Abstract
In this report, Chair Heterogeneity Index (CHI) was introduced to assess the dose heterogeneity inside the target with a boost volume. CHI was defined by dividing (V Rx − V Dl ) by (V Dm − V Dh ): V Rx , V Dl , V Dm and V Dh were four points selected from the target cumulative dose volume histogram curve. The effectiveness of CHI was validated by assessing the treatment plans for nasopharyngeal cancer (NPC, 12 cases), breast cancer after breast-conserving-surgery (BC, 10 cases), and stereotactic radiosurgery after whole brain irradiation (SRS, 9 cases). Our results indicate that both CHI and HI of the target can distinguish Volumetric Modulated Arc Therapy (VMAT) from Intensity Modulated Radiation Therapy (IMRT, p < 0.05) while the mean differences in CHI (NPC 1.16, BC 1.19 and SRS 3.3) were larger than those in HI (NPC 0.03, BC 0.02 and SRS 0.02). In addition, CHI of the combination volume (the target minus the boost) were statistically higher in VMAT than IMRT in all three kinds of cancer. In conclusion, CHI was effective in assessing the dose heterogeneity inside a target containing a boost volume.
Similar content being viewed by others
Introduction
Simultaneously Integrated Boost technique (SIB) is a fractionation scheme for accelerated radiation therapy1. With the advent of intensity modulated radiation therapy (IMRT), SIB has been widely used in radiotherapy of patients with head and neck cancer1,2,3, breast cancer4,5,6, esophageal cancer7, and so on. SIB delivers different doses to different target volumes within a single radiotherapy fraction, which will reduce the overall treatment time and lower the expense of patients6,7,8. Additionally, SIB may be beneficial in term of increased tumor control probability due to an increased fractional dose to the tumor bed4,9. For example, the standard regime of radiotherapy for patients after breast conserving surgery is to irradiate the whole breast (WBI) 45–50 Gy in about 5 weeks, followed by a boost treatment to the tumor bed for additional 10–16 Gy. The entire radiation treatment is 6–7 weeks. But with SIB, the tumor bed boost will be integrated into the WBI and the overall treatment time of radiotherapy is diminished to only 5 weeks. The fractionation dose for tumor bed is also elevated with SIB.
To evaluate the dose homogeneity of radiotherapy plans, homogeneity index (HI)2,7 was widely applied:
where D2, D50 and D98 represent the doses for 2%, 50% and 98% of the target volume, respectively. Meanwhile, D2 and D98 also indicate the maximum and minimum doses received by the target. Smaller HI indicates better homogeneity inside the target volume (HI ≥ 0).
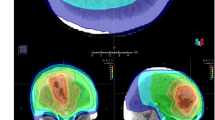
However, the application of HI in evaluating the target homogeneity for SIB would be problematic. When there is a boost volume inside the target, D2 is much higher than D98 due to the two levels of prescription dose (Fig. 1). As a consequence, Chair Heterogeneity Index (CHI) was introduced to characterize the dose homogeneity for a target volume in SIB. In this case, the ideal cumulative dose volume histogram (cDVH) curve for the target is not a vertical line but shapes like an outline of a chair (Fig. 1), which makes the CHI more suitable than HI in describing the dose heterogeneity inside the target. We further validated the effectiveness of CHI and compared it with other heterogeneity indexes.
Materials and Methods
Formula of chair heterogeneity index (CHI)
CHI is defined by:
where D l , D m and D h were reference low dose, medium dose and high dose values selected between the prescription dose (Rx) of the target and of the boost (Fig. 1). Vx was the percent of the target volume received X dose. The selection for reference doses D l , D m , and D h were specified as the following:
The chair-shaped target cumulative DVH curve could be divided into three parts (Fig. 1): the first fall-off, the plateau and the final fall-off:
-
1.
The first fall-off was formed by the doses of the voxels inside the target but a little far from the boost—the high-dose volume. The doses of these voxels were basically free of the influence of the boost. The closer the voxel to the boost, the higher the dose to the voxel. The value of (VRx − VDl) reflects the gradient of the first fall-off of the Target cumulative DVH curve. The higher the value of (VRx − VDl) indicated the steeper the first fall-off of target cumulative DVH curve. Based on the recommendation of the ICRU Report 5010 that the dose coverage of the target be kept within +7% and −5% of the prescribed dose, D l is about 7% higher than the Rx dose for the target.
-
2.
Dm might be set as the mean of the Rx dose values of the main target and the boost. Dm should be in the plateau of the target cDVH curve. The Dm and D l values so selected ensure that VDl be greater than VDm (Fig. 1).
-
3.
Dh is around 5% lower than the prescription dose to boost volume and also based on the recommendation of ICRU Report 5010. The value (V Dm − V Dh ) indicated the slope of the plateau of the target cDVH curve, which reflected the dose conformity around the boost. The gentler the slope of the plateau indicated better dose conformity of the boost. VDh should be less than VDm.
Higher CHI, better dose distribution inside the target (outside the boost volume).
Evaluating the SIB plans with CHI
12 patients with nasopharyngeal cancer (NPC, Stage I or II), 10 cases of whole breast irradiation with SIB after the breast conserving surgery(BC), and 9 cases of brain metastasis accepted stereotactic radiosurgery after whole brain irradiation (SRS) were selected in this study. This study was given IRB approval by the First People’s Hospital of Changzhou. Written informed consent was obtained from the patients before treatment. The methods used were in compliance with the guidelines in the Declaration of Helsinki. Patients were treated using a 6 MV photon with an Axesse® linac (Elekta AB, Stockholm, Sweden). This linac is equipped with a high-definition interdigitation-capable multileaf collimator (160 leaves with a width of 5 mm at isocenter). The image guidance system is comprised of 4D cone-beam computer tomography and XVI software (version 4.5, Elekta AB), and a robotic six-degree-of -freedom patient positioning system (treatment couch HexaPOD with iGuide Software Version 1.1, Medical Intelligence, Schwabmünchen, Germany). The planning CT scan was acquired using a Siemens Somatom® Sensation Open 40-slice CT scanner (Siemens Medical Solutions, Forchheim, Germany). The slice thickness of CT images was 3 mm. The image set was exported to a Monaco Treatment Planning System (Monaco version 3.3, Elekta AB, Stockholm, Sweden) for planning. The plans were designed with two different techniques: IMRT with dynamic multileaf collimator, volumetric modulated arc therapy (VMAT). The prescription protocols for the chosen plans and the specific plan parameters were concisely listed as follows:
SIB plans for whole breast irradiation
-
1.
Boost volume was generated by adding 5 mm to this tumor-bed and cropped 5 mm to the skin contour. The prescription for Boost was 60 Gy/25fractions.
-
2.
Target volume included the glandular breast tissue cropped 5 mm inside to the skin contour. The prescription for it was 50 Gy/25fractions. Target included Boost totally.
For breast SIB plans, D l , D m , D h in CHI were set as 53, 55 and 58 Gy respectively. The techniques for the plans: IMRT with two tangential paired fields, VMAT with a around 230° dual-arc beam (Supplemental Fig. 1). Supplemental Fig. 2 was an example of the plan constraints.
Plans for NPC
-
1.
Boost volume was created with a 5 mm margin on the gross tumor volume (GTV): visible nasopharyngeal neoplasm in the images of MRI and CT, and the lymph node metastasis. The Rx dose for Boost was 70 Gy/33fractions.
-
2.
Target included Boost and all cervical lymph drainage zones. The Rx dose for Target was 60 Gy/33 fractions.
-
3.
For simplifying the study, the low-risk lymph nodes and lymph drainage zones were taken as a part of Target and the Rx dose was 60 Gy.
For NPC plans, D l , D m , D h in CHI were 63, 65 and 68 Gy respectively. The techniques for the plans: IMRT with nine equidistant, coplanar fields, VMAT with one dual-arc beam.
Frameless stereotactic radiosurgery for brain metastases after whole brain irradiation
-
1.
The GTV was the visible brain metastasis in the images of MRI and CT. Boost volume included GTV plus 3 mm margin. The patients enrolled had only one brain metastasis.
-
2.
Target volume was the whole brain plus 3 mm margin.
This was a two-step plan for each patient: Target was irradiated 30 Gy/10 fractions by two parallel opposed lateral fields, and then Boost volume was irradiated 12 Gy a single treatment. The techniques of the plans for SRS: IMRT with five coplanar fields and two non-coplanar fields, VMAT with one arc beam and a partial arc beam with the couch 90° (or 270°).
Target was irradiated first and the SRS plan for Boost was based on the dose of former plan. As a consequence, there was a gradual decrease in the first fall-off of the Target cumulative DVH curve (Fig. 2). D l , D m and D h in CHI were set to be 33, 36, 40 Gy respectively.
STD: Another homogeneity index11
where v i is the ith voxel receiving a dose of D i , and V is the total volume. Here the D i is normalized by taking the Rx dose of the target as 100. DSD represents the standard deviation of the normalized voxel dose. The lower the value of STD represented the better dose homogeneity inside the target.
Statistics
The STD, HI and CHI were calculated for each plan.The data were auto-collected with Macros from both differential and cumulative DVHs. Paired T Test and Pearson correlation test were used in this study.Two sided statistical significance level of P < 0.05 was used. All statistical analyses were performed by using SPSS software (version 13.0, SPSS Inc., Chicago, IL, USA).
Results
Table 1 listed the relations of the volume ratio of Boost to Target (Boost/Target) with V Dl , V Dm and V Dh . The V Dm and V Dh in VMAT plans have good correlations with Boost/Target, but only V Dh in IMRT plans has statistical correlation with Boost/Target (p < 0.05). In SRS plans, all the Pearson linear correlation coefficients were greater than 0.8 between Boost/Target and the parameters V Dl , V Dm and V Dh . The values of Boost/Target, V Dl , V Dm and V Dh of NPC plans were shown in Supplemental Fig. 3.
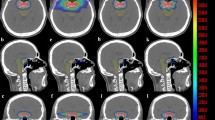
CHI, HI and STD were listed in the Table 2 for NPC plans, BC plans and SRS plans. CHI of the Targets in VMAT plans (NPC, 2.49 ± 1.08, Breast cancer, 3.51 ± 0.9 and SRS, 40.1 ± 12.2) are statistically higher than those in IMRT plans (NPC, 1.33 ± 0.58, Breast cancer, 2.32 ± 1.1 and SRS, 36.2 ± 13.6). This was also clearly shown in Figs 2–5: the Target cDVH curves of VMAT plans were better than those of IMRT plans. It was interesting that HI of the Targets in VMAT plans, like CHI, were better than those in IMRT plans for all three cancers. But the mean differences of HIs were tiny between two kinds of plans (less than 0.03 in NPC, BC and SRS plans). Unfortunately, STD of Target was failed in distinguishing two techniques in NPC as the P value is higher than 0.05 (Table 2).
The statistical analyses of CHI and HI for the combination structure of T-B (Target minus Boost) were similar with those for Targets. The average CHI in T-B was very close to those in Targets, no matter what type of the cancer or the technique. In all three cancers, the differences between them were not greater than 0.01 in both VMAT and IMRT in all three cancers (Table 2).
There were only HI and STD calculated for Boost in three cancers. Table 2 indicated that both indexes are better in VMAT than in IMRT in plans for BC and NPC, but worse in VMAT than IMRT in plans for SRS.
Discussion
There were different target volumes in Radiation Oncology which were clearly defined in The International Commission on Radiation Units and Measurements (ICRU) Report 5010, such as gross tumor volume (GTV), Clinical Target Volume (CTV), planning tumor volume (PTV) and so on. Subclinical microscopic extensions of tumor (SMET) were classified as one kind of CTV. As the hypoxic cancer cells may be less likely in SMET than in bulky tumors (the GTV), SMET should be controlled by a lower dose than is required for GTV12. In this study, Target was the low-dose volume and Boost was the high-dose volume. Target contained the entire Boost.
IMRT, including volumetric modulated arc therapy (VMAT), has the ability to deliver different doses to different volumes at the same time12. This feature makes the implementation of SIB feasible and simple. It has been proven that SIB is better than sequential boost in head and neck cancer, breast cancer, etc2,3,7,9,13,14.
However, owing to the existence of the Boost—high dose volume, we usually overlooked the dose distribution inside the combination structure (Target minus Boost) when evaluating the plan quality of SIB plans.
HI represents the gradient of the target cumulative DVH curve and is a very good index in describing the dose homogeneity in a target volume. However in case there are two prescribed dose levels HI becomes problematic. The high dose tail in the lower dose target elevates the HI value, and insensitive to the qualitative difference in the dose distribution (Table 2 and Fig. 1). For example, Table 2 indicated that VMAT is better than IMRT in the dose homogeneity inside the Boost volume in NPC and BC. The HI values of Boost were around 0.1. But the HI values of Target, the low dose volume which contained the high dose volume Boost, were dramatically up to around 0.25 and higher. The high HI values revealed that the HI may be problematic to assess the dose homogeneity in this case. The HI values of Targets in VMAT technique were statistically better than that in IMRT technique in both NPC and BC, but it might be influenced by the high dose volume (Boost) inside Target.
On the other hand, CHI was designed for this type of target. (V Dl − V Dm ) and (V Dm − V Dh ) represented the gradients of the first fall-off and the plateau of the target cumulative DVH curve, respectively. The higher the (V Dl − V Dm ) and the lower the (V Dm − V Dh ) indicated the better dose distribution inside the target. This also leaded to a high value of CHI.
As shown in the Table 2 and Supplemental Fig. 4, CHI of the Targets in VMAT were significantly higher than that in IMRT and their mean differences were obvious(1.16 for NPC and 1.19 for Breast cancer). On the contrary, for HI, the mean differences between VMAT and IMRT plans were tiny (NPC: 0.03, BC: 0.02). In conclusion, CHI was more sensitive to HI in assessing the dose distribution inside the target containing a boost volume.
In this study we also assessed the dose distribution of plans for SRS for brain metastasis after whole brain irradiation. This type of plans belonged to sequential boost technique. The characteristic of this plan is the rather small volume ratio of Boost to Target (around 1%, Table 1). This was the reason why we chose these patients to verify the efficacy of CHI. It was shown in Table 2 that HI of all volumes, including Target, T-B and Boost, were better in IMRT than in VMAT. But this did not mean that IMRT was superior to VMAT in this condition. CHIs of both Target and T-B were statistically higher in VMAT than in IMRT. And it was obviously shown in Fig. 5 that the dose distribution in VMAT is better than IMRT. It was truth that the dose homogeneity inside Boost in IMRT is better than that in VMAT. However, it was expected that there is a higher dose inside the target volume in SRS15. Here was the conclusion that VMAT is better than IMRT in SRS and CHI is more suitable than HI in evaluated the dose distribution inside the target with a boost volume.
We must choose D l , D m and D h properly and carefully, especially D l . For example in SRS, the difference of the Target cDVH curve between VMAT and IMRT was apparent at the dose range 33–35 Gy (Fig. 2). If D l was selected in other values, we might get a wrong result. The selection of D m and D h was relatively easy as D m and D h were in the middle or the end of the plateau of the curve.
STD was the standard deviation of the Target differential DVH curve11 and used to assess the dose homogeneity inside the target volumes in this study. Table 2 indicated that STDs of Target and T-B were better in VMAT than those in IMRT for NPC, but the result of the paired T test showed that the differences between two techniques were insignificant at two-tailed significant level 0.05. On the other side, both CHI and STD of Target and T-B were statistically better in VMAT than those in IMRT for SRS (Table 2). The results aforementioned illustrated that STD was not superior to HI and CHI in evaluating the dose distribution inside a volume.
CHI and HI were defined with limited number of points in the Target curve of cDVH. The simplicity of the formula for HI was essential and made it attractive for people to quantify the dose homogeneity inside a volume11. We would like to propose that CHI will also be widely used in the near future. CHI was designed for assessing the dose distribution inside a target containing a boost volume. With the widespread use of SIB technique in the treatment for cancers, CHI is expected to be adopted as an index to evaluate the plan quality, along with the HI and conformity index.
References
Butler, E. B. et al. Smart (Simultaneous Modulated Accelerated Radiation Therapy) Boost: A New Accelerated Fractionation Schedule for the Treatment of Head and Neck Cancer with Intensity Modulated Radiotherapy. Int J Radiat Oncol Biol Phys. 45, 21–32 (1999).
Wu, Q., Mohan, R., Morris, M., Lauve, A. & Schmidt-Ullrich, R. Simultaneous Integrated Boost Intensity-Modulated Radiotherapy for Locally Advanced Head-And-Neck Squamous Cell Carcinomas. I: Dosimetric Results. Int J Radiat Oncol Biol Phys. 56, 573–585 (2003).
Orlandi, E. et al. Radiobiological Basis and Clinical Results of the Simultaneous Integrated Boost (SIB) in Intensity Modulated Radiotherapy (IMRT) for Head and Neck Cancer: A Review. Crit Rev Oncol Hematol. 73, 111–125 (2010).
Guerrero, M., Li, X. A., Earl, M. A., Sarfaraz, M. & Kiggundu, E. Simultaneous Integrated Boost for Breast Cancer Using IMRT: A Radiobiological and Treatment Planning Study. Int J Radiat Oncol Biol Phys. 59, 1513–1522 (2004).
Fiorentino, A. et al. Intensity Modulated Radiation Therapy with Simultaneous Integrated Boost in Early Breast Cancer Irradiation. Report of Feasibility and Preliminary Toxicity. Cancer Radiother. 19, 289–294 (2015).
Lee, H. H. et al. Intensity Modulated Radiotherapy with Simultaneous Integrated Boost Vs. Conventional Radiotherapy with Sequential Boost for Breast Cancer - a Preliminary Result. Breast. 24, 656–660 (2015).
Guerrero, M. et al. Simultaneous Integrated Intensity-Modulated Radiotherapy Boost for Locally Advanced Gynecological Cancer: Radiobiological and Dosimetric Considerations. Int J Radiat Oncol Biol Phys. 62, 933–939 (2005).
Wu, S. et al. Dosimetric Comparison of the Simultaneous Integrated Boost in Whole-Breast Irradiation After Breast-Conserving Surgery: IMRT, IMRT Plus an Electron Boost and VMAT. Plos One. 10, e120811, https://doi.org/10.1371/journal.pone.0120811 (2015).
De Rose, F. et al. Phase II Trial of Hypofractionated VMAT-based Treatment for Early Stage Breast Cancer: 2-Year Toxicity and Clinical Results. Radiat Oncol 11, 120, https://doi.org/10.1186/s13014-016-0701-z (2016).
International Commission on Radiation Units and Measurements. Report 50: Prescribing, recording, and reporting photon beam therapy. Bethesda, (MD:International Commission on Radiation Units and Measurements; 1993).
Yoon, M. et al. A New Homogeneity Index Based On Statistical Analysis of the Dose-Volume Histogram. J Appl Clin Med Phys. 8, 9–17 (2007).
Halperin, E. C., Perez, C. A. & Brady, L. W. Perez and Brady’s Principle and Practice of Radiation Oncology, 6th Edition: Lippincott Williams & Wilkins, Philadelphia, Pennsylvania, p8-9, 228–229 (2008).
Davies, K. R., Cantor, S. B. & Brewster, A. M. Better Contralateral Breast Cancer Risk Estimation and Alternative Options to Contralateral Prophylactic Mastectomy. Int J Womens Health. 7, 181–187 (2015).
Mondal, D. et al. Accelerated Hypofractionated Adjuvant Whole Breast Radiation with Simultaneous Integrated Boost Using Volumetric Modulated Arc Therapy for Early Breast Cancer: A Phase I/II Dosimetric and Clinical Feasibility Study From a Tertiary Cancer Care Centre of India. J Egypt Natl Canc Inst. 29, 39–45 (2017).
International Commission on Radiation Units and Measurements. Report 91: Prescribing, Recording, and Reporting of Stereotactic Treatments with Small Photon Beams. J. Seuntjens, (MD: International Commission on Radiation Units and Measurements; 2017).
Author information
Authors and Affiliations
Contributions
Mr. Q.L.: conceived the idea and reviewed the manuscript, Mr. J.M. and Dr. D.X.: designed the study and wrote the manuscript, Dr. Y.D., Dr. W.G. and Mr. J.M. collected the data.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mu, J., Xi, D., Ding, Y. et al. Chair Heterogeneity Index: Describing the dose heterogeneity inside the tumor volume where there is a boost volume. Sci Rep 8, 9763 (2018). https://doi.org/10.1038/s41598-018-28110-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28110-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.