Abstract
To examine the ability of total cholesterol (TC), a low-density lipoprotein cholesterol (LDL-C) proxy widely used in public health initiatives, to capture important population-level shifts away from ideal and intermediate LDL-C throughout adulthood. We estimated age (≥20 years)-, race/ethnic (Caucasian, African American, and Hispanic/Latino)-, and sex- specific net transition probabilities between ideal, intermediate, and poor TC and LDL-C using National Health and Nutrition Examination Survey (2007–2014; N = 13,584) and Hispanic Community Health Study/Study of Latinos (2008–2011; N = 15,612) data in 2016 and validated and calibrated novel Markov-type models designed for cross-sectional data. At age 20, >80% of participants had ideal TC, whereas the race/ethnic- and sex-specific prevalence of ideal LDL-C ranged from 39.2%-59.6%. Net transition estimates suggested that the largest one-year net shifts away from ideal and intermediate LDL-C occurred approximately two decades earlier than peak net population shifts away from ideal and intermediate TC. Public health and clinical initiatives focused on monitoring TC in middle-adulthood may miss important shifts away from ideal and intermediate LDL-C, potentially increasing the duration, perhaps by decades, that large segments of the population are exposed to suboptimal LDL-C.
Similar content being viewed by others
Introduction
The American Heart Association (AHA) “2020 Strategic Impact Goals for 2020 and Beyond” introduced the novel aim to improve cardiovascular health (CVH), which is measured by several indices, including total cholesterol (TC)1. High TC is a major risk factor for cardiovascular disease (CVD)2 and shows sex-and race/ethnic-specific patterning across the lifecourse3. Even though declines in mean TC have been observed over the past decades4, contemporary estimates suggest that 53.7% of United States (US) adults still do not meet the criteria for ideal TC5.
While TC is used frequently in health promotion initiatives, including AHA’s Life’s Simple 71, Healthy People 20206, and the SCORE Project7, it serves as a surrogate for low density lipoprotein (LDL-C)8. LDL-C, which carries most of the circulating cholesterol in the body and constitutes 60–70% of TC, is the primary target for cholesterol lowering treatment, with LDL-C lowering drug therapies shown to reduce CVD risk9. Although TC is easier to measure than LDL-C, as it can be assessed directly through a lipid panel6, few studies have evaluated how well TC transitions across adulthood mirror LDL-C transitions in contemporary diverse populations10, despite the utility of such research to inform the targeting of interventions to maintain or improve ideal cholesterol levels11. One possible reason why so few studies have contrasted TC and LDL-C transitions across adulthood among diverse populations is that such investigations would require decades-long longitudinal studies including multiple race/ethnicities to evaluate how cholesterol changes over adulthood. However, given strong secular trends in health behaviors and risk factors known to affect TC and LDL-C (e.g. physical activity, adiposity, and diet)12,13,14, results from longitudinal studies may not be generalizable to contemporary settings. Longitudinal studies also likely do not adequately capture populations who have undergone demographic shifts over the past decades, including Hispanic/Latinos. Therefore, using a novel extension to traditional Markov-type state transition models, we addressed these research gaps by estimating age, sex- and race/ethnic-specific net transition probabilities between ideal, intermediate, and poor cholesterol as measured by TC and LDL-C in African American, Caucasian, and Hispanic/Latino male and female populations using contemporary cross-sectional data15.
Results
A maximum of 29,196 participants (14.6% African American; 32.0% Caucasian; 53.4% Hispanic/Latino) were included in this analysis (Table 1). At age 20, the prevalence of ideal TC ranged from 79.0% (Hispanic/Latino men) to 89.7% (Hispanic/Latino women), notably higher than the prevalence of ideal LDL-C, which ranged from 38.2% (Hispanic/Latino men) to 59.6% (African American women) (Supplementary Figs S1, S2). Additionally, to assess the influence of small changes in cholesterol levels on net transition probabilities, we evaluated TC and LDL-C medians (IQRs) and found the values were distinct from category-specific cutpoints (Supplementary Table S1).
Net transition probabilities from ideal to intermediate to poor TC
Net transition probability patterns from ideal to intermediate TC across adulthood varied by race/ethnicity and sex. For example, net transition probabilities from ideal to intermediate TC peaked earlier for men than women, with peak net transition probabilities among men occurring between age 36 (African American and Caucasian) and 37 (Hispanic) (Supplementary Fig. S3). For example, a net 2.5% (95% CI: 1.6%, 3.5%) of African American men aged 36 years of age with ideal TC transitioned to intermediate TC by age 37. For women, peak ideal to intermediate TC net transition probabilities occurred between 42 (Caucasian) and 57 years (African American) of age.
In contrast to ideal to intermediate TC net transition probabilities that suggested distinct net transition probability patterns by sex that peaked in middle adulthood, net transition probabilities from intermediate to poor TC peaked approximately 15 years earlier and differed more by race/ethnicity than sex (Supplementary Fig. S4). For example, net transition probabilities from intermediate to poor TC peaked at age 20, the youngest age under investigation, for both Caucasian men (net transition probability = 3.6% [95% CI: 2.5%, 4.7%]) and Caucasian women (net transition probability = 3.0% [95% CI: 2.0%, 3.9%]). In contrast, intermediate to poor TC net transition probabilities were approximately equivalent through age 40 for African Americans and Hispanic/Latinos.
Net transition probabilities from ideal to intermediate to poor LDL-C
In contrast to ideal to intermediate TC net transition probabilities that peaked between 36–57 years of age, net transition probabilities from ideal to intermediate LDL-C peaked considerably earlier; by age 29 for men (age range: 26–29) and age 46 for women (age range: 32–46) (Supplementary Fig. S5).
Liken to net transition results from intermediate to poor TC, all net transition probabilities from intermediate to poor LDL-C also peaked before age 40 (age range: 20–36), although intermediate to poor LDL-C net transition probabilities were approximately equivalent for African Americans and Caucasians (Supplementary Fig. S6). Also, intermediate to poor LDL-C net transition probabilities in African American men and women were notably less precise than intermediate to poor LDL-C net transition probabilities estimated in Caucasian and Hispanic/Latino men and women.
Population Extrapolations
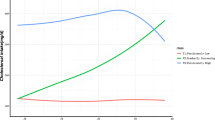
Finally, we extrapolated results to Caucasian and African American 2010 civilian noninstitutionalized men and women aged 20 years and greater. As described above, extrapolating age-, sex-, and race/ethnic-specific net transition probabilities allowed us to combine estimates of relative effect size (in example net transition probabilities) with population size estimates and ideal and intermediate TC and LDL-C prevalence estimates, facilitating examination of the one-year age-specific net number of African American and Caucasian men and women transitioning to intermediate and poor TC and LDL-C. Overall, net population extrapolations demonstrated considerable variation between TC and LDL-C in the ages associated with the largest shifts away from ideal and intermediate TC and LDL-C. For example, in contrast to ideal to intermediate TC net population extrapolations, which suggested that the largest one-year net population shifts occurred in mid-life for African Americans and Caucasians, these same net population extrapolations for LDL-C peaked at age 20, after which steep declines were observed (Figs 1 and 2). Results for intermediate to poor TC and LDL-C showed a slightly different picture that varied by sex; here we focused on Caucasians given limited precision of estimated net transition probabilities in African Americans. Specifically, among Caucasian men, the largest net population shifts from intermediate to poor LDL-C occurred at age 20, again in contrast with one-year net population extrapolations estimated for intermediate to poor TC, which suggested that net population transitions from intermediate to poor TC were approximately constant through age 40. For Caucasian women, TC and LDL-C intermediate to poor net population extrapolations were consistent, suggesting approximately constant age-specific net population transitions until 40 years of age, when declines in LDL-C net transitions were observed. Equivalent declines in TC were not observed until 10 years later at 50 years of age. Additionally, extrapolation to the 2010 Hispanic/Latino population within HCHS/SOL study center census tracts displayed high variability between net population increases, likely due to the smaller sample size of census tract populations (Supplementary Fig. S7), although TC and LDL-C net population extrapolations remained constant through age 40 for both men and women.
Discussion
In this study, we showed that net population shifts toward intermediate and poor LDL-C levels in adulthood peaked approximately 20 years earlier than net population shifts toward intermediate and poor TC. Variation by sex was also observed, with the magnitude of decline in intermediate and poor LDL-C net population shifts occurring more rapidly for men than women. Overall, these results suggest public health and preventive medicine initiatives monitoring TC in mid-adulthood may miss important shifts away from ideal and intermediate LDL-C that occur as early as age 20.
Although past studies have found TC and LDL-C to be highly correlated16, TC levels are easier to collect compared to LDL-C17. Yet, as we demonstrated herein, focusing on TC as a surrogate to LDL-C could direct population-wide interventions and goals toward midlife. Although consistent with prior longitudinal research examining TC transitions in mid-adulthood18, this focus would target populations approximately one to two decades after peak net population shifts away from ideal and intermediate LDL-C occurred. Reliance on TC to monitor and direct initiatives therefore has the potential to increase the duration, perhaps by decades, that large segments of the population are exposed to suboptimal LDL-C levels, increasing CVD risk19.
Re-evaluation of public health efforts to maintain ideal levels of LDL-C throughout adulthood are therefore warranted, especially among younger male populations for whom net transitions away from ideal and intermediate LDL-C are highest, but are less likely to receive routine medical care including routine cholesterol screening20. Indeed, the American Heart Association/American College of Cardiology (AHA/ACC) recommended that risk reduction should begin as early as possible in order to effectively reduce lifetime risk of CVD, suggesting every adult ≥20 years of age receive cholesterol screenings every five years. However, the low levels of preventive service utilization highlight the need to strengthen preventive efforts beyond the clinic and before LDL-C levels become elevated, especially in light of adverse effects of prolonged exposure to even moderate elevations in TC and LDL-C on CVD risk (in example primordial prevention)19. Dietary and lifestyle interventions are key components of such primordial prevention initiatives. For example, the AHA/ACC Guidelines on Lifestyle Management to Reduce Cardiovascular Risk21 endorsed dietary patterns such as the DASH dietary pattern, which lowered LDL-C by 11 mg/dl (9.3% relative change from baseline) compared to an American diet in the 1990s21,22. Indeed, for every 1% reduction in LDL-C levels, dietary trials have shown the relative risk for major CVD events is reduced by approximately 1%22, emphasizing that even modest LDL-C reductions represent a meaningful and effective goal if sustained over the course of early life23,24. Public health initiatives to reduce LDL-C are not limited to adult populations. For example, the Special Turku Coronary Risk Factor Intervention Project (STRIP) initiated low saturated fat diets and parental counseling for infants and observed lower LDL-C levels in the intervention group compared to the control group at multiple follow-up time points spanning 3 years to 19 years23,24, which is relevant given the modest prevalence of ideal LDL-C observed at the beginning of adulthood.
Additionally, increased primordial prevention is important for populations with intermediate LDL-C, given that large segments of the population transition into poor LDL-C, have difficulties retaining intermediate or ideal levels, and are ineligible for treatment under current guidelines25. Previous clinical trials have shown diet and exercise interventions to reduce LDL-C by up to 11 mg/dl in trial settings among older participants and those with poor LDL-C levels22. While promoting healthier lifestyles may delay the progression of elevated LDL-C levels and shift large segments of the population back to healthier LDL-C levels, the degree to which modest population-wide lifestyle shifts could delay net transitions away from ideal LDL-C and subsequently elevated CVD risk deserves further evaluation.
It is important to note that our results demonstrating the divergence between population-wide LDL-C and TC net population shifts complement rather than oppose current cholesterol treatment guidelines. For example, current cholesterol treatment guidelines recommended by the American College of Cardiology/American Heart Association suggest evaluating traditional clinical risk factors, while recommendations from the European Society of Cardiology/European Atherosclerosis Society also consider factors such as elevated triglyceride, social deprivation, central obesity, elevated lipoprotein (a), subclinical atherosclerosis, or family history of CVD as part of a global risk score to calculate total CVD risk25,26. In contrast to cholesterol treatment guidelines that assess CVD risk for treatment purposes, our study highlights populations most at-risk and the most appropriate metric to monitor LDL-C levels to prevent peak net population shifts away from ideal LDL-C. The biggest gains in primordial prevention will occur from targeting young adults before net population shifts away from ideal LDL-C occur to ensure populations maintain ideal levels and delay exposure to elevated CVD risk.
Past research examining cholesterol through the life course has been limited by short follow-up periods4, examination of specific life epochs (in example childhood)10, use of non-contemporary data27, or restrictions to largely Caucasian populations28. Our present study was developed to respond to these limitations and instead utilized contemporary, population-based studies of multiethnic populations that spanned early to late adulthood, enabled by the application of novel statistical methodology15. Additionally, we limited examination to one-year net transition probabilities in an attempt to avoid introducing biases from age-specific factors (in example reasons for immigration) that could influence longer-term age-specific effects. Furthermore, we conducted the analyses separately for each race/ethnicity and reported results for Hispanic/Latino men and women separately from African American and Caucasian men and women, reducing the extent differences between studies may have influenced results. Yet, several limitations must be noted. Our study did not examine children because age-specific changes in cholesterol profiles across childhood may reflect screening inaccuracies during pubertal years. Second, while it might be useful to quantitate the extent to which transitions are accounted for by small increments in TC and LDL-C, it would likely require longitudinal data to calculate the individual transitions instead of the net transition probabilities from cross-sectional data presented by this study. Third, although net transition probabilities highlight important population level movements, however, they may not be well-suited for examining the complex interplay between cholesterol sub-fractions (LDL-C, high density lipoprotein, and triglycerides), motivating future studies that evaluate these metrics longitudinally. Fourth, we were unable to evaluate the influence of other factors that may affect net transition probabilities (in example diet9 or physical activity14) as this examination would require further stratification of our data, likely beyond the ability of the current sample sizes.
Using TC as an indicator for LDL-C may miss population shifts toward intermediate and poor LDL-C that occur in early adulthood. Population-wide initiatives that maintain ideal levels of LDL-C in early adulthood through lifestyle changes can be an effective approach to prevent elevated levels of LDL-C and subsequent downstream CVD events and deserve further evaluation.
Methods
Study Populations
We characterized the ages at which African American, Caucasian, and Hispanic/Latino populations transitioned between ideal, intermediate, and poor TC and LDL-C using cross-sectional data from two population-based studies: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL)29 and the National Health and Nutrition Examination Survey (NHANES)30. The following review boards approved the study: Institutional Review Board (IRB) of Albert Einstein College of Medicine (Montefiore Medical Center), IRB of Feinberg School of Medicine at Northwestern University, IRB of Miller School of Medicine at the University of Miami, and the San Diego State University IRB. In addition, all participants in both NHANES and HCHS/SOL provided informed consent and methods were performed in accordance with the relevant guidelines and regulations.
The HCHS/SOL is a population-based cohort designed to examine risk and protective factors for chronic diseases and to quantify morbidity and mortality prospectively29. At study baseline (2008 to 2011), 16,415 Hispanic/Latino men and women aged 18–76 years who self-identified as Hispanic/Latino were enrolled from sampled households in four US communities (Bronx, NY; Chicago, IL; Miami, FL; San Diego, CA). For this study, we evaluated n = 15,612 HCHS/SOL participants aged 20–75 years of age at baseline.
NHANES includes demographic, nutritional, and health status information on a nationally representative biennial probability sample of the US civilian population (aged 0–80+ years)30. For this study, we used data from the four most contemporary NHANES population cross-sections (2007–2014) and evaluated Caucasian and African American populations aged 20–75 years. We excluded non-Hispanic Asian participants who were available as of the 2011–12 population cross-section as well as participants who identified as “Mexican American”, “Other Hispanic” or “Other Race – Including Multi-Racial” due to small sample sizes, particularly for Hispanic/Latino populations when compared to the HCHS/SOL study.
Measurement and classification of TC and LDL-C
TC (mg/dl) was measured using a cholesterol oxidase enzymatic method and characterized using AHA defined cutpoints as ideal (<200 mg/dl untreated), intermediate (200–239 mg/dl or treated to goal), or poor (≥240 mg/dl)1. Although AHA did not define ideal, intermediate, and poor LDL-C, we used the National Cholesterol Education Program (NCEP) Adult Treatment Panel III categories17. Briefly, LDL-C (mg/dl),measured among participants reporting fasting for at least eight hours, was calculated using the Friedewald equation, and was characterized as ideal (<100 mg/dl untreated), intermediate (100–130 mg/dl or treated to <100 mg/dl), or poor (>130 mg/dl)31. Medication data were collected using medication inventories. Participants were asked to provide containers for medications taken in the last 30 days. If any of the medications reported were lipid-lowering medications, the participants were classified as current lipid-lowering medication users.
Statistical analysis
Estimation of net transition probabilities
We characterized the ages at which African American, Caucasian, and Hispanic/Latino populations transitioned between ideal, intermediate, and poor TC and LDL-C categories using cross-sectional data from HCHS/SOL and NHANES, and statistical models that estimate one-year net transition probabilities15. For example, in a longitudinal study of 100 participants with ideal TC aged 20 years, if 10 participants transitioned from ideal to intermediate TC by age 21 and three participants transitioned from intermediate to ideal TC by age 21, the ideal-to-intermediate TC net transition would be seven participants; dividing by the number of ideal TC participants at age 20 (n = 100) would yield the net transition probability, which in this case is 7%. The intermediate to ideal TC net transition is defined as 0 because fewer participants moved from intermediate to ideal TC than from ideal to intermediate TC15. Under the assumption that the age-specific TC and LDL-C transitions probabilities remained approximately stable across time (see Supplementary Information), we can use cross-sectional data to estimate net transition probabilities; estimation of the number of participants transitioning from ideal to intermediate TC and intermediate to ideal TC (in example individual transition probabilities) would require longitudinal data.
Estimation of net transition probabilities from cross-sectional data required three steps. First, we estimated the age-, sex-, and race/ethnic-specific prevalence of each category (in example ideal; intermediate; poor) using a multinomial logit model32,33 and P-spline smoothing34. Cluster sampling methods were used to accommodate family structure (HCHS/SOL) and complex sampling designs (HCHS/SOL and NHANES). Next, we used a series of simplex algorithms from linear programming theory to estimate age-, sex-, and race/ethnic-specific net transition probabilities (see Supplementary Information). Results were then examined and showed exceptional calibration and validation (see Supplementary Information). Finally, bootstrapping was used to estimate 95% confidence intervals (95% CI), where the age-specific prevalence was simulated from its asymptotic distribution and net transition probabilities were computed for each simulated prevalence15.
Finally, we extrapolated our results to African American and Caucasian 2010 civilian, non-institutionalized U.S. population and to the 2010 Hispanic/Latino population within HCHS/SOL community census tracts to estimate the net population of individuals transitioning between TC and LDL-C levels. Extrapolation was accomplished by multiplying the age, sex-, and race/ethnicity-specific net transition probabilities (e.g., ideal to intermediate) by the prevalence of the initial TC and LDL-C level (e.g., ideal) and the appropriate age-, race/ethnicity-, and sex-specific 2010 population sizes. Statistical analyses were performed using SAS (Cary, NC), STATA (College Station, TX), and R (Vienna, Austria). All data analyses took place in 2016.
Data availability
The NHANES dataset generated during and analyzed during the current study is available from the corresponding author on reasonable request; however, HCHS/SOL dataset cannot be made publically available without consent from the HCHS/SOL study.
Change history
13 April 2018
A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has not been fixed in the paper
References
Lloyd-Jones, D. M. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613, https://doi.org/10.1161/CIRCULATIONAHA.109.192703 (2010).
Kronmal, R. A., Cain, K. C., Ye, Z. & Omenn, G. S. Total serum cholesterol levels and mortality risk as a function of age. A report based on the Framingham data. Archives of internal medicine 153, 1065–1073 (1993).
Keys, A. et al. The seven countries study: 2,289 deaths in 15 years. Preventive medicine 13, 141–154 (1984).
Carroll, M. D., Kit, B. K., Lacher, D. A., Shero, S. T. & Mussolino, M. E. Trends in lipids and lipoproteins in US adults, 1988-2010. JAMA: the journal of the American Medical Association 308, 1545–1554, https://doi.org/10.1001/jama.2012.13260 (2012).
Mozaffarian, D. et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation 131, e29–322, https://doi.org/10.1161/CIR.0000000000000152 (2015).
People, H. 2020. (2010). Healthy People 2020 (2013).
Conroy, R. et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. European heart journal 24, 987–1003 (2003).
Bachorik, P. S. & Ross, J. W. National Cholesterol Education Program recommendations for measurement of low-density lipoprotein cholesterol: executive summary. The National Cholesterol Education Program Working Group on Lipoprotein Measurement. Clinical chemistry 41, 1414–1420 (1995).
Rifkind, B. The Lipid Research Clinics Coronary Primary Prevention Trial Results. 2. The Relationship of Reduction in Incidence of Coronary Heart-Disease to Cholesterol Lowering. Jama-Journal of the American Medical Association 251, 365–374 (1984).
Dai, S. et al. Blood lipids in children: age-related patterns and association with body-fat indices: Project HeartBeat! American journal of preventive medicine 37, S56–S64 (2009).
Bambs, C. et al. Low prevalence of “ideal cardiovascular health” in a community-based population: the heart strategies concentrating on risk evaluation (Heart SCORE) study. Circulation 123, 850–857, https://doi.org/10.1161/CIRCULATIONAHA.110.980151 (2011).
Ogden, C. L. & Carroll, M. D. Prevalence of overweight, obesity, and extreme obesity among adults: United States, trends 1960–1962 through 2007–2008. National Center for Health Statistics 6, 1–6 (2010).
Popkin, B. M., Siega-Riz, A. M. & Haines, P. S. A comparison of dietary trends among racial and socioeconomic groups in the United States. New England Journal of Medicine 335, 716–720 (1996).
Simpson, M. E. et al. Walking trends among US adults: the behavioral risk factor surveillance system, 1987–2000. American journal of preventive medicine 25, 95–100 (2003).
Kassteele, J., Hoogenveen, R. T., Engelfriet, P. M., Baal, P. H. & Boshuizen, H. C. Estimating net transition probabilities from cross-sectional data with application to risk factors in chronic disease modeling. Statistics in medicine 31, 533–543, https://doi.org/10.1002/sim.4423 (2012).
Castelli, W. P. et al. Distribution of triglyceride and total, LDL and HDL cholesterol in several populations: a cooperative lipoprotein phenotyping study. Journal of chronic diseases 30, 147–169 (1977).
National Cholesterol Education Program Expert Panel on Detection, E. & Treatment of High Blood Cholesterol in, A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106, 3143–3421 (2002).
Statistics, N. C. f. H. Health, United States, 2015: with special feature on racial and ethnic health disparities (2016).
Navar-Boggan, A. M. et al. Hyperlipidemia in early adulthood increases long-term risk of coronary heart disease. Circulation, CIRCULATIONAHA. 114, 012477 (2015).
Callahan, S. T. & Cooper, W. O. Changes in ambulatory health care use during the transition to young adulthood. Journal of Adolescent Health 46, 407–413 (2010).
Eckel, R. H. et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology 63, 2960–2984, https://doi.org/10.1016/j.jacc.2013.11.003 (2014).
Grundy, S. M. et al. Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. Journal of the American College of Cardiology 44, 720–732 (2004).
Gillman, M. W. Primordial prevention of cardiovascular disease. Circulation 131, 599–601, https://doi.org/10.1161/CIRCULATIONAHA.115.014849 (2015).
Niinikoski, H. et al. Effect of repeated dietary counseling on serum lipoproteins from infancy to adulthood. Pediatrics, peds. 2011–1503 (2012).
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology 63, 2889–2934, https://doi.org/10.1016/j.jacc.2013.11.002 (2014).
Reiner, Ž. et al. ESC/EAS Guidelines for the management of dyslipidaemias. European heart journal 32, 1769–1818 (2011).
Anderson, K. M., Castelli, W. P. & Levy, D. Cholesterol and mortality: 30 years of follow-up from the Framingham Study. JAMA: the journal of the American Medical Association 257, 2176–2180 (1987).
Anderson, K. M., Wilson, P. W., Garrison, R. J. & Castelli, W. P. Longitudinal and secular trends in lipoprotein cholesterol measurements in a general population sample The Framingham offspring study. Atherosclerosis 68, 59–66 (1987).
Sorlie, P. D. et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Annals of epidemiology 20, 629–641, https://doi.org/10.1016/j.annepidem.2010.03.015 (2010).
Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey, http://www.cdc.gov/nchs/nhanes.htm (2012).
Friedewald, W. T., Levy, R. I. & Fredrickson, D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry 18, 499–502 (1972).
Hosmer, D. W. & Lemeshow, S. Applied Logistic Regression, Second Edition. (Wiley, 2000).
McCullagh, P. & Nelder, J. Generalized Linear Models, Second Edition. (Chapman and Hall/CRC, 1989).
Eilers, P. H. C. & Marx, B. D. Flexible smoothing with B-splines and penalties (with discussion). Statistical Science 11, 89–121 (1996).
Acknowledgements
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201300025C & HHSN268201300026C), Northwestern University (HHSN268201300027C), University of Minnesota (HHSN268201300028C), Kaiser Foundation Research Institute (HHSN268201300029C), and Johns Hopkins University School of Medicine (HHSN268200900041C). CARDIA is also partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intra-agency agreement between NIA and NHLBI (AG0005). This manuscript has been reviewed by CARDIA for scientific content. This work was supported by National Heart, Lung, and Blood Institute training grant T32 predoctoral fellow T32HL007055.
Author information
Authors and Affiliations
Contributions
J.C.E. served as the main author for the manuscript. K.M.H., S.T.H., G.A.T., B.V.H., M.L.D., A.P. and P.J.S. helped write the main manuscript. S.C., D.L. and D.Z. helped complete the analyses. C.L.A. helped construct the idea of the manuscript and helped write the main text of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Engeda, J.C., Holliday, K.M., Hardy, S.T. et al. Transitions from Ideal to Intermediate Cholesterol Levels may vary by Cholesterol Metric. Sci Rep 8, 2782 (2018). https://doi.org/10.1038/s41598-018-20660-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-20660-2
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.