not historically. However, using prospective data starting at sampling we estimate that approximately 10% switched to another antipsychotic drug in a year. If mtDNA copy number depletion and accelerated cellular ageing occur as a result of these antipsychotic treatments, further investigation on mitochondria dysfunction as mediator between antipsychotics and associated comorbidities may be warranted. Another limitation is that the type of mood stabilizers used, in the 11% of patient cohort who were treated with them, was unknown. Amongst mood stabilizers, lithium has been shown to have beneficial effects on mitochondria through enhanced oxidative phosphorylation103 and restoring defunct vacuolated mitochondria to their healthy baseline structure104. A reduction of mtDNA observed in lithium treated C. elegans with increased longevity, a finding going against the grain of understanding that a reduction of mtDNA signals cellular ageing, which was possibly explained by increasingly efficient mitochondrial bioenergetics105. Valproic acid, similarly has been reported to enhance mitochondrial biogenesis, accompanied with an increase in mtDNA copy number in hepatocytes106. Conversely lamotrigine an anti-convulsant and mood stabilizer used in more acute cases was reported to have toxic effects on mitochondria107.
Metabolic comorbidity and inflammation are gaining ground as bona-fide hallmarks of psychotic disorders4. It has been previously reported that metabolic syndrome per se is associated with a reduced mtDNA copy number65. We detected an association for blood mtDNA copy number to level of LDL, similarly strong as that to CGI-S in the psychosis patients not on clozapine or risperidone. The effect of metabolic syndrome on mtDNA copy number and mitochondrial functionality could be enhanced and mediated by systemic inflammation108. Therefore, a limitation of the present study is the lack of quantified inflammatory markers.
We adjusted the mtDNAcn for platelet to leukocyte ratio, but not for subpopulations of leukocytes as their counts were unavailable. While we cannot exclude that our observations might be due to changes in relative WBC subpopulation ratios, existing literature suggests that in a large patient group, total WBC count and platelet count capture the relevant information we need to correct for when making conclusions on changes in peripheral mtDNA69,70,109. Variation between subpopulations are rarely accounted for in mtDNAcn analyses. The mtDNA copy number variance explained by significant predictors was low, 4–6%. However, this is comparable with previous studies investigating the relationship between psychiatric disorders and cellular ageing markers (depression and telomere length)110,111,112. Several association tests were performed which requires correction for multiple testing. However, the regression model reported (models 1, 2 and 4 (model 3 building on 1 and 2)) were designed to test individual hypotheses. Within each model, the findings we report passed a multiple testing correction according to Bonferroni.
The focus of our study was to investigate the relationship between mtDNA copy number, psychosis severity and antipsychotic drug treatment in a psychosis outpatient clinic setting. Here the appropriate controls would have been anti-psychotic drug treatment naïve psychosis patients. However, in the Swedish healthcare setting patients who are diagnosed with the schizophrenia spectrum of disorders are always offered treatment. Therefore we were not able to obtain material from age and gender matched drug-naïve patients. A further limitation is that our study lacks healthy controls, however, previous comparisons performed have reported mtDNA copy number to be reduced in anti-psychotic treatment naïve patients of psychotic disorders (SZ and BD-I) compared to healthy controls10,43,44.
The patient group in our study belongs to multiple DSM-IV-based diagnostic categories, but all patients showed symptoms of severe psychosis and experienced impaired functionality. A unifying criteria of the study cohort was that, all patients were recruited from specialist psychosis outpatient clinics in Sweden, where they received anti-psychotic treatment, unless refused. Our decision to include data from all psychosis patients regardless of diagnoses is in accordance with the Research Domain Criteria (RDoC) paradigm. The RDoC is based on domains of human behavior and functionality e.g cognitive impairment in the presence of psychotic symptoms113. The presence of psychotic symptoms are relevant to the cognitive systems domain of the RDoC matrix, regardless of the DSM-IV criteria based diagnosis114.
To further address the heterogeneity of the patient cohort from the DSM-IV perspective we performed a sensitivity analysis by repeating linear modelling on the subset of the patients who had a SZ diagnosis. The main findings of the study were well replicated in the SZ cohort. Furthermore, we found no statistically significant effect of the DSM-IV-based diagnoses mtDNA copy number levels, even if this may have been due to a limited sample size within certain diagnostic groups i.e BD or delusion. In place of a symptom severity scale such as the positive and negative symptom scale (PANSS), which was unavailable in this study, we used the clinician-rated CGI-S, an indication of the patients’ mental well-being, which has a significant overlap (21–60%) with PANSS115. The present study is limited by the unavailability of a validated symptom severity measure for psychotic cohorts, such as PANSS, in view of the heterogeneity of the patient cohort.
In conclusion, the present study describes a whole blood mtDNA copy number reduction with increasing psychosis severity, potentially driven by the use of antipsychotic drugs in those treated with clozapine and risperidone. The drug-dosage dependent reduction by clozapine and risperidone was present in both whole blood and human neurons after in vitro exposure. Our novel findings support earlier studies that reported mtDNA copy number reduction in blood from SZ and BD-I patients. However, before whole blood mtDNA copy number can be evaluated as a possible biomarker of psychosis or its progression, e.g. reflect psychosis-intrinsic mitochondrial changes, further research is required to estimate the relative contribution of other antipsychotic drugs and comorbidities to the whole blood mtDNA copy number.
Data Availability Statement
The authors report no biomedical financial interests, non-financial interests or other competing interests. The authors adhere to the data availability policy of Scientific Reports.
Change history
05 November 2019
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Association, A. P. Diagnostic and Statistical Manual of Mental Disorders. 4th Ed (1994).
Jindal, R., MacKenzie, E. M., Baker, G. B. & Yeragani, V. K. Cardiac risk and schizophrenia. J Psychiatry Neurosci 30, 393–395 (2005).
Muller, N., Weidinger, E., Leitner, B. & Schwarz, M. J. The role of inflammation in schizophrenia. Front Neurosci 9, 372, https://doi.org/10.3389/fnins.2015.00372 (2015).
Vancampfort, D. et al. A meta-analysis of cardio-metabolic abnormalities in drug naive, first-episode and multi-episode patients with schizophrenia versus general population controls. World Psychiatry 12, 240–250, https://doi.org/10.1002/wps.20069 (2013).
Fraguas, D., Diaz-Caneja, C. M., Rodriguez-Quiroga, A. & Arango, C. Oxidative Stress and Inflammation in Early Onset First Episode Psychosis: A Systematic Review and Meta-Analysis. Int J Neuropsychopharmacol 20, 435–444, https://doi.org/10.1093/ijnp/pyx015 (2017).
Boskovic, M., Vovk, T., Kores Plesnicar, B. & Grabnar, I. Oxidative stress in schizophrenia. Curr Neuropharmacol 9, 301–312, https://doi.org/10.2174/157015911795596595 (2011).
Correll, C. U., Lencz, T. & Malhotra, A. K. Antipsychotic drugs and obesity. Trends Mol Med 17, 97–107, https://doi.org/10.1016/j.molmed.2010.10.010 (2011).
Sahin, E. & DePinho, R. A. Axis of ageing: telomeres, p53 and mitochondria. Nat Rev Mol Cell Biol 13, 397–404, https://doi.org/10.1038/nrm3352 (2012).
Sahin, E. et al. Telomere dysfunction induces metabolic and mitochondrial compromise. Nature 470, 359–365, https://doi.org/10.1038/nature09787 (2011).
Li, Z. et al. Association of telomere length and mitochondrial DNA copy number with risperidone treatment response in first-episode antipsychotic-naive schizophrenia. Sci Rep 5, 18553, https://doi.org/10.1038/srep18553 (2015).
Tyrka, A. R. et al. Alterations of Mitochondrial DNA Copy Number and Telomere Length With Early Adversity and Psychopathology. Biol Psychiatry 79, 78–86, https://doi.org/10.1016/j.biopsych.2014.12.025 (2016).
Kowaltowski, A. J., de Souza-Pinto, N. C., Castilho, R. F. & Vercesi, A. E. Mitochondria and reactive oxygen species. Free Radic Biol Med 47, 333–343, https://doi.org/10.1016/j.freeradbiomed.2009.05.004 (2009).
Wang, C. H., Wu, S. B., Wu, Y. T. & Wei, Y. H. Oxidative stress response elicited by mitochondrial dysfunction: implication in the pathophysiology of aging. Exp Biol Med (Maywood) 238, 450–460, https://doi.org/10.1177/1535370213493069 (2013).
Cunha-Oliveira, T. et al. Mitochondrial dysfunction and caspase activation in rat cortical neurons treated with cocaine or amphetamine. Brain Res 1089, 44–54, https://doi.org/10.1016/j.brainres.2006.03.061 (2006).
Ryter, S. W. et al. Mechanisms of cell death in oxidative stress. Antioxid Redox Signal 9, 49–89, https://doi.org/10.1089/ars.2007.9.49 (2007).
Kim, H. K., Chen, W. & Andreazza, A. C. The Potential Role of the NLRP3 Inflammasome as a Link between Mitochondrial Complex I Dysfunction and Inflammation in Bipolar Disorder. Neural Plast 2015, 408136, https://doi.org/10.1155/2015/408136 (2015).
Naik, E. & Dixit, V. M. Mitochondrial reactive oxygen species drive proinflammatory cytokine production. J Exp Med 208, 417–420, https://doi.org/10.1084/jem.20110367 (2011).
Bhat, A. H. et al. Oxidative stress, mitochondrial dysfunction and neurodegenerative diseases; a mechanistic insight. Biomed Pharmacother 74, 101–110, https://doi.org/10.1016/j.biopha.2015.07.025 (2015).
Lowell, B. B. & Shulman, G. I. Mitochondrial dysfunction and type 2 diabetes. Science 307, 384–387, https://doi.org/10.1126/science.1104343 (2005).
Ongur, D., Prescot, A. P., Jensen, J. E., Cohen, B. M. & Renshaw, P. F. Creatine abnormalities in schizophrenia and bipolar disorder. Psychiatry Res 172, 44–48, https://doi.org/10.1016/j.pscychresns.2008.06.002 (2009).
Stork, C. & Renshaw, P. F. Mitochondrial dysfunction in bipolar disorder: evidence from magnetic resonance spectroscopy research. Mol Psychiatry 10, 900–919, https://doi.org/10.1038/sj.mp.4001711 (2005).
Cataldo, A. M. et al. Abnormalities in mitochondrial structure in cells from patients with bipolar disorder. Am J Pathol 177, 575–585, https://doi.org/10.2353/ajpath.2010.081068 (2010).
Uranova, N. et al. Electron microscopy of oligodendroglia in severe mental illness. Brain Res Bull 55, 597–610 (2001).
Uranova, N. et al. The ultrastructure of lymphocytes in schizophrenia. World J Biol Psychiatry 8, 30–37, https://doi.org/10.1080/15622970600960207 (2007).
Kato, T., Kunugi, H., Nanko, S. & Kato, N. Association of bipolar disorder with the 5178 polymorphism in mitochondrial DNA. Am J Med Genet 96, 182–186 (2000).
Kato, T., Stine, O. C., McMahon, F. J. & Crowe, R. R. Increased levels of a mitochondrial DNA deletion in the brain of patients with bipolar disorder. Biol Psychiatry 42, 871–875, https://doi.org/10.1016/S0006-3223(97)00012-7 (1997).
Kato, T., Kunugi, H., Nanko, S. & Kato, N. Mitochondrial DNA polymorphisms in bipolar disorder. J Affect Disord 62, 151–164 (2001).
Amar, S. et al. Mitochondrial DNA HV lineage increases the susceptibility to schizophrenia among Israeli Arabs. Schizophr Res 94, 354–358, https://doi.org/10.1016/j.schres.2007.04.020 (2007).
Quiroz, J. A., Gray, N. A., Kato, T. & Manji, H. K. Mitochondrially mediated plasticity in the pathophysiology and treatment of bipolar disorder. Neuropsychopharmacology 33, 2551–2565, https://doi.org/10.1038/sj.npp.1301671 (2008).
Ueno, H. et al. Analysis of mitochondrial DNA variants in Japanese patients with schizophrenia. Mitochondrion 9, 385–393, https://doi.org/10.1016/j.mito.2009.06.003 (2009).
Shao, L. et al. Mitochondrial involvement in psychiatric disorders. Ann Med 40, 281–295, https://doi.org/10.1080/07853890801923753 (2008).
Rollins, B. et al. Mitochondrial variants in schizophrenia, bipolar disorder, and major depressive disorder. PLoS One 4, e4913, https://doi.org/10.1371/journal.pone.0004913 (2009).
Munakata, K., Iwamoto, K., Bundo, M. & Kato, T. Mitochondrial DNA 3243A > G mutation and increased expression of LARS2 gene in the brains of patients with bipolar disorder and schizophrenia. Biol Psychiatry 57, 525–532, https://doi.org/10.1016/j.biopsych.2004.11.041 (2005).
Munakata, K. et al. Mitochondrial DNA 3644T– >C mutation associated with bipolar disorder. Genomics 84, 1041–1050, https://doi.org/10.1016/j.ygeno.2004.08.015 (2004).
Kim, J. H., Kim, H. K., Ko, J. H., Bang, H. & Lee, D. C. The relationship between leukocyte mitochondrial DNA copy number and telomere length in community-dwelling elderly women. PLoS One 8, e67227, https://doi.org/10.1371/journal.pone.0067227 (2013).
Lee, H. C. & Wei, Y. H. Mitochondrial biogenesis and mitochondrial DNA maintenance of mammalian cells under oxidative stress. Int J Biochem Cell Biol 37, 822–834, https://doi.org/10.1016/j.biocel.2004.09.010 (2005).
Bratic, A. & Larsson, N. G. The role of mitochondria in aging. J Clin Invest 123, 951–957, https://doi.org/10.1172/JCI64125 (2013).
Malik, A. N. & Czajka, A. Is mitochondrial DNA content a potential biomarker of mitochondrial dysfunction? Mitochondrion 13, 481–492, https://doi.org/10.1016/j.mito.2012.10.011 (2013).
Masayesva, B. G. et al. Mitochondrial DNA content increase in response to cigarette smoking. Cancer Epidemiol Biomarkers Prev 15, 19–24, https://doi.org/10.1158/1055-9965.EPI-05-0210 (2006).
Beekman, M., Dowling, D. K. & Aanen, D. K. The costs of being male: are there sex-specific effects of uniparental mitochondrial inheritance? Philos Trans R Soc Lond B Biol Sci 369, 20130440, https://doi.org/10.1098/rstb.2013.0440 (2014).
Tang, C. et al. Changes in mitochondrial DNA and its encoded products in alcoholic cirrhosis. Int J Clin Exp Med 5, 245–250 (2012).
Tyrka, A. R. et al. Association of telomere length and mitochondrial DNA copy number in a community sample of healthy adults. Exp Gerontol 66, 17–20, https://doi.org/10.1016/j.exger.2015.04.002 (2015).
Chang, C. C., Jou, S. H., Lin, T. T. & Liu, C. S. Mitochondrial DNA variation and increased oxidative damage in euthymic patients with bipolar disorder. Psychiatry Clin Neurosci 68, 551–557, https://doi.org/10.1111/pcn.12163 (2014).
de Sousa, R. T. et al. Leukocyte mitochondrial DNA copy number in bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 48, 32–35, https://doi.org/10.1016/j.pnpbp.2013.09.002 (2014).
Cai, N. et al. Molecular signatures of major depression. Curr Biol 25, 1146–1156, https://doi.org/10.1016/j.cub.2015.03.008 (2015).
Lin, P. I. & Mitchell, B. D. Approaches for unraveling the joint genetic determinants of schizophrenia and bipolar disorder. Schizophr Bull 34, 791–797, https://doi.org/10.1093/schbul/sbn050 (2008).
Thaker, G. K. Neurophysiological endophenotypes across bipolar and schizophrenia psychosis. Schizophr Bull 34, 760–773, https://doi.org/10.1093/schbul/sbn049 (2008).
Heckers, S. et al. Differential hippocampal expression of glutamic acid decarboxylase 65 and 67 messenger RNA in bipolar disorder and schizophrenia. Arch Gen Psychiatry 59, 521–529 (2002).
Post, R. M. Comparative pharmacology of bipolar disorder and schizophrenia. Schizophr Res 39, 153–158; discussion 163 (1999).
Craddock, N., O’Donovan, M. C. & Owen, M. J. The genetics of schizophrenia and bipolar disorder: dissecting psychosis. J Med Genet 42, 193–204, https://doi.org/10.1136/jmg.2005.030718 (2005).
Berrettini, W. Evidence for shared susceptibility in bipolar disorder and schizophrenia. Am J Med Genet C Semin Med Genet 123C, 59–64, https://doi.org/10.1002/ajmg.c.20014 (2003).
Berrettini, W. H. Susceptibility loci for bipolar disorder: overlap with inherited vulnerability to schizophrenia. Biol Psychiatry 47, 245–251 (2000).
Prayson, R. A. & Wang, N. Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS) syndrome: an autopsy report. Arch Pathol Lab Med 122, 978–981 (1998).
Clay, H. B., Sillivan, S. & Konradi, C. Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int J Dev Neurosci 29, 311–324, https://doi.org/10.1016/j.ijdevneu.2010.08.007 (2011).
Regenold, W. T. et al. Elevated cerebrospinal fluid lactate concentrations in patients with bipolar disorder and schizophrenia: implications for the mitochondrial dysfunction hypothesis. Biol Psychiatry 65, 489–494, https://doi.org/10.1016/j.biopsych.2008.11.010 (2009).
Campos, Y. et al. Mitochondrial myopathy, cardiomyopathy and psychiatric illness in a Spanish family harbouring the mtDNA 3303C > T mutation. J Inherit Metab Dis 24, 685–687 (2001).
Fattal, O., Budur, K., Vaughan, A. J. & Franco, K. Review of the literature on major mental disorders in adult patients with mitochondrial diseases. Psychosomatics 47, 1–7, https://doi.org/10.1176/appi.psy.47.1.1 (2006).
Grover, S. et al. Mania as a first presentation in mitochondrial myopathy. Psychiatry Clin Neurosci 60, 774–775, https://doi.org/10.1111/j.1440-1819.2006.01599.x (2006).
Mancuso, M. et al. Autosomal dominant psychiatric disorders and mitochondrial DNA multiple deletions: report of a family. J Affect Disord 106, 173–177, https://doi.org/10.1016/j.jad.2007.05.016 (2008).
Leucht, S. et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 382, 951–962, https://doi.org/10.1016/S0140-6736(13)60733-3 (2013).
Riordan, H. J., Antonini, P. & Murphy, M. F. Atypical antipsychotics and metabolic syndrome in patients with schizophrenia: risk factors, monitoring, and healthcare implications. Am Health Drug Benefits 4, 292–302 (2011).
Alberti, K. G., Zimmet, P. & Shaw, J. Metabolic syndrome–a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23, 469–480, https://doi.org/10.1111/j.1464-5491.2006.01858.x (2006).
McElroy, S. L. & Keck, P. E. Jr. Metabolic syndrome in bipolar disorder: a review with a focus on bipolar depression. J Clin Psychiatry 75, 46–61, https://doi.org/10.4088/JCP.13r08634 (2014).
Contreras-Shannon, V. et al. Clozapine-induced mitochondria alterations and inflammation in brain and insulin-responsive cells. PLoS One 8, e59012, https://doi.org/10.1371/journal.pone.0059012 (2013).
Huang, C. H. et al. Depleted leukocyte mitochondrial DNA copy number in metabolic syndrome. J Atheroscler Thromb 18, 867–873 (2011).
Anderson, S. et al. Sequence and organization of the human mitochondrial genome. Nature 290, 457–465 (1981).
Urata, M., Koga-Wada, Y., Kayamori, Y. & Kang, D. Platelet contamination causes large variation as well as overestimation of mitochondrial DNA content of peripheral blood mononuclear cells. Ann Clin Biochem 45, 513–514, https://doi.org/10.1258/acb.2008.008008 (2008).
Hurtado-Roca, Y. et al. Adjusting MtDNA Quantification in Whole Blood for Peripheral Blood Platelet and Leukocyte Counts. PLoS One 11, e0163770, https://doi.org/10.1371/journal.pone.0163770 (2016).
Knez, J. et al. Correlates of Peripheral Blood Mitochondrial DNA Content in a General Population. Am J Epidemiol 183, 138–146, https://doi.org/10.1093/aje/kwv175 (2016).
Knez, J. et al. Peripheral blood mitochondrial DNA content in relation to circulating metabolites and inflammatory markers: A population study. PLoS One 12, e0181036, https://doi.org/10.1371/journal.pone.0181036 (2017).
Hukic, D. S. et al. Genetic variants of increased waist circumference in psychosis. Psychiatr Genet 27, 210–218, https://doi.org/10.1097/YPG.0000000000000181 (2017).
Kumar, P. et al. Plasma GDF15 level is elevated in psychosis and inversely correlated with severity. Sci Rep 7, 7906, https://doi.org/10.1038/s41598-017-07503-2 (2017).
Busner, J. & Targum, S. D. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 4, 28–37 (2007).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Lindblom, B. & Holmlund, G. Rapid DNA purification for restriction fragment length polymorphism analysis. Gene Anal Tech 5, 97–101 (1988).
Rooney, J. P. et al. PCR based determination of mitochondrial DNA copy number in multiple species. Methods Mol Biol 1241, 23–38, https://doi.org/10.1007/978-1-4939-1875-1_3 (2015).
Venegas, V. & Halberg, M. C. Measurement of mitochondrial DNA copy number. Methods Mol Biol 837, 327–335, https://doi.org/10.1007/978-1-61779-504-6_22 (2012).
Bai, R. K. & Wong, L. J. Simultaneous detection and quantification of mitochondrial DNA deletion(s), depletion, and over-replication in patients with mitochondrial disease. J Mol Diagn 7, 613–622, https://doi.org/10.1016/S1525-1578(10)60595-8 (2005).
Lott, M. T. et al. mtDNA Variation and Analysis Using Mitomap and Mitomaster. Curr Protoc Bioinformatics 44, 1 23 21–26, https://doi.org/10.1002/0471250953.bi0123s44 (2013).
Amberger, J. S., Bocchini, C. A., Schiettecatte, F., Scott, A. F. & Hamosh, A. OMIM.org: Online Mendelian Inheritance in Man (OMIM(R)), an online catalog of human genes and genetic disorders. Nucleic Acids Res 43, D789–798, https://doi.org/10.1093/nar/gku1205 (2015).
Ingman, M. & Gyllensten, U. mtDB: Human Mitochondrial Genome Database, a resource for population genetics and medical sciences. Nucleic Acids Res 34, D749–751, https://doi.org/10.1093/nar/gkj010 (2006).
Falk, A. et al. Capture of neuroepithelial-like stem cells from pluripotent stem cells provides a versatile system for in vitro production of human neurons. PLoS One 7, e29597, https://doi.org/10.1371/journal.pone.0029597 (2012).
Boumba, V. A., Rallis, G., Petrikis, P., Vougiouklakis, T. & Mavreas, V. Determination of clozapine, and five antidepressants in human plasma, serum and whole blood by gas chromatography-mass spectrometry: A simple tool for clinical and postmortem toxicological analysis. J Chromatogr B Analyt Technol Biomed Life Sci 1038, 43–48, https://doi.org/10.1016/j.jchromb.2016.10.023 (2016).
Muly, E. C., Votaw, J. R., Ritchie, J. & Howell, L. L. Relationship between dose, drug levels, and D2 receptor occupancy for the atypical antipsychotics risperidone and paliperidone. J Pharmacol Exp Ther 341, 81–89, https://doi.org/10.1124/jpet.111.189076 (2012).
Riedel, M. et al. Risperidone plasma levels, clinical response and side-effects. Eur Arch Psychiatry Clin Neurosci 255, 261–268, https://doi.org/10.1007/s00406-004-0556-4 (2005).
Liu, S. F. et al. Leukocyte Mitochondrial DNA Copy Number Is Associated with Chronic Obstructive Pulmonary Disease. PLoS One 10, e0138716, https://doi.org/10.1371/journal.pone.0138716 (2015).
Mengel-From, J. et al. Mitochondrial DNA copy number in peripheral blood cells declines with age and is associated with general health among elderly. Hum Genet 133, 1149–1159, https://doi.org/10.1007/s00439-014-1458-9 (2014).
Hocking, R. R. A Biometrics Invited Paper. The Analysis and Selection of Variables in Linear Regression. Biometrics 32, 1–49, https://doi.org/10.2307/2529336 (1976).
Hjelm, B. E. et al. Evidence of Mitochondrial Dysfunction within the Complex Genetic Etiology of Schizophrenia. Mol Neuropsychiatry 1, 201–219, https://doi.org/10.1159/000441252 (2015).
Arion, D. et al. Distinctive transcriptome alterations of prefrontal pyramidal neurons in schizophrenia and schizoaffective disorder. Mol Psychiatry 20, 1397–1405, https://doi.org/10.1038/mp.2014.171 (2015).
Li, Z., Okamoto, K., Hayashi, Y. & Sheng, M. The importance of dendritic mitochondria in the morphogenesis and plasticity of spines and synapses. Cell 119, 873–887, https://doi.org/10.1016/j.cell.2004.11.003 (2004).
Sheng, Z. H. & Cai, Q. Mitochondrial transport in neurons: impact on synaptic homeostasis and neurodegeneration. Nat Rev Neurosci 13, 77–93, https://doi.org/10.1038/nrn3156 (2012).
Somerville, S. M., Lahti, A. C., Conley, R. R. & Roberts, R. C. Mitochondria in the striatum of subjects with schizophrenia: relationship to treatment response. Synapse 65, 215–224, https://doi.org/10.1002/syn.20838 (2011).
Anglin, R. E., Garside, S. L., Tarnopolsky, M. A., Mazurek, M. F. & Rosebush, P. I. The psychiatric manifestations of mitochondrial disorders: a case and review of the literature. J Clin Psychiatry 73, 506–512, https://doi.org/10.4088/JCP.11r07237 (2012).
Burkhardt, C. et al. Neuroleptic medications inhibit complex I of the electron transport chain. Ann Neurol 33, 512–517, https://doi.org/10.1002/ana.410330516 (1993).
Short, K. R. et al. Decline in skeletal muscle mitochondrial function with aging in humans. Proc Natl Acad Sci USA 102, 5618–5623, https://doi.org/10.1073/pnas.0501559102 (2005).
Cree, L. M. et al. Age-related decline in mitochondrial DNA copy number in isolated human pancreatic islets. Diabetologia 51, 1440–1443, https://doi.org/10.1007/s00125-008-1054-4 (2008).
Welle, S. et al. Reduced amount of mitochondrial DNA in aged human muscle. J Appl Physiol (1985) 94, 1479–1484, https://doi.org/10.1152/japplphysiol.01061.2002 (2003).
Roberts, R. C. Postmortem studies on mitochondria in schizophrenia. Schizophr Res, https://doi.org/10.1016/j.schres.2017.01.056 (2017).
Nordin, C., Alme, B. & Bondesson, U. CSF and serum concentrations of clozapine and its demethyl metabolite: a pilot study. Psychopharmacology (Berl) 122, 104–107 (1995).
Modica-Napolitano, J. S., Lagace, C. J., Brennan, W. A. & Aprille, J. R. Differential effects of typical and atypical neuroleptics on mitochondrial function in vitro. Arch Pharm Res 26, 951–959 (2003).
Casademont, J. et al. Neuroleptic treatment effect on mitochondrial electron transport chain: peripheral blood mononuclear cells analysis in psychotic patients. J Clin Psychopharmacol 27, 284–288, https://doi.org/10.1097/JCP.0b013e318054753e (2007).
Maurer, I. C., Schippel, P. & Volz, H. P. Lithium-induced enhancement of mitochondrial oxidative phosphorylation in human brain tissue. Bipolar Disord 11, 515–522, https://doi.org/10.1111/j.1399-5618.2009.00729.x (2009).
Pasquali, L. et al. Autophagy, lithium, and amyotrophic lateral sclerosis. Muscle Nerve 40, 173–194, https://doi.org/10.1002/mus.21423 (2009).
Tam, Z. Y., Gruber, J., Ng, L. F., Halliwell, B. & Gunawan, R. Effects of lithium on age-related decline in mitochondrial turnover and function in Caenorhabditis elegans. J Gerontol A Biol Sci Med Sci 69, 810–820, https://doi.org/10.1093/gerona/glt210 (2014).
Sitarz, K. S. et al. Valproic acid triggers increased mitochondrial biogenesis in POLG-deficient fibroblasts. Mol Genet Metab 112, 57–63, https://doi.org/10.1016/j.ymgme.2014.03.006 (2014).
Finsterer, J. Toxicity of Antiepileptic Drugs to Mitochondria. Handb Exp Pharmacol 240, 473–488, https://doi.org/10.1007/164_2016_2 (2017).
Rajasekaran, A., Venkatasubramanian, G., Berk, M. & Debnath, M. Mitochondrial dysfunction in schizophrenia: pathways, mechanisms and implications. Neurosci Biobehav Rev 48, 10–21, https://doi.org/10.1016/j.neubiorev.2014.11.005 (2015).
Lee, J. et al. The Effect of Clozapine on Hematological Indices: A 1-Year Follow-Up Study. J Clin Psychopharmacol 35, 510–516, https://doi.org/10.1097/JCP.0000000000000387 (2015).
Ridout, K. K., Ridout, S. J., Price, L. H., Sen, S. & Tyrka, A. R. Depression and telomere length: A meta-analysis. J Affect Disord 191, 237–247, https://doi.org/10.1016/j.jad.2015.11.052 (2016).
Lindqvist, D. et al. Psychiatric disorders and leukocyte telomere length: Underlying mechanisms linking mental illness with cellular aging. Neurosci Biobehav Rev 55, 333–364, https://doi.org/10.1016/j.neubiorev.2015.05.007 (2015).
Lin, P. Y., Huang, Y. C. & Hung, C. F. Shortened telomere length in patients with depression: A meta-analytic study. J Psychiatr Res 76, 84–93, https://doi.org/10.1016/j.jpsychires.2016.01.015 (2016).
Ford, J. M. et al. Studying hallucinations within the NIMH RDoC framework. Schizophr Bull 40(Suppl 4), S295–304, https://doi.org/10.1093/schbul/sbu011 (2014).
Insel, T. et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 167, 748–751, https://doi.org/10.1176/appi.ajp.2010.09091379 (2010).
Rabinowitz, J., Mehnert, A. & Eerdekens, M. To what extent do the PANSS and CGI-S overlap? J Clin Psychopharmacol 26, 303–307, https://doi.org/10.1097/01.jcp.0000218407.10362.6e (2006).
Acknowledgements
We are grateful to all patients and research assistant Carina Schmidt. The study was financially supported by a regional accord on medical training and clinical research between Stockholm County Council and Karolinska Institutet, by the Söderström-Königska Foundation. In addition we thank the Swedish Brain Foundation, the Swedish Research Council and the Regional Drug and Therapeutic Committee in Stockholm (Läksak).
Author information
Authors and Affiliations
Contributions
Parvin Kumar (P.K.), Paschalis Esthathopoulos (P.E.), Vincent Millischer (V.M.), Eric Olsson (E.O.), Ya Bin Wei (Y.B.W.), Oliver Brüstle (O.B.), Martin Schalling (M.S.), J. Carlos Villaescusa (C.V.), Urban Ösby (U.Ö.), Catharina Lavebratt (C.L.). Authors P.K., V.M., P.E. and C.L. designed the study. Authors U.Ö., M.S., E.O. organized the patient recruitment, blood sampling, DNA extraction and phenotype collection. Authors V.M. and Y.B.W. optimized mtDNA copy number measurement assay. Author P.K. performed the mtDNA copy number measurements. Authors C.V. and Author O.B. designed and provided material for cell culture experiments. P.K. and P.E. performed cell culture experiments. Authors P.K., V.M. and C.L. undertook the statistical analyses, and authors P.K., V.M., C.V. and C.L. interpreted the results. Author P.K. wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kumar, P., Efstathopoulos, P., Millischer, V. et al. Mitochondrial DNA copy number is associated with psychosis severity and anti-psychotic treatment. Sci Rep 8, 12743 (2018). https://doi.org/10.1038/s41598-018-31122-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-31122-0
This article is cited by
-
Mitochondria DNA copy number, mitochondria DNA total somatic deletions, Complex I activity, synapse number, and synaptic mitochondria number are altered in schizophrenia and bipolar disorder
Translational Psychiatry (2022)
-
Subcortical volume reduction and cortical thinning 3 months after switching to clozapine in treatment resistant schizophrenia
Schizophrenia (2022)
-
Genome-wide analysis of mitochondrial DNA copy number reveals loci implicated in nucleotide metabolism, platelet activation, and megakaryocyte proliferation
Human Genetics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.